Abstract
Purpose
To understand the experience of adolescent systemic juvenile idiopathic arthritis (SJIA) patients and those of their parents based on their social media posts.
Methods
English language posts related to SJIA, Still’s disease, or juvenile arthritis were collected and analyzed.
Results
In total, 71 posts created between 2009 and 2015 on 15 websites were identified in November 2015. Of the 32 unique authors, 17 were SJIA patients aged 13–20 years (40 posts), 7 were mothers of SJIA patients (12 posts), and 8 patients had unspecified forms of juvenile arthritis (19 posts). Many patients posted about similar diagnostic experiences marked by 5 phases: 1) early prediagnosis: pain and fatigue overlooked until crisis occurred, 2) first misdiagnosis: doctors talked about “growing pains” and psychosocial problems (“fake pains” to avoid school), 3) second misdiagnosis: severity acknowledged, but diagnosed as leukemia or another cancer, 4) tests: tests leading to diagnosis and treatment conducted, and 5) cognitive identity: patient accepted the diagnosis and its implications. Many adolescent patients, looking back at disease onset in their childhood, described themselves as a “sleeping child” rather than the typical active child. Several patients tried to hide their illness from friends, but expressed concerns openly online. Many patients described SJIA as a powerful external enemy, using terms like “bulldozer,” “dragon,” and “monster.” Many posts from patients and their mothers used superhero language/imagery to help “fight” SJIA. Some patients also posted about the risk of death.
Conclusion
Although most adolescent SJIA patients openly posted about the difficulties of their disease online, they made efforts to hide their disease in the real world. They frequently used superhero words and images in describing their fight for better health. Physicians can use these insights when counseling SJIA patients to provide a narrative that meshes with the patients’ worldview and perhaps to improve physician–patient communication to increase treatment adherence.
Keywords: adolescents, juvenile arthritis, SJIA, social media, Still’s disease, superheroes
Introduction
Systemic juvenile idiopathic arthritis (SJIA), also known as Still’s disease, is a rare autoinflammatory form of chronic arthritis in pediatric patients, characterized by spiking fever, skin rash, arthralgia or arthritis, myalgia, hepatosplenomegaly, lymphadenopathy, and serositis.1,2 SJIA represents 4%–17% of all juvenile idiopathic arthritis (JIA) cases worldwide,2 and accounts for 5%–10% of all JIA cases in the USA and Europe.1,3,4 It affects the health-related quality of life of patients, impacts functioning in school and at home, and imposes a significant social and economic burden on patients and their families.5–7
To minimize the impact of SJIA on the physical and psychosocial development of patients, it is essential to know patients’ perspectives about the disease and associated factors. Social media posts from patients and their caregivers are helpful in obtaining important real-world patient-focused information related to patient needs and the disease burden on their lives. Understanding how patients and caregivers process this information could facilitate better understanding by health care professionals of the patients’ conditions to better assess treatment effectiveness and help counsel appropriately.8
Prior work has identified social media posting behaviors of parents of children with potential SJIA, as well as of parents of diagnosed children, in the time periods before and after SJIA diagnosis, showing the impact of the disease journey on the families.9 The objective of this study was to understand the experience of adolescent SJIA patients and those of their parents evident from their own social media posts.
Methods
In this study, posts that indicated a direct reference to the disease (SJIA/Still’s disease or juvenile arthritis [JA]) and posted by adolescent patients were collected and manually analyzed by a linguistic analysis team (Treato, Princeton, NJ, USA). In addition, posts from caregivers talking about childhood or adolescent experiences of patients with SJIA were collected and analyzed. The dataset was obtained from existing publicly available sites and posts (i.e., posts viewable by all and not requiring a password to access) and was limited to English-language public social media (Facebook, Instagram, Tumblr, and Twitter). The majority of the posts were collected from the USA; however, some posts were also collected from the UK and Canada owing to similarities in disease experience.
