Abstract
Introduction Juvenile Idiopathic Arthritis (JIA) is the most common rheumatological condition in children and frequently affects the wrist. The roles for wrist arthroscopy and arthroscopic synovectomy (AS) in JIA are unclear. Our aim was to find the current evidence supporting its use.
Methods Systematic literature review of relevant publications from 1990 to present in the Cochrane Library, Clinical Knowledge Summaries, DynaMed, PEMSoft, NICE Guidance, MEDLINE, EMBASE, and PubMed.
Results We found no publications detailing the use of arthroscopy or AS specifically in patients with JIA involving the wrist. There is evidence that AS reduces pain, improves function, and induces remission in patients with rheumatoid arthritis resistant to medical management.
Discussion and Conclusion Although there is paucity in evidence for the use of AS in the wrists of patients with JIA, studies suggest it to be safe and effective, and could be applied to patients with refractive JIA. It is possible that early identification of patients suffering from JIA with extensive joint destruction and little symptoms could benefit from AS, delaying joint destruction and preserving function.
Keywords: juvenile idiopathic arthritis, wrist, arthroscopy, synovectomy
The term juvenile idiopathic arthritis (JIA) covers a group of arthritides of unknown etiology with onset before 16 years of age and persisting for 6 weeks or more in duration. JIA is the most common chronic rheumatic condition in children and one of the most common chronic conditions of childhood. 1 It has a yearly incidence of 2 to 20 cases and a prevalence of 16 to 150 cases per population of 100,000. 2
The International League of Associations for Rheumatology classification of JIA includes the following subtypes: systemic-onset arthritis, oligoarthritis, extended oligoarthritis, polyarthritis (rheumatoid factor [RF] negative), polyarthritis RF-positive arthritis, psoriatic arthritis, enthesitis-related arthritis, and undifferentiated arthritis. 3 Oligoarthritis is the most prevalent subtype (∼50%) with a peak age of onset between 2 to 4 years, and a female-to-male ratio of approximately 3:1. 4 The wrist joint is the fourth most commonly affected joint in JIA, both at onset and at 5-year follow-up, and conventional drug treatment may not be effective in preventing structural damage. 5 Early involvement of the wrist joint has been cited as a poor prognostic factor in JIA outcome. 6 The inability to control disease may result in significant morbidity, including pain, joint contracture, and permanent joint destruction. 4
Current practice in the assessment of the wrist in JIA includes clinical evaluation, imaging by ultrasound (US) or magnetic resonance imaging (MRI), and response to treatment. Current imaging modalities have clinically important limitations. MRI is considered to be the most sensitive imaging modality for detecting subclinical synovitis. 2 7 8 This had led to the development of MRI scoring systems assessing disease activity, particularly in the knee and wrist. 9 10 11 12 However, MRI may be unable to differentiate normal anatomical variants from inflammatory changes, especially in the growing skeleton. 13 14 US has some advantages over MRI for imaging inflammatory disease in the pediatric population, such as being noninvasive and quick to perform, but reproducibility is limited and operator-dependent. 15
The role of direct visualization using arthroscopy in JIA wrist evaluation is unclear. Over the past 30 years, direct imaging of the wrist joint with arthroscopy and arthroscopic synovectomy (AS), have become well-established techniques in adults with rheumatoid arthritis (RA). 16 AS is a minimally invasive procedure associated with low morbidity and an early return to work in adults. 16 Lee et al demonstrated that wrist AS in adults with RA provided pain relief, improvement of function, and long-term control of synovitis in 75% of patients not responding to medication. 17 Open wrist synovectomy for patients with JIA has been demonstrated to improve grip strength and range of motion (ROM), with outcomes not differing significantly from results following wrist synovectomy for adults with chronic arthritis. 18 For children, it is likely that minimally invasive procedures will be superior to open procedures in the radio- and midcarpal joints, with less scarring and loss of mobility. Additionally, it is possible that AS could delay the need for complex open surgery. Our aim was to ascertain and summarize the current evidence supporting its use in the pediatric population.
Methods
The Cochrane Library, Clinical Knowledge Summaries, DynaMed, PEMSoft, NICE Guidance, MEDLINE, EMBASE, and PubMed were searched for relevant publications from 1990 to present. MeSH terms used included arthritis, juvenile, arthroscopy, child, pediatrics, wrist and free text words arthroscopy, debridement, hand, juvenile arthritis, “juvenile idiopathic arthritis,” synovectomy, and wrist. Reference lists of retrieved articles were hand-searched for further relevant publications. No language restrictions were applied.
