Abstract
Objective:
Adult cannabis use has increased in the United States since 2002, particularly after 2007, contrasting with stable/declining trends among youth. We investigated whether specific age groups disproportionately contributed to changes in daily and nondaily cannabis use trends.
Method:
Participants ages 12 and older (N = 722,653) from the 2002–2014 National Survey on Drug Use and Health reported past-year cannabis use frequency (i.e., daily = ≥300 days/year; nondaily = 1–299 days/year; none). Multinomial logistic regression was used to model change in past-year daily and nondaily cannabis use prevalence by age group (i.e., 12–17, 18–25, 26–34, 35–49, 50–64, ≥65), before and after 2007. Multinomial logistic regressions estimated change in relative odds of cannabis use frequency over time by age, adjusting for other sociodemographics.
Results:
Daily cannabis use prevalence decreased in ages 12–17 before 2007 and increased significantly across adult age categories only after 2007. Increases did not differ significantly across adult ages 18–64 and ranged between 1 and 2 percentage points. Nondaily cannabis use decreased among respondents ages 12–25 and 35–49 before 2007 and increased across adult age categories after 2007, particularly among adults 26–34 (i.e., 4.5 percentage points). Adjusted odds of daily versus nondaily cannabis use increased after 2007 for ages 12–64.
Conclusions:
Increases in daily and nondaily cannabis use prevalence after 2007 were specific to adult age groups in the context of increasingly permissive cannabis legislation, attitudes, and lower risk perception. Although any cannabis use may be decreasing among teens, relative odds of more frequent use among users increased in ages 12–64 since 2007. Studies should assess not only any cannabis use, but also frequency of use, to target prevention efforts of adverse effects of cannabis that are especially likely among frequent users.
In 2014, 35 MILLION PEOPLE ages 12 and older (13.2%) in the United States reported having used cannabis in the past year (Center for Behavioral Health Statistics and Quality [CBHSQ], 2015a), and 26.3% of adult users used cannabis 5 or more days per week (Compton et al., 2016). As of September 2017, 29 states and the District of Columbia had medical cannabis laws, and 8 states and the District of Columbia had recreational cannabis laws (National Conference of State Legislatures, 2017, 2018). These laws predict increased perceived access and cannabis use among adults (Chu et al., 2014; Hasin et al., 2017; Martins et al., 2016; Wen et al., 2015) but not adolescents (Anderson et al., 2015; Choo et al., 2014; Harper et al., 2012; Hasin et al., 2015; Johnson et al., 2017; Johnson et al., 2015; Keyes et al., 2016; Pacula et al., 2015; Smart, 2015; Wall et al., 2016). Prevalence of past-year cannabis use increased from 2001–2002 to 2012–2013 among adults (Hasin et al., 2015), particularly after 2007 (Carliner et al., 2017b; Compton et al., 2016), although adolescents’ prevalence changed little over the same period (CBHSQ, 2015c; Grucza et al., 2016a; Johnson et al., 2015). Studies have reported increases in cannabis use among all adults or broad age ranges of adults (e.g., 18–25, 26–49, ≥50; Compton et al., 2016; Grucza et al., 2016b; Pacek et al., 2015), but little is known about differential trends in cannabis use in more refined age categories. Studies with a life course approach that estimate associations within and across age strata are needed to understand age-specific trends in cannabis use frequency.
Cannabis use, particularly chronic or frequent use, is associated with a variety of adverse correlates and consequences (Hall & Degenhardt, 2014; Hasin, 2018; Volkow et al., 2014, 2016). These include cannabis or other substance use disorders (Blanco et al., 2016; Hall, 2009; Hall & Degenhardt, 2009; Hasin et al., 2015, 2016), cognitive impairments (Aharonovich et al., 2017; Auer et al., 2016; Meier et al., 2012), psychiatric symptoms (Davis et al., 2013; Di Forti et al., 2015), driving impairments, and motor vehicle crash injuries (Brady & Li, 2014; Hartman & Huestis, 2013; Hartman et al., 2015, 2016). Differentiating between frequent and infrequent use is clinically meaningful because some people can use cannabis without harm (Fergusson et al., 2015), whereas those who use cannabis frequently (Hall & Degenhardt, 2014) are reported to be more vulnerable to adverse consequences (Hall, 2015; Hall & Degenhardt, 2009; Volkow et al., 2014, 2016). Therefore, reported trends in use at the population level should differentiate between daily cannabis use and less frequent use across age groups.
Understanding age-specific trends is also important, as cannabis use may have different developmental correlates and consequences across the life course (Hall, 2015; Volkow et al., 2016). Various studies have focused on younger age groups because of concerns about the effects on neurophysiology and role acquisition during this developmental period (Carliner, 2017a; Cohn et al., 2015; DiNardo & Lemieux, 2001; Grucza et al., 2016a; Hayaki et al., 2016; Keyes et al., 2015; Redonnet et al., 2012; Sinclair et al., 2013). For youth, emerging adults, and young adults, frequent cannabis use may affect ongoing brain development (Gogtay et al., 2004; Volkow et al., 2014), educational attainment, and employment opportunities reaching into later adulthood (Lee et al., 2015; Zhang et al., 2016). Among all adults of reproductive age, cannabis use may affect issues related to family planning (Brown et al., 2017; Gundersen et al., 2015). For older adults, cannabis may be metabolized more slowly or could interact with medications taken for chronic health conditions (Blow, 1998; Dowling et al., 2008; Kuerbis et al., 2014; Wu & Blazer, 2011). Cannabis use could also increase adverse effects among people with chronic diseases, which are common in older adults, such as cardiovascular disease (Hall & Degenhardt, 2009). This is particularly concerning given that the aging baby boomer generation reports higher substance use than previous cohorts of middle-age and older adults (Kerr et al., 2007, 2018; Miech & Koester, 2012). Therefore, recent studies have called attention to cannabis and other substance use among middle-age and older adults (Han et al., 2017; Salas-Wright et al., 2017).
Comparing changes in cannabis use frequency across ages could inform population-based harm reduction or prevention interventions. Although past studies have identified 2007 as a change point in cannabis use trends across adults (Carliner et al., 2017b; Compton et al., 2016), age-specific changes in trends have not been explored. This information could help better identify the mechanisms that may lead to prevalence changes at the population level. In this study, we examined trends in daily and nondaily cannabis use prevalence in the past year among six age categories between 2002 and 2014, and compared change over time across these categories to identify ages that may have disproportionately increased use, particularly daily use of cannabis.
Method
Data source and sample
The National Survey on Drug Use and Health (NSDUH) is a cross-sectional nationally representative survey of noninstitutionalized individuals ages 12 and older in the United States (CBHSQ, 2015b; Substance Abuse and Mental Health Services Administration [SAMHSA], 2003). A multistage sampling design was used, oversampling young participants. Survey weights were created to produce national estimates of substance use and other health outcomes. Lay interviewers used computer-assisted personal interviews (CAPI) and audio computer-assisted self-interviewing (ACASI) to increase the privacy and confidentiality of sensitive information. Weighted interview response rates ranged from 78.56% in 2002 to 71.20% in 2014 (CBHSQ, 2015b; SAMHSA, 2003). The RTI International Institutional Review Board approved NSDUH procedures; additional information on data collection procedures and confidentiality are reported elsewhere (CBHSQ, 2014).
Data were obtained from participants ages 12 and older (N = 722,653) in the 2002–2014 publically available NSDUH, which included corrected sample weights that accounted for the combination of all 13 years of survey data.
Measures
Daily and nondaily cannabis use in the past year.
