Abstract
Background Imaging of the triangular fibrocartilaginous complex (TFCC) remains difficult, as no single imaging modality demonstrates perfect sensitivity and specificity.
Purpose This study performs a meta-analysis of multiple previous publications to guide noninvasive imaging selection for the diagnosis of TFCC injuries.
Methods A literature search was performed and conducted. Studies were included that compared the diagnostic accuracy of magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA), and computed tomography (CT)/computed tomographic arthrography (CTA) for the evaluation of TFCC injuries. All studies included either arthroscopic or open surgical findings as the “gold standard.” A meta-analysis was performed comparing the diagnostic accuracy of MRA, MRI, and CT for the detection of TFCC injuries.
Results Initial search returned 2,568 candidate articles. Studies were then reviewed and narrowed yielding a total of 28 independent studies (20 MRI, 9 MRA, 4 CT/CTA with some studies including multiple modalities) considered in the qualitative data synthesis. Pooling of the raw data in a meta-analysis demonstrated sensitivities of 0.76 (0.72–0.80), 0.78(0.70–0.84), and 0.89 (0.81–0.95) for MRI, MRA, and CT arthrogram, respectively, with specificities of 0.82 (0.77–0.86), 0.85 (0.77–0.92), and 0.89 (0.81–0.95), respectively. Additionally, across all imaging modalities, diagnostic accuracy was highest for central TFCC lesions versus peripheral lesions.
Conclusion This study represents the largest meta-analysis to date to compare multiple imaging modalities for the diagnosis of TFCC injuries. Pooled data demonstrated that CTA and MRA had statistically equivalent sensitivity and specificity for the diagnosis of TFCC injuries. Diagnostic accuracy was highest for central TFCC injuries.
Keywords: triangular fibrocartilaginous complex, MRI, computed tomographic arthrography, wrist pain, diagnosis
The cartilaginous–ligamentous stabilization mechanism of the ulnar wrist, termed as the triangular fibrocartilaginous complex (TFCC), represents a frequently injured structure that results in ulnar-sided wrist pain and instability. 1 2 The TFCC acts to stabilize the distal radioulnar joint particularly in pronation and supination. 2 3 Injuries to this complex may result in permanent joint laxity and pain possibly requiring operative intervention. 4
Imaging of the TFCC remains difficult, as no single imaging modality, to date, has demonstrated perfect sensitivity and specificity. Traditionally, arthroscopy or open surgical diagnosis has been considered the gold standard but represents invasive techniques that are only employed when clinical suspicion is high. 5 6 In an effort to diagnose these injuries and guide treatment in less invasive manners, clinicians have employed magnetic resonance imaging (MRI), magnetic resonance arthrogram (MRA), computed tomography (CT), CT arthrograms (CTAs), ultrasound, and X-rays. MRI/MRA has emerged as a leading method to diagnose the presence of ligamentous injuries because of its increased soft tissue fidelity and reported ability to localize the injury within the TFCC. 7 To that end, multiple studies have examined MRI/MRA along with the more traditional imaging methods. Over the past two decades, studies have assessed the diagnostic accuracy of the aforementioned imaging modalities for the diagnosis of TFCC injuries. Unfortunately, the reported data are often varied and without clear consensus when comparing individual studies. While several reviews have been published, they report a wide array of results with large ranges in their operational statistics. 8 9 10 11
Previous meta-analyses from a single group examined the diagnostic accuracy of MRI versus MRA and X-ray arthrography separately. 12 13 While these studies provide pooled statistics supporting the use of MRA (high sensitivity and specificity) as the radiographic method of choice, the analyses did not include comparisons between multiple imaging modalities (CT vs. MRI/MRA) and did not evaluate the diagnostic accuracy of site-specific injuries. The presented study aims to address these concerns to guide clinicians in diagnostic imaging selection for suspected TFCC injuries. The analysis reports on the diagnostic accuracy of MRI/MRA, CT, and CTA with regard to their overall utility in the evaluation of global TFCC injury and more specifically in a site-specific injury manner.