Results
Our search did not produce any publications detailing the use of arthroscopy or AS specifically in patients with JIA involving the wrist ( Table 1 ). Two authors expressed opinions that arthroscopy and AS of the wrist in JIA are safe and reliable and that patients can experience long-term comfort and improved function. 16 19 Their opinions, however, appear to have been based on personal experience from unpublished data (level V evidence). There have been no controlled studies to assess the benefits and risks of AS in patients with JIA.
Table 1. Summary of evidence.
| Level of evidence | Article | Intervention and study population | Safety | Pain | Function | Disease progression |
|---|---|---|---|---|---|---|
| IV | Adolfsson, 2011 | AS of the wrist in adults with RA | ↓ | ↑ | ||
| V | Slutsky, 2012 | AS in JIA | ↓ (long-term) |
|||
| IV | Hanff et al, 1990 | Open synovectomy of the wrist in JIA | ↓ in 50% | ↑ Grip strength ↓ Range of motion |
Early intervention prevents recurrent synovitis | |
| V | Evans et al, 1991 | Open synovectomy of the wrist in JIA (one patient) | ↓ | ↑ Range of motion ↓ Swelling |
Healing erosions after 2 y | |
| IV | Kim and Jung, 2007 | AS of the wrist in adults with RA | Neurapraxia of the superficial radial nerve in one patient Injury to the posterior interosseous nerve reported |
↓ | ↑ Functional state (Mayo wrist score) |
|
| IV | Farr et al, 2012 | AS of the wrist in children/adolescents with chronic wrist pain | No intra- or postoperative complications | |||
| IV | Adolfsson and Frisén, 1997 | AS of the wrist in adults with RA | No complications | ↓ | ↑ Function (subjective assessment of pain and level of activity) |
Delayed progression |
| IV | Wei et al, 2001 | AS of the wrist in adults with RA (office-based procedure) | No complications | |||
| IV | Lee et al, 2014 | AS of the wrist in adults with RA | ↓ | ↑ Function (Mayo wrist score) |
No recurrence of synovitis | |
| IV | Kim et al, 2012 |
AS of the wrist in adults with inflammatory arthritis not responding to medical management | ↓ | ↑ Function (Mayo wrist score) |
No recurrence of synovitis | |
| IV | Park et al, 2003 | AS of the wrist in adults with RA not responding to medical management | ↓ | ↑ Patient satisfaction (VAS) | Slowed progression of degenerative radiographic changes | |
| IV | Toledo et al, 2006 |
AS in oligoarticular JIA refractory to NSAIDs and/or corticosteroid treatment | Safe, one patient with hemarthrosis and persistent effusion | 36% remained in remission after a mean of 65 mo follow-up Best results achieved with AS when performed in early disease |
Abbreviations: AS, arthroscopic synovectomy; JIA, juvenile idiopathic arthritis; NSAIDs, nonsteroidal anti-inflammatory drugs; RA; rheumatoid arthritis; VAS, visual analog scale.
Open Synovectomy for Juvenile Idiopathic Arthritis Affecting the Wrist
Hanff et al performed open synovectomy on 20 wrists of patients suffering from JIA. 18 Of the 20 patients, 17 reported improvement in pain and 7 were completely pain-free. Improvements in grip strength were also noted, but persistently decreased ROM was found. The authors concluded that there was no significant difference in outcome following open wrist synovectomy between JIA and adult arthritic patients. 18 Evans et al replicated these findings by demonstrating that open synovectomy for JIA relieved pain, reduced swelling, and improved ROM. Radiographs taken 2 years following the procedure revealed healing of periarticular erosions. 20 There are concerns, however, that conventional, open synovectomy often leads to joint stiffness due to disruption of the capsule and ligaments.
Arthroscopy and Arthroscopic Synovectomy of the Wrist
The potential benefits of arthroscopy in adults with wrist arthritis have been reviewed by Slutsky, including its use as a minimally invasive diagnostic tool for obtaining tissue biopsy ( Fig. 1 ). Synovial biopsies may be useful for quantitative analysis of the inflammatory response in RA as a prognostic marker. Arthroscopy and AS have also been used for treating degenerative arthritis and posttraumatic arthritis in the wrist, especially in patients who have not responded to appropriate medical management within 3 to 6 months, but the role of AS in JIA was not discussed. 19
Fig. 1 (A–B).