Tools from sociolinguistics (mainly praxematics) and semiotics were applied to both word posts and visual posts (i.e., posts using memes, gifs, and pictures) to understand the cognitive relationship between young patients and their disease. Evaluation of semantic networks, rhetoric supports (metaphors, symbols, and ellipses), and recurrence of representational schemes (concepts, representations, and stereotypes) allowed for an understanding of the patients’ socio-cognitive patterns in relation to their disease. No ethical approval or informed consent was obtained as the posts were retrieved from public, open-access websites.
Results
In total, 71 posts created between 2009 and 2015 on 15 websites were reviewed in November 2015. Of the 24 unique authors identified, 17 were SJIA patients (40 posts) and 7 were mothers of SJIA patients (12 posts; Table 1). Moreover, there were 8 unique JA patients (19 posts; using the term JA, JIA, or juvenile rheumatoid arthritis without mentioning SJIA) included in the analysis to compare the specific mention of SJIA with these less-specific posts. Patients whose posts were included were between 13 and 20 years of age, as determined from patient/caregiver declarations in the posts. Some posts were included because the patients talked about their past school and teenage years, although they did not reveal their current age; however, the subtext and context showed that they were in their mid-20s when they posted them (Table 2).
Table 1.
Number of posts by patients and mothers on public social media sites
| Diseases | Number of patients/caregivers | Message countsa |
|---|---|---|
| SJIA | 17 | 40 |
| SJIA (mothers speaking about their kids with SJIA, reporting a child’s perspective) | 7 | 12 |
| JA without SJIA (terms used included JRA, JIA, and JA) | 8 | 19 |
Notes:
Focus was on posts from the USA; however, some posts were from non-US sites (UK and Canada) and were retained because of their value (ie, similarity of disease experience) and a relatively limited number of posts by adolescents
Abbreviations: JA, juvenile arthritis; JIA, juvenile idiopathic arthritis; JRA, juvenile rheumatoid arthritis; SJIA, systemic juvenile idiopathic arthritis.
Table 2.
Number of posts by adolescent patients
| Age of patients (years) | Number of SJIA posts/messagesa | Number of JA/JIA posts/messages (with no mention of SJIA)a |
|---|---|---|
| 13 | 1 | 6 |
| 14 | 1 | 1 |
| 17 | 8 | 0 |
| 19 | 1 | 6 |
| 20 | 6 | 0 |
| Those who talked about school and teenage without revealing their age | 11 | 4 |
| Young adults/graduate students who talked about their past | 12 | 2 |
| Total number of posts by adolescents/about teenage years | 40 | 19 |
Notes:
Focus was on posts from the USA; however, some posts were from non-US sites (UK and Canada) and were retained because of their value (ie, similarity in disease experience) and a relatively limited number of posts by adolescents. Bold text represent total number of posts by teenagers.
Abbreviations: JA, juvenile arthritis; JIA, juvenile idiopathic arthritis; SJIA, systemic juvenile idiopathic arthritis.
Patients’ experiences with SJIA
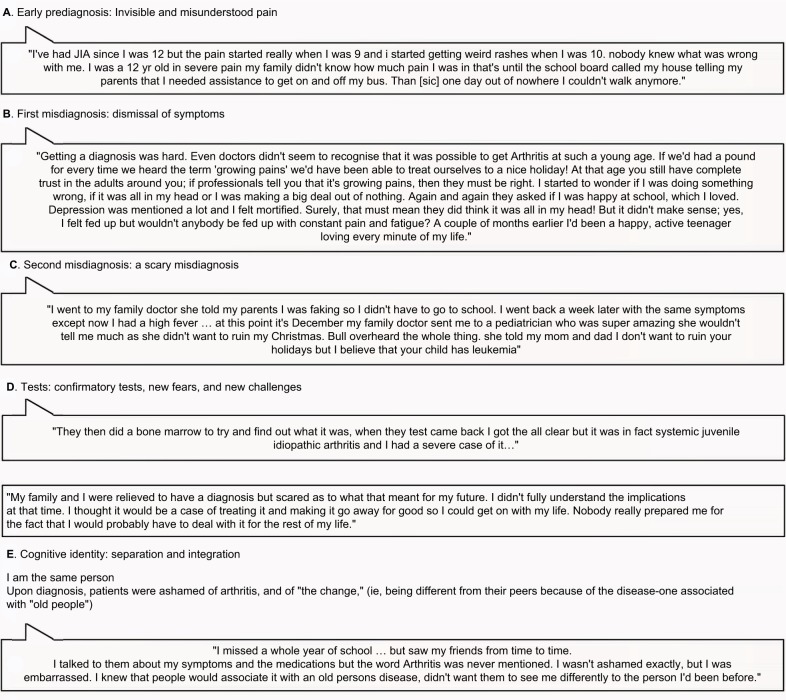
