Abstract
Background and Aims
Gastroparesis, a chronic gastrointestinal disorder defined by delayed stomach emptying in the absence of obstruction, is often associated with frequent and costly visits to the Emergency Department (ED). The aim of this study was to analyze trends in gastroparesis-related ED visits from 2006–2013.
Methods
Patients with a primary diagnosis of gastroparesis were identified from the National Emergency Department Sample (NEDS), the largest publicly available ED all-payer representative database in the United States (US). ED visits, admission rates, duration of hospitalizations, and charges were compiled. Patients with a secondary diagnosis of diabetes mellitus (DM) were analyzed as a subgroup.
Results
The number of ED visits for gastroparesis as a primary diagnosis in the US increased from 15,459 in 2006 to 36,820 in 2013, an increase from 12.9 to 27.3 per 100,000 ED visits. The total charges associated with these ED visits and subsequent admissions increased from $286 million to $592 million. In contrast, admission rates through the ED decreased by 22%, procedure rates decreased by 6.2%, and the mean length of stay was shortened by 0.6 days. ED visits for patients with diabetic gastroparesis increased from 5,696 to 14,114, an increase from 4.7 to 10.5 per 100,000 ED visits, with an increase in total associated charges for ED visits and subsequent admissions from $84 million to $182 million.
Conclusions
The number of ED visits and associated charges for a primary diagnosis of gastroparesis with or without a secondary diagnosis of DM rose significantly from 2006 to 2013.
Keywords: Gastroparesis, Emergency Departments, Diabetes-Related Complications, Health Care Utilization
Introduction
Gastroparesis is a chronic gastrointestinal disorder defined by delayed stomach emptying in the absence of obstruction1–4 and associated with symptoms of nausea, vomiting, abdominal pain, early satiety, and bloating1–3,5–8. The most common causes of gastroparesis are diabetes mellitus (DM), post-surgical complications, and idiopathic or post-infectious processes9,10. In the community setting, 5 to 12% of patients with diabetes present with symptoms attributable to gastroparesis11,12, and in academic settings, diabetes can represent nearly a third of gastroparesis patients9. Due to the high overlap between symptoms of gastroparesis and other common GI disorders, diagnosis requires documentation of delayed emptying on a gastric emptying scan13–15. Few safe and effective treatment options are currently available to manage the symptoms of gastroparesis3,8. Gastroparesis appears to be relatively uncommon, with the age adjusted incidence per 100,000 persons estimated at 9.6 for men and 37.8 for women16.
Gastroparesis is associated with increased healthcare burden and notably reduced health-related quality of life 17–19. A significant portion of the economic burden associated with gastroparesis relates to emergency department (ED) and hospitalization costs. In a recent outpatient survey study, nearly 54% of gastroparesis patients reported having visited the ED in the past year due to symptom exacerbation20. Similarly, a retrospective, single-center study of 326 gastroparesis patients followed from 2004–2008 found that nearly one third of patients required hospitalizations for symptom exacerbations or nutritional support each year21. The most recent analysis of a representative sample of the United States (US) population found that, gastroparesis-related hospitalizations in the United States increased 158% from 1995 to 2004. This was significantly greater than the rate of DM-related hospitalizations, which in the same time period only increased 53%22.
The primary aim of this study is to provide data on nationwide ED trends in prevalence, demographics, admissions, and charges associated with gastroparesis in the US from 2006 to 2013. A secondary aim of this study is to examine these same trends in a subset of patients with a comorbid diagnosis of DM.
Materials and Methods
This study evaluates trends in ED visits from 2006–2013 by analyzing patients with a primary diagnosis of gastroparesis as well as patients with a primary diagnosis of gastroparesis plus a secondary diagnosis of DM using International Classification of Diseases, 9th Revision (ICD-9) codes. This analysis was done through utilization of the Nationwide Emergency Department Sample (NEDS) from the Healthcare Cost and Utilization Project (HCUP) which is maintained by the Agency for Healthcare Research and Quality (AHRQ)23,24. Statistics on trends and demographic data are freely available through HCUPnet.
