Abstract
Background
Widely recommended developmental surveillance methods include developmental monitoring (DM) and development screening (DS). Much research has been done on DS, but very little research has compared the effectiveness of DM and DS together.
Objectives
To investigate the relationship between DM and DS in Part C early intervention (EI) service receipt.
Methods
Authors used data from the 2007/2008 and 2011/2012 National Survey of Children's Health (NSCH). Authors report the prevalence of children aged 10 months to 3 years who received (a) DM only, (b) DS only, (c) both DM and DS, and (c) no DM or DS across survey years. Authors compare the odds of EI receipt across these groups.
Results
During both periods, estimated EI receipt prevalence was higher for children receiving both DM and DS (8.38% in 2007/2008; 6.47% in 2011/2012) compared to children receiving no DM or DS (1.31% in 2007/2008; 1.92% in 2011/2012), DM alone (2.74% in 2007/2008; 2.70% in 2011/2012), or DS alone (3.59% in 2007/2008; 3.09% in 2011/2012) (for both time frames, p < .05). From 2007/2008 to 2011/2012, the proportion of children receiving DS only and both DM and DS increased, while children receiving DM only and no DM or DS decreased.
Conclusions
Children receiving DM and DS together were more likely to receive EI compared to children receiving DM alone, DS alone, or neither DM nor DS. These findings support the AAP recommendations indicating that DM and DS are complementary strategies for improving early identification and linkage to EI for young children.
Keywords: Bright futures, Child find, Developmental epidemiology, Developmental surveillance, Developmental screening, Developmental monitoring, Early intervention, Individuals with disabilities education act, Part C
Early intervention (EI) programs effectively improve developmental skills and help children at risk of developmental disabilities or delays thrive socially as well as academically.1,2 Unfortunately, only a small proportion of children who could benefit from EI are identified early enough to receive it.3–5 To facilitate early identification, several federal organizations and non-profit agencies have developed policy guidelines and quality care indicators for pediatricians and other child health care providers (CHCP).6–9 The American Academy of Pediatrics (AAP) recommends that CHCPs engage in early identification efforts via periodic developmental monitoring (DM) and developmental screening (DS).6 DM is a flexible and ongoing process whereby healthcare professionals ask about children's developmental progress and make informed clinical judgments based on their education and experience. DS is a more formal early identification method in which professionals use validated developmental screeners to help identify the presence of developmental concerns. There is mounting evidence that indicates DM alone is insufficient to identify many children at risk for developmental delays and disabilities.6,10–12 Thus, in recent years there has been an expansion of policy and research activities focusing on expanding the number of CHCPs conducting DS.6–8,13–26 Ideally DM and DS should be used in tandem to maximize sensitivity to potential developmental delays.
Children with developmental delays are a heterogeneous group. Not all developmental screeners identify children with the same delays or diagnoses, and different screeners measure different aspects of development27–29 and vary widely in how they were normed and which particular developmental conditions they target.30–34 Thus, DS should occur in the context of DM whereby “knowledgeable healthcare providers identify children who may have healthcare problems” (AAP, 2006, p. 407).6 Part of what knowledgeable a CHCP may bring to DM includes information on which screeners are most appropriate for particular developmental concerns, particularly as related to their patients' unique backgrounds.27–29,35,36
While there is abundant research on the sensitivity and specificity of developmental screeners, very little exists on the effectiveness of DM and/or DS at identifying children who ultimately receive EI.15,37 Research indicates that increased DM or DS predicts increased EI referrals,17,20,21,24,26,37 assessments,37 and eligibility.17,21,24,37 One study showed that DM in tandem with DS resulted in more EI referrals (13.9%) compared to DM alone (5.84%).20 However, while increased referral rates are certainly promising, increased positive screens do not always lead to accurate identification.35,36 Thus, more research is needed on the relative utility of DM in tandem with DS and, separately, on whether use of DS and DM together improves CHCPs' ability to identify children who ultimately receive EI services.