Methods
Literature Search
The search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. 14 The search was conducted utilizing the following databases: the Cochrane Bone, Joint and Muscle Trauma Specialized Register, the Cochrane Central Register of Controlled Trials, MEDLINE, BioMed Central, PubMed, and Embase electronic search engines. The studies examined were limited to those published in or after 1989 in English. A systematic electronic search was conducted by a single author. In general, no manual search of recently published articles in pertinent journals was undertaken. A manual search of recent similar meta-analyses was conducted to ensure no studies were missed. The corresponding authors were not contacted for additional information. The first author performed the primary study selection. Once complete this selection was validated in duplicate by the second author. The senior author confirmed the final selection of articles. Screening was initially performed by reading the title and abstract. Full text was only examined for inclusion if the tile and abstract were insufficient. The full text of the articles was not always assessed. The quality assessment of included studies was performed using the revised Quality Assessment of Diagnostic Accuracy Studies 2 tool 15 by a single reviewer. Risk of bias and applicability was rated as low, high, or unclear.
Inclusion/Exclusion Criteria
Studies were included that compared the diagnostic accuracy of MRI/MRA, and CT with and without arthrography for the evaluation of TFCC injuries. All studies must have included either arthroscopic or open surgical findings as the “gold standard.” All study design types were eligible and exclusion was not performed on the basis of methodological quality.
Data Extraction and Synthesis
All data was extracted by author and independently verified by a second reviewer in series. The data extracted included participants, diagnostic imaging modality utilized, sample size, bias, diagnostic sensitivity and specificity, frequencies of true-positive, true-negative, false-negative, and false-positive findings. For all studies, reported raw data was utilized to calculate the summary statistics de novo. If the data was unable to be calculated, the study was excluded. Studies where the raw data was parsed and reported in a site-specific manner were analyzed for both TFCC injury in general and later for site specificity.
Outcome Measures
The primary outcome measure was the sensitivity and specificity for each individual imaging modality with corresponding 95% confidence intervals.
Results
Search Results
The search results are demonstrated in Fig. 1 . In total 2,568 articles were identified in the Cochrane Bone, Joint and Muscle Trauma Specialized Register; the Cochrane Central Register of Controlled Trials, MEDLINE, BioMed Central, PubMed, and Embase electronic search engines. Of these, 1,712 were removed because they were either non-English or redundant articles among the different searches. These yielded 856 articles that were screened based on their abstracts and titles for relevance, completeness, and use of either arthroscopy or open wrist surgery for diagnostic confirmation. One-hundred sixteen articles were selected from this group and their full text evaluated. Full-text articles were then screened similarly for relevance, completeness, and use of either arthroscopy or open wrist surgery for diagnostic confirmation with 28 total independent studies included in the final analysis. Within these 28 studies, 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 20 studies evaluated MRI, 9 studies evaluated MRA, and 4 studies evaluated CTA for the diagnosis of TFCC injuries.
Fig. 1.
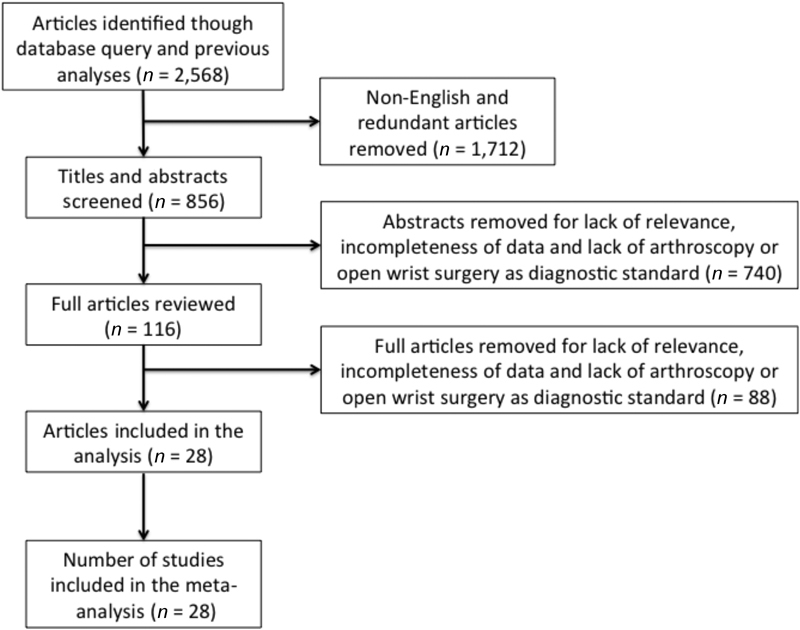
Study selection flow chart.