The NEDS is the largest publicly available ED all-payer database in the US. The NEDS contains information on approximately 30 million ED visits from approximately 950 hospitals in the US each year, weighted to represent the over 120 million ED visits each year. Individual years of the NEDS are available for purchase and include patient-level data on topics such as demographics, location, primary payer, income quartile, and associated costs. Information on admission rates, procedures performed, and associated charges of those admitted to the hospital from the ED are also analyzed using information contained in the NEDS.
Study Variables
For the primary aim of this study, only patients with a primary diagnosis of gastroparesis (ICD-9) code 536.3) were included, as this most accurately reflects the chief complaint for the ED visit. In secondary analyses, a subgroup of patients who received a primary diagnosis of gastroparesis and a secondary diagnosis of DM (ICD-9 code 250.XX), defined as diabetic gastroparesis, was identified and analyzed separately.
For descriptive and comparative purposes, we examined trends in patients with other GI disorders such as Dyspepsia (ICD-9 787.1), Gastroesophageal Reflux Disease (GERD) (ICD-9 530.81), and Non-specific Nausea and Vomiting (ICD-9 787.01). We also examined a group of patients with either a primary or a secondary diagnosis of gastroparesis.
Demographic data were retrieved according to predefined categories set by HCUP such as age, sex, charge (both ED and inpatient), primary payer (Medicare, Medicaid, private – including HMO, self-pay, no charge, and other), hospital region (Northeast, Midwest, South, and West), hospital location (large central metropolitan (city with greater than 1 million population), large fringe metropolitan (city suburb with greater than 1 million population), medium metropolitan (metro area with 50,000 – 1 million population), and small metropolitan (metro area with 50,000 or less population), and household income.
Inpatient data for patients admitted through the ED with a primary diagnosis of gastroparesis include charges, procedures performed, and length of stay. Inpatient procedure data examined in this study include endoscopy (ICD-9 45.12 – 45.16), Colonoscopy (ICD-9 45.23 – 45.25), Vascular Catheterization (ICD-9 38.93), Hemodialysis (ICD-9 39.95), Transfusion (ICD-9 99.0), Nutritional Support (ICD-9 96.6 and 99.15), Gastrostomy (ICD-9 43.1), Enterostomy (ICD-9 44.3), Mechanical Ventilation (ICD-9 96.7), Gastrectomy (ICD-9 43.5 – 43.9), Adhesiolysis (ICD-9 54.51 and 54.59), Cholecystectomy (ICD-9 51.2), and Radiology (Ultrasound ICD-9 88.76, CT Scan 88.01, and MRI 88.97).
Statistical Analysis
Statistical analysis was performed using STATA/SE 14.1 using the source files for the 2006 and 2013 NEDS, and all cost data reported are inflation adjusted to 2016 dollars using the Consumer Price Index (CPI) inflation calculator25. Total charge data were obtained by multiplying the mean charge in a year by the total number of visits for a year. Rates per 100,000 ED visits were obtained by dividing the number of gastroparesis ED visits by the total number of ED visits and multiplying by 100,000.
Results
ED Rates
Gastroparesis
The number of ED visits for gastroparesis as a primary diagnosis in the US increased from 15,459 in 2006 to 36,820 in 2013, a 138% increase (Table 1). This represents a rise from 12.9 to 27.3 per 100,000 ED visits (Table 1).
Table 1.