Purpose of the study
The purposes of this analysis are two-fold: (a) determine the rates of DM and DS singly and in tandem in 2007/2008 and 2011/2012 to identify trends; and (b) compare the difference in odds of EI receipt between groups of children receiving DM or DS alone and DM/DS in tandem. EI in this study refers to children receiving Individuals with Disabilities Education Act Part C services, a federally funded EI program for infants and toddlers, via the receipt of an Individualized Family Service Plan (IFSP).38
Methods
Study data and key variables
Data for this study on children between 10 months and 3 years of age came from the National Survey of Children's Health (2007/2008; 2011/2012). Ten months was selected as the lower age threshold because the AAP recommends DS begin at 9 months and DS is not likely a widespread practice under this age.6 The NSCH (2007/2008) data were collected between April 2007 and July 2008 and for NSCH (2011/2012) between February 2011 and June 2012.39,40 The Maternal and Child Health Bureau of the Health Resources and Services Administration funded both NSCH surveys; the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention administered both surveys to parents and other caregivers using the State and Local Area Integrated Telephone Survey.40 For both datasets, estimates are adjusted for non-response bias and weighted to represent the ages 0–17 non-institutionalized U.S. population. The NSCH (2007) was conducted over landlines and the NSCH (2011/2012) was conducted over both landlines and cell phones; this difference was accounted for in their stratifications. The NSCH (2007) collected data from 91,642 caretakers with a 51.2% response rate and NSCH (2011/2012) from 95,677 caretakers with a 54.1% and 41.2% response rate respectively for landline and cell phone samples. National population estimates were developed according to NCHS criteria. Further details are described in publications available from the NCHS.39,40
The key predictor variables for our analyses were whether, in the last year, a parent reported that the child's CHCP provided (a) DS without DM, (b) DM without DS, (c) both DM and DS, or (d) no DM or DS. Authors measured DS from a single survey item: “Did a doctor or other health care provider have you fill out a questionnaire about specific concerns or observations you may have about [S.C.]'s development, communication, or social behaviors? ” DM was measured with the item: “During the past 12 months, did [child's] doctor or other health care providers ask if you have concerns about [his/her] learning, development, or behavior?” The key outcome variable was whether the child received an IFSP in the last year measured by: “Does [child] have any developmental problems for which [he/she] has a written intervention plan called an Individualized Family Service Plan or IFSP?”
Authors included two sets of independent variables related to the receipt of EI. The first was a binary item identifying children with special health care needs (CSHCN); this item was developed from other items indicating that the child has a known medical, behavioral or health condition limiting his or her abilities or the child requires health and related services of a type or amount beyond that generally required by children of the same age. The second set of independent variables included individual, household/socio-demographic, medical care, and Part C variables associated with EI receipt. Details for these variables—age, race/ethnicity, gender, English as the primary household language, metropolitan area, federal poverty level, Part C eligibility criteria, parent education, and insurance type—are found in Tables 1 and 2. Medical care variables included whether children had family centered care or not. Part C variables included whether states had broad, moderate, or narrow eligibility criteria based on cut-off scores on developmental assessments states require to determine EI eligibility.5 Broad states have relatively less stringent cut-off scores for disability and delay assessments allowing more children to be EI eligible (e.g., cut off ≤ 90%ile), narrow have more stringent cut-off scores disallowing more children (e.g., cut off ≤ 75%ile), and moderate states are in the middle.
Table 1.
Descriptive statistics and differences in parent reported IFSP receipt for U.S. children ages 10 months to 3 years in 2007/2008.
| Variable | Sample N | Percentage IFSP (S.E.) | Differences^ |
|---|---|---|---|
| IFSP | |||
| No | 13,004 | ||
| Yes | 506 | 3.32 (0.33) | |
| Developmental Surveillance Method | |||
| No DM or DS | 4972 | 1.31 (0.45)*** | DM & DS > No, DS alone, DM alone |
| DM & DS | 2745 | 8.38 (1.18) | |
| DS alone | 1148 | 3.59 (0.87) | |
| DM alone | 4690 | 2.74 (0.46) | |
| CSHCN | |||
| Yes | 1568 | 19.78 (2.26)*** | CSHCN > not CSHCN |
| No | 11,987 | 1.31 (0.22) | |
| Metro 50,000+ | |||
| Yes | 7525 | 3.03 (0.00) | NA |
| No | 1942 | 3.79 (0.01) | |
| Age | |||
| 10–18 months | 3447 | 3.30 (0.86) | NA |
| 19–23 months | 1953 | 2.16 (0.50) | |
| 2-year-olds | 3736 | 3.29 (0.50) | |
| 3-year-olds | 4419 | 3.89 (0.63) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 8843 | 3.33 (0.40) | NA |
| Non-Hispanic Black | 1136 | 4.60 (1.09) | |
| Non-Hispanic Other/Unreported | 1619 | 3.01 (0.70) | |
| Hispanic | 1957 | 2.68 (0.95) | |
| Gender | |||
| Male | 7033 | 4.23 (0.46)** | Male > Female |
| Female | 6514 | 2.34 (0.48) | |
| Language | |||
| English | 12,592 | 3.40 (0.33) | NA |
| Non-English | 805 | 2.45 (1.42) | |
| Federal Poverty Level | |||
| 400%+ | 4847 | 2.46 (0.61) | NA |
| 300–399% | 1976 | 3.54 (0.69) | |
| 200–299% | 2412 | 3.41 (0.78) | |
| 100–199% | 2374 | 4.49 (0.98) | |
| Less than 100% | 1946 | 3.06 (0.54) | |
| State EI eligibility criteria | |||
| Broad | 4728 | 3.07 (0.57) | NA |
| Moderate | 2122 | 3.33 (0.67) | |
| Narrow | 4833 | 3.84 (0.54) | |
| Parent education | |||
| Less than high school | 1038 | 3.96 (1.58) | NA |
| High school | 2150 | 2.92 (0.51) | |
| More than high school | 9797 | 3.20 (0.40) | |
| Family Centered Care | |||
| Yes | 10,469 | 2.22 (0.00)* | Family Centered Care < none |
| No | 2950 | 4.51 (0.01) | |
| Insurance | |||
| Private | 9053 | 2.54 (0.36)*** | Public > Private, No Insurance |
| Public | 3533 | 4.96 (0.75) | |
| None | 856 | 2.09 (0.70) |
Notes.