The NSDUH included detailed questions on cannabis use history and patterns. Participants reporting lifetime cannabis use were asked, “How long has it been since you last used marijuana or hashish?” Participants reporting cannabis use “within the past 30 days” or “more than 30 days ago but within the past 12 months” were coded as reporting past-year cannabis use, 0 otherwise. Participants then reported the number of days they used cannabis in the last 12 months. Consistent with prior epidemiologic studies (Carliner et al., 2017b; Pacek et al., 2015; SAMHSA, 2014), daily cannabis use was operationalized as 300–365 days of use in the past year (i.e., ≥25 days/month), and nondaily cannabis use was 1–299 days of use in the past year. A mutually exclusive three-level categorical variable differentiated no past-year cannabis use, past-year nondaily use, and past-year daily use.
Age and sociodemographic variables.
Age categories used for this study included 12–17, 18–25, 26–34, 35–49, 50–64, and 65 and older. Sociodemographic variables were selected based on their association with cannabis use (Compton et al., 2014; Copeland & Swift, 2009; Guxens et al., 2007; Kerr et al., 2007; Pacek et al., 2015); these were sex (female, male), race/ethnicity (Hispanic, non-Hispanic Black/African American, non-Hispanic other, non-Hispanic White), education (adults with less than high school, high school, at least some college), household income ($0–$19,999; $20,000–$49,999; $50,000–$74,999; ≥$75,000), and marital status (married, previously married, never married). See Supplemental Table A for distributions of sociodemographic characteristics by age, and Supplemental Table B for changes in adult marital status, household income, education, and employment (fulltime, part-time, unemployed, other) over time.
Statistical analysis
First, we assessed changes in time trends of any past-year cannabis use by age using piecewise logistic regressions (Toms & Lesperance, 2003). Although previous studies identified 2007 as a change point in adult cannabis use (Carliner et al., 2017b; Compton et al., 2016), we estimated whether this secular trend was observed across age categories by estimating log-odds of past-year use. As done previously (Carliner et al., 2017b), we fit age-specific models with a linear time term and then assessed each year as a potential “knot” in the trends (i.e., as change points between 2003 and 2013). Knots were specified as 0 up to the change point, and then as a 1-point linear increase each year after the change point. We systematically assessed whether each of the knot years was significantly associated with the outcome, beyond a linear time trend, for each age category. A statistically significant knot indicated a significant change in the linear time trends after that year. Pseudo R-squared values were used to compare model fit, with higher values indicating better fit (Freese & Long, 2006). Although multiple models had significant knots, the year 2007 emerged as a consistent change in trends for ages 12–17, 18–25, 26–34, and 35–49, with both significant knots and higher pseudo R-squared across the four age categories (see Supplemental Table C for all age-stratified models with coefficient and pseudo R-squared for the model with only a linear trend, and subsequent models with different knot years). There was no significant change point for ages 50–64 or 65 and older because none of the knots was significantly associated with cannabis use in these age groups. Despite this lack of change in trends in past-year use among older adults, we compared changes in trends in cannabis use frequency before and after 2007 for all age groups in subsequent analyses for consistency.
To calculate prevalence of daily and nondaily cannabis use by age over time, we fit a multinomial logistic regression model estimating the effects of age and year on cannabis use frequency, including an interaction term between age and time. Models adjusted for the complex survey design and used sample weights to account for oversampling of young participants and nonresponse to derive nationally representative estimates. Prevalences of each frequency of cannabis use by age group were estimated using model-based predicted marginal probabilities (Bieler et al., 2010; Williams, 2012) and were used to evaluate the changes over the time period by age (i.e., year difference, 2007–2002, 2014–2007, 2014–2002). To determine if changes over time differed significantly by age categories, additive interactions between year and age were examined, and interaction contrasts (IC) estimated (Rothman et al., 2008). The IC evaluates a “difference-in-differences,” or the difference in the prevalence differences over time for each age category relative to the reference age category. Wald t tests indicated the statistical significance of the prevalence differences and ICs. To correct for multiple testing in pairwise comparisons, corrected α levels of .05 / 15 =.0033 were used to declare significant ICs.
Then, a second multinomial logistic regression model estimated the change in adjusted relative odds over time by age comparing cannabis use frequency: nondaily versus no past-year use, daily versus no past-year use, and daily versus nondaily use (i.e., comparing frequency of use among cannabis users). We included two time interactions (i.e., Linear Year × Age; Knot × Age) to estimate age-specific time trends, and adjusted for sociodemographic covariates. Linear combinations were used to estimate age-specific change in the relative odds before and after 2007. We conducted sensitivity analyses among adults only, fitting multinomial logistic regressions to test whether controlling for employment status (i.e., part-time, full-time, unemployed, other) influenced the estimated associations between age and time. All analyses were conducted using Stata Version 14SE (StataCorp LP, College Station, TX).
Results
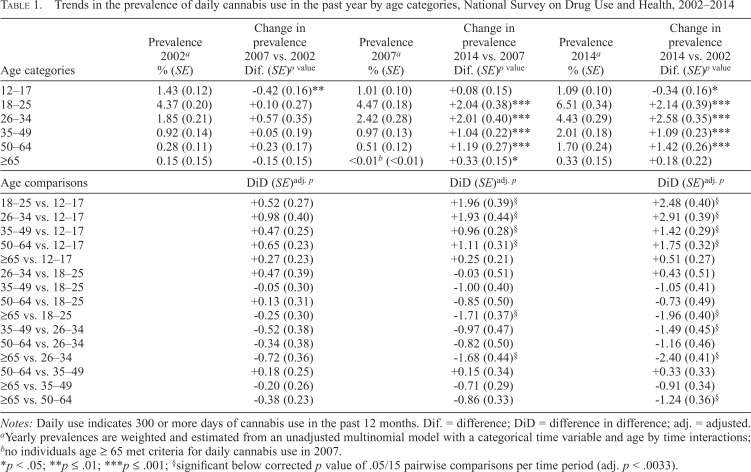
Daily cannabis use across age categories
Model-based prevalences of past-year daily cannabis use by age are shown in Table 1. Daily cannabis use was highest among 18–25 and 26–34-year-olds across all years (Supplemental Figure A). Daily cannabis use estimates in 2014 were significantly higher than in 2002 for age groups 18–64. Before 2007, daily cannabis use remained stable across adult age categories and decreased among adolescents from 1.43% to 1.01%. After 2007, daily cannabis use increased significantly across adult age categories, whereas adolescent daily use remained stable at about 1.09%. Although the absolute change between 2007 and 2014 was largest for ages 18–34, increases after 2007 were comparable across adult ages 18– 64 after multiple testing adjustment and were significantly higher than for adolescents.
Table 1.