Our analysis of social media posts from SJIA patients revealed 5 diagnosis-related phases: early prediagnosis, first misdiagnosis, second misdiagnosis, tests, and cognitive identity (Figure 1). These phases, which surfaced in several patients’ posts, are similar to the phases identified in the preceding SJIA social media study with younger patients.9 Each phase was characterized by certain language behaviors that demonstrated the journey of their emotional experience. Many posts described experiences of children falling ill during the early prediagnosis phase, with no knowledge regarding the cause of pain and intense fatigue. Several adolescent patients, while looking back at the onset of the disease when they were children, described themselves as a “sleeping child” rather than a typical active, playful child (Figure 1A). The same posts described how no family member takes action until the patient’s body “stops working,” and the patient was incapable of going to school or even getting out of bed. In addition, most doctors initially misdiagnosed SJIA as “growing pains” or infection. One child posted that all the doctors she initially visited did not diagnose arthritis from her symptoms and instead used the words “growing pains” or questioned her willingness to go to school or her mental state (Figure 1B). Patients stated that as time passed without diagnosis and the illness worsened over time, parents finally took the child to a specialist during the late prediagnosis phase. However, doctors often misdiagnosed it again (Figure 1C), and the second misdiagnosis would be scarier than the first; in general, leukemia or another cancer was suspected. Patients mentioned that they and their families were relieved after the final and true diagnosis of SJIA and knowing that it can be treated. However, the relief was for a short duration, with the relief receding when they came to understand that SJIA cannot be cured with treatment (Figure 1D). After diagnosis of SJIA, patients found it difficult to integrate “the new me” into their identity and life, and they talked about embarrassment or shame; they feared people would associate their arthritis with the typical arthritis experienced by old people. Many adolescent patients wanted to adhere to their pre-illness identity, to conceal the disease from their peers, so that they could remain as normal or similar to their peers as possible (Figure 1E).
Figure 1.
Social media posts from patients with SJIA or their caregivers regarding the experience of diagnosis through 5 phases.
Notes: (A) Early prediagnosis: patients and their families misunderstood their pain and fatigue, overlooking the problems until a crisis occurred; (B) first misdiagnosis: patients were dismissed as “fakers,” where their initial misdiagnosis was often “growing pains” or “fake pains”; (C) second misdiagnosis: misdiagnosed often as cancer, when the symptoms acutely worsened; (D) tests: confirmatory tests that lead to an SJIA diagnosis; and (E) cognitive identity: focus on the difficulties of dealing with a chronic invisible disease where patients feel ashamed of their arthritis and distressed at being different from their peers.
Abbreviations: JIA, juvenile idiopathic arthritis; SJIA, systemic juvenile idiopathic arthritis.