= p < .001;
= p < .01;
= p < .05;
= sub-groups differ p < .01;
Broad = state uses liberal cut-off scores on developmental assessments to determine which children require EI services; CSHCN = children with special healthcare needs; DM= developmental monitoring; DS = developmental surveillance; EI = Part C early intervention; IFSP = Individualized Family Service Plan; Moderate = state uses moderately strict cut-off scores on developmental assessments to determine which children require EI services; Narrow = state uses very strict cut-off scores on developmental assessments to determine which children require EI services; SES = socio-economic status.
Table 2.
Descriptive statistics and differences in parent reported IFSP receipt for U.S. children ages 10 months to 3 years in 2011/2012.
| Variable | Sample N | Percentage IFSP (S.E.) | Differences^ |
|---|---|---|---|
| IFSP | |||
| No | 13,820 | ||
| Yes | 558 | 3.64 (0.31) | |
| Developmental Surveillance Method | |||
| No DM or DS | 4461 | 1.92 (0.50)*** | DM & DS > No, DS alone, DM alone |
| DM & DS | 4355 | 6.47 (0.72) | |
| DS alone | 1581 | 3.09 (0.95) | |
| DM alone | 4017 | 2.70 (0.42) | |
| CSHCN | |||
| Yes | 1486 | 16.72 (1.77)*** | CSHCN > no CSHCN |
| No | 12,928 | 2.11 (0.28) | |
| Metro 50,000+ | |||
| Yes | 7757 | 3.49 (0.00) | NA |
| No | 2032 | 4.39 (0.01) | |
| Age | |||
| 10–18 months | 3723 | 2.22 (0.54) | NA |
| 19–23 months | 1869 | 4.16 (0.91) | |
| 2-year-olds | 3784 | 3.77 (0.57) | |
| 3-year-olds | 5038 | 4.38 (0.59) | |
| Race/Ethnicity | |||
| Non-Hispanic White | 8925 | 3.58 (0.36) | NA |
| Non-Hispanic Black | 1244 | 5.80 (1.33) | |
| Non-Hispanic Other/Unreported | 2074 | 3.61 (0.12) | |
| Hispanic | 2171 | 2.70 (0.61) | |
| Gender | |||
| Male | 7300 | 3.50 (0.38) | NA |
| Female | 7103 | 3.78 (0.51) | |
| Language | |||
| English | 13,327 | 3.92 (0.35) | NA |
| Non-English | 725 | 1.93 (0.85) | |
| Federal Poverty Level | |||
| 400%+ | 4795 | 3.30 (0.61) | NA |
| 300–399% | 1876 | 4.11 (0.87) | |
| 200–299% | 2253 | 3.25 (0.62) | |
| 100–199% | 2706 | 3.38 (0.67) | |
| Less than 100% | 2793 | 4.20 (0.71) | |
| State EI eligibility criteria | |||
| Broad | 5069 | 2.95 (0.46)* | Moderate > Broad |
| Moderate | 2306 | 5.06 (0.91) | |
| Narrow | 4972 | 3.49 (0.47) | |
| Parent education | |||
| Less than high school | 1030 | 1.98 (0.68) | NA |
| High school | 2358 | 3.26 (0.73) | |
| More than high school | 10,187 | 4.09 (0.41) | |
| Family Centered Care | |||
| Yes | 10,679 | 2.87 (0.00) | NA |
| No | 3607 | 3.61 (0.01) | |
| Insurance | |||
| Private | 8670 | 3.31 (0.42) | NA |
| Public | 5118 | 4.24 (0.52) | |
| None | 476 | 2.27 (0.85) |
Notes.
