Abstract
Objective:
Polydrug users have been shown to be at higher risk for alcohol consumption and crash involvement. However, research has shown that polydrug groups differ in some important ways. It is currently unknown how polydrug-using groups differ in terms of crash involvement and alcohol consumption.
Method:
The current study used latent class analysis to examine subgroups of polydrug users (n = 384) among a sample of drivers in Virginia Beach, Virginia (N = 10,512). A series of logistic regression analyses were conducted to determine the relationship between polydrug use categories and crash involvement and alcohol consumption.
Results:
Four distinct subclasses of users were identified among polydrug-using drivers: Class 1 is the “marijuana-amphetamines class” and accounts for 21.6% of polydrug users. Class 2 is the “benzo-antidepressant class” and accounts for 39.0% of polydrug users. Class 3 is the “opioid-benzo class” and accounts for 32.7% of polydrug users. Finally, Class 4 is the “marijuana-cocaine class” and accounts for 6.7% of the study sample. Drivers in the opioid-benzo class were significantly more likely than those in any other class as well as non–drug users and single-drug users to be involved in a crash and were more likely than those in most other conditions to consume alcohol. No significant difference was found between marijuana-amphetamine users or benzo-antidepressant users and non–drug users on crash risk.
Conclusions:
Some polydrug users are indeed at greater risk for crash involvement and alcohol consumption; however, not all polydrug users are significantly worse than single-drug users and/or non–drug users, and the practice of lumping polydrug users together when predicting crash risk runs the risk of inaccurately attributing crash involvement to certain drivers.
The prevalence of drivers who are under the influence of drugs has been steadily increasing throughout the United States. In a 2007 roadside survey, researchers found that approximately 12.4% of drivers screened positive for illegal drugs in their oral fluid and/or blood, 17.2% of whom were polydrug users (Lacey et al., 2009). In a similar study conducted in 2013–2014, the number of drivers who screened positive for any illegal drug increased to 15.1%, whereas the number of drivers screening positive for medications rose from 3.9% in 2007 to 4.9% in 2013–2014 (Berning et al., 2015; Kelley-Baker et al., 2017).
Prior laboratory-based research demonstrated that numerous individual substances have detrimental effects on driving performance. For example, marijuana impedes response time (Hart et al., 2010), coordination, and motor functioning (Lane et al., 2004), which may affect driving performance (Dubois et al., 2015). Cocaine users are two to three times more likely to be involved in automobile crashes than are those in the general public (Mann et al., 1993). The use of benzodiazepines doubles the risk of crash involvement (Barbone et al., 1998; LeRoy & Morse, 2008) and notably impairs cognitive and motor functioning necessary for adequate driving performance (Couper & Logan, 2004). Similarly, opioid use has been linked to impaired concentration, delayed reaction time, slowed information processing, and poorer visual acuity and has sedating effects (Dassanayake et al., 2011; Hetland & Carr, 2014; Leung, 2011; Meuleners et al., 2011; Nilsen et al., 2011). Prior research has also shown that drivers who use benzodiazepines, opioids, and antipsychotics make numerous errors on cognitive tests used to assess driving ability (Dassanayake et al., 2012). Further, drivers who test positive for opioids have been found to have a 30%–74% increased likelihood of making unsafe choices while driving, whereas drivers who test positive for cannabinoids have a 10% increase, and those who test positive for stimulants are twice as likely as those who do not to make poor choices while driving (Dubois et al., 2010). Finally, adults older than age 65 years are 10% more likely to be involved in a crash when they are taking antidepressants, and this risk is notably increased when antidepressants are combined with another substance—namely benzodiazepines (Rapoport et al., 2011; Sansone & Sansone, 2009).
Although the effects of individual drugs on cognitive ability and driving skills have been well documented in experimental studies, epidemiological studies examining the risk of crash involvement have yielded some contradictory results (Sewell et al., 2009). In this regard, our understanding of the impact of polydrug use on crashes is somewhat nebulous. Polydrug users are theorized to be at higher risk for crash involvement than single-drug users largely because of the potentially compounding effects of multiple substances (Midanik et al., 2007). Further, polydrug users are also more likely than non–polydrug users to consume alcohol (Scherer et al., 2013; Stinson et al., 2005), and alcohol has been shown to have substantial adverse effects on driving performance (Blomberg et al., 2009; Borkenstein et al., 1974; Compton & Berning, 2015; Voas et al., 2012; Zador et al., 2000). Despite the notable potential for crash involvement associated with polydrug use, much of the prior literature has simply lumped all polydrug users together (e.g., Hels et al., 2011; Lacey et al., 2009; Ramirez et al., 2016), thereby making the implicit assumption that they are comparable—or not worth differentiating. This suggests that research is needed into which polydrug users are at an increased risk for alcohol consumption and crash involvement. To begin to address this gap in the literature, recent efforts by this research team examined how polydrug users differ from one another on self-report measures of prior crash involvement and results from breath alcohol analysis (Scherer et al., 2015). Interestingly, we found that drivers who tested positive for both marijuana and cocaine were more likely than all other subgroups to have a positive breath alcohol concentration (BrAC) and were more likely to report driving after having had too much to drink, but no significant differences were found between subgroups on self-reported prior crash involvement. This research highlighted key differences among polydrug users on adverse outcomes. This means that the propensity of researchers to lump all polydrug users together may erroneously attribute the adverse outcomes of a specific polydrug user to all polydrug users (Scherer et al., 2015). Although informative, that research did not address whether different types of polydrug-using drivers (a) show different rates of alcohol consumption and (b) differ in their rates of crash involvement (among polydrug, single-drug, and non–drug users).