Trends in the prevalence of daily cannabis use in the past year by age categories, National Survey on Drug Use and Health, 2002–2014
| Age categories | Prevalence 2002a (SE) | Change in prevalence 2007 vs. 2002 Dif. (SE)p value | Prevalence 2002a (SE) | Change in prevalence 2014 vs. 2007 Dif. (SE)p value | Prevalence 2002a (SE) | Change in prevalence 2014 vs. 2002 Dif. (SE)p value |
| 12–17 | 1.43 (0.12) | -0.42 (0.16)** | 1.01 (0.10) | +0.08 (0.15) | 1.09 (0.10) | -0.34 (0.16)* |
| 18–25 | 4.37 (0.20) | +0.10 (0.27) | 4.47 (0.18) | +2.04 (0.38)*** | 6.51 (0.34) | +2.14 (0.39)*** |
| 26–34 | 1.85 (0.21) | +0.57 (0.35) | 2.42 (0.28) | +2.01 (0.40)*** | 4.43 (0.29) | +2.58 (0.35)*** |
| 35–49 | 0.92 (0.14) | +0.05 (0.19) | 0.97 (0.13) | +1.04 (0.22)*** | 2.01 (0.18) | +1.09 (0.23)*** |
| 50–64 | 0.28 (0.11) | +0.23 (0.17) | 0.51 (0.12) | +1.19 (0.27)*** | 1.70 (0.24) | +1.42 (0.26)*** |
| ≥65 | 0.15 (0.15) | -0.15 (0.15) | <0.01b (<0.01) | +0.33 (0.15)* | 0.33 (0.15) | +0.18 (0.22) |
| Age comparisons | DiD (SE)adj. p | DiD (SE)adj. p | DiD (SE)adj. p |
| 18–25 vs. 12–17 | +0.52 (0.27) | +1.96 (0.39)§ | +2.48 (0.40)§ |
| 26–34 vs. 12–17 | +0.98 (0.40) | +1.93 (0.44)§ | +2.91 (0.39)§ |
| 35–49 vs. 12–17 | +0.47 (0.25) | +0.96 (0.28)§ | +1.42 (0.29)§ |
| 50–64 vs. 12–17 | +0.65 (0.23) | +1.11 (0.31)§ | +1.75 (0.32)§ |
| ≥65 vs. 12–17 | +0.27 (0.23) | +0.25 (0.21) | +0.51 (0.27) |
| 26–34 vs. 18–25 | +0.47 (0.39) | -0.03 (0.51) | +0.43 (0.51) |
| 35–49 vs. 18–25 | -0.05 (0.30) | -1.00 (0.40) | -1.05 (0.41) |
| 50–64 vs. 18–25 | +0.13 (0.31) | -0.85 (0.50) | -0.73 (0.49) |
| ≥65 vs. 18–25 | -0.25 (0.30) | -1.71 (0.37)§ | -1.96 (0.40)§ |
| 35–49 vs. 26–34 | -0.52 (0.38) | -0.97 (0.47) | -1.49 (0.45)§ |
| 50–64 vs. 26–34 | -0.34 (0.38) | -0.82 (0.50) | -1.16 (0.46) |
| ≥65 vs. 26–34 | -0.72 (0.36) | -1.68 (0.44)§ | -2.40 (0.41)§ |
| 50–64 vs. 35–49 | +0.18 (0.25) | +0.15 (0.34) | +0.33 (0.33) |
| ≥65 vs. 35–49 | -0.20 (0.26) | -0.71 (0.29) | -0.91 (0.34) |
| ≥65 vs. 50–64 | -0.38 (0.23) | -0.86 (0.33) | -1.24 (0.36)§ |
Notes: Daily use indicates 300 or more days of cannabis use in the past 12 months. Dif. = difference; DiD = difference in difference; adj. = adjusted.
Yearly prevalences are weighted and estimated from an unadjusted multinomial model with a categorical time variable and age by time interactions;
no individuals age ≥ 65 met criteria for daily cannabis use in 2007.
p < .05;
p ≤ .01;
p ≤ .001;
significant below corrected p value of .05/15 pairwise comparisons per time period (adj. p < .0033).
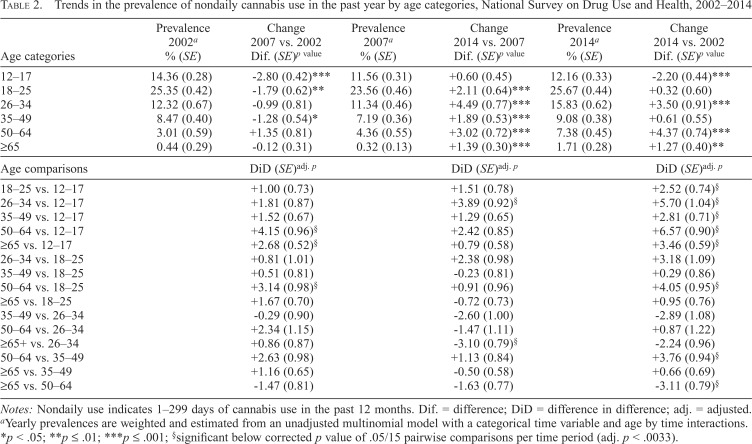
Nondaily cannabis use across age categories
Model-based prevalences of past-year nondaily cannabis use by age are shown in Table 2. Nondaily cannabis use was highest among 18- to 25-year-olds across all years. In 2002, prevalence was higher among those 12–17 than 26–34, but this pattern reversed by 2014, when nondaily cannabis use was higher among those 26–34 than 12–17 (Supplemental Figure B). Before 2007, nondaily cannabis use decreased significantly in ages 12–17, 18–25, and 35–49, and remained stable among ages 26–34 and 50 and older. After 2007, nondaily cannabis use increased significantly across all adult age categories and remained stable among ages 12–17. The largest increase in nondaily cannabis use after 2007 was observed among ages 26–34 (i.e., 4.49% increase); this increase was significantly larger than changes in ages 12–17 and 65 and older, but not significantly different from increases in other age groups after multiple testing adjustment.
Table 2.
Trends in the prevalence of nondaily cannabis use in the past year by age categories, National Survey on Drug Use and Health, 2002–2014
| Age categories | Prevalence 2002a (SE) | Change in prevalence 2007 vs. 2002 Dif. (SE)p value | Prevalence 2002a (SE) | Change in prevalence 2014 vs. 2007 Dif. (SE)p value | Prevalence 2002a (SE) | Change in prevalence 2014 vs. 2002 Dif. (SE)p value |
| 12–17 | 14.36 (0.28) | -2.80 (0.42)*** | 11.56 (0.31) | +0.60 (0.45) | 12.16 (0.33) | -2.20 (0.44)*** |
| 18–25 | 25.35 (0.42) | -1.79 (0.62)** | 23.56 (0.46) | +2.11 (0.64)*** | 25.67 (0.44) | +0.32 (0.60) |
| 26–34 | 12.32 (0.67) | -0.99 (0.81) | 11.34 (0.46) | +4.49 (0.77)*** | 15.83 (0.62) | +3.50 (0.91)*** |
| 35–49 | 8.47 (0.40) | -1.28 (0.54)* | 7.19 (0.36) | +1.89 (0.53)*** | 9.08 (0.38) | +0.61 (0.55) |
| 50–64 | 3.01 (0.59) | +1.35 (0.81) | 4.36 (0.55) | +3.02 (0.72)*** | 7.38 (0.45) | +4.37 (0.74)*** |
| ≥65 | 0.44 (0.29) | -0.12 (0.31) | 0.32 (0.13) | +1.39 (0.30)*** | 1.71 (0.28) | +1.27 (0.40)** |
| Age comparisons | DiD (SE)adj. p | DiD (SE)adj. p | DiD (SE)adj. p |
| 18–25 vs. 12–17 | +1.00 (0.73) | +1.51 (0.78) | +2.52 (0.74)§ |
| 26–34 vs. 12–17 | +1.81 (0.87) | +3.89 (0.92)§ | +5.70 (1.04)§ |
| 35–49 vs. 12–17 | +1.52 (0.67) | +1.29 (0.65) | +2.81 (0.71)§ |
| 50–64 vs. 12–17 | +4.15 (0.96)§ | +2.42 (0.85) | +6.57 (0.90)§ |
| ≥65 vs. 12–17 | +2.68 (0.52)§ | +0.79 (0.58) | +3.46 (0.59)§ |
| 26–34 vs. 18–25 | +0.81 (1.01) | +2.38 (0.98) | +3.18 (1.09) |
| 35–49 vs. 18–25 | +0.51 (0.81) | -0.23 (0.81) | +0.29 (0.86) |
| 50–64 vs. 18–25 | +3.14 (0.98)§ | +0.91 (0.96) | +4.05 (0.95)§ |
| ≥65 vs. 18–25 | +1.67 (0.70) | -0.72 (0.73) | +0.95 (0.76) |
| 35–49 vs. 26–34 | -0.29 (0.90) | -2.60 (1.00) | -2.89 (1.08) |
| 50–64 vs. 26–34 | +2.34 (1.15) | -1.47 (1.11) | +0.87 (1.22) |
| ≥65+ vs. 26–34 | +0.86 (0.87) | -3.10 (0.79)§ | -2.24 (0.96) |
| 50–64 vs. 35–49 | +2.63 (0.98) | +1.13 (0.84) | +3.76 (0.94)§ |
| ≥65 vs. 35–49 | +1.16 (0.65) | -0.50 (0.58) | +0.66 (0.69) |
| ≥65 vs. 50–64 | -1.47 (0.81) | -1.63 (0.77) | -3.11 (0.79)§ |
Notes: Nondaily use indicates 1–299 days of cannabis use in the past 12 months. Dif. = difference; DiD = difference in difference; adj. = adjusted.