= p < .001;
= p < .01;
= p < .05;
= sub-groups differ p < .01;
Broad= state uses liberal cut-off scores on developmental assessments to determine which children require EI services; CSHCN = children with special healthcare needs; DM= developmental monitoring; DS= developmental surveillance; EI = Part C early intervention; IFSP = Individualized Family Service Plan; Moderate = state uses moderately strict cut-off scores on developmental assessments to determine which children require EI services; Narrow= state uses very strict cut-off scores on developmental assessments to determine which children require EI services; SES = socio-economic status.
Analytic methods
Authors estimated national IFSP receipt percentages and stratified them by the key variables considered in this study (Tables 1 and 2). To detect proportional differences across years and between groups, authors conducted Rao Scott χ2 tests. Furthermore, authors determined the relationship between DM and DS on EI receipt by binary logistic regression, with IFSP receipt as the outcome variable; CSHCN and individual, household/sociodemographic, and Part C variables displaying significant differences on χ2 tests were included as independent variables in final models. For analyses, authors used the survey package available in the R domain and accounted for design effects via NCHS recommended procedures.39–42 All analyses used datasets with imputed SES data, and were weighted and stratified per published recommendations. Statistical significance is set at p < .05.
Results
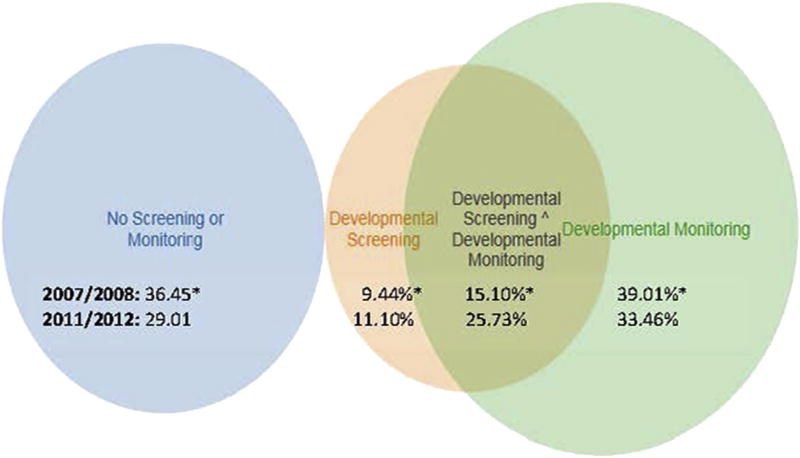
In 2007/2008, according to parent report, about 36% of children received DM alone, 9% received DS alone, 15% received both, and 39% received neither (Fig. 1). In 2011/2012, about 29% of children received DM alone, 12% received DS alone, 26% received both, and 33% received neither (Fig. 1). χ2 tests indicated that all developmental surveillance changes across time were statistically significant (p < .05).
Fig. 1.
Percentage of children in the United States ages 10 months to 3 years who received developmental monitoring and/or screening according to parent report in 2007/2008 and 2011/2012. Notes. * = statistically significant change in percentages across years, p < .001. All percentages are estimates accounting for complex survey weighting and stratification as recommended by the National Survey of Children's Health (NSCH 2007/2008 [top rows]; 2011/2012 [bottom rows]).
Tables 1 and 2 show NSCH weighted and stratified frequencies of IFSP receipt by major variables for 2007/2008 and 2011/2012, respectively. In 2007/2008, an estimated 396,522 children had an IFSP (estimated 11,562,957 children with no IFSP) and in 2011/2012, an estimated 408,175 children had an IFSP (estimated 10,832,367 children with no IFSP). These results yielded estimated national IFSP receipt prevalence, according to parent report, of 3.32% and 3.64%, respectively. During both periods, estimated IFSP receipt prevalence was higher for children receiving both DM and DS (8.38% in 2007/2008; 6.47% in 2011/2012) compared to children receiving no DM or DS (1.31% in 2007/2008; 1.92% in 2011/2012), DM alone (2.74% in 2007/2008; 2.70% in 2011/2012), or DS alone (3.59% in 2007/2008; 3.09% in 2011/2012) (for both time frames, p < .05). Estimated IFSP receipt for CSHCN (19.78% in 2007/2008; 16.72% in 2011/2012) was higher than for children who were not identified as CSHCN (1.31% in 2007/2008; 2.11% in 2011/2012) (for both time frames, p < .05).
In 2007/2008, but not 2011/2012, estimated IFSP receipt prevalence was higher for males (4.23%) than females (2.34%); for children who had public insurance (4.96%) compared to those with private (2.54%) or no insurance (2.09%); and for children without family centered care (4.51%) compared to those with (2.22%) (p < .05). In 2011/2012, but not 2007/2008, prevalence was higher for children in states with moderate eligibility criteria (5.06%) compared to those with broad (2.95%) or narrow (3.49%) criteria (p < .05).