Method
Data for this study come from the Drug and Alcohol Crash Risk Study (DACRS) conducted by the National Highway Traffic Safety Administration in Virginia Beach, VA, from 2010 to 2011 (Compton & Berning, 2015). The DACRS is based on a rigorous design that sought a precise matching of crashes and controls similar in design to prior studies to estimate alcohol-related crash risk (Blomberg et al., 2005). The study screened a total of 12,790 drivers who were classified as either crash condition (n = 5,375) or noncrash control condition drivers (n = 7,415). Riding along with a police officer, research technician/phlebotomist teams responded to crashes 24 hours a day, 7 days a week over a 20-month period. To maximize comparability, 1 week after a driver involved in a crash provided data for the study, the police technician team returned to the same crash location to collect two control drivers on the same day of the week, at the same time of day, and going in the same direction of travel as the original crash. Crash participants provided consent, were surveyed, and provided biological samples (i.e., breath, oral fluid, and blood samples) at the site of the crash when it was deemed safe and possible. If crash participants were taken to the hospital or jail, study personnel obtained the consent of participants at the crash site and accompanied them to the secondary location to complete the survey and to collect samples. Control drivers were waved by police to a safe location as close to the crash site as possible where they gave consent and data were collected. Biological samples were collected and screened for the presence of alcohol and other drugs. The current study used participants in the DACRS who (a) were eligible for the parent study, (b) provided breath samples to measure alcohol use, and (c) provided an oral fluid and/or blood sample to measure drug use. Of the total sample, 10,512 participants provided an oral fluid and/or blood sample as well as a breath sample and were included in this study. Of those, 8,738 did not screen positive for any drug, 1,390 screened positive for only one drug, and 384 screened positive for multiple drugs.
To address the concern that the most problematic drivers would likely refuse participation, researchers attempted to examine those who refused by “converting” drivers who initially refused. In these cases, researchers offered an additional incentive of $100 for participation. This resulted in 156 participants who initially refused but then agreed to participate. Preliminary analysis conducted on these drivers showed that they did not differ meaningfully from the general population pool (Lacey et al., 2016), as their main motivation for refusing participation was a time restriction. As such, they were retained for analysis in the proposed study as well.
Biological matrices
Drug information was obtained via two biological matrices: oral fluid and blood. A total of 3,353 crash and 6,868 control drivers in the DACRS provided a valid oral fluid sample (Lacey et al., 2016). Another 291 drivers failed to provide an oral fluid sample but provided a blood sample from which drug information was also obtained, adding to the total of 10,512 drivers we included in this study. The analysis of the DACRS considered only triads of one crash and two control drivers, each with a valid drug result (Lacey et al, 2016). Because of the relatively small number of polydrug users in the file and to preserve statistical power, we relaxed the DACRS 1 crash:2 control design to include all drivers with a valid drug test result regardless of whether they satisfied the 1:2 design, resulting in a higher total sample size for the current study.
Measures
Outcome measures.
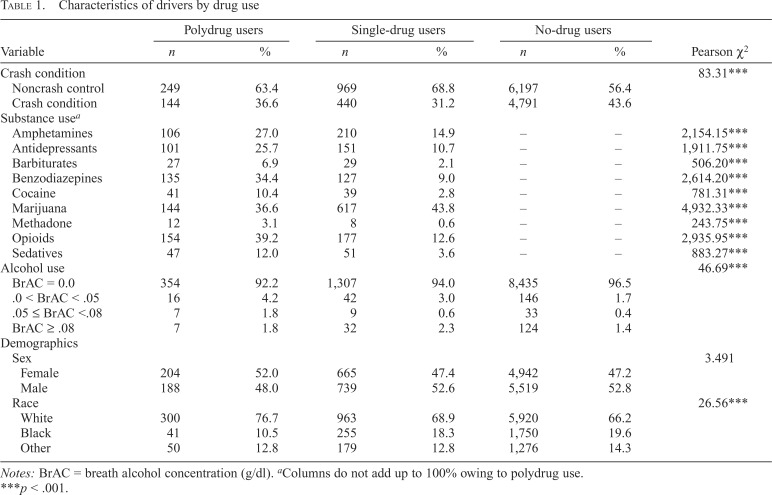
Classes of polydrug users were examined with regard to two outcome measures: alcohol consumption and crash involvement. Participants were asked to provide breath samples to estimate blood alcohol concentration. Alcohol consumption is measured as alcohol negative (BrAC = .00 g/dl) versus alcohol positive (BrAC > .00 g/dl). Crash involvement was identified by a dummy-coded variable denoting crash drivers (1) and control drivers (0). Rates of crash involvement and alcohol use among polydrug users, single-drug users, and non–drug users can be found in Table 1.
Table 1.
Characteristics of drivers by drug use
| Variable | Polydrug users |
Single-drug users |
No-drug users |
Pearson χ2 | |||
| n | % | n | % | n | % | ||
| Crash condition | 83.31*** | ||||||
| Noncrash control | 249 | 63.4 | 969 | 68.8 | 6,197 | 56.4 | |
| Crash condition | 144 | 36.6 | 440 | 31.2 | 4,791 | 43.6 | |
| Substance usea | |||||||
| Amphetamines | 106 | 27.0 | 210 | 14.9 | – | – | 2,154.15*** |
| Antidepressants | 101 | 25.7 | 151 | 10.7 | – | – | 1,911.75*** |
| Barbiturates | 27 | 6.9 | 29 | 2.1 | – | – | 506.20*** |
| Benzodiazepines | 135 | 34.4 | 127 | 9.0 | – | – | 2,614.20*** |
| Cocaine | 41 | 10.4 | 39 | 2.8 | – | – | 781.31*** |
| Marijuana | 144 | 36.6 | 617 | 43.8 | – | – | 4,932.33*** |
| Methadone | 12 | 3.1 | 8 | 0.6 | – | – | 243.75*** |
| Opioids | 154 | 39.2 | 177 | 12.6 | – | – | 2,935.95*** |
| Sedatives | 47 | 12.0 | 51 | 3.6 | – | – | 883.27*** |
| Alcohol use | 46.69*** | ||||||
| BrAC = 0.0 | 354 | 92.2 | 1,307 | 94.0 | 8,435 | 96.5 | |
| .0 < BrAC < .05 | 16 | 4.2 | 42 | 3.0 | 146 | 1.7 | |
| .05 ≤ BrAC <.08 | 7 | 1.8 | 9 | 0.6 | 33 | 0.4 | |
| BrAC ≥ .08 | 7 | 1.8 | 32 | 2.3 | 124 | 1.4 | |
| Demographics | |||||||
| Sex | 3.491 | ||||||
| Female | 204 | 52.0 | 665 | 47.4 | 4,942 | 47.2 | |
| Male | 188 | 48.0 | 739 | 52.6 | 5,519 | 52.8 | |
| Race | 26.56*** | ||||||
| White | 300 | 76.7 | 963 | 68.9 | 5,920 | 66.2 | |
| Black | 41 | 10.5 | 255 | 18.3 | 1,750 | 19.6 | |
| Other | 50 | 12.8 | 179 | 12.8 | 1,276 | 14.3 | |
Notes: BrAC = breath alcohol concentration (g/dl).
