Abstract
Purpose
To systematically review the available literature regarding outcomes for the treatment of anterior cruciate ligament (ACL) injuries in the skeletally immature at skeletal maturity or more than five years after surgery.
Methods
A systematic search was performed of seven online databases for literature reporting patient reported outcomes for the treatment of ACL injuries in the skeletally immature. A systematic review of this literature was performed examining the outcomes and their association with skeletal immaturity and treatment techniques.
Results
A total of 18 articles reported the outcomes of 425 subjects. The mean age at surgery ranged from 10.3 to 15 years. Mean follow-up ranged from 36 to 163 months. Ten studies followed up subjects until skeletal maturity. Mean outcome scores were similar for extraphyseal (Lysholm 96.2 (95.7 to 97.4), Tegner 6.75, IKDC 95.4 (94 to 100)) and transphyseal surgery (Lysholm 94.3 (84.6-100), Tegner 7.6 (6 to 8.7), International Knee Documentation Committee (IKDC) 93.6 (84 to 99)). However, the lower range boundary for Lysholm and IKDC was worse for the transphyseal group. The results for non-surgical treatments were worse (Lysholm 63.2, Tegner 4.8, IKDC 87). No significant differences were found in the incidence of limb-length discrepancy (p = 0.32), coronal plane growth disturbance (p = 0.48), graft rupture (p = 0.88) and persistent symptomatic instability (p = 0.11) with transphyseal and extraphyseal surgical techniques.
Conclusion
Both transphyseal and extraphyseal reconstructive techniques produced good patient reported outcomes, with no significant differences in the incidence of limb-length discrepancy, coronal plane growth disturbance, graft rupture and persistent symptomatic instability. They compare favourably with the repair techniques reviewed and the natural history of the condition. Further high-quality studies comparing the transphyseal and extraphyseal techniques are required.
Level of Evidence
Level IV
Keywords: Patient reported outcomes, anterior cruciate ligament, skeletal immaturity, ACL reconstruction, systematic review
Introduction
The incidence of anterior cruciate ligament (ACL) injuries amongst paediatric patients has been increasing over the last 20 years, with rates currently estimated to be 12 per 10 000 patient-years.1 Multiple factors are believed to contribute to this increase, including higher sports participation from an earlier age, and an increased awareness and recognition of this injury.1 Several studies have demonstrated an increased risk of further injury and poor functional outcomes with non-surgical management of these injuries.2,3 A recent meta-analysis has suggested a benefit with early surgical reconstruction in this group compared with non-surgical treatment4 and rates of surgical reconstruction of these injuries are increasing.5
The surgical treatment of ACL injuries in skeletally immature patients has produced extensive debate in the literature regarding the relevance of the physis to surgical treatments. Physeal injury during ACL reconstruction is a recognized complication resulting in a variety of deformities associated with abnormal growth. Injury to the physis in the growing skeleton produces deformities that occur over time with growth, resulting in leg-length discrepancies (LLDs) and angular deformities around the knee.6 Several surgical techniques for the treatment of the ACL injuries in this group have been described to minimize these risks. These techniques have included primary repair7 and reconstruction that avoids the physis (extraphyseal).8-10 However, adult-like surgical reconstruction that crosses the physis (transphyseal)11-13 is also a widely-accepted technique. Much of the available literature on these techniques consists of longitudinal case series with varying durations of follow-up.14 The duration of all these studies may not allow for the effect of these growth deformities on patient reported outcomes to be demonstrated. There have been no reviews of the literature concerning outcomes exclusively in the long term or at skeletal maturity, thus allowing the effect of growth deformities to be seen.
The measurement of outcomes with objective clinical tests alone may not sufficiently capture patient experience and the use of patient reported outcome measures (PROMS) have become an important tool to evaluate this.15 This review will, therefore, focus on patient reported outcomes as a measure of success in the treatments reviewed.
The aim of this review is to evaluate the patient reported outcomes for the treatment of ACL injuries in the skeletally immature. The long-term outcomes or outcomes at skeletal maturity will be explored. The relationship between skeletal immaturity, surgical techniques and outcomes will be reviewed.
Materials and methods
A systematic review of the literature relevant to patient reported outcomes for the treatment of ACL injuries in the skeletally immature was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.16
The search terms ‘anterior cruciate ligament’ or the abbreviation ‘ACL’, were used in conjunction with several terms to identify a skeletally immature population with ACL injuries. The search terms used were ‘skeletally immature’, ‘paediatric’, ‘pediatric’, ‘juvenile’, ‘adolescent’, ‘teenage’ and ‘child’. No limitations were placed on the search, e.g. language or study type.
An online search of seven literature databases was performed in May 2017 to identify all relevant literature. The databases searched were MEDLINE, Embase, CENTRAL, Scopus, Web of Knowledge, Sport Discus and CINAHL. After exclusion of duplicate literature, all titles and abstracts were reviewed by the author (CB). A full text review was then performed on those articles identified as relevant to this study or where the relevance could not be determined from the title and abstract. Only those articles available in full text online and in the English language were reviewed. Articles were excluded from the full text review if electronic copies were not available online.
Articles were considered eligible for inclusion in this review where:
the population studied was skeletally immature;
a radiologically, or intraoperatively, proven complete tear of the ACL was present in the treated population;
follow-up of five or more years, or until skeletal maturity, with PROMs recorded at final follow-up.
Studies in which all subjects were not skeletally immature at the time of surgery or where this was not made clear were excluded. Articles that included partial tears of the ACL, bony avulsion injuries and congenital aplasia of the cruciates were also excluded. Articles with less than five years follow-up and where the final evaluation was before skeletal maturity or this was not clear were excluded. Single case reports, multiple publications and review articles were excluded.
Skeletal immaturity
Across the studies reviewed, several means to evaluate skeletal immaturity where used. There was no generalized consensus regarding a definition of skeletal immaturity. Radiological assessments of physeal patency at the distal femur and proximal tibia; bone age estimates using Greulich and Pyle’s Atlas;17 Tanner stages,18 which are a measure of physical development and correlate with growth velocity; and the Green-Anderson growth remaining model19, were all used to estimate skeletal maturity and the potential for remaining growth. For the purpose of inclusion, in this review skeletal immaturity was defined as the presence of open physes on radiological imaging (x-ray or MRI) and remaining growth potential. Remaining growth potential was assumed using skeletal age, growth prediction tools or Tanner stages 1 to 3 (in which less than 5% have reached peak growth velocity).18 Studies in which subjects were identified as having little or no growth potential were excluded.