Table 3 presents adjusted regression models for 2007/2008 and 2011/2012. In 2007/2008, estimated IFSP receipt was more likely for (a) children who received DM and DS (aOR: 6.25), DS alone (aOR: 2.48), and DM alone (aOR: 2.41) compared to children receiving no DM or DS; (b) CSHCN (aOR: 16.03) compared to children not identified as CSHCN; and (c) children with public (aOR = 1.67) and private (aOR = 1.67) compared to no uninsured children. Further, IFSP receipt was lower for children without family centered care compared to those with (aOR = 0.41). In 2011/2012, estimated IFSP receipt was more likely for (a) children who received DM and DS (aOR: 2.94) compared to children receiving no DM or DS; (b) CSHCN (aOR: 7.79) compared to children not identified as CSHCN; and (c) moderate eligibility category (aOR= 1.73) compared to broad. For both years, comparison of confidence intervals indicates substantial overlap for most variables, except CSHCN status.
Table 3.
Adjusted odds of IFSP receipt for U.S. children ages 10 months to 3 years in 2007/2008 and 2011/2012.
| Variable | 2007/2008 | 2011/2012 |
|---|---|---|
| Developmental Surveillance Method | ||
| No DM or DS | Reference | Reference |
| DM and DS | 6.25 (2.93–13.32)*** | 2.94 (1.56–5.52)** |
| DS alone | 2.48 (1.02–5.20)* | 1.23 (0.69–2.42) |
| DM alone | 2.41 (1.11–5.20)* | 1.71 (0.63–4.42) |
| CSHCN | ||
| No | Reference | Reference |
| Yes | 16.03 (11.25–29.69)*** | 7.79 (5.30–11.47)*** |
| State eligibility criteria | ||
| Broad | Reference | Reference |
| Moderate | NA | 1.73 (1.04–2.89)* |
| Narrow | NA | 1.17 (0.76–1.81) |
| Gender | ||
| Male | Reference | Reference |
| Female | 0.65 (0.40–1.04) | NA |
| Family Centered Care | ||
| Yes | 0.41 (0.24–0.72)** | NA |
| No | Reference | |
| Insurance | ||
| Private | Reference | Reference |
| Public | 1.67 (1.38–5.03) | NA |
| None | 1.67 (0.99–2.79) | NA |
Notes.
= p < .05;
= p < .01;
= p < .001;
Broad = state uses liberal cut-off scores on developmental assessments to determine which children require EI services; CSHCN = children with special healthcare needs; DM= developmental monitoring; DS = developmental surveillance; EI = Part C early intervention; IFSP = Individualized Family Service Plan; Moderate = state uses moderately strict cut-off scores on developmental assessments to determine which children require EI services; Narrow = state uses very strict cut-off scores on developmental assessments to determine which children require EI services.
Discussion
DM and DS are the initial methods by which many children with developmental delays and disabilities are identified for EI services.6 Currently, many groups recommend DM and/or DS, but there is very little research comparing the impacts of these distinct yet related approaches, alone or in tandem.37
This analysis suggests that when CHCPs both engage parents by eliciting developmental concerns (DM) and use a developmental screening tool (DS), more children are identified and connected with services than when a screener is used alone. However, eliciting those concerns without using a screener is also less successful in connecting children with EI. Unfortunately, the cross-sectional nature of this NSCH data prevents a firm conclusion regarding the temporal relationship between DM, DS and EI receipt. On the one hand, children may receive DM and DS in tandem leading to identification. Alternatively, DM and DS could occur at multiple points with one or the other flagging concerns at one time, and initiating a series of clinical inquiries post-concern. Future longitudinal research is necessary to better determine the longitudinal relationship between DM, DS, and EI receipt.
According to parent report here and similar to other findings,23 CHCPs are increasing their early identification practices—a very positive step toward helping children with developmental delays access the benefits of EI. This result was driven primarily by statistically significant increases in DM and DS in tandem and to a lesser degree by increases in DS alone. There were also statistically significant decreases in the proportion of children who received DM alone and in the proportion of children who received neither DM nor DS.