Population Characteristics
The pooled population represented a total of 1,155 wrists (754, 232 and 169 for the MRI, MRA, and CTA cohorts, respectively). The mean age was 35.7 years with a standard deviation of 5.9 years. The mean age was not documented in four studies and one study was performed on cadaveric specimens. The time from injury until diagnosis was either not documented or highly variable among the studies preventing analysis of this facet. The years of publication of the examined studies ranged from 1989 to 2015.
Analysis
Forest plots for the individual included studies with true positives, false positives, false negatives, true negatives, sensitivity, and specificity with 95% confidence intervals were extracted for the listed studies. Fig. 2 demonstrates the summary statistics for MRI in the diagnosis of TFCC injuries. Individual sensitivity ranged from 0.52 to 1.00 and specificity from 0.00 to 1.00. Of note, in two studies the specificity was not calculable secondary to a lack of negative findings. Fig. 3 demonstrates the summary statistics for MRA and CTA data, respectively. For MRA ( Fig. 3 ), the sensitivity ranged from 0.48 to 1.00 and the specificity ranged from 0.50 to 1.00. For the CTA ( Fig. 3 ), the sensitivity ranged from 0.82 to 1.00 and the specificity ranged from 0.42 to 1.00. Pooling of the raw data in a meta-analysis demonstrated sensitivities of 0.76 (0.72–0.80), 0.78 (0.70–0.84), and 0.89 (0.81–0.95) for MRI, MRA, and CTA, respectively, with specificities of 0.82 (0.77–0.86), 0.85 (0.77–0.92), and 0.89 (0.81–0.95), respectively ( Fig. 4 ). In analyzing the data for the evaluation of peripheral versus central tears, three studies met criteria in terms of identification of TFCC injury location (central vs peripheral) and were confirmed with either arthroscopy or open surgical exploration. 16 17 18 Detection of central lesions occurred with a sensitivity of 0.92 (0.84–0.97) and a specificity of 0.93 (0.85–0.97), whereas peripheral lesions occurred with a sensitivity of 0.71 (0.55–0.84) but with a specificity of 0.98 (0.94–0.99) ( Fig. 5 ).
Fig. 2.
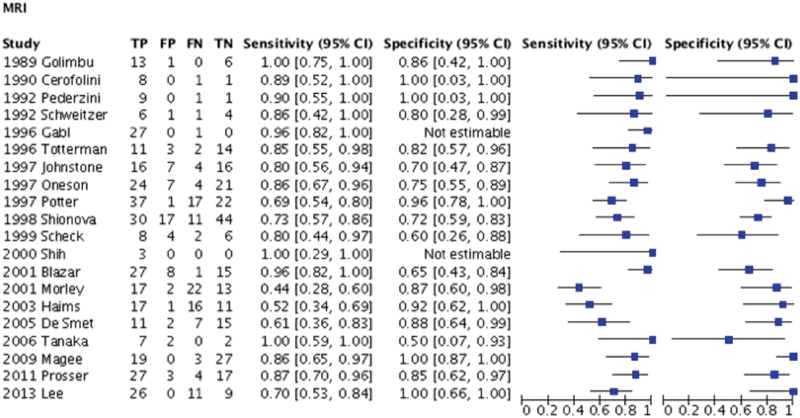
Forest plot of the diagnostic statistics of individual studies using MRI for the diagnosis of triangular fibrocartilaginous complex tears. CI, confidence interval; FN, false negatives; FP, false positives; MRI, magnetic resonance imaging; TN, true negatives; TP, true positives.
Fig. 3.
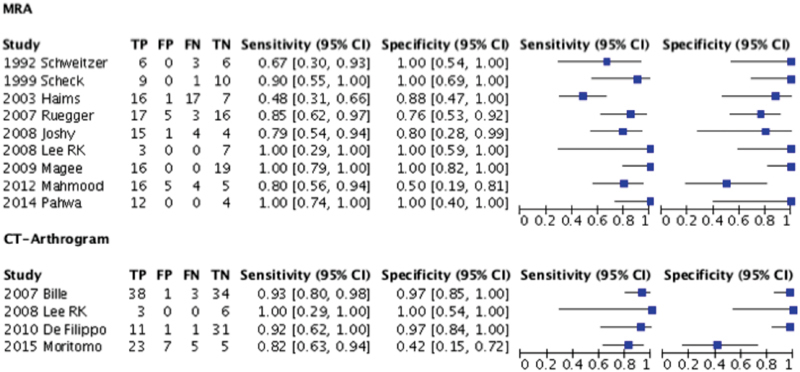
Forest plots of the diagnostic statistics of individual studies using MRA versus CT arthrogram for the diagnosis of triangular fibrocartilaginous complex tears. CI, confidence interval; CT, computed tomography; FN, false negatives; FP, false positives; FN, false negatives; MRA, magnetic resonance arthrography; TN, true negatives; TP, true positives.