Yearly prevalences are weighted and estimated from an unadjusted multinomial model with a categorical time variable and age by time interactions.
p < .05;
p ≤ .01;
p ≤ .001;
significant below corrected p value of .05/15 pairwise comparisons per time period (adj. p < .0033).
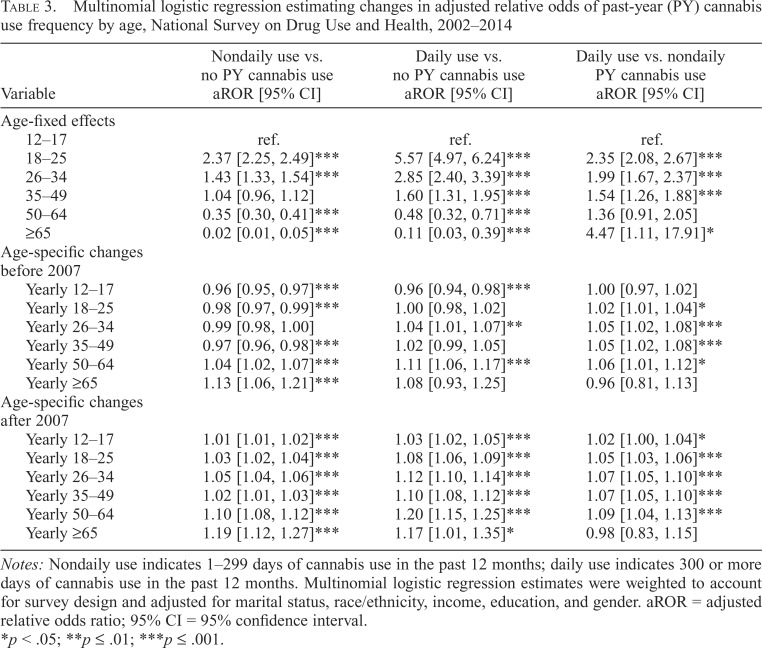
Relative odds of past-year cannabis use: daily, nondaily, and no past-year use
Adjusted multinomial logistic regression findings are presented in Table 3. Adults 18–34 had significantly higher adjusted odds of nondaily (or daily) cannabis use versus no past-year use and had approximately twice the odds of daily versus nondaily cannabis use, relative to ages 12–17. Before 2007, odds of daily versus nondaily use increased for adults ages 18–64, and among ages 12–64 after 2007, indicating more frequent use among cannabis users after 2007. Consistent with findings of no change in trends for middle-aged adults, ages 50–64 had significant increases in the odds of more frequent cannabis use (e.g., nondaily vs. none, daily vs. none, and daily vs. nondaily) both before and after 2007. For example, before 2007, each year was associated with a 6% increase in the adjusted odds of daily versus nondaily cannabis use among ages 50–64, and a 9% increase each year after 2007. Adjusted odds of more frequent cannabis use (e.g., nondaily vs. none, daily vs. none, and daily vs. nondaily) increased significantly after 2007 for all ages 12–64. Sensitivity analyses including employment status did not substantially change the magnitude or direction of any of the time trend associations of interest (Supplemental Table D).
Table 3.
Multinomial logistic regression estimating changes in adjusted relative odds of past-year (PY) cannabis use frequency by age, National Survey on Drug Use and Health, 2002–2014
| Variable | Nondaily use vs. no PY cannabis use aROR [95% CI] | Daily use vs. no PY cannabis use aROR [95% CI] | Daily use vs. nondaily PY cannabis use aROR [95% CI] |
| Age-fixed effects | |||
| 12–17 | ref. | ref. | ref. |
| 18–25 | 2.37 [2.25, 2.49]*** | 5.57 [4.97, 6.24]*** | 2.35 [2.08, 2.67]*** |
| 26–34 | 1.43 [1.33, 1.54]*** | 2.85 [2.40, 3.39]*** | 1.99 [1.67, 2.37]*** |
| 35–49 | 1.04 [0.96, 1.12] | 1.60 [1.31, 1.95]*** | 1.54 [1.26, 1.88]*** |
| 50–64 | 0.35 [0.30, 0.41]*** | 0.48 [0.32, 0.71]*** | 1.36 [0.91, 2.05] |
| ≥65 | 0.02 [0.01, 0.05]*** | 0.11 [0.03, 0.39]*** | 4.47 [1.11, 17.91]* |
| Age-specific changes before 2007 | |||
| Yearly 12–17 | 0.96 [0.95, 0.97]*** | 0.96 [0.94, 0.98]*** | 1.00 [0.97, 1.02] |
| Yearly 18–25 | 0.98 [0.97, 0.99]*** | 1.00 [0.98, 1.02] | 1.02 [1.01, 1.04]* |
| Yearly 26–34 | 0.99 [0.98, 1.00] | 1.04 [1.01, 1.07]** | 1.05 [1.02, 1.08]*** |
| Yearly 35–49 | 0.97 [0.96, 0.98]*** | 1.02 [0.99, 1.05] | 1.05 [1.02, 1.08]*** |
| Yearly 50–64 | 1.04 [1.02, 1.07]*** | 1.11 [1.06, 1.17]*** | 1.06 [1.01, 1.12]* |
| Yearly ≥65 | 1.13 [1.06, 1.21]*** | 1.08 [0.93, 1.25] | 0.96 [0.81, 1.13] |
| Age-specific changes after 2007 | |||
| Yearly 12–17 | 1.01 [1.01, 1.02]*** | 1.03 [1.02, 1.05]*** | 1.02 [1.00, 1.04]* |
| Yearly 18–25 | 1.03 [1.02, 1.04]*** | 1.08 [1.06, 1.09]*** | 1.05 [1.03, 1.06]*** |
| Yearly 26–34 | 1.05 [1.04, 1.06]*** | 1.12 [1.10, 1.14]*** | 1.07 [1.05, 1.10]*** |
| Yearly 35–49 | 1.02 [1.01, 1.03]*** | 1.10 [1.08, 1.12]*** | 1.07 [1.05, 1.10]*** |
| Yearly 50–64 | 1.10 [1.08, 1.12]*** | 1.20 [1.15, 1.25]*** | 1.09 [1.04, 1.13]*** |
| Yearly ≥65 | 1.19 [1.12, 1.27]*** | 1.17 [1.01, 1.35]* | 0.98 [0.83, 1.15] |
Notes: Nondaily use indicates 1–299 days of cannabis use in the past 12 months; daily use indicates 300 or more days of cannabis use in the past 12 months. Multinomial logistic regression estimates were weighted to account for survey design and adjusted for marital status, race/ethnicity, income, education, and gender. aROR = adjusted relative odds ratio; 95% CI = 95% confidence interval.
p < .05;
p ≤ .01;
p ≤ .001.