ED visits with a primary diagnosis of Gastroparesis in 2006 and 2013.
| 2006 | 2013 | |
|---|---|---|
| N Primary Dx of Gastroparesis | 15,459 | 36,820 |
| N per 100,000 ED Visits | 12.9 | 27.3 |
| Mean Age | 48.1 (95% CI: 47.8 – 48.4) | 44.3 (95% CI: 44.1 – 44.5) |
| Female | 67.3% | 70.2% |
| Mean Cost of ED Visit | $2,171 (95% CI: 2,120 – 2,222) | $4,352 (95% CI: 4,288 – 4,417) |
| Median Cost of ED Visit | $1,524 | $2,787 |
| Mean Cost of Inpatient Stay | $28,135 (95% CI: 27,264 – 29,005) | $32,563 (95% CI: 31,955 – 33,171) |
| Median Cost of Inpatient Stay | $18,465 | $23,225 |
| Admitted through ED | 58.1% | 36.1% |
| Procedure Performed after Admission | 58.1% | 51.9% |
| Mean Length of Stay (Days) | 5.4 (95% CI: 5.3 – 5.5) | 4.8 (95% CI: 4.7 – 4.9) |
| Primary Insurer % | ||
| Medicare | 36.9 | 33.8 |
| Medicaid | 19.6 | 23.6 |
| Private (Including HMO) | 33.2 | 27.5 |
| Self-Pay | 6.9 | 10.2 |
| No Charge | 0.4 | 1.5 |
| Other | 3.0 | 3.4 |
| Region % | ||
| Northeast | 18.0 | 16.5 |
| Midwest | 23.5 | 17.5 |
| South | 43.3 | 49.1 |
| West | 15.2 | 16.9 |
| Location % | ||
| Large Central Metropolitan | 24.5 | 27.3 |
| Large Fringe Metropolitan | 25.1 | 21.7 |
| Medium Metropolitan | 25.2 | 26.8 |
| Small Metropolitan | 25.0 | 23.9 |
| Household Income | ||
| Lowest Quartile | 30.1 | 37.0 |
| 2nd Quartile | 25.7 | 26.6 |
| 3rd Quartile | 25.0 | 20.6 |
| Highest Quartile | 17.4 | 14.3 |
All Charge Data Reported in 2016 dollars.
Procedure Performed after Admission includes patients who had any inpatient procedure performed
Data may not add up to 100% due to missing data
Large central metropolitan - city with greater than 1 million population; Large fringe metropolitan - city suburb with greater than 1 million population; Medium metropolitan - metro area with 50,000 – 1 million population; Small metropolitan – an area with 50,000 or less population
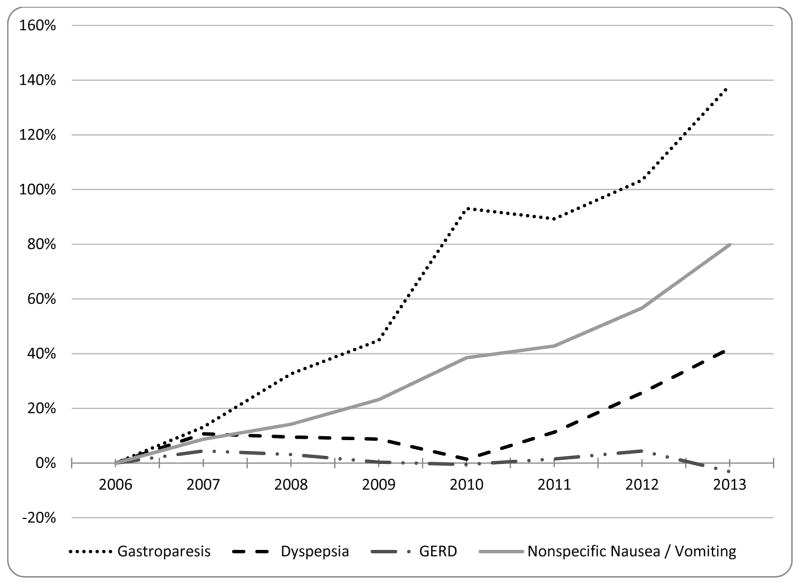
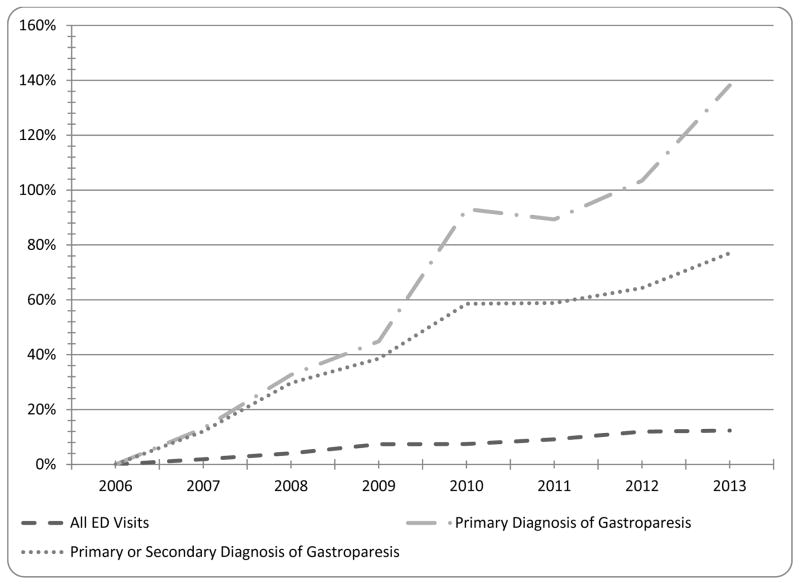