Fig. 4.
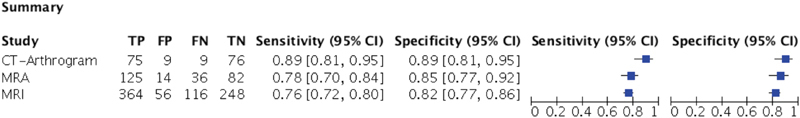
Summary forest plots of the summary diagnostic statistics of MRI, MRA, and CT arthrograms for the diagnosis of triangular fibrocartilaginous complex tears. CI, confidence interval; CT, computed tomography; FN, false negatives; FP, false positives; MRA, magnetic resonance arthrography; MRI, magnetic resonance imaging; TN, true negatives; TP, true positives.
Fig. 5.
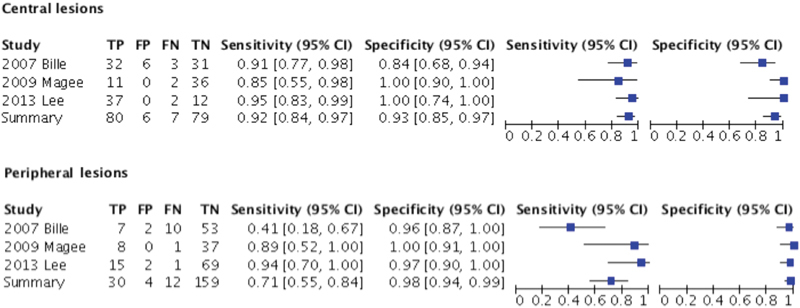
Forest plots comparing the performance of imaging modalities for the diagnosis of peripheral versus central triangular fibrocartilaginous complex tears. CI, confidence interval; FN, false negatives; FP, false positives; TN, true negatives; TP, true positives.
Discussion
This study examines the operating characteristics of MRI, MRA, and CTA for the diagnosis of TFCC injuries as derived from a meta-analysis of multiple previous studies. The pooled analysis of the study indicates that MRA provides improved diagnostic accuracy over standard MRI in terms of both sensitivity and specificity. This finding is in agreement with previous meta-analyses that examined the two modalities in head-to-head comparisons. 12 17 19 Pooled sensitivities and specificities reported in this study of 0.78 and 0.85 for MRA and 0.76 and 0.82 for MRI ( Fig. 3 ) are similar to those reported by Smith et al 12 being within a similar margin of error despite the inclusion of nine more studies. CTA demonstrates statistically similar sensitivity and specificity, as compared with MRA, for the diagnosis of TFCC injuries. Both arthrographic imaging techniques (MRA and CTA) provide improved operating characteristics over the nonarthrographic techniques (MRI/CT). This improved sensitivity likely stems from the enriched delineation of soft tissues provided with the introduction of contrast material into the joint space. 16 20 This study finds that MR does not inherently provide better diagnostic accuracy over CT even though MRI is traditionally viewed as better for the identification of soft tissue lesions of the wrist. 21 Both MRI and MRA had improved specificity over sensitivity and thus were more adept at excluding a TFCC injury in the absence of one; whereas CTA had similar sensitivity and specificity indicating that CTA was similarly able to exclude TFCC injuries when one is not present as to identify an injury when one is present. This finding is congruent with previous studies that have proposed CTA as a viable alternative to MR-based imaging for ulnar-sided wrist pain. 16 22 23 24
To further characterize the operating statistics of radiologic modalities for the diagnosis of TFCC injuries, this study examines the diagnosis of central versus peripheral TFCC injuries ( Fig. 4 ). TFCC injuries of the central portion of the TFCC are diagnosed with a significantly higher sensitivity than peripheral tears, however, with a similar specificity. The ability to accurately identify central lesions over peripheral lesions may stem from the lack of contrast that is seen ulnarly during standard arthrographic imaging. Some authors have proposed that allowing contrast to pool ulnarly may improve the accuracy for arthrography of peripheral lesions as the ability to visualize contrast flowing over the peripheral TFCC fibers may enhance visualization. 6 16 20 Historically within the literature, the diagnosis of peripheral tears via radiographic methods has had reduced sensitivity and specificity. 6 25 The specificity of peripheral lesions is similar among central and peripheral lesions when pooled within this study, in contrast to the historic literature. 6 25 It is important to note that among the four included studies examining site-specific lesions, the reported sensitivities for peripheral lesions by Bille et al 2 are significantly below those of the other three. This skews the pooled sensitivity lower than it would be with the exclusion of this study possibly resulting in a pooled statistic that is below the true sensitivity. Also of note, peripheral lesions had a lower incidence of occurrence. Central lesions are documented in 87 out of 172 cases (51%) versus peripheral lesions that occur in 42 out of 205 cases (20%). Although this finding will affect the positive and negative predictive values, it should have no influence on the sensitivity and specificities of the diagnostic modality.