Discussion
This nationally representative study estimated age-specific trends in cannabis use, differentiating trends in past-year daily and nondaily cannabis use between 2002 and 2014. Using a strict daily use definition of 300 days or more of use in the past year (Pacek et al., 2015; SAMHSA, 2014), we found significant increases in daily cannabis use across adult age categories after 2007 that contrasted with stable prevalence before 2007 and decreases among adolescents. Steady or declining cannabis use among adolescents is consistent with previous studies of recent cannabis use trends in youth and contrasts with increasing use among adults (Carliner et al., 2017a). Daily cannabis use increased after 2007 across adult ages. Of note, however, is the yearly increase in more frequent use among cannabis users 18–64 since 2002, and ages 12–64 since 2007, evidenced by the temporal increases in the adjusted odds of daily versus nondaily use in these ages. Although any cannabis use may be decreasing among teens, odds of more frequent use have been increasing among users since 2007. To identify youth who may be in need of additional support, studies should assess not only any cannabis use but also frequency of use, because adverse effects of cannabis are especially likely among frequent users.
We partially confirmed previous findings indicating 2007 as a change point in cannabis use trends (Carliner et al., 2017b; Compton et al., 2016), finding no significant change in trends for adults 50 and older, although statistical power could be limited in age groups 65 and older given the low prevalence of use. Changing trends in 2007 occurred in the context of an economic crisis, which has been suggested as a contributor to the widening gender gap in adult cannabis use (Carliner et al., 2017b). In addition, the legal status of cannabis for medicinal and recreational use rapidly evolved between 2007 and 2014: The number of states with medical cannabis laws doubled from 12 to 24, and four states also legalized recreational cannabis use (National Conference of State Legislatures, 2018). Future studies should explore the combined effect of both economic fluctuations and changing cannabis use laws across age strata, particularly among middle-age and older adults who have traditionally not been the focus of cannabis use research (Han et al., 2017).
Emerging and young adults ages 18–34 had the largest absolute increases in daily cannabis use since 2007, although these increases were not significantly different from those of other age groups. However, because the youngest groups also had the highest prevalence of use, this indicated a lower relative increase in prevalence over time as compared with older age groups. The increasing similarity in patterns of cannabis use in the two youngest adult age categories is consistent with Arnett and colleagues’ extension of emerging adulthood to include ages 18–29 (Arnett et al., 2014). Age differences in cannabis use remained after adjusting for various demographic variables including education, marital status, and household income; a sensitivity model that further adjusted for employment yielded consistent results. The sociodemographic distributions by age may be shifting over time (Supplemental Table B), which could lead to changes in cannabis use patterns within other demographic subgroups, such as married individuals. However, the observed increase in cannabis use frequency among adults since 2007 does not seem to be fully explained by individual characteristics, calling for further attention to structural and policy factors.
The prevalence of nondaily cannabis use among ages 35–49 remained stable from 8.5% in 2002 to 9.1% in 2014. This is consistent with prior studies indicating lower use in this age group compared with younger ages (Chen & Kandel, 1998; Jochman & Fromme, 2010; Labouvie, 1996). However, the prevalence of daily cannabis use doubled from 0.9% to 2.0%, and the odds of daily versus nondaily use increased significantly over the whole period among 35 to 49-year-olds. Given the overall lower prevalence of cannabis use in this age group compared with younger ages, future research should investigate the characteristics of these frequent users. Factors related to both discontinuation of use as well as maintained daily use should be examined further in this particular age group in the context of current demographic and social trends.
Daily cannabis use prevalence among middle-age adults more than tripled between 2007 and 2014 but remained smaller in magnitude than younger age groups. Our findings also indicate that absolute 1.2% prevalence increase in daily cannabis use among middle-age adults was comparable to increases reported by their younger counterparts after 2007. Middle-age adults 50–64 were the only group with increases in nondaily cannabis use both before and after 2007, and had the largest prevalence increases in nondaily cannabis use from 2002 to 2014. By 2014, the NSDUH age category of 50–64 comprised entirely baby boomers (born 1946–1964). If trends continue, prevalence estimates of cannabis use among ages 50–64 could surpass those of adults ages 35–49. Research about the patterns, correlates, and consequences of cannabis use in baby boomers is needed, since prevalence of use is higher than that of previous cohorts and is expected to continue to increase (Colliver et al., 2006; Han et al., 2009). Moreover, significant increases in nondaily cannabis use among adults 65 and older defy perceptions that older adults do not use cannabis, although daily use in this age group remains rare.
Cannabis use in older adults presents unique physiological concerns, as older adults metabolize drugs more slowly with age (Blazer & Wu, 2009; Blow, 1998; Blow & Barry, 2012). Current cannabis use in older age is associated with higher odds of having a substance use disorder than in previous or never cannabis users 50 and older (Choi et al., 2016; DiNitto & Choi, 2011). Older adults may increasingly be using cannabis to treat conditions that are more prevalent with age; for example, a qualitative study of this birth cohort in California indicated that many used cannabis as a harm-reduction approach to self-medicate pain (Lau et al., 2015). Cannabis use may reduce opioid use among older adults, particularly through access to medical cannabis (Smart, 2015). Because of the federal restrictions on conducting cannabis research, there are substantial gaps in the evidence about medical harms and benefits of cannabis (National Academies of Science, Engineering, and Medicine, 2017). Future studies should focus on consequences of medical and recreational use of cannabis, and particularly among older adults, to inform appropriate clinical recommendations.
Study limitations are noted: Cannabis use was based on self-report, which could lead to biased estimates. The NSDUH aimed to reduce bias in substance use estimates by using CAPI and ACASI to ensure confidentiality and honest responses (CBHSQ, 2015b). Although the changing legal status of cannabis could increase people’s willingness to disclose a previously illegal behavior, the increased trends shown in NSDUH data are consistent with other national increases in indicators of cannabis-related harms (Hasin, 2018; Hasin & Grant, 2016), supporting the validity of the present findings. Because of the NSDUH design (Kennet & Gfroerer, 2005), we were not able to assess trends before 2002; as previously noted, estimates before and after 2002 differed significantly, partially attributed to methodological differences (Miech & Koester, 2012). The NSDUH methodology was largely consistent during 2002–2014 (CBHSQ, 2014), enhancing our confidence that the observed significant increase in cannabis use prevalence is not a methodological artifact. The repeated cross-sectional design of the NSDUH did not follow individual participants over time. Longitudinal studies following groups as they age could provide additional information about causes of transitions to use or re-initiation of use of cannabis.
In conclusion, patterns of increasing daily and nondaily cannabis use prevalence over time among adults since 2007 contrasted with stable or decreasing prevalence of use among adolescents. In the context of changing medical and recreational cannabis legislation, prevalence of daily cannabis use should be monitored, particularly among adult age groups with the largest relative increases in cannabis use frequency. Studies should estimate how increases in daily cannabis use among adults affect the prevalence of other substance use, such as alcohol, tobacco, and opioids. Because the legal status of cannabis use is changing so rapidly and could have benefits among older adults and risks among young adults (Smart, 2015), continued research is needed to track changes in cannabis use frequency and its consequences by age in this new social and legal context. Nonetheless, trends indicating higher odds of more frequent use across past-year users ages 12–64, including adolescents, call for a more targeted prevention and harm-reduction approaches for people reporting daily cannabis use.