Patient reported outcomes
There are numerous PROMS used to assess the outcomes following ACL injury and treatment. The Lysholm knee score is a validated tool used to evaluate functional instability in the young active patient. It is scored across eight domains with a score > 90 representing an excellent outcome.20 The Tegner activity rating scale complements the Lysholm score, evaluating the subject’s level of activity. It is scored from 0 to 10, where 10 represents competitive sports at national level.20 These two scores together are deemed to be the benchmark in ACL outcome scores.21 The International Knee Documentation Committee (IKDC) Subjective Knee Form and the population-specific Paediatric IKDC are used to evaluate subjective function following knee ligamentous injury and treatment, with equivalent results obtained in this population using either score.22 It is scored out of 100, with high scores representing high function and low symptom levels. The Knee injury and Osteoarthritis Outcome Score (KOOS) is a knee specific outcome score for younger, higher activity patients with knee injuries and arthritis and incorporates a measure of health-related quality of life.23
Treatments
Several strategies are reported for the treatment of ACL injuries in the skeletally immature. Non-surgical treatment for ACL injuries typically involves rehabilitation, bracing or reduction in activity. Various repair techniques of the ruptured ACL have been described, although many of these original techniques been abandoned due to the poor outcomes and high failure rates.7
Reconstruction of the ACL in the skeletally immature can broadly be divided into two groups, those in which the physis is breached (transphyseal) and those in which the physis is spared (extraphyseal). The transphyseal technique involves the drilling of bone tunnels across one or both of the femoral and tibial physes. A ligament or tendon graft is placed within the tunnels to restore stability and function. This graft also acts to prevent bony bar formation across the physis.24 This technique more closely replicates adult reconstruction techniques. Extraphyseal techniques do not involve placing bone tunnels across the physis. The modified Macintosh technique describes an extraphyseal, combined intra- and extra-articular reconstruction, where an iliotibial band graft is passed over the top of the lateral femoral condyle and into the joint, avoiding the physes.8-10 Hybrid techniques, in which a transphyseal technique is used within the tibia and an extraphyseal technique is used with in the femur have also been described.11 Finally, techniques involving graft fixation within the epiphysis, sparing the physis, have been described.25,26
Methodological appraisal and risk of bias
An assessment of the methodological quality of the included studies was undertaken using the modified Coleman Methodology Score. This is a recognized tool for the evaluation of the quality of studies of orthopaedic treatments, including ACL reconstruction.28 The Cochrane Collaborations tool for assessing risk of bias was also used to evaluate bias within the included studies.28
Data extraction
Demographic data were extracted from each study. These included the number of subjects, gender, age at time of surgery, associated injuries, follow-up and evidence of skeletal maturity at follow-up. Evidence of skeletal immaturity, Tanner stage and other evidence of growth remaining at the time of surgery were recorded. Information concerning surgical and non-surgical treatments was recorded. Where surgical treatments were undertaken, data were extracted regarding surgical techniques (transphyseal or extraphyseal), graft type, graft fixation and time to surgery. Follow-up data concerning growth arrest, LLD, angular deformities and other complications were collected. A LLD of > 1 cm was deemed to be clinically significant.29 Outcome scores at final follow-up (Tegner, Lysholm, IKDC) and return to sport were also recorded. Data were collected onto a database and the literature searched managed using Mendeley reference management software (Mendeley Ltd, London, United Kingdom).
Statistical analysis
Descriptive systematic analysis of the synthesized data was performed. Pooled means and sds were calculated where possible to describe continuous variables according to treatment type and potential growth remaining. Chi-squared testing was used to analyze categorical outcomes. Statistical analysis was performed using SPSS (IBM, New York, New York).
Review
Study selection
The search strategy utilized identified 4996 unique articles. In all, 4934 articles were excluded during screening of the titles and abstracts. A total of 62 articles underwent full text review using the specified inclusion and exclusion criteria, and 44 articles were excluded as they did not meet the inclusion criteria. The remaining 18 articles will be discussed in this review (Fig. 1).
Figure 1.
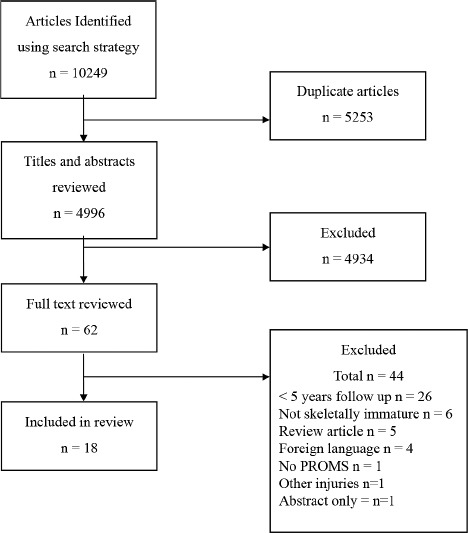
Search strategy and results (PROMs, patient reported outcomes measures).
Study characteristics
The 18 studies included in this review are summarized in Table 1. A total of 425 subjects were included in all the studies, the mean number of subjects was 21 (5 to 68). The level of evidence for the included papers in this systematic review ranged from level II to level IV. One paper presented the results of a prospective cohort study,3 one of a retrospective cohort study2 and the remainder from case series. The mean age at the time of surgery ranged from 10.3 to 15 years old. Two studies compared transphyseal reconstruction and conservative treatment (35 subjects);2,3 in one of these studies only the conservative treatment arm was included as the surgical arm did not meet the inclusion criteria.2 In all, 11 articles (256 subjects) reported the use of a transphyseal or hybrid reconstruction techniques. Four articles (126 subjects) reported on an extraphyseal reconstruction technique. Mean follow-up in each study was from 36 to 163 months. Where the average follow-up was less than 60 months, all subjects in these studies were followed up until skeletal maturity. Ten studies followed up subjects until skeletal maturity.
Table 1.