Emotional impact of SJIA on adolescents
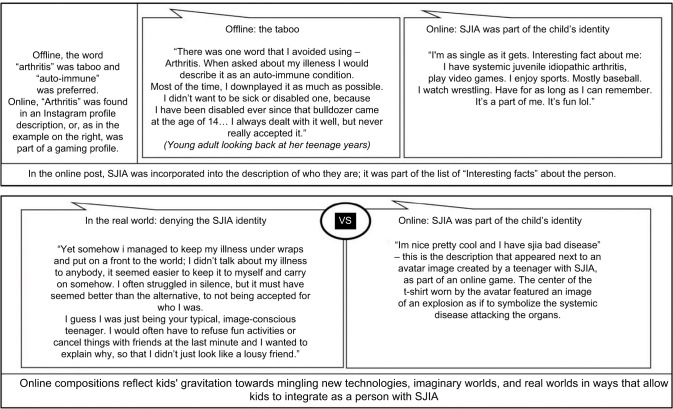
Posts from adolescents showed that they posted online about the difficulties of their disease; however, in the real world, they tried to conceal their disease. Posts demonstrated that adolescent patients preferred to use other names for SJIA, such as “autoimmune [sic] disease,” instead of SJIA or arthritis in the physical world. In the real world, adolescents reported that they acted as if they were persons with no pain or real reasons to skip joining friends at the mall or pool. They also struggled to prevent the “sleeping child” from becoming a “sleeping teenager.” However, this is a challenge given the toll the disease can take on their ability to engage in similar activities performed by their healthy counterparts at an equal level (Figure 2). On the contrary, in the online community, adolescent patients accepted SJIA as a part of their identity and expressed their pain and despair associated with the disease (Figure 2).
Figure 2.
Social media posts from patients on the emotional impact of SJIA.
Abbreviation: SJIA, systemic juvenile idiopathic arthritis.
Patients’ description of SJIA
SJIA patients expressed anger and described SJIA as an invisible disease (Figure 3A) and a powerful external enemy attacking their body by using terms, such as “bulldozer,” “dragon,” and “monster.” The term “Still’s” was also used, but only by older adolescents. Patients shared hashtags, such as #stillssucks, #notstandingstillsdisease, and #ihatearthritis. Many patients have adopted the term “spoonie” to describe themselves as someone living with a chronic disease; the term originated in the autoimmune community to describe how people with chronic conditions manage their energy throughout the day (Figure 3B). This term was coined by a lupus patient during an explanation given to a friend in a restaurant using the spoons on the table as symbols of units of energy to be sparingly used throughout the day: imagine you start each day with 8 spoons of energy, if you use 6 in the morning because you go shopping, you have only 2 left to finish the day with. SJIA teenagers relate to the “spoonie” conceptualization and feel part of this community.10 SJIA patients described the lack of energy as a significant challenge to living a normal adolescent life. Figure 3B shows an image of how climbing stairs was a physical challenge for a SJIA patient in college.
Figure 3.
Patients’ description of SJIA.
Abbreviations: PT, physical training; SJIA, systemic juvenile idiopathic arthritis.
Posts demonstrated that patients did not feel associated with their disease and imagined SJIA as an external enemy that they have to fight. The warrior image of themselves was frequent in the representations shared online (Figure 3C) and aligns with the monster conceptualization of the disease. Mothers of SJIA patients also used warrior-child imagery and language in their posts (Figure 3C).
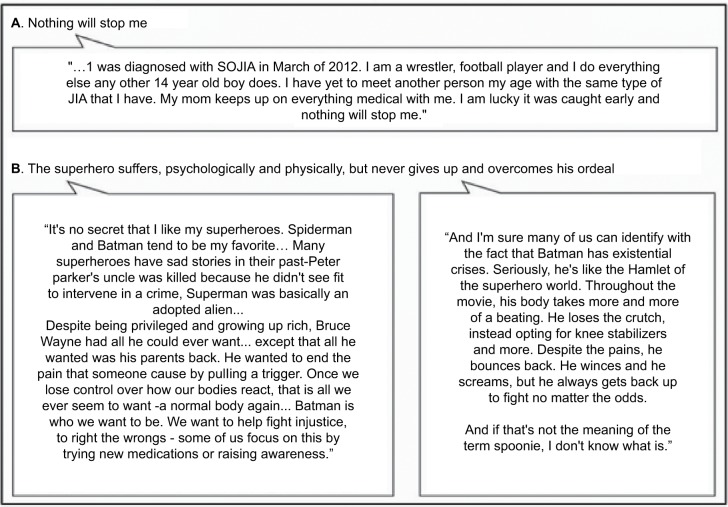
Along with the warrior image of themselves, numerous patients used superhero language or imagery in their social media posts to help them “fight” the disease and its burden, based on the idea that superheroes can fight dragons and monsters. A 14-year-old patient mentioned that he felt lucky his disease was caught earlier and that nothing can stop him from living a normal life like other boys of his age (Figure 4A).