The rate of rise in ED visits with a primary diagnosis of gastroparesis from 2006–2013 outpaced the rates for other functional upper-gastrointestinal disorders such as functional dyspepsia, GERD, and non-specific nausea and vomiting (Figure 1). Also, the rate of rise in patients with a primary diagnosis of gastroparesis in the ED was higher than the combined rate of patients with either a primary or secondary diagnosis of gastroparesis (Figure 2).
Figure 1.
Trends in ED visits by year by primary diagnosis. Percentages are reported as relative changes from a baseline of 2006.
Figure 2.
Trends in ED visits by year by visit type. Percentages are reported as relative changes from a baseline of 2006.
Diabetic Gastroparesis
The number of ED visits for patients with diabetic gastroparesis increased by 148% from 5,696 in 2006 to 14,114 in 2013, representing a rise from 4.7 to 10.5 visits per 100,000 ED visits. During the same time period, the total number of DM-related ED visits (patients with a primary or secondary diagnosis of DM) rose by 45%. However, diabetic gastroparesis accounted for a stable proportion of all primary gastroparesis visits across this time-frame, constituting 36.8% and 38.3% of all primary gastroparesis visits in 2006 and 2013 respectively (Table 2).
Table 2.
ED visits of patients with a primary diagnosis of gastroparesis and a secondary diagnosis of DM.
| 2006 | 2013 | |
|---|---|---|
| N Primary Dx Gastroparesis and Secondary Dx DM (% of all primary dx gastroparesis visits) | 5,696 (36.8) | 14,114 (38.3) |
| N per 100,000 ED Visits | 4.7 | 10.5 |
| Mean Age | 49.3 (95% CI: 48.9 – 49.7) | 46.0 (95% CI: 45.8 – 46.3) |
| Female | 61.2% | 64.0% |
| Mean Cost of ED Visit | $2,393 (95% CI: 2,308 – 2,478) | $4,531 (95% CI: 4,425 – 4,638) |
| Median Cost of ED Visit | $1,718 | $2,916 |
| Mean Cost of Inpatient Stay | $25,596 (95% CI: 24,659 – 26,533) | $29,890 (95% CI: 28,941 – 30,795) |
| Median Cost of Inpatient Stay | $17,939 | $20,812 |
| Admitted through ED | 48.5% | 28.2% |
| Procedure Performed after Admission | 53.8% | 44.6% |
| Mean Length of Stay (Days) | 4.8 (95% CI: 4.6 – 4.9) | 4.2 (95% CI: 4.1 – 4.4) |
All Charge Data Reported in 2016 dollars.