The present study identifies and suffers from several limitations in the methodology. The ability to radiographically diagnose TFCC injuries is both user and equipment dependent. Numerous studies have examined different hardware parameters and settings ranging from the strength of the coils used, 6 18 26 27 imaging protocols/sequences, 17 28 and the imaging plane used. 24 This study did not seek to standardize these parameters and thus variations among studies may relate to variations in these technical parameters. While it may seem that with advances in imaging technology that diagnostic accuracy would improve, this was not seen within the data. In fact, some of the worst diagnostic performers were the more modern studies and some of the best the older studies ( Fig. 2 ). Additionally, correct diagnosis of a TFCC injury on imaging is dependent on the ability of the reviewing radiologist and hand surgeon to accurately diagnose the presence or lack thereof of a TFCC injury. Studies have demonstrated that when comparing different end users of the imaging modalities, there are discrepancies in the diagnostic statistics. 16 25 29 While some studies accounted for this intraobserver variability, other did not, and this may explain the variability seen in studies even with newer technologies. Also, acute injuries to the joint may result in joint fluid within the area of injury acting as a “contrast medium.” As none of the papers cataloged the time from injury until time of imaging, it is difficult to determine if this may result in better operating characteristics in the acutely injured joint. Unfortunately, there is no feasible method to account for the lack of standardization in radiographic reading as this often represents a subjective process, especially when comparing across studies. Additionally, blinding of the studies was sometimes inconsistent or poorly documented, thus not all included studies were adequately blinded so as to prevent any bias from radiographic diagnosis from the arthroscopic/surgical confirmation.
This study found statistical diagnostic equivalence between MRA and CTA. This is relevant to the clinician as certain circumstances may favor the selection of one modality over the other. MR studies have advantages in that their utility expands beyond the diagnosis of TFCC injuries, but also includes other causes of ulnar-sided wrist pain that may be within the differential diagnosis. MR has been shown to be useful in the diagnosis of osteonecrosis, occult fractures, tendon inflammation/tears, synovitis, and joint fluid collections. 12 Therefore, MR allows the evaluation of multiple diagnostic end points within a single assessment. However, currently the best performing MRA methodologies often require 3 Tesla dedicated wrist coils to provide the quality images needed to be comparable with CT methods, 18 in addition to radiologists and hand surgeons who are familiar with reading these images. These requirements may result in decreased access to these diagnostic tools in some areas as well as increased cost. CTA generally requires a standard CT scanner that may be more easily read, more available, and at a lower cost 16 but with the added exposure to radiation fields. Additionally, arthrography represents an invasive procedure, whose risks may outweigh the added diagnostic benefit in both CT and MR modalities.
This study represents the largest meta-analysis and review to date to examine the role of MRI and MRA for the diagnosis of TFCC injuries, and the only study we are aware of to include CTA. Furthermore, this work examines the fidelity of detecting central versus peripheral lesions across all imaging modalities. There appeared to be operating equivalence in terms of sensitivity and specificity of the arthrographic techniques, which were superior to MRI alone without arthrography. These findings may help to guide clinicians in choosing the radiologic test when patients present with ulnar-sided wrist pain concerning for a TFCC injury. Given the similar equivalency between CTA and MRA found in this meta-analysis, this study recommends that the ultimate selection of diagnostic imaging tool occurs based on the patient's desire to undergo an invasive procedure, the ability of clinicians to read and accurately diagnose TFCC injuries via MRI and CT, and the availability of the appropriate machinery at individual institutions (e.g., dedicated 3T wrist coils).