Summary of included studies
| Author | Study type | n | M/F | Mean age at surgery, yrs (range) | Treatment | Mean follow-up, mths | Skeletal maturity at final follow-up |
| Engebretsen et al,7 1988 | Case series | 8 | 2/6 | 15 (13 to 16) | Extraphyseal repair | 65 | No |
| Lo et al,11 1997 | Case series | 5 | 12.9 (8 to 14) | Hybrid | 88 | No | |
| Micheli et al,8 1999 | Case series | 17 | 7/1 | 11 (2 to 14) | Extraphyseal | 63 | Yes |
| Aichroth et al,2 2002 | Retrospective cohort | 68 | 48/20 | 13 (11 to 15) | Conservative/transphyseal | 72 | Yes |
| Guzzanti et al,26 2003 | Case series | 8 | 5/0 | 11.15 (10 to 12) | Extraphyseal | 69.2 | Yes |
| Seon et al,30 2005 | Case series | 11 | 11/0 | 14.7 (13.1 to 15.5) | Transphyseal | 77.7 | Yes |
| Kocher et al,9 2006 | Case series | 44 | 10.3 | Extraphyseal | 63.6 | No | |
| Mcintosh et al,31 2006 | Case series | 16 | 11/5 | 13.8 (11.2 to 14.9) | Transphyseal | 41.1 | Yes |
| Kopf et al,32 2010 | Case series | 14 | 8/6 | 14.4 (11 to 16) | Transphyseal | 94 | No |
| Streich et al,3 2010 | Prospective cohort | 28 | 17/11 | 11 (9 to 12) | Conservative/transphyseal | 70 | No |
| Courvoisier,13 2011 | Case series | 37 | 17/20 | 14 (11 to 15) | Transphyseal | 36 | Yes |
| Bonnard et al,10 2011 | Case series | 57 | 43/13 | 12.2 (6.8 to 14.5) | Extraphyseal | 66 | Yes |
| Kumar et al,12 2013 | Case series | 32 | 28/4 | 11.25 (9.5 to 14) | Transphyseal | 72.3 | No |
| Calvo et al,33 2014 | Case series | 27 | 16/11 | 13 (12 to 16) | Transphyseal | 127.2 | No |
| Placella et al,34 2016 | Case series | 24 | 14/10 | 13.15 (9 to 14) | Transphyseal | 96 | No |
| Falciglia et al,35 2016 | Case series | 33 | 27/6 | 12.4 (10 to 14.2) | Transphyseal | 163 | Yes |
| Domzalski,36 2016 | Case series | 22 | 16/6 | 12 (10.5 to 13.2) | Transphyseal | 77.2 | Yes |
| Dei Giudici,37 2016 | Case series | 19 | 14/5 | 13.9 (12 to 16) | Transphyseal | 60 | Yes |
Methodological assessment and risk of bias
The methodological quality of the studies included had a mean Coleman methodology score of 40.5 (24 to 57). There was significant weakness across all the studies with various forms of bias present. A total of 16 out of 18 studies included were case series, often with small sample sizes (8/18 contained < 20 subjects), without controls and without randomization. Two studies2,3 used prospective or retrospective cohort study methods comparing conservative and transphyseal reconstruction techniques. No prospective randomized control trials were found. Surgical treatments were frequently well described but postoperative rehabilitation or non-surgical treatments were not specified in the literature. Reasons for attrition from the included studies were not reported in those studies where less than 100% follow-up was achieved.2,3,8,26 Outcome measures used were reliable and valid in all studies, but collection of these data was not independent of surgeon or therapeutic team.
Results
Conservative management
Two studies reported the results of non-operative treatment and the natural history of ACL injuries,2,3, summarized in Table 2. Data were provided for 35 patients: mean age 11.9 years, mean follow-up 70 to 72 months. One study2 presented a group of skeletally immature subjects with ACL tears and other associated injuries (meniscal tears and collateral ligament injuries), the other study3 excluded all subjects with other associated injuries. Both groups were treated with bracing, reduction in activities and physiotherapy but the exact rehabilitation protocols were not explicit. Both studies show reported Lysholm (mean 63.2) and Tegner scores (mean 4.8) and one study3 reported IKDC (mean 87). The Lysholm and Tegner scores were higher in the group without associated injuries,3 compared with those with associated injuries.2 High rates of persistent instability requiring surgical stabilization, associated meniscal injuries and early radiological signs of joint degeneration were also seen.
Table 2.
Summary of outcomes for non-operative treatment
| Author | n | Age at operation, yrs (range) | Treatment | Mean outcome score (range/sd) | Mean LLD/coronal plane malalignment (range) | Complications |
| Aichroth et al,2 2002 | 23 | 12.5 (11 to 15) | Nonoperative Group | Lysholm: 52.4 (30-83) Tegner: 4.2 (2-6) |
None reported | 10 patients with degenerative joint on x-ray (10 Fairbank sign, 3 narrowing, 4 osteophytes), 4 arthroscopic meniscal surgeries |
| Streich et al,3 2010 | 12 | 11 (9 to 12) | Nonoperative Group | Lysholm: 84 Tegner: 6 (5-7) IKDC: 87 (sd +/-0.8) |
No LLD No malalignment |
7 surgical reconstructions by 21 months |
Repair
One article7 presented the results of ACL repair in eight subjects, mean age 15 years (13 to 16) using a suture repair technique with a mean follow-up of 65 months (Table 3). Lysholm scores were reported as fair in five subjects (65 to 83), and good in three subjects (84 to 93). There was a high incidence (60%) of radiological joint degeneration (osteophytes and subchondral sclerosis).
Table 3.
Summary of outcomes for anterior cruciate ligament repair
| Author | n | Age at operation, yrs (range) | Treatment | Mean outcome score (range/sd) | Mean LLD/coronal plane malalignment (range) | Complications |
| Engebretsen et al,7 1988 | 8 | 15 (13 to16) | REPAIR: (Marshall and Rubin technique) | Lysholm: 5 Fair (65 to 83), 3 Good (84 to 94) Tegner: 4.8 (3 to 7) |
No clinical LLD No malalignment |
5 early osteoarthritis (osteophytes, subchondral sclerosis) |
Extraphyseal reconstruction
Four articles8-10,26 presented the results of extraphyseal reconstruction techniques in 126 subjects, mean age 11.3 years, summarized in Table 4. No clinically significant LLD or malalignment was seen. Five graft ruptures (4%) were observed, four of these required revision surgeries. The mean Lysholm score was 96.2 (sd 5.9, 95.7 to 97.4), the mean IKDC score was 95.4, with the majority achieving A grade (normal) or > 95%. Tegner activity scores also returned to pre-injury levels (mean 6.75).10 Two studies8,26 reported return to the same level sport as pre-injury in all subjects, whereas another article reported up to 60% return to sport at a lower level or not at all.10
Table 4.