Procedure Performed after Admission includes patients who had any inpatient procedure performed
Charges
Gastroparesis
The total combined ED and inpatient charges (adjusted to 2016 dollars) for visits related to patients with a primary diagnosis of gastroparesis increased from $286,270,059 (95% CI: 277,658,328 – 294,872,808) in 2006 to $592,774,969 (95% CI: 582,342,425 – 603,244,333) in 2013. The increase in total aggregate charges from 2006 to 2013 can be broken down into increases in both ED and inpatient charges. The mean ED charge per visit increased from $2,171 (95% CI: 2,120 – 2,222) in 2006 to $4,352 (95% CI: 4,288 – 4,417) in 2013 (Table 1). Additionally, the mean inpatient charge per admission increased from $28,135 (95% CI: 27,264 – 29,005) in 2006 to $32,563 (95% CI: 31,955 – 33,171) in 2013 (Table 1). For comparison, from 2006 to 2013, the mean charge for all ED visits in the US increased from $1,560 to $2,759 and the mean inpatient charge increased from $33,169 to $41,327.
Diabetic Gastroparesis
The total combined ED and inpatient charges for patients with diabetic gastroparesis increased from $84,341,014 (95% CI: 81,268,335 – 87,413,692) in 2006 to $182,917,158 (95% CI: 177,643,913 – 188,029,390) in 2013. The mean ED charge per visit increased from $2,393 (95% CI: 2,308 – 2,478) to $4,531 (95% CI: 4,425 – 4,638) and the mean inpatient charge per admission increased from $25,596 (95% CI: 24,659 – 26,533) in 2006 to $29,890 (95% CI: 28,941 – 30,795) in 2013 (Table 2).
Admissions and Procedures
Gastroparesis
Admissions to the hospital from the ED among patients with gastroparesis as a primary diagnosis fell from 58.1% in 2006 to 36.1% in 2013 (Table 1). The mean length of stay for patients admitted from the ED decreased from 5.4 to 4.8 days from 2006 to 2013 (Table 1). The percentage of patients admitted through the ED who had a procedure performed decreased from 58.1% in 2006 to 51.9% in 2013. The rates of commonly performed procedures can be found in Table 3.
Table 3.
Inpatient procedures performed on patients with a primary diagnosis of gastroparesis admitted from the ED.
| Procedure | 2006 (N, %) | 2013 (N, %) |
|---|---|---|
| Admitted to the Hospital | 8,982 (100) | 13,292 (100%) |
| Endoscopy | 3292 (36.7) | 4282 (32.2) |
| Vascular Catheterization | 1078 (12.0) | 708 (5.3) |
| Hemodialysis | 516 (5.7) | 668 (5.0) |
| Colonoscopy | 414 (4.6) | 459 (3.5) |
| Nutritional Support | 371 (4.1) | 721 (5.4) |
| Transfusion | 308 (3.4) | 350 (2.6) |
| Radiology | 233 (2.6) | 234 (1.8) |
| Gastrostomy | 98 (1.1) | 169 (1.3) |
| Cholecystectomy | 39 (0.4) | 56 (0.4) |
| Adhesiolysis | 38 (0.4) | 41 (0.3) |
| Enterostomy | 36 (0.4) | 41 (0.3) |
| Mechanical Ventilation | 26 (0.3) | 37 (0.3) |
| Gastrectomy | 24 (0.3) | 20 (0.2) |
Diabetic Gastroparesis
Patients with diabetic gastroparesis were admitted through the ED at a lower rate than those with only a primary diagnosis of gastroparesis between 2006 and 2013 from 48.5% to 28.2% (Table 2). The mean length of stay for patients with diabetic gastroparesis decreased from 4.8 to 4.2 days from 2006 to 2013 (Table 2). Additionally, the percentage of diabetic gastroparesis patients admitted to the hospital through the ED who had an inpatient procedure performed decreased from 53.8% in 2006 to 44.6% in 2013.