Our results may have implications for developmental surveillance policy and for future research efforts. Since the AAP's 2006 recommendations on DS and surveillance, there has been an increasing number of published reports on the utility of DS for identifying children who need EI.13–26,37 There has also been some research into the relative usefulness of DM compared to DS, indicating that DS is superior to DM at identifying children who need to receive EI.37 Much of the research, however, attends solely to DS and has not focused on current recommendations that DM and DS be used in tandem.6
It is possible that an unintended consequence of research focusing on and promotion of DS is that CHCPs may infer that DM is less important or not effective. This interpretation is bolstered by the finding that the percentage of parents reporting their children received DS alone increased from 9% to 12% across time periods. In reality, CHCPs should use DM and DS in tandem, as well as educate themselves on the strengths and limitations of available screeners.6 A federal initiative promoting DM and DS, Birth to Five: Watch Me Thrive!,44 provides a helpful compendium of screening tools. Furthermore, parents and care providers can partner with CHCPs to increase DM in tandem with DS in health care settings using free materials offered by the Centers for Disease Control and Prevention's Learn the Signs. Act Early.45,46
Limitations
This study is limited in a number of ways. Foremost, relying on caregiver reports may have led to IFSP receipt estimates higher than official Part C estimates.43 However, official estimates are based on a single point in time, and IFSP receipt is closer to 5% when collected for an entire year.47 Thus, our estimates fall between official point-in-time and entire-year data. Furthermore, these data do not capture fine-grained clinical processes that may influence the accurate identification of children who need EI (e.g., some CHCPs may provide DM and DS only for the most easily identified children). Additionally, caregiver recollection of receiving and filling out a screener (DS) may be more accurate than recollection of answering a few questions about development (DM) nested among many questions asked by CHCPs. Moreover, the NSCH DM and DS items are single item measures that minimally represent various monitoring and screening techniques available to CHCPs. Finally, our data are cross-sectional and the temporal relationship between surveillance and EI receipt cannot be firmly established.
Future research
Our findings have important implications for research. First, our current understanding of DM practices is extremely limited. While DS has a clear operational definition and a wide research base, DM is much more imprecise and may represent a wide range of unexplored CHCP behaviors. Furthermore, CHCPs may conduct DS by asking questions that appear like DM to caretakers. Future research should seek to better understand how CHCPs perform developmental surveillance. Second, focusing solely on DS likely leads to an incomplete understanding of developmental surveillance. Thus, research on DS rates should expand to consider the joint role of DM and DS.23 Finally, there is a need for research on the effectiveness of developmental surveillance methods within communities in linking identified children to EI services. This will require a shift from considering effectiveness from a psychometric perspective to an implementation science perspective and should be a focus of future research.
Conclusion
Current policy and research on early identification of children with developmental disabilities and delays focus strongly on the importance of DS, with less emphasis on DM. Children who, according to parent report, received DM and DS had the greatest odds of EI receipt compared to children receiving DM only, DS only, or no DM or DS. Rates of DS alone and DM and DS in tandem are increasing, while rates of DM alone and no DM or DS are decreasing. Results of this study indicate that the receipt of DM and DS in tandem may identify more children with developmental delays and disabilities who need EI than do either DM or DS separately.
Acknowledgments
Funding sources
This research was funded in part by a Policy Research Fellowship sponsored by the University of South Carolina: Disability Research and Dissemination Center in collaboration with the Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, Learn the Signs. Act Early. Team.
Abbreviations
- CHCP
Child health care provider
- DM
Developmental monitoring
- DS
Developmental screening
- EI
Early intervention
- IFSP
Individualized Family Service Plan
- NSCH
National Survey of Children's Health
Footnotes
Conflicts of interest
The authors have no conflicts of interest.
Financial disclosure
The authors have indicated they have no financial relationships relevant to this article to disclose.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributors statement
What's known on this subject: Developmental monitoring (DM) and screening (DS) should co-occur to identify children for early intervention (EI) (American Academy of Pediatrics [AAP], 2006). Most published evidence focuses on DS; relatively little is published on DM or on DM and DS occurring together.
What this study adds: This study provides the first national data showing that DM and DS together predict EI receipt. Contrary to available research focused primarily on DS, this study shows that neglecting DM may limit efforts to identify children who need EI.