Figure 4.
Social media posts from adolescents and their parents on how to fight SJIA.
Abbreviation: SJIA, systemic juvenile idiopathic arthritis; SOJIA, systemic onset juvenile idiopathic arthritis.
Patients mentioned that superheroes are not only strong and fearless enough to fight monsters, lift and destroy bulldozers, and eradicate dragons (which are the concepts used to describe the disease), but they also have a special history (Figure 4B). SJIA patients used writings to appreciate what they share with superheroes; similar to the adolescent SJIA patients, most superheroes discovered an alienation of self in their own childhoods (Figure 4A). Superheroes overcame their alienation (e.g., Batman from his beloved murdered parents) by choosing to be strong and fighting back, a response the kids appreciated and aimed to model in their own life and world (Figure 4B).
SJIA and death
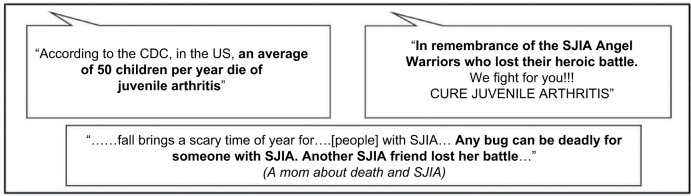
Adolescent SJIA patients and their parents posted about the risk of death related to JA and SJIA or shared stories about the death of other SJIA patients, which were distinct from patients suffering from other forms of JA. Three of the posts related to death posted by SJIA patients/caregivers are presented in Figure 5.
Figure 5.
Social media posts from adolescents with SJIA and their parents on death*. (No reference to death was made in posts from patients who posted as having JA, JRA, or JIA).
Notes: *These quotes were contained within pictures that presented imagery of short-life beauties (flowers, butterflies) and an afterlife (angels).
Abbreviations: JA, juvenile arthritis; JIA, juvenile idiopathic arthritis; JRA, juvenile rheumatoid arthritis; SJIA, systemic juvenile idiopathic arthritis; SOJIA, systemic onset juvenile idiopathic arthritis.
Discussion
We analyzed social media posts from adolescent SJIA patients to examine the impact of SJIA on the physical, social, and emotional aspects of patients and their families. Posts regarding childhood were studied to understand adolescents’ perspectives on their diagnosis and history with SJIA, and posts from patients in their 20s were studied if they provided a view on their adolescent years. In this study, patients’ experience of SJIA diagnosis was categorized in 5 phases, as reported previously by Modica et al.9 As a result of misdiagnosis, patients encountered considerable stress and needless suffering. This also broke the confidence of some of the patients in their health care providers. The issue of misdiagnosis may stem, in a great part, from the difficulty in accessing pediatric rheumatologists in many parts of the country.11 Delays in diagnosis and gaps in communication with health care providers not only affects the patients but also leads to frustration and distress among the caregivers.9 Patients and parents of children with other chronic diseases also reported experiencing confusion and distress before and after the diagnosis of the disease.12–15 Our findings confirm that accurate diagnosis of the disease provides relief to patients and their families. However, once a patient is aware of the fact that there is only treatment and no cure for SJIA, one of the difficult aspects for patients, particularly adolescents, is the loss of “normal” life for the forseeable future, and this is stressful for patients as well as caregivers of SJIA patients. The importance of “being normal” has also been demonstrated in adolescent patients with other chronic diseases.16
We observed that adolescents with SJIA prefer to adhere to their pre-illness identity and conceal the disease from their peers so that they can remain as normal or similar to their peers as possible. It was also observed for adolescents with JA in general and chronic illnesses.16–18 The fear of being stigmatized, which prevented SJIA patients from revealing their disease, is also reflected in other long-term diseases, including rheumatoid arthritis, chronic back pain, cancer, acquired immunodeficiency syndrome, and mental disorders.19–25 Similar to patients with rheumatoid arthritis, adolescent SJIA patients were ashamed and embarrassed of being perceived as abnormal and feared discrimination. Furthermore, concurrently, patients diagnosed with SJIA have a basic need to express their emotions about the illness they experience. Patients resolve these opposing needs by going online where they find disease- and non-disease-specific communities and forums to talk about the difficulties of living with the disease. This helps them unburden the emotional weight of the disease by giving voice to the unending challenges it brings, outside the lens of their real-world peers.