Demographics
Gastroparesis
The observed increased incidence of ED visits for patients with a primary diagnosis of gastroparesis was also characterized by predominantly more women. The percentage of visits by women increased from 67.3% to 70.2% and the mean age declined from 48.1 years (95% CI: 47.8 – 48.4) to 44.3 years (95% CI: 44.1 – 44.5) of those presenting to the ED with gastroparesis from 2006 to 2013 (Table 1).
From 2006 to 2013, the percentage of ED visits paid by Medicaid increased from 19.6% to 23.6% while the percentage paid by private insurance decreased from 33.2% to 27.5% (Table 1). Between 2006 and 2013, the percentage of patients with a primary diagnosis of gastroparesis from the South increased from 43.3% to 49.1% while the percentage from the Midwest decreased from 23.5% to 17.5% (Table 1). The percentage of patients from large central metropolitan areas increased from 24.5% to 27.3% between 2006 and 2013 while the percentage of patients from large fringe metropolitan areas decreased from 25.1% to 21.7%.
Diabetic Gastroparesis
The mean age of patients entering the ED with diabetic gastroparesis was approximately the same as patients with a primary diagnosis of gastroparesis decreasing from 49.3 (95% CI: 48.9 – 49.7) in 2006 to 46.0 (95% CI: 45.8 – 46.3) in 2013 (Table 2). The percentage of women with diabetic gastroparesis was lower than those only with a primary gastroparesis diagnosis, but rose at a similar rate between 2006 and 2013 from 61.2% to 64.0% (Table 2).
Discussion
This study shows that the total number of ED visits for gastroparesis increased 138% from 2006 to 2013. In contrast, admission rates through the ED decreased 22%, procedure rates decreased by 6.2%, and the mean length of stay was shortened by 0.6 days. Combined ED and inpatient charges for patients with a primary diagnosis of gastroparesis increased by 107% from 2006 to 2013 compared to a rise of 46% in all ED and inpatient charges in the US during the same time period. The number of ED visits for patients with diabetic gastroparesis increased 148%. The total associated charges with these ED visits and subsequent admissions rose 117% from about $84 million in 2006 to about $182 million in 2013.
Although the total number of ED visits for patients with a primary diagnosis of gastroparesis increased, the proportion of diabetic and non-diabetic patients was consistent from 2006 to 2013. Thus, the increased rates of gastroparesis in the ED can be attributed to increases in both non-diabetic and diabetic gastroparesis visits. Non-diabetic gastroparesis is often attributed to post-infectious processes, post-surgical complications affecting the vagus nerve, and complications of other conditions such as anorexia nervosa26. While very little is known about the natural history of gastroparesis, a study in Olmstead County showed a stable incidence of gastroparesis from 1996 to 2000 and 2001 to 200616. The increases in non-diabetic gastroparesis ED visits may reflect an increased incidence of these processes, an increased awareness of idiopathic gastroparesis among emergency room providers, or both. On the other hand, the increase in diabetic gastroparesis ED visits seems is likely to be tied to the increasing prevalence of DM as seen in the 45% increase in all DM-related ED visits from 2006 to 2013.
It is worth noting that the rate of inpatient admission for gastroparesis from the ED fell from 58% in 2006 to 36% in 2013 and the mean length of stay decreased by 0.6 days. This is in contrast to a prior study which reported increasing admission rates from the ED for gastroparesis and increasing length of stay for these visits from 1995 to 200422. Mean ED charges for gastroparesis patients were higher than the national mean for all ED charges; however their mean inpatient charges were lower than the national mean. This may be attributable to a shift in gastroparesis care in the ED to an outpatient setting. A significant increase in charges may be due to an increasing use of prokinetic and anti-emetic drugs as well as increasing nursing staff resources utilized in caring for these patients in the ED.
One reason for the smaller rate of increase in inpatient charges compared to ED charges in the care of gastroparesis patients is the simultaneous decline in inpatient procedure performed. Similar to a prior study, upper endoscopic procedures occurred in a third of admissions27. However, radiology, colonoscopy, and vascular catheterizations show a decreasing trend in from 2009 to 2013. This may indicate less patient complexity or providers choosing less costly interventions that may not be warranted. This is reasonable given the evidence indicating fewer than 5% of non-therapeutic endoscopies result in a change in treatment, and fewer than one sixth of CT scans identify relevant findings in gastroparesis21.