Summary of outcomes for extraphyseal reconstruction
| Author | n | Age at operation, yrs (range) | Treatment, TRANS/EXTRA physeal (fixation) | Mean outcome score (range/sd) | Mean LLD/coronal plane malalignment (range) | Complications |
| Micheli et al,8 1999 | 17 | 11 (2 to 14) | EXTRA: tibia (native), femur (suture) (Macintosh technique) | Lysholm: 97.4 (2.95) | No clinical LLD No malalignment |
None reported |
| Guzzanti et al,26 2003 | 8 | 11.15 (10 to 12) | EXTRA: tibia (native), femur (staple) | OAK: 97 (96 to 98) | LLD: femur 0 mm (-0.2 to +0.1), tibia 0 mm (-2 to +2) No malalignment |
None reported |
| Kocher et al,9 2006 | 44 | 10.3 | EXTRA: tibia (native), femur (suture) (Macintosh technique) | Lysholm: 95.7 (6.7) IKDC: 96.7 (6) |
No clinical LLD No malalignment |
2 graft ruptures (revised) |
| Bonnard et al,10 2011 | 57 | 12.2 (6.8 to 14.5) | EXTRA: tibia (sutures), femur (interference) (Clocheville technique) | IKDC: 94.4 (64 to 100) Tegner: 6.75 (4 to 9) |
LLD: -0.4 mm (-5 to +15) 0.7° (-4° to +4°) | 3 graft ruptures (2 revised, 1 non-operative management) |
IKDC, International Knee Documentation committee; LLD, Leg Length Discrepancy; OAK, Orthopädische Arbeitsgruppe Knie score
Transphyseal reconstruction
In all, 11 articles3,12,13,30-37 presented the results of transphyseal reconstruction techniques in 256 subjects, mean age 12.9 years. One article11 presented the results of a hybrid technique. These studies are summarized in Table 5. Two cases were observed in which the operated limb demonstrated an overgrowth resulting in a +15 mm LLD; one was symptomatic requiring a shoe raise,31 and the other was asymptomatic.37 One study reported a case of asymptomatic valgus deformity (7.1° compared with 0.9° on the contralateral side) that required no treatment.12 A total of 11 graft ruptures (5%) requiring revision surgery or withdrawal from sporting activity were observed.12,13,31,33,35 Individualized outcomes scores for patients with these complications were not presented. Five cases (2%) of persistent instability were observed,13,33,37 of which three underwent revision surgery and two failed to return to sports. In one study IKDC scores were low (score = D)13 for those patients requiring revision surgery. The mean Lysholm score was 94.3 (84.6 to 100), mean IKDC score 93.6 (84 to 99) and mean Tegner score 7.6 (6 to 8.7), which was comparable with pre-injury levels.
Table 5.
Summary of outcomes for transphyseal reconstruction
| Author | n | Age at operation, yrs (range) | Treatment, TRANS/EXTRA physeal (fixation) | Mean outcome score (range/sd) | Mean LLD/coronal plane malalignment (range) | Complications |
| Lo et al,11 1997 | 5 | 12.9 (8 to 14) | HYBRID: tibia transphyseal vertical (native), femur extra physeal (staple) | IKDC: 4A, 1C | LLD: -0.8 mm (-5 to +4) 1° (-2° to +3°) |
1 osteochondral fracture (low IKDC) |
| Seon et al,30 2005 | 11 | 14.7 (13.1 to 15.5) | TRANS: tibia (interference screw), femur (screw/staple) | Lysholm 97.8 | LLD: +3.9 mm (-10 to 10) 0.1° (-1° to +1°) |
None reported |
| Mcintosh et al,31 2006 | 16 | 13.8 (11.2 to 14.9) | TRANS: tibia (screw), femur (suspensory) | Lysholm: 90 (74 to 94) Tegner: 8.1 (7 to 9) IKDC: 99 (94 to 100) |
LLD: 6.2 mm (2 to 15). 1 case: +15 mm LLD (shoe raise) No malalignment |
2 graft ruptures (1 revision) 3 failed meniscal repair |
| Courvoisier et al,13 2010 | 37 | 14 (11 to 15) | TRANS: tibia (interference screw), femur (suspensory) | IKDC: 28 A, 4 B, 5 D | No LLD (not quantified) 1° (sd 1.5°) |
3 graft ruptures (revised) 2 revisions for instability |
| Kopf et al,32 2010 | 14 | 14.4 (11 to 16) | TRANS: tibia (staples), femur (suspensory) | Lysholm: 96 (IQ 93 to 100) IKDC: 95 (92 to 98) 8A 5B 1C |
No clinical LLD No malalignment |
None reported |
| Streich et al,3 2010 | 16 | 11 (9 to 12) | TRANS: tibia (staple), femur (suspensory) | Lysholm: 93 Tegner: 7 (6 to 8), IKDC: 95 |
LLD: +1.7 mm (sd 6.6) No malalignment |
None Reported |
| Kumar et al,12 2013 | 32 | 11.25 (9.5 to 14) | TRANS: tibia (screw), femur (suspensory) | Lysholm: 95.86 Tegner: 7.66 |
1 case: 7.1° valgus with LLD -1.6 mm | 1 graft rupture |
| Calvo et al,33 2014 | 27 | 13 (12 to 16) | TRANS (vertical tunnels): tibia (interference/staples tanner 2/3), femur (button, suspensory) | Lysholm: 94 (55 to 100) Tegner: 6 (3 to 9) IKDC 92 (44 to 100) |
LLD: +1.6 mm (-4 to 8) 3.6° valgus (3.4° to 4.3°) (4.05° control leg) | 4 revisions (3 graft ruptures, 1 instability) 2 osteochondral fractures 1 meniscal tear |
| Falciglia et al,35 2016 | 33 | 12.4 (10 to 14.2) | TRANS: tibia (native), femur (staple) | IKDC 10 year: 88.2 (8.4 to 97.7) Skeletal maturity: 91.8 (68.9 to 97.7) |
LLD: femur -1 mm (-5 to +3), tibia +0.2 mm (-0.6 to +0.6) No malalignment |
2 graft ruptures (not re-operated) 1 Kellgren and Lawrence grade 2 |
| Domzalski et al,36 2016 | 22 | 12 (10.5 to 13.2) | TRANS: tibia (screw), femur (screw) | Lysholm 95.9 (94 to 100) Tegner 7 IKDC 14 A, 7 B, 1 C |
LLD: +2 mm (0 to +8), 5 > 5 mm No malalignment |
None reported |
| Dei Giudici et al,37 2016 | 19 | 13.9 (12 to 16) | TRANS: tibia (interference screw), femur (unclear) | Lysholm: 84.6 (40 to 100) Tegner: 8.2 (7 to 10) IKDC: 84 (29.9 to 100) |
1 case: +15 mm LLD | 2 persistent instability (both failed to return to sports) |
| Placella et al,34 2016 | 24 | 13.15 (9 to 14) | TRANS: tibia (interference screw), femur (suspensory) | Lysholm: 100 Tegner: 8.7 IKDC: 98.58 (95.4 to 100) |
LLD: + 4 mm (2 to 7) No malalignment |
10 contralateral ACL, 5 meniscal tears (repaired) |
IKDC, International Knee Documentation committee; LLD, Leg Length Discrepancy
Age and skeletal maturity
The mean age at the time of surgery 12.3 years (10.3 to 15) old. The presence of open physis was confirmed in all studies. Tanner staging was used in 12 articles. Five articles described predicted growth remaining. Those articles in which predicted growth was > 5 cm or the subjects were in Tanner stages 1 to 3 were analyzed as a group with significant growth remaining at the time of surgery. Table 6 summarizes these groups.