Columns do not add up to 100% owing to polydrug use.
p < .001.
Demographics.
Participants self-reported demographic information including age, sex, and race.
Time of day.
Researchers recorded the time of day when the data were collected (i.e., daytime or nighttime).
Substance use.
The oral fluid sampling system collected 1 ml of saliva for which consenting participants were remunerated an additional $10. Participants who also consented to provide 10 ml of blood for the study were remunerated an additional $50. Oral fluid and blood samples were forwarded to a laboratory for screening using enzyme-linked immunosorbent assays followed by verification of positive samples with mass spectral detection using liquid chromatography–mass spectrometry technology (Moore et al., 2007). Categories tested in the current study included amphetamines (i.e., amphetamine, 3,4-methylenedioxymethamphetamine [MDMA; Ecstasy], methamphetamine, and phentermine), antidepressants (i.e., fluoxetine, sertraline, citalopram, paroxetine, trazadone, venlafaxine, amitriptyline, nortriptyline, and doxepin), barbiturates (i.e., butalbital, phenobarbital), benzodiazepines (i.e., alprazolam, diazepam, lorazepam, temazepam, clonazepam, bromazepam, nordiazepam), cocaine, marijuana, methadone, opioids (i.e., codeine, morphine, hydrocodone, hydromorphone, oxycodone, buprenorphine, tramadol, and propoxyphene), and other sedatives (i.e., carisoprodol, meprobamate).
Statistical analyses
Latent class analysis (LCA) is a method of data reduction used to identify groupings of individuals that illustrate similar patterns or profiles of behavior (McCutcheon, 1987). LCA is commonly used in substance use research (Harrell et al., 2012; Scherer et al., 2015; Schwartz et al., 2010). Mplus 6.0 (Muthén & Muthén, 2010) was used for LCA modeling.
Based on commonly used software guidelines, we initially used 500 random starts to have high likelihood of obtaining global, rather than local, maxima. In the event the log likelihood was not replicated a minimum of five times, the number of starts was increased until this threshold was met (Muthén & Muthén, 2010). Multiple fit statistics are reported, including Bayesian Information Criterion (BIC; Schwarz, 1978), the Lo–Mendell–Rubin adjusted likelihood ratio test (LMR; Lo et al., 2001), and the parametric bootstrap likelihood ratio test (BLRT; MacLachlan & Peel, 2000). A lower BIC is generally preferred. The LMR and BLRT both evaluate the increase in model fit between the k − 1 and k class models (Nylund et al., 2007). In Monte Carlo simulations, the BLRT outperforms both the LMR and the BIC, but the LMR is more robust under a variety of model and distributional assumptions (Nylund et al., 2007). These fit statistics provide helpful guidelines for evaluating and choosing between models, but the choice of latent class solution was ultimately informed by substantive criteria involving the meaningfulness of the solution in terms of current drug use epidemiology (Petras & Masyn, 2010). Given established trends of reduced risk perception, findings in the literature, and increased use of marijuana and opioids, class solution selection was also guided by utility in evaluating and discriminating between classes relevant to marijuana and opioid use, for these substances are currently the focus of attention of researchers and policymakers.
Entropy is reported as well. Although not designed for use in class selection, entropy was used to assess the utility of the classes and the appropriateness of the use of Most Likely Latent Class Membership (MLLCM). Entropy ranges from 0 to 1, with higher scores representing better class separation (Celeux & Soromenho, 1996). MLLCM was used to export individual class membership to SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY). MLLCM can be an appropriate approach if entropy is high. A series of logistic regression analyses was conducted to determine differences between latent classes, BrAC levels, and crash involvement. All analyses controlled for race, sex, age, and time of day.
Latent class indicators
Latent classes were determined using the presence of substances as indicated by screening of oral fluid and/or blood samples. Because of the relatively high rates of alcohol use in the DACRS data set, it was omitted as a latent class indicator but retained as an outcome measure. Substance use (i.e., latent class indicators) and demographics are noted in Table 1.
Results
Class membership
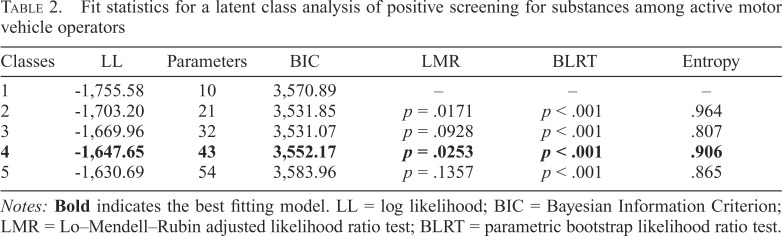
Table 2 demonstrates the overall fit statistics for substance use of various numbers of latent classes. Per the LMR adjusted likelihood ratio test—a test commonly used to identify strong-performing models—the two- and four-class models perform notably better than the one- and three-class models (p = .017 and .025, respectively). On further examination of the models, the two-class model had one class that consisted of individuals who had a high probability of using marijuana and very low probabilities of using any other substance (36.1%), whereas the second class consisted of drivers with relatively low probabilities of using all substances (63.9%). This class distribution did not allow us to adequately address the research questions and, as such, was not selected.
Table 2.
Fit statistics for a latent class analysis of positive screening for substances among active motor vehicle operators
| Classes | LL | Parameters | BIC | LMR | BLRT | Entropy |
| 1 | -1,755.58 | 10 | 3,570.89 | – | – | – |
| 2 | -1,703.20 | 21 | 3,531.85 | p = .0171 | p < .001 | .964 |
| 3 | -1,669.96 | 32 | 3,531.07 | p = .0928 | p < .001 | .807 |
| 4 | -1,647.65 | 43 | 3,552.17 | p = .0253 | p < .001 | .906 |
| 5 | -1,630.69 | 54 | 3,583.96 | p = .1357 | p < .001 | .865 |
Notes: Bold indicates the best fitting model. LL = log likelihood; BIC = Bayesian Information Criterion; LMR = Lo–Mendell–Rubin adjusted likelihood ratio test; BLRT = parametric bootstrap likelihood ratio test.