Footnotes
Financial support was provided by National Institute on Drug Abuse Grants T32DA031099 (principal investigator: Deborah S. Hasin), R01DA037866 (principal investigator: Silvia S. Martins), and R01DA034244 (principal investigator: Deborah S. Hasin), and the New York State Psychiatric Institute. The authors have no conflicts of interest to report.
References
- Aharonovich E., Shmulewitz D., Wall M. M., Grant B. F., Hasin D. S. Self-reported cognitive scales in a US National Survey: Reliability, validity, and preliminary evidence for associations with alcohol and drug use. Addiction. 2017;112:2132–2143. doi: 10.1111/add.13911. doi:10.1111/add.13911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson M. D., Hansen B., Rees D. I. Medical marijuana laws and teen marijuana use. American Law and Economics Review. 2015;17:495–528. doi:10.1093/aler/ahv002. [Google Scholar]
- Arnett J. J., Žukauskieneæ R., Sugimura K. The new life stage of emerging adulthood at ages 1829 years: Implications for mental health. The Lancet Psychiatry. 2014;1:569–576. doi: 10.1016/S2215-0366(14)00080-7. doi:10.1016/S2215-0366(14)00080-7. [DOI] [PubMed] [Google Scholar]
- Auer R., Vittinghoff E., Yaffe K., Künzi A., Kertesz S. G., Levine D. A., Pletcher M. J. Association between lifetime marijuana use and cognitive function in middle age: The coronary artery risk development in young adults (CARDIA) study. JAMA Internal Medicine. 2016;176:352–361. doi: 10.1001/jamainternmed.2015.7841. doi:10.1001/jamainternmed.2015.7841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieler G. S., Brown G. G., Williams R. L., Brogan D. J. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. American Journal of Epidemiology. 2010;171:618–623. doi: 10.1093/aje/kwp440. doi:10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- Blanco C., Hasin D. S., Wall M. M., Flórez-Salamanca L., Hoertel N., Wang S., Olfson M. Cannabis use and risk of psychiatric disorders: Prospective evidence from a US national longitudinal study. JAMA Psychiatry. 2016;73:388–395. doi: 10.1001/jamapsychiatry.2015.3229. doi:10.1001/jamapsychiatry.2015.3229. [DOI] [PubMed] [Google Scholar]
- Blazer D. G., Wu L. T. The epidemiology of substance use and disorders among middle aged and elderly community adults: National survey on drug use and health. American Journal of Geriatric Psychiatry. 2009;17:237–245. doi: 10.1097/JGP.0b013e318190b8ef. doi:10.1097/JGP.0b013e318190b8ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow F. C. Rockville, MD: Substance Abuse and Mental Health Services Administration; 1998. Substance abuse among older adults. [PubMed] [Google Scholar]
- Blow F. C., Barry K. L. Alcohol and substance misuse in older adults. Current Psychiatry Reports. 2012;14:310–319. doi: 10.1007/s11920-012-0292-9. doi:10.1007/s11920-012-0292-9. [DOI] [PubMed] [Google Scholar]
- Brady J. E., Li G. Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999–2010. American Journal of Epidemiology. 2014;179:692–699. doi: 10.1093/aje/kwt327. doi:10.1093/aje/kwt327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Q. L., Sarvet A. L., Shmulewitz D., Martins S. S., Wall M. M., Hasin D. S. Trends in marijuana use among pregnant and nonpregnant reproductive-aged women, 2002–2014. JAMA. 2017;317:207–209. doi: 10.1001/jama.2016.17383. doi:10.1001/jama.2016.17383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H., Brown Q. L., Sarvet A. L., Hasin D. S. Cannabis use, attitudes, and legal status in the U.S.: A review. Preventive Medicine. 2017a;104:13–23. doi: 10.1016/j.ypmed.2017.07.008. doi:10.1016/j.ypmed.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H., Mauro P. M., Brown Q. L., Shmulewitz D., Rahim-Juwel R., Sarvet A. L., Hasin D. S. The widening gender gap in marijuana use prevalence in the U.S. during a period of economic change, 2002–2014. Drug and Alcohol Dependence. 2017b;170:51–58. doi: 10.1016/j.drugalcdep.2016.10.042. doi:10.1016/j.drugalcdep.2016.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. National Survey on Drug Use and Health (NSDUH): Summary of methodological studies, 1971–2014. [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015a. 2014 National Survey on Drug Use and Health: Detailed tables. [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015b. 2014 National Survey on Drug Use and Health: Methodological summary and definitions. [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015c. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50) Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf. [Google Scholar]
- Chen K., Kandel D. B. Predictors of cessation of marijuana use: An event history analysis. Drug and Alcohol Dependence. 1998;50:109–121. doi: 10.1016/s0376-8716(98)00021-0. doi:10.1016/S0376-8716(98)00021-0. [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N. Older-adult marijuana users and ex-users: Comparisons of sociodemographic characteristics and mental and substance use disorders. Drug and Alcohol Dependence. 2016;165:94–102. doi: 10.1016/j.drugalcdep.2016.05.023. doi:10.1016/j.drugalcdep.2016.05.023. [DOI] [PubMed] [Google Scholar]
- Choo E. K., Benz M., Zaller N., Warren O., Rising K. L., McConnell K. J. The impact of state medical marijuana legislation on adolescent marijuana use. Journal of Adolescent Health. 2014;55:160–166. doi: 10.1016/j.jadohealth.2014.02.018. doi:10.1016/j.jadohealth.2014.02.018. [DOI] [PubMed] [Google Scholar]
- Chu Y. W. The effects of medical marijuana laws on illegal marijuana use. Journal of Health Economics. 2014;38:43–61. doi: 10.1016/j.jhealeco.2014.07.003. doi:10.1016/j.jhealeco.2014.07.003. [DOI] [PubMed] [Google Scholar]
- Cohn A., Villanti A., Richardson A., Rath J. M., Williams V., Stanton C., Mermelstein R. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addictive Behaviors. 2015;48:79–88. doi: 10.1016/j.addbeh.2015.02.005. doi:10.1016/j.addbeh.2015.02.005. [DOI] [PubMed] [Google Scholar]
- Colliver J. D., Compton W. M., Gfroerer J. C., Condon T. Projecting drug use among aging baby boomers in 2020. Annals of Epidemiology. 2006;16:257–265. doi: 10.1016/j.annepidem.2005.08.003. doi:10.1016/j.annepidem.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Compton W. M., Gfroerer J., Conway K. P., Finger M. S. Unemployment and substance outcomes in the United States 2002– 2010. Drug and Alcohol Dependence. 2014;142:350–353. doi: 10.1016/j.drugalcdep.2014.06.012. doi:10.1016/j.drugalcdep.2014.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W. M., Han B., Jones C. M., Blanco C., Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: Analysis of annual cross-sectional surveys. The Lancet Psychiatry. 2016;3:954–964. doi: 10.1016/S2215-0366(16)30208-5. doi:10.1016/S2215-0366(16)30208-5. [DOI] [PubMed] [Google Scholar]
- Copeland J., Swift W. Cannabis use disorder: Epidemiology and management. International Review of Psychiatry. 2009;21:96–103. doi: 10.1080/09540260902782745. doi:10.1080/09540260902782745. [DOI] [PubMed] [Google Scholar]
- Davis G. P., Compton M. T., Wang S., Levin F. R., Blanco C. Association between cannabis use, psychosis, and schizotypal personality disorder: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Schizophrenia Research. 2013;151:197–202. doi: 10.1016/j.schres.2013.10.018. doi:10.1016/j.schres.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M., Marconi A., Carra E., Fraietta S., Trotta A., Bonomo M., Murray R. M. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: A case-control study. The Lancet Psychiatry. 2015;2:233–238. doi: 10.1016/S2215-0366(14)00117-5. doi:10.1016/S2215-0366(14)00117-5. [DOI] [PubMed] [Google Scholar]
- DiNardo J., Lemieux T. Alcohol, marijuana, and American youth: The unintended consequences of government regulation. Journal of Health Economics. 2001;20:991–1010. doi: 10.1016/s0167-6296(01)00102-3. doi:10.1016/S0167-6296(01)00102-3. [DOI] [PubMed] [Google Scholar]