The South had a disproportionately high rate of gastroparesis ED visits compared to other regions in the US. This could possibly be tied to the high rates of DM and low income levels, which are both tied to increased ED visits. Consistent with this trend, the percentage of patients in the bottom quartile of household income saw the largest increase between 2006 and 2013.
There are several limitations to this study. Since symptoms of gastroparesis are nonspecific and given the nature of using ICD-9 billing codes as evidence of gastroparesis, we cannot confirm each instance of gastroparesis based on a gastric emptying scan. Additionally, the hospitals that are included in the NEDS database may vary in their coding practices. Also, patients that visit the ED multiple times are counted as separate individuals. We do not account for ambulatory data or patients admitted to the hospital outside of the ED in our analysis. Despite these limitations, we believe the sample size and the fact that the NEDS is a representative database of patients in the US outweigh these limitations.
In conclusion, this study highlights a disproportionately high rate of gastroparesis-related ED visits. While the mean length of inpatient stay and inpatient procedure rates have decreased, ED and hospitalization charges are rising in this population. Given the demands on costs due to healthcare utilization and individual costs on quality of life, further research should focus on the causes of this increasing rate of gastroparesis in the ED as well as on the associated charges.
Acknowledgments
Financial Support: This project was funded in part by R01AT008573 (AL) and T32DK007760-17 (SB).
Footnotes
Potential Competing Interests: None
Author Contributions: The idea for the article was conceived by A.L. The manuscript was drafted by W.H., J.N., and S.B. Statistical analysis was performed by W.H and T.P. The draft manuscript was critically reviewed by D.F., H.L., and V.C. All authors reviewed and approved the final version of the manuscript.
References
- 1.Bharucha AE. Epidemiology And Natural History Of Gastroparesis. Gastroenterol Clin North Am. 2015;44:9–19. doi: 10.1016/j.gtc.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. Clinical Guideline: Management of Gastroparesis. Am J Gastroenterol. 2013;108:18–37. doi: 10.1038/ajg.2012.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagarwala J, Dev S, Markin A. The Vomiting Patient: Small Bowel Obstruction, Cyclic Vomiting, and Gastroparesis. Emerg Med Clin North Am. 2016;34:271–291. doi: 10.1016/j.emc.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Parkman HP, Hasler WL, Fisher RS. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127:1592–1622. doi: 10.1053/j.gastro.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 5.Cherian D, Sachdeva P, Fisher RS, Parkman HP. Abdominal Pain Is a Frequent Symptom of Gastroparesis. Clin Gastroenterol Hepatol. 2010;8:676–681. doi: 10.1016/j.cgh.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 6.Hasler WL. Gastroparesis: Symptoms, Evaluation, and Treatment. Gastroenterol Clin North Am. 2007;36:619–647. doi: 10.1016/j.gtc.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Hoogerwerf WA, Pasricha PJ, Kalloo AN, Schuster MM. Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol. 1999;94:1029–1033. doi: 10.1111/j.1572-0241.1999.01008.x. [DOI] [PubMed] [Google Scholar]
- 8.Horowitz M, Su YC, Rayner CK, Jones KL. Gastroparesis: prevalence, clinical significance and treatment. Can J Gastroenterol J Can Gastroenterol. 2001;15:805–813. doi: 10.1155/2001/628102. [DOI] [PubMed] [Google Scholar]