Table 6.
Summary of subject age, skeletal immaturity and growth remaining
| Author | n | Age at operation, yrs (range) | Bone age | Physis | Tanner | Growth remaining | Skeletal maturity at follow-up | Treatment |
| Group 1: Significant growth potential | ||||||||
| Lo et al,11 1997 | 5 | 12.9 (8 to 14) | Wide open | >5cm | No | Hybrid | ||
| Guzzanti et al,26 2003 | 8 | 11.15 (10 to 12) | Open | 1 | >7cm | Yes | Extraphyseal | |
| Seon et al,30 2005 | 11 | 14.7 (13.1 to 15.5) | Open | 1 to 2 | Pre-growth spurt | Yes | Transphyseal | |
| Kocher et al,9 2006 | 44 | 10.3 | Open | 1 to 2 | No | Extraphyseal | ||
| Kopf et al,32 2010 | 14 | 14.4 (11 to 16) | Open | 2 to 3 | 8cm growth seen | No | Transphyseal | |
| Streich et al,3 2010 | 31 | 11 (9 to 12) | Wide open | 1 to 2 | No | Transphyseal | ||
| Bonnard et al,10 2011 | 57 | 12.2 (6.8 to 14.5) | 11.5 (7 to 15) | Open | >5cm Female, >9cm males | Yes | Extraphyseal | |
| Kumar et al,12 2013 | 32 | 11.25 (9.5 to 14) | Open | 1 to 2 (or 3 if < 12) | No 78% | Transphyseal | ||
| Falciglia et al,35 2016 | 33 | 12.4 (10 to 14.2) | Open | 2 to 3 | >5cm | Yes | Transphyseal | |
| Domzalski et al,36 2016 | 22 | 12 (10.5 to 13.2) | Open | 1 to 2 | Yes | Transphyseal | ||
| Dei Giudici et al,37 2016 | 19 | 13.9 (12 to 16) | Open | 2 to 3 | Yes | Transphyseal | ||
| Growth potential mixed or unclear | ||||||||
| Engebretsen et al,7 1988 | 8 | 15 (13 to16) | Open | No | Extraphyseal repair | |||
| Micheli et al,8 1999 | 17 | 11 (2 to 14) | 10 (2 to 13) | Open | Yes | Extraphyseal | ||
| Mcintosh et al,31 2006 | 16 | 13.8 (11.2 to 14.9) | Wide open | Yes | Transphyseal | |||
| Courvoisier et al,13 2010 | 37 | 14 (11 to 15) | Wide open | Yes | Transphyseal | |||
| Calvo et al,33 2014 | 27 | 13 (12 to 16) | Open >2mm | 1 to 4 | No | Transphyseal | ||
| Placella et al,34 2016 | 24 | 13.15 (9 to 14) | Open | 1 to 4 | No | Transphyseal | ||
In all, 11 articles, containing 261 subjects with a mean age of 12.0 (10.3 to 14.7) were reviewed in the group with significant growth remaining, summarized in Table 7. Seven studies used transphyseal reconstruction, one study used hybrid reconstruction and three used extraphyseal techniques. In this group one clinically significant asymptomatic LLD37 and one asymptomatic valgus deformity12 were observed, both cases were described earlier. Eight (3%) graft ruptures were observed,9,10,12,35 requiring revision surgery in five cases and withdrawal from sport in the others. Two (0.7%) persistent instabilities were observed; both were not surgically reconstructed and were unable to return to sport at pre-injury levels. The mean Lysholm score was 94.3 (84.6 to 97.8), mean Tegner score 7.2 (6.75 to 8.2), mean IKDC score 93.7 (88 to 96) and one study reported outcome data using the Orthopädische Arbeitsgruppe Knie score.38
Table 7.