Young patients used their online writing and imagery choices to describe their disease and express their true feelings about the disease and what they aim for in real life. Patients preferred to use other names for SJIA as they wanted to avoid association with the word “arthritis,” because the word “arthritis” is associated with being “old” and kids are quite sensitive to such potential perceptions of them by others. Online, some patients described SJIA as an “autoimmune disease,” although it is an autoinflammatory disease, a nomenclature issue that may stem from lack of adequate knowledge of patients about the disease.
SJIA was described as coming from the outside and attacking them, an attacker they express feelings of hatred against, as it affects their psychosocial potential, physical and mental health, and overall well-being.
Adolescents also used superhero language/imagery to build the fortitude they need to persevere through the disease and to be as normal as possible offline, among their real-world peers. Imageries of superheroes are important for SJIA adolescents, including girls to fight SJIA. Social media posts and reports on using superhero narratives to cope with long-term disease have been documented in patients with other disorders, including cancer, JIA, and rheumatoid arthritis.21,26,27 The “illusive” aspect of the monster or the dragon hark back to the prediagnosis period, when the child’s credibility or truthfulness was called into question-the invisible disease causing family physicians to suggest that SJIA was nothing more than a child faking an illness to avoid school. This period presented the first fissures in a patient’s image. However, this symbolical illusive aspect can also be linked to the fact that adolescents do not mention visible symptoms or handicap (versus JA patients); instead, they frequently talk about SJIA as the “invisible illness” that is hard to fight and integrate in to their identity. Opposing the illness and hating it keeps the boundaries up between “I” (the patient) and “it” (the disease). The patients’ methods of battling “it” involve being stronger than the disease (e.g., exercise 2 times a day, go to class then to work, date), but that also goes with denying their disease in real life. The use of metaphors to describe the illness and cope with it is common in pediatric as well as adult patients with other diseases as well.28,29 We observed that some patients and their parents struggled with a fear of death due to the association of SJIA with death. The threat of death due to chronic disease has also been documented in patients and families of children with other disorders, including Marfan syndrome and cancer.12,23 Interestingly, adolescents self-identify themselves on non-disease-specific online locations, including gaming locations or on Twitter (e.g., “my hips don’t lie, they really freaking hurt,” the first phrase from a Shakira song and the second creatively playing off Shakira’s line); peers from school might find these profiles, which may explain the low number of identifiable SJIA adolescents talking online on open forums.
These findings should be interpreted in light of the qualitative nature of the study and the small sample size. Most patients were from the USA, so our findings may not reflect the diagnostic experience of all SJIA patients. The posts from SJIA patients were collected between 2009 and 2015 and may be markedly different now, given that there are more therapeutic options approved for the treatment of SJIA (e.g., interleukin [IL]-1/IL-6 inhibitors).30,31
Conclusion
Adolescent SJIA patients posted openly about the difficulties of their disease that were causing them to be different from their healthy peers, whereas in the real world, they tried to minimize or hide the effects of their disease. Adolescent SJIA patients frequently used narratives and images of superheroes in their posts to describe their fight for health. Physicians can use these insights when counseling adolescent SJIA patients to provide a narrative that meshes with patients’ worldview, and perhaps to improve physician–patient communication to increase treatment adherence. Nevertheless, medical teams could also encourage adolescents to seek help for endorsing the disease in real life; hiding can be adding weight to the burden, and although expressing themselves online through modern social media may help considerably, it still instills a cognitive schism that demands organization and division of the “Self.”