- DiNitto D. M., Choi N. G. Marijuana use among older adults in the U.S.A.: User characteristics, patterns of use, and implications for intervention. International Psychogeriatrics. 2011;23:732–741. doi: 10.1017/S1041610210002176. doi:10.1017/S1041610210002176. [DOI] [PubMed] [Google Scholar]
- Dowling G. J., Weiss S. R., Condon T. P. Drugs of abuse and the aging brain. Neuropsychopharmacology. 2008;33:209–218. doi: 10.1038/sj.npp.1301412. doi:10.1038/sj.npp.1301412. [DOI] [PubMed] [Google Scholar]
- Fergusson D. M., Boden J. M., Horwood L. J. Psychosocial sequelae of cannabis use and implications for policy: Findings from the Christchurch Health and Development Study. Social Psychiatry and Psychiatric Epidemiology. 2015;50:1317–1326. doi: 10.1007/s00127-015-1070-x. doi:10.1007/s00127-015-1070-x. [DOI] [PubMed] [Google Scholar]
- Freese J., Long J. S. College Station, TX: Stata Press; 2006. Regression models for categorical dependent variables using Stata. [Google Scholar]
- Gogtay N., Giedd J. N., Lusk L., Hayashi K. M., Greenstein D., Vaituzis A. C., Thompson P. M. Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. doi:10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza R. A., Agrawal A., Krauss M. J., Bongu J., Plunk A. D., CavazosRehg P. A., Bierut L. J. Declining prevalence of marijuana use disorders among adolescents in the United States, 2002 to 2013. Journal of the American Academy of Child and Adolescent Psychiatry. 2016a;55:487–494.e6. doi: 10.1016/j.jaac.2016.04.002. doi:10.1016/j.jaac.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza R. A., Agrawal A., Krauss M. J., Cavazos-Rehg P. A., Bierut L. J. Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA Psychiatry. 2016b;73:300–301. doi: 10.1001/jamapsychiatry.2015.3111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen T. D., Jorgensen N., Andersson A.-M., Bang A. K., Nordkap L., Skakkebaek N. E., Jensen T. K. Association between use of marijuana and male reproductive hormones and semen quality: A study among 1,215 healthy young men. American Journal of Epidemiology. 2015;182:473–481. doi: 10.1093/aje/kwv135. doi:10.1093/aje/kwv135. [DOI] [PubMed] [Google Scholar]
- Guxens M., Nebot M., Ariza C. Age and sex differences in factors associated with the onset of cannabis use: A cohort study. Drug and Alcohol Dependence. 2007;88:234–243. doi: 10.1016/j.drugalcdep.2006.10.018. doi:10.1016/j.drugalcdep.2006.10.018. [DOI] [PubMed] [Google Scholar]
- Hall W. The adverse health effects of cannabis use: What are they, and what are their implications for policy? International Journal on Drug Policy. 2009;20:458–466. doi: 10.1016/j.drugpo.2009.02.013. doi:10.1016/j.drugpo.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110:19–35. doi: 10.1111/add.12703. doi:10.1111/add.12703. [DOI] [PubMed] [Google Scholar]
- Hall W., Degenhardt L. Adverse health effects of non-medical cannabis use. The Lancet. 2009;374:1383–1391. doi: 10.1016/S0140-6736(09)61037-0. doi:10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- Hall W., Degenhardt L. The adverse health effects of chronic cannabis use. Drug Testing and Analysis. 2014;6:39–45. doi: 10.1002/dta.1506. doi:10.1002/dta.1506. [DOI] [PubMed] [Google Scholar]
- Han B., Gfroerer J. C., Colliver J. D., Penne M. A. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. doi:10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- Han B. H., Sherman S., Mauro P. M., Martins S. S., Rotenberg J., Palamar J. J. Demographic trends among older cannabis users in the United States, 2006–13. Addiction. 2017;112:516–525. doi: 10.1111/add.13670. doi:10.1111/add.13670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S., Strumpf E. C., Kaufman J. S. Do medical marijuana laws increase marijuana use? Replication study and extension. Annals of Epidemiology. 2012;22:207–212. doi: 10.1016/j.annepidem.2011.12.002. doi:10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Hartman R. L., Brown T. L., Milavetz G., Spurgin A., Pierce R. S., Gorelick D. A., Huestis M. A. Cannabis effects on driving lateral control with and without alcohol. Drug and Alcohol Dependence. 2015;154:25–37. doi: 10.1016/j.drugalcdep.2015.06.015. doi:10.1016/j.drugalcdep.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman R. L., Brown T. L., Milavetz G., Spurgin A., Pierce R. S., Gorelick D. A., Huestis M. A. Cannabis effects on driving longitudinal control with and without alcohol. Journal of Applied Toxicology. 2016;36:1418–1429. doi: 10.1002/jat.3295. doi:10.1002/jat.3295. [DOI] [PubMed] [Google Scholar]
- Hartman R. L., Huestis M. A. Cannabis effects on driving skills. Clinical Chemistry. 2013;59:478–492. doi: 10.1373/clinchem.2012.194381. doi:10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S. U.S. epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 2018;43:195–212. doi: 10.1038/npp.2017.198. doi:10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Grant B. NESARC findings on increased prevalence of marijuana use disorders—consistent with other sources of information. JAMA Psychiatry. 2016;73:532. doi: 10.1001/jamapsychiatry.2015.3158. doi:10.1001/jamapsychiatry.2015.3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Kerridge B. T., Saha T. D., Huang B., Pickering R., Smith S. M., Grant B. F. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: Findings from the national epidemiologic survey on alcohol and related conditions-III. American Journal of Psychiatry. 2016;173:588–599. doi: 10.1176/appi.ajp.2015.15070907. doi:10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Saha T. D., Kerridge B. T., Goldstein R. B., Chou S. P., Zhang H., Grant B. F. Prevalence of marijuana use disorders in the united states between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. doi:10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Sarvet A. L., Cerdá M., Keyes K. M., Stohl M., Galea S., Wall M. M. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991–1992 to 2012–2013. JAMA Psychiatry. 2017;74:579–588. doi: 10.1001/jamapsychiatry.2017.0724. doi:10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayaki J., Anderson B. J., Stein M. D. Dual cannabis and alcohol use disorders in young adults: Problems magnified. Substance Abuse. 2016;37:579–583. doi: 10.1080/08897077.2016.1176613. doi:10.1080/08897077.2016.1176613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jochman K. A., Fromme K. Maturing out of substance use: The other side of etiology. In: Schemer L. M., editor. Handbook of drug use etiology: Theory, methods, and empirical findings. Washington, DC: American Psychological Association; 2010. pp. 565–578. [Google Scholar]
- Johnson J. Waltham, MA: The Heller School for Social Policy and Management, Brandeis University; 2015. Do state liberalized marijuana policies affect adolescent marijuana and alcohol use? A state-level analysis. [Google Scholar]
- Johnson J., Hodgkin D., Harris S. K. The design of medical marijuana laws and adolescent use and heavy use of marijuana: Analysis of 45 states from 1991 to 2011. Drug and Alcohol Dependence. 2017;170:1–8. doi: 10.1016/j.drugalcdep.2016.10.028. doi:10.1016/j.drugalcdep.2016.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. M., Fairman B., Gilreath T., Xuan Z., Rothman E. F., Parnham T., Furr-Holden C. D. Past 15-year trends in adolescent marijuana use: Differences by race/ethnicity and sex. Drug and Alcohol Dependence. 2015;155:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. doi:10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennet J., Gfroerer J. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. Evaluating and improving methods used in the national survey on drug use and health (DHHS Publication No. SMA 05-4044, Methodology Series M-5) [Google Scholar]