Summary of Group 1 (significant growth remaining)
| Author | n | Age at operation, yrs (range) | Treatment, TRANS/EXTRA physeal (fixation) | Mean outcome score (range/sd) | Mean LLD/coronal plane malalignment (range) | Complications |
| Lo et al,11 1997 | 5 | 12.9 (8 to 14) | MIXED: tibia transphyseal vertical (native), femur extra physeal (staple) | IKDC: 4A, 1C | LLD: -0.8 mm (-5 to +4) 1° (-2° to +3°) | Osteochondral fracture (low IKDC) |
| Guzzanti et al,27 2003 | 8 | 11.15 (10 to 12) | EXTRA: tibia (native), femur (staple) | OAK: 97 (96 to 98) | LLD: femur 0 mm (-0.2 to +0.1), tibia 0 mm (-2 to +2) No malalignment |
None reported |
| Seon et al,30 2005 | 11 | 14.7 (13.1 to 15.5) | TRANS: tibia (interference screw), femur (screw/staple) | Lysholm 97.8 | LLD: +3.9 mm (-10 to 10) 0.1° (-1° to +1°) | None reported |
| Kocher et al,9 2006 | 44 | 10.3 | EXTRA: tibia (native), femur (suture) (Macintosh) | Lysholm: 95.7 (sd 6.7) IKDC: 96.7 (sd 6) |
No clinical LLD No malalignment |
2 graft ruptures (revised) |
| Kopf et al,32 2010 | 14 | 14.4 (11 to 16) | TRANS: tibia (staples), femur (suspensory) | Lysholm: 96 (IQ 93 to 100) IKDC: 95 (92 to 98) 8A 5B 1C |
No clinical LLD No malalignment |
None reported |
| Streich et al,3 2010 | 16 | 11 (9 to 12) | TRANS: tibia (staple), femur (suspensory). | Lysholm: 93 Tegner: 7 (6 to 8), IKDC: 95 |
LLD: 1.7 mm (sd 6.6) No malalignment |
None reported |
| Bonnard et al,10 2011 | 57 | 12.2 (6.8 to 14.5) | EXTRA: tibia (sutures), femur (interference) (Clocheville technique) | IKDC: 39A, 14B, 2C, 1D Tegner: 6.75 (4 to 9) LLD: -0.4 mm (-5 to +15) 0.7° (-4° to +4°) |
3 graft ruptures (revised) | |
| Kumar et al,12 2013 | 32 | 11.25 (9.5 to 14) | TRANS: tibia (screw), femur (suspensory) | Lysholm: 95.86 Tegner: 7.66 |
1 case: 7.1° valgus with LLD -1.6 mm | 1 graft rupture (not re-operated) |
| Falciglia et al,35 2016 | 33 | 12.4 (10 to 14.2) | TRANS: tibia (native), femur (staple) | IKDC 10 year: 88.2 (8.4 to 97.7) Skeletal maturity: 91.8 (68.9 to 97.7) |
LLD: femur -1 mm (-5 to +3), tibia +0.2 mm (-0.6 to +0.6) No malalignment |
2 graft ruptures (not re-operated) 1 Kellgren and Lawrence grade 2 |
| Domzalski et al,36 2016 | 22 | 12 (10.5 to 13.2) | TRANS: tibia (screw), femur (screw) | Lysholm: 95.9 (94 to 100) Tegner: 7 IKDC: 14 A, 7 B, 1 C |
LLD: +2 mm (0 to +8), 5 > 5 mm No malalignment |
None reported |
| Dei Giudici et al,37 2016 | 19 | 13.9 (12 to 16) | TRANS: tibia (interference screw), femur (unclear) | Lysholm: 84.6 (40 to 100) Tegner: 8.2 (7 to 10) IKDC: 84 (29.9 to 100) |
1 case: 15 mm LLD | 2 persistent instability (both failed to return to sports) |
IKDC, International Knee Documentation committee; LLD, Leg Length Discrepancy; OAK, Orthopädische Arbeitsgruppe Knie score
Associated injuries
All except two studies26,32 reported associated injuries at the time of surgery. High rates of meniscal and other associated ligament injuries were found in up to 75% of included subjects (27% to 75%). In all studies, treatment of these associated injuries was undertaken at the time of ACL surgery using meniscectomy or meniscal repair techniques. However, no study described outcomes in relation to the presence or absence of associated injuries at the time of initial surgery.
Discussion
The literature presented in this systematic review suggests that early surgical reconstruction offers more favourable long-term patient reported outcomes over conservative management in the treatment of ACL injuries in the skeletally immature. The conservative treatments reviewed2,3 result in higher rates of persistent instability and secondary injury resulting in the need for late reconstructive surgery. Mean Lysholm (63.2) and Tegner (4.8) scores after conservative treatment were seen to be lower than the mean Lysholm (94.7) and Tegner (7.5) observed in the reconstructed groups. However, the two non-surgical studies reviewed both used treatments which included periods of immobilization, reduced weight-bearing and unspecified rehabilitation techniques. These do not accurately reflect more modern rehabilitation techniques in use today. There is some evidence in the young adult population that early surgical reconstruction does not offer significant improvements in patient reported outcomes over non-surgical treatment or delayed surgical treatment.39,40 Additionally, there is some supporting evidence that non-surgical treatments in young skeletally immature subjects may produce adequate outcomes comparable with surgical reconstruction.41 The literature presented in this review would also suggest that repair of the torn ACL offers poor long-term patient reported outcomes and high rates of radiological joint degeneration.7 However, significant advancements have occurred recently regarding ACL repair. These have provided an improved understanding of ACL biology and along with significant advancements in tissue engineering and biosynthetics, these have led to the introduction of biologically augmented ACL repair techniques.11,42-46 It has been suggested that these promising new repair techniques could offer a viable option for skeletally immature patients but will require long-term evaluation.42 It is therefore important not to dismiss non-surgical treatments or ligament repair techniques based on the outdated techniques presented and further review of repair techniques should be undertaken in the light of recent and future studies in these areas.
Those groups deemed to have significant growth potential remaining were also analyzed together. The results for this sub-group were in keeping with the overall results; in general, showing good long-term patient reported outcomes using Lysholm (mean 94.3), Tegner (mean 7.2) and IKDC (mean 93.7). Adverse events including LLD, malalignment, graft rupture (3%) and persistent instability (0.7%) were not concentrated within this group. As there was no agreed consensus within the literature defining skeletal immaturity, the definition of this group involved the use of several surrogate measures of skeletal maturity and growth remaining. Although an attempt was made to differentiate the subjects used in this group from the overall population, the results are in keeping with the cohort as a whole. This may suggest the overall population under review was homogenous and that a group at higher risk was not defined adequately.
Concerns regarding injury to the physis and resultant growth disturbance in the skeletally immature patient have led to the innovation of physeal sparing surgical techniques. These techniques theoretically minimize the risk of physeal injury and resultant growth disturbance.26 This review found outcome scores between extraphyseal and transphyseal groups to be comparable. Mean Lysholm score was 96.2 (95.7 to 97.4) in the extraphyseal group and 94.3 (84.6 to 100) in the transphyseal group, mean Tegner score was 6.75 and 7.5 (6 to 8.7), respectively and mean IKDC score was 95.4 (94 to 100) and 93.6 (84 to 99). Very few studies provided variance data for these results, limiting the ability to draw conclusions from statistical analysis. However, it should be acknowledged that the lower boundaries for the range of Lysholm and IKDC scores are lower for the transphyseal group.