References
- 1.Guralnick MJ. The next decade of research on the effectiveness of early intervention. Except Child. 1991;58(2):174. doi: 10.1177/001440299105800209. [DOI] [PubMed] [Google Scholar]
- 2.Guralnick MJ. Effectiveness of early intervention for vulnerable children: a developmental perspective. Am J Ment Retard. 1997;102(4):319–345. doi: 10.1352/0895-8017(1998)102<0319:eoeifv>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 3.Boulet S, Boyle C, Schieve L. Health care use and health and functional impact of developmental disabilities among US children, 1997–2005. Arch Pediatr Adolesc Med. 2009;163(1):19–26. doi: 10.1001/archpediatrics.2008.506. [DOI] [PubMed] [Google Scholar]
- 4.Boyle C, Boulet S, Schieve L, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127(6):1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg S, Zhang D, Robinson C. Prevalence of developmental delays and participation in early intervention services for young children. Pediatrics. 2008;121(6):e1503–e1509. doi: 10.1542/peds.2007-1680. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. Council on children with disabilities, section on developmental behavioral pediatrics, bright futures steering committee, medical home initiatives for children with special needs project advisory committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–420. doi: 10.1542/peds.2006-1231. [DOI] [PubMed] [Google Scholar]
- 7.Bright futures. Guidelines for Health Supervision of Infants, Children, and Adolescents. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 8.Zima BT, Murphy JM, Scholle SH, et al. National quality measures for child mental health care: background, progress, and next steps. Pediatrics. 2013;131:S38–S49. doi: 10.1542/peds.2012-1427e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagnato S, Smith, Jones J, Matesa M, et al. Research foundations for using clinical judgment (informed opinion) for early intervention eligibility determination. Cornerstones. 2006;2(3):1–14. [Google Scholar]
- 10.Bagnato S, McKeating-Esterle E, Fevola A, et al. Valid use of clinical judgment (informed opinion) for early intervention eligibility: evidence base and practice characteristics. Infants Young Child. 2008;21(4):334–349. [Google Scholar]
- 11.Glascoe F, Dworkin P. Obstacles to effective developmental surveillance: errors in clinical reasoning. J Dev Behav Pediatr. 1993;14(5):344–349. [PubMed] [Google Scholar]
- 12.Glascoe F, Dworkin P. The role of parents in the detection of developmental and behavioral problems. Pediatrics. 1995;95(6):829–836. [PubMed] [Google Scholar]
- 13.Sand N, Silverstein M, Glascoe F, et al. Pediatricians' reported practices regarding developmental screening: do guidelines work? Do they help? Pediatrics. 2005;116(1):174–179. doi: 10.1542/peds.2004-1809. [DOI] [PubMed] [Google Scholar]
- 14.Ben-Sasson A, Habib S, Tirosh E. Feasibility and validity of early screening for identifying infants with poor social-communication development in a well-baby clinic system. J Pediatr Nurs. 2014;29(3):238–247. doi: 10.1016/j.pedn.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Bethell C, Reuland C, Schor E, et al. Rates of parent-centered developmental screening: disparities and links to services access. Pediatrics. 2011;128(1):146–155. doi: 10.1542/peds.2010-0424. [DOI] [PubMed] [Google Scholar]
- 16.Earls M, Shackelford Hay S. Setting the stage for success: implementation of developmental and behavioral screening and surveillance in primary care practice-the North Carolina Assuring Better Child Health and Development (ABCD) Project. Pediatrics. 2006;118(1):e183–e188. doi: 10.1542/peds.2006-0475. [DOI] [PubMed] [Google Scholar]
- 17.Hix-Small H, Marks K, Squires J, et al. Impact of implementing developmental screening at 12 and 24 months in a pediatric practice. Pediatrics. 2007;120(2):381–389. doi: 10.1542/peds.2006-3583. [DOI] [PubMed] [Google Scholar]
- 18.Kavanagh J, Gerdes M, Sell K, Jimenez M, Guevara J. An Integrated Approach to Supporting Child Development. PolicyLab: Center to Bridge Research Practice and Policy; 2012. [Accessed July 20, 2015]. Summer http://coloradoabcd.org/files/5613/8117/9045/policylab_e2a_summer2012_series.pdf. [Google Scholar]
- 19.King T, Tandon S, Macias M, et al. Implementing developmental screening and referrals: lessons learned from a national project. Pediatrics. 2010;125(2):350–360. doi: 10.1542/peds.2009-0388. [DOI] [PubMed] [Google Scholar]
- 20.Marks K, Hix-Small H, Clark K, et al. Lowering developmental screening thresholds and raising quality improvement for preterm children. Pediatrics. 2009;123(6):1516–1523. doi: 10.1542/peds.2008-2051. [DOI] [PubMed] [Google Scholar]