BIC supported a three-class model, but on further examination of the three- and four-class models, the fourclass model was deemed to yield more useful information, particularly with regard to marijuana and opioid use. The three-class model had a class in which individuals had a high probability of using marijuana (33.6%) and another in which individuals had a high probability of using opioids (33.1%), as well as a third class in which individuals had a high probability of using antidepressants (33.3%). Although marijuana and opioids were the substances of interest in the current endeavor, the four-class model yielded substantive differences. Specifically, the four-class model yielded two classes in which individuals had a high probability of using marijuana, allowing for discernment of polydrug use among marijuana users, as well as a class with a high propensity for opioid use. This, plus the results of the LMR adjusted likelihood ratio test, resulted in the selection of the four-class model for the current analyses. The five-class model did not perform significantly better than the four-class model (p =.136).
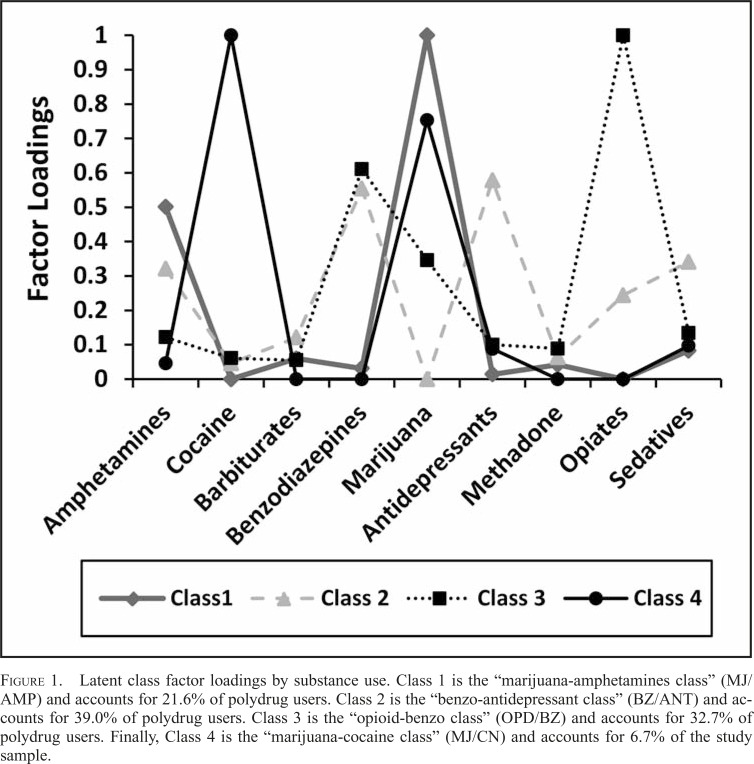
As noted in Figure 1, the first of the four classes displayed shows that 21.6% of the sample had a high propensity for the simultaneous use of marijuana and amphetamines. Thus, this class was labeled the marijuana-amphetamines class (MJ/AMP). Thirty-nine percent of the study sample fell into the second class, which consisted primarily of drivers who screened positive for both benzodiazepines and antidepressants. Accordingly, this class was labeled the benzoantidepressant class (BZ/ANT). Approximately a third of the sample (32.7%) had a high propensity for using opioids and benzodiazepines and was thus named the opioid-benzo class (OPD/BZ), whereas the remainder of the sample (6.7%) screened positive for primarily marijuana and cocaine and was thus named the marijuana-cocaine class (MJ/CN).
Figure 1.
Latent class factor loadings by substance use. Class 1 is the “marijuana-amphetamines class” (MJ/AMP) and accounts for 21.6% of polydrug users. Class 2 is the “benzo-antidepressant class” (BZ/ANT) and accounts for 39.0% of polydrug users. Class 3 is the “opioid-benzo class” (OPD/BZ) and accounts for 32.7% of polydrug users. Finally, Class 4 is the “marijuana-cocaine class” (MJ/CN) and accounts for 6.7% of the study sample.
Polydrug classes and alcohol consumption
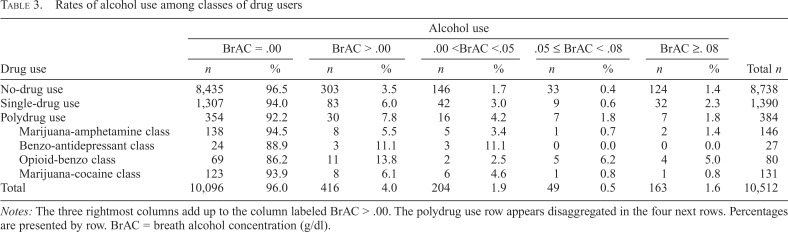
Table 3 shows the associations between latent class membership and levels of alcohol use. Of the 10,512 drivers in the sample, 416 (4%) were alcohol positive. Because of problems with small sample sizes after stratification of BrAC-positive drivers, we conducted analyses only to determine the adjusted odds ratios (aORs) of having a positive BrAC (i.e., BrAC > .0 g/dl) instead of examining various levels of BrAC. There are similar distributions of alcohol use among non–drug users, single-drug users, and all classes apart from the OPD/BZ class, which demonstrated notably higher levels of alcohol use at the .05 and .08 g/dl levels.
Table 3.