- 9.Soykan I, Sivri B, Sarosiek I, Kiernan B, McCallum RW. Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci. 1998;43:2398–2404. doi: 10.1023/a:1026665728213. [DOI] [PubMed] [Google Scholar]
- 10.Naftali T, Yishai R, Zangen T, Levine A. Post-infectious gastroparesis: clinical and electerogastrographic aspects. J Gastroenterol Hepatol. 2007;22:1423–1428. doi: 10.1111/j.1440-1746.2006.04738.x. [DOI] [PubMed] [Google Scholar]
- 11.Maleki D, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Arch Intern Med. 2000;160:2808–2816. doi: 10.1001/archinte.160.18.2808. [DOI] [PubMed] [Google Scholar]
- 12.Bytzer P, et al. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161:1989–1996. doi: 10.1001/archinte.161.16.1989. [DOI] [PubMed] [Google Scholar]
- 13.Abell TL, et al. Consensus Recommendations for Gastric Emptying Scintigraphy: A Joint Report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008;36:44–54. doi: 10.2967/jnmt.107.048116. [DOI] [PubMed] [Google Scholar]
- 14.Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24–29. doi: 10.1023/a:1005697422454. [DOI] [PubMed] [Google Scholar]
- 15.Ziessman HA, Bonta DV, Goetze S, Ravich WJ. Experience with a Simplified, Standardized 4-Hour Gastric-Emptying Protocol. J Nucl Med. 2007;48:568–572. doi: 10.2967/jnumed.106.036616. [DOI] [PubMed] [Google Scholar]
- 16.Jung H, et al. The Incidence, Prevalence, and Outcomes of Patients With Gastroparesis in Olmsted County, Minnesota, From 1996 to 2006. Gastroenterology. 2009;136:1225–1233. doi: 10.1053/j.gastro.2008.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hasler WL, et al. Psychological dysfunction is associated with symptom severity but not disease etiology or degree of gastric retention in patients with gastroparesis. Am J Gastroenterol. 2010;105:2357–2367. doi: 10.1038/ajg.2010.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bielefeldt K, Raza N, Zickmund SL. Different faces of gastroparesis. World J Gastroenterol. 2009;15:6052–6060. doi: 10.3748/wjg.15.6052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jaffe JK, Paladugu S, Gaughan JP, Parkman HP. Characteristics of nausea and its effects on quality of life in diabetic and idiopathic gastroparesis. J Clin Gastroenterol. 2011;45:317–321. doi: 10.1097/MCG.0b013e3181eeb5e9. [DOI] [PubMed] [Google Scholar]
- 20.Lacy BE, Crowell MD, Mathis C, Bauer D, Heinberg LJ. Gastroparesis Quality of Life and Health Care Utilization. J Clin Gastroenterol. 2017 doi: 10.1097/MCG.0000000000000728. Published Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 21.Dudekula A, O’Connell M, Bielefeldt K. Hospitalizations and testing in gastroparesis. J Gastroenterol Hepatol. 2011;26:1275–1282. doi: 10.1111/j.1440-1746.2011.06735.x. [DOI] [PubMed] [Google Scholar]
- 22.Wang YR, Fisher RS, Parkman HP. Gastroparesis-Related Hospitalizations in the United States: Trends, Characteristics, and Outcomes, 1995–2004. Am J Gastroenterol. 2008;103:313–322. doi: 10.1111/j.1572-0241.2007.01658.x. [DOI] [PubMed] [Google Scholar]
- 23.(NEDS) HNEDS. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2006. p. 2013. [PubMed] [Google Scholar]
- 24. [Accessed: 12th August 2016];HCUPnet: A tool for identifying, tracking, and analyzing national hospital statistics. Available at: http://hcupnet.ahrq.gov/
- 25.Consumer Price Index Inflation Calculator 2015.
- 26.Bityutskiy LP, Soykan I, McCallum RW. Viral gastroparesis: a subgroup of idiopathic gastroparesis--clinical characteristics and long-term outcomes. Am J Gastroenterol. 1997;92:1501–1504. [PubMed] [Google Scholar]
- 27.Bielefeldt K. Factors influencing admission and outcomes in gastroparesis. Neurogastroenterol Motil. 2013;25:389–e294. doi: 10.1111/nmo.12079. [DOI] [PubMed] [Google Scholar]