Acknowledgments
We thank the patients and their families that shared their posts online, and thus their thoughts were available for inclusion in this study. The authors thank Amit Agarwal (Novartis Healthcare Pvt Ltd, Hyderabad, India) for medical writing and editorial support. This research was funded by Novartis Pharmaceuticals Corporation. The authors had full control of the contents of this article. The abstract of this paper was presented at the EULAR (The European League Against Rheumatism) 2016 Congress as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Annals of the Rheumatic Diseases: http://dx.doi.org/10.1136/annrheumdis-2016-eular.3240.
Footnotes
Author contributions
RFM and AC designed the research, identified the samples, analyzed and interpreted data, and drafted and edited the article. PB contributed to design and implementation of research and edited the article. KGL contributed to the analysis of the results and to the writing of the article. All authors discussed the results and approved the article for publication.
Disclosure
KGL is an employee of Novartis Pharmaceuticals Corporation. The other authors report no conflicts of interest in this work.
References
- 1.Bruck N, Schnabel A, Hedrich CM. Current understanding of the pathophysiology of systemic juvenile idiopathic arthritis (sJIA) and target-directed therapeutic approaches. Clin Immunol. 2015;159(1):72–83. doi: 10.1016/j.clim.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369(9563):767–778. doi: 10.1016/S0140-6736(07)60363-8. [DOI] [PubMed] [Google Scholar]
- 3.Mellins ED, Macaubas C, Grom AA. Pathogenesis of systemic juvenile idiopathic arthritis: some answers, more questions. Nat Rev Rheumatol. 2011;7(7):416–426. doi: 10.1038/nrrheum.2011.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Correll CK, Binstadt BA. Advances in the pathogenesis and treatment of systemic juvenile idiopathic arthritis. Pediatr Res. 2014;75(1–2):176–183. doi: 10.1038/pr.2013.187. [DOI] [PubMed] [Google Scholar]
- 5.Bailey KM, McDonagh JE, Prieur AM. Systemic juvenile idiopathic arthritis presenting in a young child with long-term disability as an adolescent. Ann Rheum Dis. 2004;63(12):1544–1548. doi: 10.1136/ard.2004.021568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amine B, Rostom S, Benbouazza K, Abouqal R, Hajjaj-Hassouni N. Health related quality of life survey about children and adolescents with juvenile idiopathic arthritis. Rheumatol Int. 2009;29(3):275–279. doi: 10.1007/s00296-008-0672-y. [DOI] [PubMed] [Google Scholar]
- 7.Minden K, Niewerth M, Listing J, Biedermann T, Schöntube M, Zink A. Burden and cost of illness in patients with juvenile idiopathic arthritis. Ann Rheum Dis. 2004;63(7):836–842. doi: 10.1136/ard.2003.008516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benetoli A, Chen TF, Aslani P. How patients’ use of social media impacts their interactions with healthcare professionals. Patient Educ Couns. 2018;101(3):439–444. doi: 10.1016/j.pec.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Modica RF, Lomax KG, Batzel P, Shapardanis L, Katzer KC, Elder ME. The family journey-to-diagnosis with systemic juvenile idiopathic arthritis: a cross-sectional study of the changing social media presence. Open Access Rheumatol. 2016;8:61–71. doi: 10.2147/OARRR.S105778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miserandino C. The spoon theory. [Accessed February 02, 2018]. Available from: https://butyoudontlooksick.com/articles/written-by-christine/the-spoon-theory.