Rates of alcohol use among classes of drug users
| Drug use | Alcohol use |
|||||||||||||
| BrAC = .00 |
BrAC > .00 |
.00 <BrAC <.05 |
.05 ≤ BrAC < .08 |
BrAC ≥. 08 |
||||||||||
| n | % |
n | % | n | % |
n | % |
n |
% | Total n | ||||
| No-drug use | 8,435 |
96.5 | 303 | 3.5 | 146 | 1.7 | 33 |
0.4 |
124 | 1.4 | 8,738 | |||
| Single-drug use | 1,307 |
94.0 | 83 | 6.0 | 42 | 3.0 | 9 |
0.6 |
32 | 2.3 | 1,390 | |||
| Polydrug use | 354 |
92.2 | 30 | 7.8 | 16 | 4.2 | 7 |
1.8 |
7 | 1.8 | 384 | |||
| Marijuana-amphetamine class | 138 |
94.5 | 8 | 5.5 | 5 | 3.4 | 1 |
0.7 |
2 | 1.4 | 146 | |||
| Benzo-antidepressant class | 24 |
88.9 | 3 | 11.1 | 3 | 11.1 | 0 |
0.0 |
0 | 0.0 | 27 | |||
| Opioid-benzo class | 69 |
86.2 | 11 | 13.8 | 2 | 2.5 | 5 |
6.2 |
4 | 5.0 | 80 | |||
| Marijuana-cocaine class | 123 |
93.9 | 8 | 6.1 | 6 | 4.6 | 1 |
0.8 |
1 | 0.8 | 131 | |||
| Total | 10,096 |
96.0 | 416 | 4.0 | 204 | 1.9 | 49 |
0.5 |
163 | 1.6 | 10,512 | |||
Notes: The three rightmost columns add up to the column labeled BrAC > .00. The polydrug use row appears disaggregated in the four next rows. Percentages are presented by row. BrAC = breath alcohol concentration (g/dl).
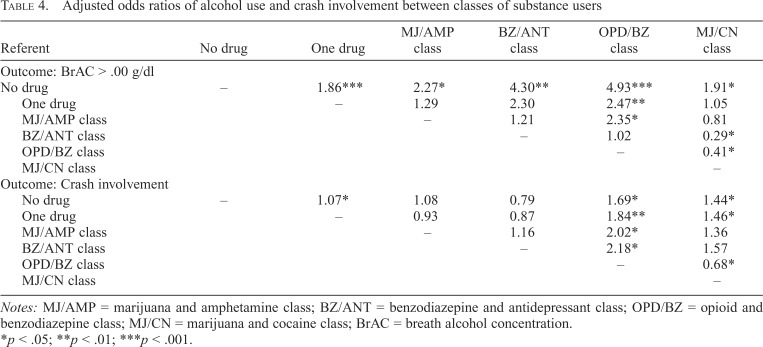
Single-drug users and all classes of polydrug users were significantly more likely than non–drug users to have a positive BrAC. Drivers who were positive for only one drug, as well as the MJ/CN class, were almost twice as likely as non–drug users to have a positive BrAC (aOR = 1.86, p < .001 and aOR = 1.91, p < .05, respectively), the MJ/AMP class was more than twice as likely as the non–drug users to be BrAC positive (aOR = 2.27, p < .05), and drivers in the BZ/ANT and OPD/BZ classes were more than four times more likely to have a positive BrAC (aOR = 4.30, p < .001 and aOR = 4.93, p < .05, respectively). The OPD/BZ class was also more than twice as likely as the MJ/AMP and BZ/ANT classes to have a positive BrAC (aOR = 2.47, p < .01 and aOR = 2.35, p < .05, respectively), although not significantly different from the BZ/ANT class. Also of note is that the MJ/CN class was less than half as likely to have a positive BrAC as the BZ/ANT and OPD/BZ classes of polydrug users (aOR = 0.29, p < .05 and aOR = 0.41, p < .05, respectively).
Polydrug classes and crash involvement
Table 4 shows the association between classes of substance users and crash involvement. In terms of crash involvement, single-drug users were 7% more likely to be involved in a crash than were non–drug users (aOR = 1.07, p < .05). Interestingly, of the polydrug classes, only the OPD/BZ and MJ/CN classes were significantly more likely to be involved in a crash than were the non–drug users (aOR = 1.69, p < .05 and aOR = 1.44, p < .05, respectively). The MJ/AMP and BZ/ANT classes were not significantly different from the non–drug users in terms of crash involvement. Similarly, the OPD/BZ and MJ/CN were significantly more likely to be involved in a crash than were single-drug users (aOR = 1.84, p < .01, and aOR = 1.46, p < .05, respectively), whereas the MJ/AMP and BZ/ANT classes showed no significant difference from the single-drug users. Of note, the OPD/BZ class was significantly more likely than all other classes to be involved in a crash.
Table 4.
Adjusted odds ratios of alcohol use and crash involvement between classes of substance users
| MJ/AMP | BZ/ANT | OPD/BZ | MJ/CN | |||
| Referent | No drug | One drug | class | class | class | class |
| Outcome: BrAC > .00 g/dl | ||||||
| No drug | – | 1.86*** | 2.27* | 4.30** | 4.93*** | 1.91* |
| One drug | . – | 1.29 | 2.30 | 2.47** | 1.05 | |
| MJ/AMP class | .– | 1.21 | 2.35* | 0.81 | ||
| BZ/ANT class | .– | 1.02 | 0.29* | |||
| OPD/BZ class | .– | 0.41* | ||||
| MJ/CN class | .– | |||||
| Outcome: Crash involvement | ||||||
| No drug | – | 1.07* | 1.08 | 0.79 | 1.69* | 1.44* |
| One drug | . – | 0.93 | 0.87 | 1.84** | 1.46* | |
| MJ/AMP class | .– | 1.16 | 2.02* | 1.36 | ||
| BZ/ANT class | .– | 2.18* | 1.57 | |||
| OPD/BZ class | .– | 0.68* | ||||
| MJ/CN class | .– |
Notes: MJ/AMP = marijuana and amphetamine class; BZ/ANT = benzodiazepine and antidepressant class; OPD/BZ = opioid and benzodiazepine class; MJ/CN = marijuana and cocaine class; BrAC = breath alcohol concentration.
p < .05; **p < .01; ***p < .001.
Discussion
The goal of the current research is to expand on our prior study by examining how groups of polydrug users differ from one another and single-drug-using or non–drugusing drivers in terms of alcohol consumption and crash involvement.