Footnotes
Conflict of Interest None.
References
- 1.Abe Y, Tominaga Y. Ulnar-sided wrist pain due to isolated disk tear of triangular fibrocartilage complex within the distal radioulnar joint: two case reports. Hand Surg. 2011;16(02):177–180. doi: 10.1142/S0218810411005308. [DOI] [PubMed] [Google Scholar]
- 2.Bille B, Harley B, Cohen H. A comparison of CT arthrography of the wrist to findings during wrist arthroscopy. J Hand Surg Am. 2007;32(06):834–841. doi: 10.1016/j.jhsa.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Blazar P E, Chan P S, Kneeland J B, Leatherwood D, Bozentka D J, Kowalchick R. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg Am. 2001;26(04):742–748. doi: 10.1053/jhsu.2001.24966. [DOI] [PubMed] [Google Scholar]
- 4.Cerofolini E, Luchetti R, Pederzini L et al. MR evaluation of triangular fibrocartilage complex tears in the wrist: comparison with arthrography and arthroscopy. J Comput Assist Tomogr. 1990;14(06):963–967. doi: 10.1097/00004728-199011000-00018. [DOI] [PubMed] [Google Scholar]
- 5.De Filippo M, Pogliacomi F, Bertellini A et al. MDCT arthrography of the wrist: diagnostic accuracy and indications. Eur J Radiol. 2010;74(01):221–225. doi: 10.1016/j.ejrad.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 6.De Smet L. Magnetic resonance imaging for diagnosing lesions of the triangular fibrocartilage complex. Acta Orthop Belg. 2005;71(04):396–398. [PubMed] [Google Scholar]
- 7.Gabl M, Lener M, Pechlaner S, Judmaier W. The role of dynamic magnetic resonance imaging in the detection of lesions of the ulnocarpal complex. J Hand Surg [Br] 1996;21(03):311–314. doi: 10.1016/s0266-7681(05)80191-3. [DOI] [PubMed] [Google Scholar]
- 8.Golimbu C N, Firooznia H, Melone C P, Jr, Rafii M, Weinreb J, Leber C. Tears of the triangular fibrocartilage of the wrist: MR imaging. Radiology. 1989;173(03):731–733. doi: 10.1148/radiology.173.3.2813778. [DOI] [PubMed] [Google Scholar]
- 9.Haims A H, Schweitzer M E, Morrison W B et al. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology. 2003;227(03):701–707. doi: 10.1148/radiol.2273020398. [DOI] [PubMed] [Google Scholar]
- 10.Johnstone D J, Thorogood S, Smith W H, Scott T D. A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg [Br] 1997;22(06):714–718. doi: 10.1016/s0266-7681(97)80431-7. [DOI] [PubMed] [Google Scholar]
- 11.Joshy S, Ghosh S, Lee K, Deshmukh S C. Accuracy of direct magnetic resonance arthrography in the diagnosis of triangular fibrocartilage complex tears of the wrist. Int Orthop. 2008;32(02):251–253. doi: 10.1007/s00264-006-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee R K, Ng A W, Tong C S et al. Intrinsic ligament and triangular fibrocartilage complex tears of the wrist: comparison of MDCT arthrography, conventional 3-T MRI, and MR arthrography. Skeletal Radiol. 2013;42(09):1277–1285. doi: 10.1007/s00256-013-1666-8. [DOI] [PubMed] [Google Scholar]
- 13.Lee Y H, Choi Y R, Kim S, Song H T, Suh J S. Intrinsic ligament and triangular fibrocartilage complex (TFCC) tears of the wrist: comparison of isovolumetric 3D-THRIVE sequence MR arthrography and conventional MR image at 3 T. Magn Reson Imaging. 2013;31(02):221–226. doi: 10.1016/j.mri.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 14.Magee T. Comparison of 3-T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. AJR Am J Roentgenol. 2009;192(01):80–85. doi: 10.2214/AJR.08.1089. [DOI] [PubMed] [Google Scholar]
- 15.Mahmood A, Fountain J, Vasireddy N, Waseem M. Wrist MRI arthrogram v wrist arthroscopy: what are we finding? Open Orthop J. 2012;6:194–198. doi: 10.2174/1874325001206010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moritomo H, Arimitsu S, Kubo N, Masatomi T, Yukioka M. Computed tomography arthrography using a radial plane view for the detection of triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2015;40(02):245–251. doi: 10.1016/j.jhsa.2014.10.051. [DOI] [PubMed] [Google Scholar]