- 21.Morelli D, Pati S, Butler A, et al. Challenges to implementation of developmental screening in urban primary care: a mixed methods study. BMC Pediatr. 2014;14(1):16. doi: 10.1186/1471-2431-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinto-Martin J, Dunkle M, Earls M, et al. Developmental stages of developmental screening: steps to implementation of a successful program. Am J Publ Health. 2005;95(11):1928–1932. doi: 10.2105/AJPH.2004.052167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Radecki L, Sand-Loud N, O'Connor K, et al. Trends in the use of standardized tools for developmental screening in early childhood: 2002–2009. Pediatrics. 2011;128(1):14–19. doi: 10.1542/peds.2010-2180. [DOI] [PubMed] [Google Scholar]
- 24.Schonwald A, Huntington N, Chan E, et al. Routine developmental screening implemented in urban primary care settings: more evidence of feasibility and effectiveness. Pediatrics. 2009;123(2):660–668. doi: 10.1542/peds.2007-2798. [DOI] [PubMed] [Google Scholar]
- 25.Sices L. Developmental Screening in Primary Care: the Effectiveness of Current Practice and Recommendations for Improvement. Commonwealth Fund; 2007. [Google Scholar]
- 26.Roux A, Herrera P, Wold C, et al. Developmental and autism screening through 2-1-1: reaching underserved families. Am J Prev Med. 2012;43(6):S457–S463. doi: 10.1016/j.amepre.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Limbos M, Joyce D. Comparison of the ASQ and PEDS in screening for developmental delay in children presenting for primary care. J Dev Behav Pediatr. 2011;32(7):499–511. doi: 10.1097/DBP.0b013e31822552e9. [DOI] [PubMed] [Google Scholar]
- 28.Rydz D, Srour M, Oskoui M, et al. Screening for developmental delay in the setting of a community pediatric clinic: a prospective assessment of parent-report questionnaires. Pediatrics. 2006;118(4):e1178–e1186. doi: 10.1542/peds.2006-0466. [DOI] [PubMed] [Google Scholar]
- 29.Sices L, Stancin T, Kirchner H, et al. PEDS and ASQ developmental screening tests may not identify the same children. Pediatrics. 2009;124(4):e640–e647. doi: 10.1542/peds.2008-2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackrides P, Ryherd S. Screening for developmental delay. Am Fam Physician. 2011;84(5):544–549. [PubMed] [Google Scholar]
- 31.Macy M. The evidence behind developmental screening instruments. Infants Young Child. 2012;25(1):19–61. [Google Scholar]
- 32.Marks K, LaRosa A. Understanding developmental-behavioral screening measures. Pediatr Rev. 2012;33(10):448–457. doi: 10.1542/pir.33-10-448. [DOI] [PubMed] [Google Scholar]
- 33.Williams J, Holmes C. Improving the early detection of children with subtle developmental problems. J Child Health Care. 2004;8(1):34–46. doi: 10.1177/1367493504041852. [DOI] [PubMed] [Google Scholar]
- 34.Marks K, Glascoe F, Aylward G, et al. The thorny nature of predictive validity studies on screening tests for developmental-behavioral problems. Pediatrics. 2008;122(4):866–868. doi: 10.1542/peds.2007-3142. [DOI] [PubMed] [Google Scholar]
- 35.Macy M, Marks K, Towle A. Missed, misused, or mismanaged: improving early detection systems to optimize child outcomes. Top Early Childh. 2014;34(2):94–105. [Google Scholar]
- 36.Bricker D, Macy M, Squires J, Marks K. Developmental Screening in Your Community: An Integrated Approach for Connecting Children with Services. Baltimore, MD: Paul H. Brookes Publishing Company; 2013. [Google Scholar]
- 37.Guevara J, Gerdes M, Localio R, et al. Effectiveness of developmental screening in an urban setting. Pediatrics. 2013;131(1):30–37. doi: 10.1542/peds.2012-0765. [DOI] [PubMed] [Google Scholar]
- 38.Individuals with Disabilities Education Act. 2004;20 U.S.C. § 1400. [Google Scholar]
- 39.Blumberg S, Foster E, Frasier A, et al. Design and operation of the national survey of Children's health, 2007. Vital Health Stat 1. 2012;55:1–149. [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. [Accessed 20 July 2015];2011–2012 National Survey of Children's Health frequently asked questions. http://www.cdc.gov/nchs/slaits/nsch.htm.
- 41.Lumley T. Complex Surveys: A Guide to Analysis Using R. John Wiley and Sons; 2011. [Google Scholar]
- 42.Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9(1):1–19. [Google Scholar]
- 43.Early Childhood Technical Assistance Center. [Accessed October 22, 2015];Part C national program data. http://ectacenter.org/partc/partcdata.asp#appropriations; 5 May 2015.
- 44.Department of Health and Human Services. [Accessed 20 July 2015];Birth to Five: Watch Me Thrive! www.acf.hhs.gov/programs/ecd/child-health-development/watch-me-thrive.
- 45.Graybill E, Self-Brown S, Lai B, et al. Addressing disparities in parent education: examining the effects of Learn the Signs/Act Early parent education materials on parent outcomes. Early Child Educ J. 2014 https://doi.org/10.1007/s10643-014-0680-3.
- 46.Centers for Disease Control and Prevention. [Accessed 20 July 2015];Learn the Signs. Act Early. www.cdc.gov/ncbddd/actearly/freematerials.html.
- 47.Greer M, Noyes D, Barger B, Rice C. Data Presented at the Association for University Centers on Disabilities 2014 Meeting. Washington D.C: Early concern to early intervention: state of the data. Accessed 20 July 2015. [Google Scholar]