This review found no reported cases of LLD in the extraphyseal reconstruction group compared with two cases in the transphyseal group, however, no significant difference was demonstrated (p = 0.32). Similarly, only one case of coronal plane growth disturbance was identified in the transphyseal reconstruction group (p = 0.48). It is not possible to interpret the effect of these complications on long-term patient reported outcomes, as they were not individually reported in the studies. It would appear that extraphyseal techniques negate the risk of LLD or malalignment, however, this is only a small risk in the transphyseal technique and the small subject numbers and relative rarity of these events means drawing absolute conclusions is not possible. A recent systematic review47 on the subject of growth abnormalities after ACL reconstruction found that LLDs occur with similar frequency in both physeal sparing and transphyseal techniques. Interestingly, the LLDs observed in this review all found the operated leg to be long. One possible explanation for this is akin to that seen with diaphyseal fractures in the growing skeleton, where injury to the periosteum leads to increased vascularity and overgrowth within the physis and subsequent overgrowth.48
The transphyseal technique more closely replicates adult reconstruction techniques. These techniques aim to achieve a more anatomical graft position and, therefore, greater stability, particularly when compared with ‘over the top’ extraphyseal techniques, which may not be able to achieve such a graft placement. In this review no cases of persistent symptomatic instability were seen in the extraphyseal group, compared with five (2%) in the transphyseal group, three of which went on to require revision surgery. However, no significant difference between the groups was demonstrated (p = 0.11). No significant difference in the frequency of graft rupture (p = 0.88) was observed, with five cases observed (4%) in the extraphyseal group compared with 11 (5%) in the transphyseal group. Several reviews have examined the causative factors leading to persistent instability and revision ACL surgery. Non-anatomic graft placement has been found to be a significant cause for revision and graft failure in most reported series.49,50 Changes in tunnel length and position were noted in one series,12 but instability and graft failures were not attributed to these changes. Additionally, this does not fully explain the differences seen between the transphyseal and extraphyseal groups, in which changes in graft position due to growth over time would be seen in both groups. Direct comparison of long-term patient reported outcomes and complications using randomization of these two techniques may provide a greater understanding of their relative efficacy and safety.
The ability to draw definite conclusions and generalize findings from this review is limited by several factors. The literature reviewed consists of small retrospective case series prone to methodological biases. Many of the trials reviewed were case series used to present novel surgical techniques. The trend towards only positive reported outcomes raises the question of publication bias across the subject area, but this is difficult to quantify. Outcome measures were reported as group average results, often without a description of variance within the outcome result reported, thus limiting the ability to undertake statistical comparisons between groups. Additionally, individual results allowing the analysis of the effects of growth deformities or complications in individual subjects was not possible. To address these issues the use of registry data may improve understanding of the long-term outcomes for the treatment of this group of patients. Finally, the definition of skeletal immaturity was not precise. Several surrogate measures of skeletal maturity and growth remaining have been used, but these failed to identify a group distinct from the overall population.
The results of this systematic review have found the long-term patient reported outcomes of ACL reconstructive surgery in the skeletally immature to be good. They compare favourably with the natural history of the condition, but the results of modern non-surgical treatments and biological augmented ligament repair techniques need to be further evaluated. Both transphyseal and extraphyseal reconstructive techniques produced good outcomes, with no significant differences in the incidence of limb length discrepancy (p = 0.32), coronal plane growth disturbance (p = 0.48), graft rupture (p = 0.88) and persistent symptomatic instability (p = 0.11). Further high-quality studies comparing the transphyseal and extraphyseal techniques are required to determine their relative efficacy and safety, and the effects of these on patient reported outcomes.
COMPLIANCE WITH ETHICAL STANDARDS
FUNDING STATEMENT
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA LICENCE TEXT
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
ETHICAL STATEMENT
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
REFERENCES
- 1.Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M.. ACL Tears in school-aged children and adolescents over 20 years. Pediatrics 2017;139:e20161877. [DOI] [PubMed] [Google Scholar]
- 2.Aichroth PM, Patel DV, Zorrilla P.. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg [Br] 2002;84-B:38-41. [DOI] [PubMed] [Google Scholar]
- 3.Streich NA, Barié A, Gotterbarm T, Keil M, Schmitt H.. Transphyseal reconstruction of the anterior cruciate ligament in prepubescent athletes. Knee Surg Sports Traumatol Arthrosc 2010;18:1481-1486. [DOI] [PubMed] [Google Scholar]
- 4.Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ.. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med 2014;42:2769-2776. [DOI] [PubMed] [Google Scholar]
- 5.Werner BC, Yang S, Looney AM, Gwathmey FW Jr.. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 6.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ.. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop 2002;22:452-457. [PubMed] [Google Scholar]
- 7.Engebretsen L, Svenningsen S, Benum P.. Poor results of anterior cruciate ligament repair in adolescence. Acta Orthop Scand 1988;59:684-686. [DOI] [PubMed] [Google Scholar]
- 8.Micheli LJ, Rask B, Gerberg L.. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clin Orthop Relat Res 1999;364:40-47. [DOI] [PubMed] [Google Scholar]
- 9.Kocher MS, Garg S, Micheli LJ.. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg [Am] 2006;88-A:283-293. [DOI] [PubMed] [Google Scholar]
- 10.Bonnard C, Fournier J, Babusiaux D, et al. . Physeal-sparing reconstruction of anterior cruciate ligament tears in children: results of 57 cases using patellar tendon. J Bone Joint Surg [Br] 2011;93-A:542-547. [DOI] [PubMed] [Google Scholar]
- 11.Lo IK, Kirkley A, Fowler PJ, Miniaci A.. The outcome of operatively treated anterior cruciate ligament disruptions in the skeletally immature child. Arthroscopy 1997;13:627-634. [DOI] [PubMed] [Google Scholar]
- 12.Kumar S, Ahearne D, Hunt DM.. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: follow-up to a minimum of sixteen years of age. J Bone Joint Surg [Am] 2013;95:e1. [DOI] [PubMed] [Google Scholar]