- 17.Morley J, Bidwell J, Bransby-Zachary M. A comparison of the findings of wrist arthroscopy and magnetic resonance imaging in the investigation of wrist pain. J Hand Surg [Br] 2001;26(06):544–546. doi: 10.1054/jhsb.2001.0645. [DOI] [PubMed] [Google Scholar]
- 18.Oneson S R, Timins M E, Scales L M, Erickson S J, Chamoy L. MR imaging diagnosis of triangular fibrocartilage pathology with arthroscopic correlation. Am J Roentgenol. 1997;168(06):1513–1518. doi: 10.2214/ajr.168.6.9168716. [DOI] [PubMed] [Google Scholar]
- 19.Pahwa S, Srivastava D N, Sharma R, Gamanagatti S, Kotwal P P, Sharma V. Comparison of conventional MRI and MR arthrography in the evaluation wrist ligament tears: a preliminary experience. Indian J Radiol Imaging. 2014;24(03):259–267. doi: 10.4103/0971-3026.137038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pederzini L, Luchetti R, Soragni O et al. Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy. 1992;8(02):191–197. doi: 10.1016/0749-8063(92)90036-b. [DOI] [PubMed] [Google Scholar]
- 21.Potter H G, Asnis-Ernberg L, Weiland A J, Hotchkiss R N, Peterson M G, McCormack R R., Jr The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am. 1997;79(11):1675–1684. doi: 10.2106/00004623-199711000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert R D. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother. 2011;57(04):247–253. doi: 10.1016/S1836-9553(11)70055-8. [DOI] [PubMed] [Google Scholar]
- 23.Rüegger C, Schmid M R, Pfirrmann C W, Nagy L, Gilula L A, Zanetti M. Peripheral tear of the triangular fibrocartilage: depiction with MR arthrography of the distal radioulnar joint. AJR Am J Roentgenol. 2007;188(01):187–192. doi: 10.2214/AJR.05.2056. [DOI] [PubMed] [Google Scholar]
- 24.Scheck R J, Romagnolo A, Hierner R, Pfluger T, Wilhelm K, Hahn K. The carpal ligaments in MR arthrography of the wrist: correlation with standard MRI and wrist arthroscopy. J Magn Reson Imaging. 1999;9(03):468–474. doi: 10.1002/(sici)1522-2586(199903)9:3<468::aid-jmri16>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 25.Schweitzer M E, Brahme S K, Hodler J et al. Chronic wrist pain: spin-echo and short tau inversion recovery MR imaging and conventional and MR arthrography. Radiology. 1992;182(01):205–211. doi: 10.1148/radiology.182.1.1727283. [DOI] [PubMed] [Google Scholar]
- 26.Shih J T, Hou Y T, Lee H M, Tan C M. Chronic triangular fibrocartilage complex tears with distal radioulna joint instability: a new method of triangular fibrocartilage complex reconstruction. J Orthop Surg (Hong Kong) 2000;8(01):1–8. doi: 10.1177/230949900000800102. [DOI] [PubMed] [Google Scholar]
- 27.Shionova K, Nakamura R, Imaeda T, Makino N. Arthrography is superior to magnetic resonance imaging for diagnosing injuries of the triangular fibrocartilage. J Hand Surg [Br] 1998;23(03):402–405. doi: 10.1016/s0266-7681(98)80068-5. [DOI] [PubMed] [Google Scholar]
- 28.Tanaka T, Yoshioka H, Ueno T, Shindo M, Ochiai N. Comparison between high-resolution MRI with a microscopy coil and arthroscopy in triangular fibrocartilage complex injury. J Hand Surg Am. 2006;31(08):1308–1314. doi: 10.1016/j.jhsa.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Totterman S M, Miller R J, McCance S E, Meyers S P. Lesions of the triangular fibrocartilage complex: MR findings with a three-dimensional gradient-recalled-echo sequence. Radiology. 1996;199(01):227–232. doi: 10.1148/radiology.199.1.8633149. [DOI] [PubMed] [Google Scholar]