- 11.McErlane F, Foster HE, Carrasco R, et al. Trends in paediatric rheumatology referral times and disease activity indices over a 10-year period among children and young people with Juvenile Idiopathic Arthritis: results from the childhood arthritis prospective study. Rheumatology (Oxford) 2016;55(7):1225–1234. doi: 10.1093/rheumatology/kew021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelleher E, Giampietro PF, Moreno MA. Marfan syndrome patient experiences as ascertained through postings on social media sites. Am J Med Genet A. 2015;167A(11):2629–2634. doi: 10.1002/ajmg.a.37255. [DOI] [PubMed] [Google Scholar]
- 13.Nelson PA, Kirk SA, Caress AL, Glenny AM. Parents’ emotional and social experiences of caring for a child through cleft treatment. Qual Health Res. 2012;22(3):346–359. doi: 10.1177/1049732311421178. [DOI] [PubMed] [Google Scholar]
- 14.McKechnie AC, Pridham K. Preparing heart and mind following prenatal diagnosis of complex congenital heart defect. Qual Health Res. 2012;22(12):1694–1706. doi: 10.1177/1049732312458371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirkpatrick S, Locock L, Farre A, Ryan S, Salisbury H, McDonagh JE. Untimely illness: when diagnosis does not match age-related expectations. Health Expect. 2018 Feb 9; doi: 10.1111/hex.12669. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hart RI, McDonagh JE, Thompson B, et al. Being as normal as possible: How young people ages 16–25 years evaluate the risks and benefits of treatment for inflammatory arthritis. Arthritis Care Res (Hoboken) 2016;68(9):1288–1294. doi: 10.1002/acr.22832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDonagh JE, Shaw KL, Prescott J, Smith FJ, Roberts R, Gray NJ. “Sometimes I feel like a pharmacist”: identity and medication use among adolescents with juvenile arthritis. Pediatr Rheumatol Online J. 2016;14(1):57. doi: 10.1186/s12969-016-0117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaushansky D, Cox J, Dodson C, McNeeley M, Kumar S, Iverson E. Living a secret: disclosure among adolescents and young adults with chronic illnesses. Chronic Illn. 2017;13(1):49–61. doi: 10.1177/1742395316655855. [DOI] [PubMed] [Google Scholar]
- 19.Kostova Z, Caiata-Zufferey M, Schulz PJ. The process of acceptance among rheumatoid arthritis patients in Switzerland: a qualitative study. Pain Res Manag. 2014;19(2):61–68. doi: 10.1155/2014/168472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eccleston C, Williams AC, Rogers WS. Patients’ and professionals’ understandings of the causes of chronic pain: blame, responsibility and identity protection. Soc Sci Med. 1997;45(5):699–709. doi: 10.1016/s0277-9536(96)00404-2. [DOI] [PubMed] [Google Scholar]
- 21.Michael Trouble’s on a mission [Accessed February 05, 2018]. Available from: http://michaeltrouble.com/parents/
- 22.Elad P, Yagil Y, Cohen L, Meller I. A jeep trip with young adult cancer survivors: lessons to be learned. Support Care Cancer. 2003;11(4):201–206. doi: 10.1007/s00520-002-0426-4. [DOI] [PubMed] [Google Scholar]
- 23.Knapp S, Marziliano A, Moyer A. Identity threat and stigma in cancer patients. Health Psychol Open. 2014;1(1):1–10. doi: 10.1177/2055102914552281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDS. 2006;20(5):359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 25.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20. [PMC free article] [PubMed] [Google Scholar]
- 26.Mendelson A, Rabinowicz N, Reis Y, et al. Comics as an educational tool for children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2017;15(1):69. doi: 10.1186/s12969-017-0198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.RA Guy Foundation: 60-second guide to rheumatoid arthritis [Accessed February 05, 2018]. Available from: https://www.raguyfoundation.org/resources/60-second-guide/
- 28.Harrington KJ. The use of metaphor in discourse about cancer: a review of the literature. Clin J Oncol Nurs. 2012;16(4):408–412. doi: 10.1188/12.CJON.408-412. [DOI] [PubMed] [Google Scholar]
- 29.Weiss M. Signifying the pandemics: metaphors of AIDS, cancer, and heart disease. Med Anthropol Q. 1997;11(4):456–476. doi: 10.1525/maq.1997.11.4.456. [DOI] [PubMed] [Google Scholar]
- 30.Giancane G, Minoia F, Davì S, Bracciolini G, Consolaro A, Ravelli A. IL-1 inhibition in systemic juvenile idiopathic arthritis. Front Pharmacol. 2016;7:467. doi: 10.3389/fphar.2016.00467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Canny S, Mellins E. New frontiers in the treatment of systemic juvenile idiopathic arthritis. F1000Res. 2017;6:971. doi: 10.12688/f1000research.11327.1. [DOI] [PMC free article] [PubMed] [Google Scholar]