- 13.Courvoisier A, Grimaldi M, Plaweski S.. Good surgical outcome of transphyseal ACL reconstruction in skeletally immature patients using four-strand hamstring graft. Knee Surg Sports Traumatol Arthrosc 2011;19:588-591. [DOI] [PubMed] [Google Scholar]
- 14.Vavken P, Murray MM.. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy 2011;27:704-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis JC, Bryan S.. Patient Reported Outcome Measures (PROMs) have arrived in sports and exercise medicine: why do they matter? Br J Sports Med 2015;49:1545-1546. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Tetzlaff J, Tricco AC, Sampson M, Altman DG.. Epidemiology and reporting characteristics of systematic reviews. PLoS Med 2007;4:e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greulich WW, Pyle SI.. Radiographic atlas of skeletal development of the hand and wrist. Redwood, PA: Stanford University Press, 1959. [Google Scholar]
- 18.Marshall WA, Tanner JM.. Variations in the pattern of pubertal changes in boys. Arch Dis Child 1970;45:13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green W, Anderson M.. Experiences with epiphyseal arrest in correcting discrepancies in length of the lower extremities in infantile paralysis: a method of predicting the effect. J Bone Joint Surg [Am] 1947;29-A:659-675. [PubMed] [Google Scholar]
- 20.Tegner Y, Lysholm J.. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985;198:43-49. [PubMed] [Google Scholar]
- 21.Briggs KK, Lysholm J, Tegner Y, et al. . The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 2009;37:890-897. [DOI] [PubMed] [Google Scholar]
- 22.Oak SR, O’Rourke C, Strnad G, et al. . Statistical comparison of the pediatric versus adult IKDC subjective knee evaluation form in adolescents. Am J Sports Med 2015;43:2216-2221. [DOI] [PubMed] [Google Scholar]
- 23.Bekkers JEJ, de Windt TS, Raijmakers NJH, Dhert WJ, Saris DB.. Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthritis Cartilage 2009;17:1434-1439. [DOI] [PubMed] [Google Scholar]
- 24.Pennock A, Murphy MM, Wu M.. Anterior cruciate ligament reconstruction in skeletally immature patients. Curr Rev Musculoskelet Med 2016;9:445-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCarthy MM, Graziano J, Green DW, Cordasco FA.. All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech 2012;1:e231-e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guzzanti V, Falciglia F, Stanitski CL.. Physeal-sparing intraarticular anterior cruciate ligament reconstruction in preadolescents. Am J Sports Med 2003;31:949-953. [DOI] [PubMed] [Google Scholar]
- 27.Moksnes H, Engebretsen L, Risberg MA.. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg [Am] 2012;94-A:1112-1119. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J, Green S.. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 2011. http://handbook-5-1.cochrane.org (date last accessed 24 June 2017).
- 29.Khamis S, Carmeli E.. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017;57:115-123. [DOI] [PubMed] [Google Scholar]
- 30.Seon JK, Song EK, Yoon TR, Park SJ.. Transphyseal reconstruction of the anterior cruciate ligament using hamstring autograft in skeletally immature adolescents. J Korean Med Sci 2005;20:1034-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McIntosh AL, Dahm DL, Stuart MJ.. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy 2006;22:1325-1330. [DOI] [PubMed] [Google Scholar]
- 32.Kopf S, Schenkengel JP, Wieners G, Stärke C, Becker R.. No bone tunnel enlargement in patients with open growth plates after transphyseal ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18:1445-1451. [DOI] [PubMed] [Google Scholar]
- 33.Calvo R, Figueroa D, Gili F, et al. . Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med 2015;43:289-294. [DOI] [PubMed] [Google Scholar]
- 34.Placella G, Bartoli M, Peruzzi M, et al. . Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years follow-up. Acta Orthop Traumatol Turc 2016;50:635-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falciglia F, Panni AS, Giordano M, Aulisa AG, Guzzanti V.. Anterior cruciate ligament reconstruction in adolescents (Tanner stages 2 and 3). Knee Surg Sports Traumatol Arthrosc 2016;24:807-814. [DOI] [PubMed] [Google Scholar]
- 36.Domzalski M, Karauda A, Grzegorzewski A, et al. . Anterior cruciate ligament reconstruction using the transphyseal technique in prepubescent athletes: midterm, prospective evaluation of results. Arthroscopy 2016;32:1141-1146. [DOI] [PubMed] [Google Scholar]
- 37.Dei Giudici L, Fabbrini R, Garro L, et al. . Arthroscopic transphyseal anterior cruciate ligament reconstruction in adolescent athletes. J Orthop Surg (Hong Kong) 2016;24:307-311. [DOI] [PubMed] [Google Scholar]
- 38.Müller W, Biedert R, Hefti F, et al. . OAK knee evaluation. A new way to assess knee ligament injuries. Clin Orthop Relat Res 1988;232:37-50. [PubMed] [Google Scholar]
- 39.Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM.. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med 2015;49:1033-1041. [DOI] [PubMed] [Google Scholar]
- 40.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS.. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010;363:331-342. [DOI] [PubMed] [Google Scholar]
- 41.Moksnes H, Engebretsen L, Eitzen I, Risberg MA.. Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med 2013;47:488-494. [DOI] [PubMed] [Google Scholar]
- 42.Waryasz GR, Marcaccio S, Gil JA, Owens BD, Fadale PD.. Anterior cruciate ligament repair and biologic innovations. JBJS Rev 2017;5:e2. [DOI] [PubMed] [Google Scholar]
- 43.Murray MM, Fleming BC.. Biology of anterior cruciate ligament injury and repair: kappa delta ann doner vaughn award paper 2013. J Orthop Res 2013;31:1501-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murray MM, Flutie BM, Kalish LA, et al. . The Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med 2016;4:2325967116672176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kiapour AM, Murray MM.. Basic science of anterior cruciate ligament injury and repair. Bone Joint Res 2014;3:20-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hohmann E. Editorial commentary: renaissance of primary anterior cruciate ligament repair: is history repeating itself? Arthroscopy 2016;32:2570-2571. [DOI] [PubMed] [Google Scholar]
- 47.Collins MJ, Arns TA, Leroux T, et al. . Growth abnormalities following anterior cruciate ligament reconstruction in the skeletally immature patient: a systematic review. Arthroscopy 2016;32:1714-1723. [DOI] [PubMed] [Google Scholar]
- 48.Chotel F, Henry J, Seil R, et al. . Growth disturbances without growth arrest after ACL reconstruction in children. Knee Surg Sports Traumatol Arthrosc 2010;18:1496-1500. [DOI] [PubMed] [Google Scholar]
- 49.Brown CH Jr, Carson EW.. Revision anterior cruciate ligament surgery. Clin Sports Med 1999;18:109-171. [DOI] [PubMed] [Google Scholar]
- 50.Wylie JD, Marchand LS, Burks RT.. Etiologic factors that lead to failure after primary anterior cruciate ligament surgery. Clin Sports Med 2017;36:155-172. [DOI] [PubMed] [Google Scholar]