Alcohol consumption
Previously, we found that drivers who used both marijuana and cocaine were about seven times more likely than other classes to have a positive BrAC (Scherer et al., 2015). The current research found similar trends in that the MJ/CN class of polydrug-using drivers were almost twice as likely as non–drug users to be alcohol positive, although not significantly different from single-drug users. Interestingly, the BZ/ANT and OPD/BZ classes were significantly more likely than any other class of polydrug users, single-drug users, or non–drug users to have a positive BrAC at the time of this study. This is consistent with prior findings in the literature showing that polydrug users are more likely than non–polydrug users to consume alcohol (e.g., Althobaiti & Sari, 2016; Jones et al., 2001; O’Grady et al., 2008; Stinson et al., 2005). Interestingly, among the BZ/ANT drivers who were BrAC positive, none had a BrAC above the legal limit. Among OPD/BZ drivers, however, about a third of drivers with a positive BrAC were over the legal limit. As such, although both BZ/ANT and OPD/BZ polydrug users were significantly more likely than any other group to have a positive BrAC, only the OPD/BZ group had a BrAC above the legal limit. Although any concurrent alcohol and drug use is concerning, those concerns could only be compounded if the alcohol use is itself impairing.
Crash involvement
Further, the difference in drinking and driving associated with drug classes did not straightforwardly translate into crash involvement. Only some of the classes that were found to be associated with drinking and driving were also associated with crash involvement (OPD/BZ and MJ/CN). Although the BZ/ANT and MJ/CN classes were about 70%–85% and 44%–46% more likely to be involved in a crash compared with either non–drug users or single-drug users, respectively, no association with crash involvement was found among MJ/AMP and BZ/ANT drivers. An intriguing finding is that benzodiazepines are part of the two polydrug classes closely associated with drinking and driving (BZ/ANT and OPD/BZ), but only OPD/BZ drivers were associated with crash involvement, suggesting that the presence of opioids may play a role in such associations.
This finding is consistent with prior laboratory-based research that found drivers who use both opioids and benzodiazepines make significant errors in cognitive tests linked to driving ability (Dassanayake et al., 2012). This may be because of the cumulative sedative effect found in both opioids and benzodiazepines. The use of these drugs may also have the additional side effects of balance loss, dizziness, and distorted vision—all of which may further impair driving performance. This has been particularly noted with the use of anxiolytic benzodiazepines such as alprazolam (Barbone et al., 1998), which accounted for nearly half of the benzodiazepine use in the current sample. Crash risk may be compounded when benzodiazepines are combined with opioids, which may contribute to fatigue, lightheadedness, and difficulty with visual tracking and which alone have been found to notably increase crash involvement (Leroy & Morse, 2008; Meuleners et al., 2011).
In the current study, the MJ/CN class was more than 40% more likely to be involved in a crash compared with either non–drug users or single-drug users. This appears to be contrary to findings in our prior research, which found no difference in classes based on prior crash involvement (Scherer et al., 2015). This difference is likely methodological. First, although the current study examines involvement in actual crashes, our previous study used self-reported prior crash involvement, which may be subject to underreporting, particularly in drivers who screened positively for one or more drugs. Further, the prior study was based on the 2007 National Roadside Survey (Lacey et al., 2009). As crash involvement in the entire driving population is relatively small, the likelihood of finding someone in the National Roadside Survey who was involved in a crash is reduced. In the current study, however, we looked specifically at drivers involved in crashes. This both eliminated self-report biases and focused on actual crashes, which allowed for a more meaningful interpretation.
Interestingly, there was no significant difference between the MJ/AMP class and the BZ/ANT class drivers and singledrug users or non–drug users in terms of crash involvement. Although the reason for this is unclear at this time, this finding emphasizes the need to avoid assuming that all polydrug-using drivers present a similar crash risk, since not all polydrug users are more likely than non–drug users to be involved in a crash.
Limitations of current study
The current endeavor has several limitations that must be taken into consideration for proper interpretation of the results. First, the crash risk estimates were pulled from a sample of drivers in Virginia Beach. Thus, the findings may not be fully applicable to locations with varied laws and/or environmental/demographic conditions. Nevertheless, the findings of the current study represent an important step forward in our understanding of how polydrug use may affect alcohol consumption and crash involvement. In addition, the current study simply examined the presence of a substance, not whether the substance existed in sufficient quantity to cause driving impairment. Including established thresholds for impairment for each substance screened would be a more precise indicator of crash risk and would yield more useful information than simply examining the presence of a substance. However, the current research incorporated 35 substances, each with different ranges and levels of impairment. In some cases, the level of impairment is augmented by other substance use. As the focus of this research was to examine substance combinations and their relationship to crash involvement, such a detailed undertaking was deemed beyond the scope of the current study. With the current study as a foundation, future research can incorporate such information to provide a richer understanding of how substance quantity in polydrug users differs among individuals, non–drug users, and single-drug users and how this may predict crash involvement.
Finally, the current study used a cross-sectional design. Such studies are appropriate for informing future research, enhancing awareness of an issue, and promoting scientific understanding of a topic, which was the goal of the current endeavor. However, this also means that the results of the current study cannot be used for making causal inferences, for which additional research is warranted.
Despite these limitations, the use of the DACRS and the analytic approach provide several vital strengths that warrant notation. First and foremost, this is the first study of its kind. To the best of our knowledge, no other study has been conducted to delineate classes of polydrug users and their relationship to actual crash involvement. Similarly, unlike much of the prior literature, the current study did not have to rely on self-report data to gather information on drug use or alcohol level and crash involvement and was not restricted to conducting laboratory-based research to test cognitive abilities associated with driving performance. Instead, we used actual crash data and biological measurement, which allowed us to accurately identify both our latent classes and our outcomes. Gaining a clearer understanding of the notably varying roles within polydrug-using groups will allow researchers, clinicians, and policymakers to identify the most at-risk individuals within polydrug-using groups for more targeted interventions.
Further, although additional research is certainly warranted, the current study also provides evidence that interventions designed to curtail drugged driving should pay additional attention to substance combinations. This research shows that although some polydrug users are at significantly higher risk of crash involvement than non–drug users, other combinations are not. This may also save time and costs for police, who can focus laboratory screenings on higher risk substance combinations rather than expend limited resources looking for substance combinations that do not elevate crash risk.
Conclusion
In terms of driving performance and alcohol consumption, there are critical differences in the classes of polydrug users. Drivers who used both opioids and benzodiazepines are at greater risk for both crash involvement and drinking and driving. The trend in research to simply lump all polydrug users together may be attempting to combine groups that are significantly different in terms of crash involvement and substance use. This could mean the increased crash risk demonstrated in prior research for drivers using more than one drug (e.g., Hels et al., 2011; Lacey et al., 2009; Ramirez et al., 2016) may be conflating the effect of opioid and benzodiazepine polydrug users and crashes with all other polydrug users, which—in some cases—may not be significantly different from non–drug and/or single-drug users in terms of crash involvement.