- Kerr W. C., Greenfield T. K., Bond J., Ye Y., Rehm J. Age-period-cohort influences on trends in past year marijuana use in the US from the 1984, 1990, 1995 and 2000 National Alcohol Surveys. Drug and Alcohol Dependence. 2007;86:132–138. doi: 10.1016/j.drugalcdep.2006.05.022. doi:10.1016/j.drugalcdep.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Kerr W. C., Lui C., Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984–2015 US National Alcohol Surveys. Addiction. 2018;113:473–481. doi: 10.1111/add.14031. doi:10.1111/add.14031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K. M., Vo T., Wall M. M., Caetano R., Suglia S. F., Martins S. S., Hasin D. Racial/ethnic differences in use of alcohol, tobacco, and marijuana: Is there a cross-over from adolescence to adulthood? Social Science & Medicine. 2015;124:132–141. doi: 10.1016/j.socscimed.2014.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K. M., Wall M., Cerdá M., Schulenberg J., O’Malley P. M., Galea S., Hasin D. S. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction. 2016;111:2187–2195. doi: 10.1111/add.13523. doi:10.1111/add.13523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A., Sacco P., Blazer D. G., Moore A. A. Substance abuse among older adults. Clinics in Geriatric Medicine. 2014;30:629–654. doi: 10.1016/j.cger.2014.04.008. doi:10.1016/j.cger.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labouvie E. Maturing out of substance use: Selection and self-correction. Journal of Drug Issues. 1996;26:457–476. doi:10.1177/002204269602600208. [Google Scholar]
- Lau N., Sales P., Averill S., Murphy F., Sato S. O., Murphy S. A safer alternative: Cannabis substitution as harm reduction. Drug and Alcohol Review. 2015;34:654–659. doi: 10.1111/dar.12275. doi:10.1111/dar.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Y., Brook J. S., Finch S. J., Brook D. W. Trajectories of marijuana use from adolescence to adulthood predicting unemployment in the mid 30s. American Journal on Addictions. 2015;24:452–459. doi: 10.1111/ajad.12240. doi:10.1111/ajad.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S. S., Mauro C. M., Santaella-Tenorio J., Kim J. H., Cerda M., Keyes K. M., Wall M. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug and Alcohol Dependence. 2016;169:26–32. doi: 10.1016/j.drugalcdep.2016.10.004. doi:10.1016/j.drugalcdep.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier M. H., Caspi A., Ambler A., Harrington H., Houts R., Keefe R. S. E., Moffitt T. E. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:E2657–E2664. doi: 10.1073/pnas.1206820109. doi:10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R., Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: An age-period-cohort analysis. Drug and Alcohol Dependence. 2012;124:259–267. doi: 10.1016/j.drugalcdep.2012.01.020. doi:10.1016/j.drugalcdep.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Science, Engineering, and Medicine. Washington, DC: The National Academies Press; 2017. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. doi:1.17226/24625. [PubMed] [Google Scholar]
- National Conference of State Legislatures. Marijuana overview. 2017, August 30 Retrieved from http://www.ncsl.org/research/civil-and-criminal-justice/marijuana-overview.aspx#2.
- National Conference of State Legislatures. State medical marijuana laws. 2018, February 1 Retrieved from http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- Pacek L. R., Mauro P. M., Martins S. S. Perceived risk of regular cannabis use in the United States from 2002 to 2012: Differences by sex, age, and race/ethnicity. Drug and Alcohol Dependence. 2015;149:232–244. doi: 10.1016/j.drugalcdep.2015.02.009. doi:10.1016/j.drugalcdep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula R. L., Powell D., Heaton P., Sevigny E. L. Assessing the effects of medical marijuana laws on marijuana use: The devil is in the details. Journal of Policy Analysis and Management. 2015;34:7–31. doi: 10.1002/pam.21804. doi:10.1002/pam.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redonnet B., Chollet A., Fombonne E., Bowes L., Melchior M. Tobacco, alcohol, cannabis and other illegal drug use among young adults: The socioeconomic context. Drug and Alcohol Dependence. 2012;121:231–239. doi: 10.1016/j.drugalcdep.2011.09.002. doi:10.1016/j.drugalcdep.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Rothman K. J., Greenland S., Lash T. L. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. Modern epidemiology (3rd ed.) [Google Scholar]
- Salas-Wright C. P., Vaughn M. G., Cummings-Vaughn L. A., Holzer K. J., Nelson E. J., AbiNader M., Oh S. Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002–2014. Drug and Alcohol Dependence. 2017;171:97–106. doi: 10.1016/j.drugalcdep.2016.11.031. doi:10.1016/j.drugalcdep.2016.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair C. F., Foushee H. R., Scarinci I., Carroll W. R. Perceptions of harm to health from cigarettes, blunts, and marijuana among young adult African American men. Journal of Health Care for the Poor and Underserved. 2013;24:1266–1275. doi: 10.1353/hpu.2013.0126. doi:10.1353/hpu.2013.0126. [DOI] [PubMed] [Google Scholar]
- Smart R. The kids aren’t alright but older adults are just fine: Effects of medical marijuana market growth on substance use and abuse (No. SSRN 2574915) 2015 Retrieved from https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2574915.
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Author; 2003. Results from the 2002 National Survey on Drug Use and Health: National findings (NHSDA Series H-22, DHHS Publication No. SMA 03-3836) [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Author; 2014. Results from the 2013 National Survey on Drug Use and Health: Summary of national findings (NSDUH Series H-48, No. (SMA) 14-4863) [Google Scholar]
- Toms J. D., Lesperance M. L. Piecewise regression: A tool for identifying ecological thresholds. Ecology. 2003;84:2034–2041. doi:10.1890/02-0472. [Google Scholar]
- Volkow N. D., Baler R. D., Compton W. M., Weiss S. R. Adverse health effects of marijuana use. The New England Journal of Medicine. 2014;370:2219–2227. doi: 10.1056/NEJMra1402309. doi:10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N. D., Swanson J. M., Evins A. E., DeLisi L. E., Meier M. H., Gonzalez R., Baler R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry. 2016;73:292–297. doi: 10.1001/jamapsychiatry.2015.3278. doi:10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- Wall M. M., Mauro C., Hasin D. S., Keyes K. M., Cerda M., Martins S. S., Feng T. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: Commentary on and reanalysis of US National Survey on Drug Use in Households data 2002–2011. International Journal on Drug Policy. 2016;29:9–13. doi: 10.1016/j.drugpo.2016.01.015. doi:10.1016/j.drugpo.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H., Hockenberry J. M., Cummings J. R. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health Economics. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. doi:10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. The Stata Journal. 2012;12:308–331. [Google Scholar]
- Wu L. T., Blazer D. G. Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health. 2011;23:481–504. doi: 10.1177/0898264310386224. doi:10.1177/0898264310386224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Brook J. S., Leukefeld C. G., Brook D. W. Trajectories of marijuana use from adolescence to adulthood as predictors of unemployment status in the early forties. American Journal on Addictions. 2016;25:203–209. doi: 10.1111/ajad.12361. doi:10.1111/ajad.12361. [DOI] [PMC free article] [PubMed] [Google Scholar]