Footnotes
The Drug and Alcohol Crash Risk Study, which provided the data for this endeavor, was funded by the National Highway Traffic Safety Administration (Grant DOT HS 812 355) and by the National Institute on Alcohol Abuse and Alcoholism (Grant R01 AA018352-02S1).
References
- Althobaiti Y. S., Sari Y. Alcohol interactions with psychostimulants: An overview of animal and human studies. Journal of Addiction Research & Therapy. 2016;7:281. doi: 10.4172/2155-6105.1000281. doi:10.4172/2155-6105.1000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbone F., McMahon A. D., Davey P. G., Morris A. D., Reid I. C., McDevitt D. G., MacDonald T. M. Association of roadtraffic accidents with benzodiazepine use. The Lancet. 1998;352:1331–1336. doi: 10.1016/s0140-6736(98)04087-2. doi:10.1016/S0140-6736(98)04087-2. [DOI] [PubMed] [Google Scholar]
- Berning A., Compton R., Wochinger K. Washington, DC: National Highway Traffic Safety Administration; 2015. Results of the 2013–2014 National Roadside Survey of Alcohol and Drug Use by Drivers (Traffic Safety Facts Research Note DOT HS 812 118) [Google Scholar]
- Blomberg R. D., Peck R. C., Moskowitz H., Burns M., Fiorentino D. Stamford, CT: Dunlap & Associates, Inc; 2005. Crash risk of alcohol involved driving: A case-control study. [Google Scholar]
- Blomberg R. D., Peck R. C., Moskowitz H., Burns M., Fiorentino D. The Long Beach/Fort Lauderdale relative risk study. Journal of Safety Research. 2009;40:285–292. doi: 10.1016/j.jsr.2009.07.002. doi:10.1016/j.jsr.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Borkenstein R. F., Crowther R. F., Shumate R. P., Ziel W. B., Zylman R. Bloomington, IN: Indiana University; 1974. The role of the drinking driver in traffic accidents (The Grand Rapids Study) [Google Scholar]
- Celeux G., Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13:195–212. [Google Scholar]
- Compton R. P., Berning A. Washington, DC: National Highway Traffic Safety Administration; 2015. Drug and alcohol crash risk (Traffic Safety Facts Research Note DOT HS 812 117) [Google Scholar]
- Couper F. J., Logan B. K. Washington, DC: National Highway Traffic Safety Administration; 2004. Drugs and human performance fact sheets (Report No. HS 809 725) [Google Scholar]
- Dassanayake T., Michie P., Carter G., Jones A. Effects of benzodiazepines, antidepressants and opioids on driving: A systematic review and meta-analysis of epidemiological and experimental evidence. Drug Safety. 2011;34:125–156. doi: 10.2165/11539050-000000000-00000. doi:10.2165/11539050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Dassanayake T. L., Michie P. T., Jones A. L., Mallard T., Whyte I. M., Carter G. L. Cognitive skills underlying driving in patients discharged following self-poisoning with central nervous system depressant drugs. Traffic Injury Prevention. 2012;13:450–457. doi: 10.1080/15389588.2012.671983. doi:10.1080/15389588.2012.671983. [DOI] [PubMed] [Google Scholar]
- Dubois S., Bédard M., Weaver B. The association between opioid analgesics and unsafe driving actions preceding fatal crashes. Accident Analysis and Prevention. 2010;42:30–37. doi: 10.1016/j.aap.2009.06.030. doi:10.1016/j.aap.2009.06.030. [DOI] [PubMed] [Google Scholar]
- Dubois S., Mullen N., Weaver B., Bédard M. The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forensic Science International. 2015;248:94–100. doi: 10.1016/j.forsciint.2014.12.018. doi:10.1016/j.forsciint.2014.12.018. [DOI] [PubMed] [Google Scholar]
- Harrell P. T., Mancha B. E., Petras H., Trenz R. C., Latimer W. W. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug and Alcohol Dependence. 2012;122:220–227. doi: 10.1016/j.drugalcdep.2011.10.001. doi:10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart C. L., Ilan A. B., Gevins A., Gunderson E. W., Role K., Colley J., Foltin R. W. Neurophysiological and cognitive effects of smoked marijuana in frequent users. Pharmacology, Biochemistry, and Behavior. 2010;96:333–341. doi: 10.1016/j.pbb.2010.06.003. doi:10.1016/j.pbb.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hels T., Bernhoft I. M., Lyckegaard A., Houwing S., Hagenzieker M., Legrand S-A., Verstraete A. Risk of injury by driving with alcohol and other drugs. 2011 (Project No. TREN-05-FP6TR-S07.61320-518404-DRUID) [Google Scholar]
- Hetland A., Carr D. B. Medications and impaired driving. Annals of Pharmacotherapy. 2014;48:494–506. doi: 10.1177/1060028014520882. doi:10.1177/1060028014520882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S. E., Oeltmann J., Wilson T. W., Brener N. D., Hill C. V. Binge drinking among undergraduate college students in the United States: Implications for other substance use. Journal of American College Health. 2001;50:33–38. doi: 10.1080/07448480109595709. doi:10.1080/07448480109595709. [DOI] [PubMed] [Google Scholar]
- Kelley-Baker T., Berning A., Ramirez A., Lacey J. H., Carr K., Waehrer G., Compton R. Washington, DC: National Highway Traffic Safety Administration; 2017. 2013–2014 National Roadside Study of Alcohol and Drug Use by Drivers: Drug results (Report No. DOT HS 812 411) [Google Scholar]
- Lacey J. H., Kelley-Baker T., Berning A., Romano E., Ramirez A., Yao J., Compton R. Washington, DC: National Highway Traffic Safety Administration; 2016. Drug and alcohol crash risk: A case-control study (Report No. DOT HS 812 355) [Google Scholar]
- Lacey J. H., Kelley-Baker T., Furr-Holden D., Voas R. B., Moore C., Brainard K., Berning A. Washington, DC: National Highway Traffic Safety Administration; 2009. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Methodology (Report No. DOT HS 811 237) Retrieved from https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/811237.pdf. [Google Scholar]
- Lane S. D., Cherek D. R., Pietras C. J., Tcheremissine O. V. Acute marijuana effects on response-reinforcer relations under multiple variable-interval schedules. Behavioural Pharmacology. 2004;15:305–309. doi: 10.1097/01.fbp.0000135003.80318.97. doi:10.1097/01.fbp.0000135003.80318.97. [DOI] [PubMed] [Google Scholar]
- LeRoy A. A., Morse M. L. Washington, DC: National Highway Traffic Safety Administration; 2008. Multiple medications and vehicle crashes: Analysis of databases (Report No. DOT HS 810 858) [Google Scholar]
- Leung S. Y. Benzodiazepines, opioids and driving: An overview of the experimental research. Drug and Alcohol Review. 2011;30:281–286. doi: 10.1111/j.1465-3362.2011.00311.x. doi:10.1111/j.1465-3362.2011.00311.x. [DOI] [PubMed] [Google Scholar]
- Lo Y., Mendell N. R., Rubin D. B. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. doi:10.1093/biomet/88.3.767. [Google Scholar]
- MacLachlan G., Peel D. New York, NY: John Wiley and Sons; 2000. Finite mixture models: Wiley series in probability and statistics. [Google Scholar]
- Mann R. E., Anglin L., Vingilis E. R., Larkin E. Self-reported driving risks in a clinical sample of substance users. Utzelmann Berghous, Kroj, editors. Alcohol, drugs and traffic safety. 1993:860–865. Cologne, Germany: TUeV Rheinland. Retrieved from http://www.icadtsinternational.com/files/documents/1992_111.pdf. [Google Scholar]
- McCutcheon A. L. Thousand Oaks, CA: Sage; 1987. Latent class analysis. [Google Scholar]
- Meuleners L. B., Duke J., Lee A. H., Palamara P., Hildebrand J., Ng J. Q. Psychoactive medications and crash involvement requiring hospitalization for older drivers: A population-based study. Journal of the American Geriatrics Society. 2011;59:1575–1580. doi: 10.1111/j.1532-5415.2011.03561.x. doi:10.1111/j.1532-5415.2011.03561.x. [DOI] [PubMed] [Google Scholar]
- Midanik L. T., Tam T. W., Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence. 2007;90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024. doi:10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore C., Coulter C., Crompton K., Zumwalt M. Determination of benzodiazepines in oral fluid using LC/MS/MS. Journal of Analytical Toxicology. 2007;31:596–600. doi: 10.1093/jat/31.9.596. doi:10.1093/jat/31.9.596. [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. 6th ed. Los Angeles, CA: Authors; 2010. Mplus user’s guide. [Google Scholar]
- Nilsen H. K., Landrø N. I., Kaasa S., Jenssen G. D., Fayers P., Borchgrevink P. C. Driving functions in a video simulator in chronic non-malignant pain patients using and not using codeine. European Journal of Pain. 2011;15:409–415. doi: 10.1016/j.ejpain.2010.09.008. doi:10.1016/j.ejpain.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Nylund K. L., Asparouhov T., Muthén B. O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. doi:10.1080/10705510701575396. [Google Scholar]
- O’Grady K. E., Arria A. M., Fitzelle D. M. B., Wish E. D. Heavy drinking and polydrug use among college students. Journal of Drug Issues. 2008;38:445–465. doi: 10.1177/002204260803800204. doi:10.1177/002204260803800204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petras H., Masyn K. General growth mixture analysis with antecedents and consequences of change. In: Piquero A. R., Weisburd D., editors. Handbook of quantitative criminology. New York, NY: Springer; 2010. pp. 69–100. [Google Scholar]
- Ramirez A., Berning A., Carr K., Scherer M., Lacey J. H., Kelley-Baker T., Fisher D. A. Washington, DC: National Highway Traffic Safety Administration; 2016. Marijuana, other drugs, and alcohol use by drivers in Washington State (Report No. DOT HS 812 299) [Google Scholar]
- Rapoport M. J., Zagorski B., Seitz D., Herrmann N., Molnar F., Redelmeier D. A. At-fault motor vehicle crash risk in elderly patients treated with antidepressants. American Journal of Geriatric Psychiatry. 2011;19:998–1006. doi: 10.1097/JGP.0b013e31820d93f9. doi:10.1097/JGP.0b013e31820d93f9. [DOI] [PubMed] [Google Scholar]
- Sansone R. A., Sansone L. A. Driving on antidepressants: Cruising for a crash? Psychiatry. 2009;6:13–16. [PMC free article] [PubMed] [Google Scholar]
- Scherer M., Harrell P., Romano E. Marijuana and other substance use among motor vehicle operators: A latent class analysis. Journal of Studies on Alcohol and Drugs. 2015;76:916–923. doi: 10.15288/jsad.2015.76.916. doi:10.15288/jsad.2015.76.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer M., Voas R. B., Furr-Holden D. Marijuana as a predictor of concurrent substance use among motor vehicle operators. Journal of Psychoactive Drugs. 2013;45:211–217. doi: 10.1080/02791072.2013.804230. doi:10.1080/02791072.2013.804230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz B., Wetzler S., Swanson A., Sung S. C. Subtyping of substance use disorders in a high-risk welfare-to-work sample: A latent class analysis. Journal of Substance Abuse Treatment. 2010;38:366–374. doi: 10.1016/j.jsat.2010.03.001. doi:10.1016/j.jsat.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. doi:10.1214/aos/1176344136. [Google Scholar]
- Sewell R. A., Poling J., Sofuoglu M. The effect of cannabis compared with alcohol on driving. American Journal on Addictions. 2009;18:185–193. doi: 10.1080/10550490902786934. doi:10.1080/10550490902786934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson F. S., Grant B. F., Dawson D. A., Ruan W. J., Huang B., Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2005;80:105–116. doi: 10.1016/j.drugalcdep.2005.03.009. doi:10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Voas R. B., Torres P., Romano E., Lacey J. H. Alcohol-related risk of driver fatalities: An update using 2007 data. Journal of Studies on Alcohol and Drugs. 2012;73:341–350. doi: 10.15288/jsad.2012.73.341. doi:10.15288/jsad.2012.73.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zador P. L., Krawchuk S. A., Voas R. B. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. Journal of Studies on Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. doi:10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]