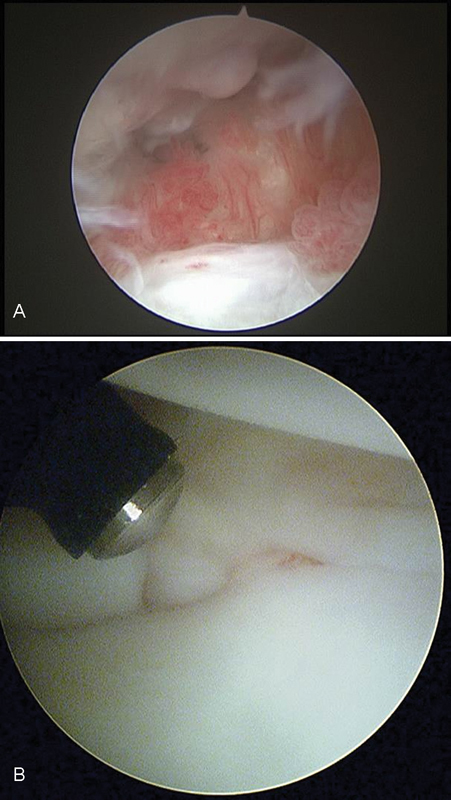
Arthroscopy and arthroscopic synovectomy of the wrist.
AS of the wrist has been proposed as an effective intervention to relieve pain and recover function in early RA before the onset of advanced radiographic changes suggesting wrist destruction. 21 It was suggested that AS may delay the need for more complex surgery, such as arthrodesis and arthroplasty, in selected cases. In addition, AS was found to offer advantages over open synovectomy due to its minimally invasive nature. AS leaves less damage to the joint capsule and ligaments, enabling patients to mobilize immediately following the procedure with consequently reduced length of inpatient stay. 21
Safety Aspects
Farr et al performed a retrospective review of their experience in 34 cases of wrist arthroscopy in children and adolescents referred for chronic wrist pain. They observed no intra- or postoperative complications and concluded that wrist arthroscopy in this population was safe. 22 Several studies in adult populations have supported the safety and efficacy of AS. 23 24 Two groups have proposed the use of AS as a day-case procedure, as it does not require an open arthrotomy and there is less joint capsule and ligament damage, allowing immediate postoperative mobilization. 23 24
Effects on Pain and Wrist Function
Lee et al in their long-term review of 49 patients (56 wrists) suffering from monoarticular RA found that early AS was associated with a significant mean reduction in visual analog scale (VAS) score from 6.3 to 1.7 as well as a mean improvement in the Mayo wrist score from 48 to 76. 17
Several reviews from different units had similar results, showing reduced levels of pain and improved wrist function following AS for patients resistant to medical management. 16 21 23 25 26
Effects on Remission and Progression
Lee et al performed a retrospective review of 49 adult patients (56 wrists) who had RA resistant to medical management. They found that early AS afforded long-term remission and noticed slowed progression of disease, with the mean Larsen stage only progressing from 2.2 to 3.3 over the mean 7.9-year follow-up. 17 Kim and Jung had similar findings in their cohort of 20 patients with undifferentiated monoarthritis of the wrist not responding to nonsteroidal anti-inflammatory drugs. Following AS, 9 of 20 patients achieved early remission, and all patients had improved clinical scores (VAS and modified Mayo score). They too noted slowed progression in disease, with 14 patients showing no radiological change and 5 patients showing slowed progression of Larsen grade over the 51.8-month follow-up period. 25 Several studies echoed these findings in their patient cohorts. 21 23 26
Kim and Jung recommended AS for pain relief and functional recovery in early RA. In addition, they found it to be helpful in advanced staged RA with Larsen stage III radiographic changes. In their opinion, AS delayed the need for complex surgery, such as wrist arthrodesis or total wrist arthroplasty, in selective cases. 21
Discussion
The evidence for the use of arthroscopy and AS in JIA affecting the wrist is sparse, and the studies found in this systematic review were retrospective descriptions of small case series. In general, standardized evaluations of pain and level of function were used and follow-up evaluations were performed, but, otherwise, the studies were uncontrolled. Patients were not matched for disease activity or stage of disease at the time of intervention, and variations in the metrics used made comparison difficult. The difficulties in obtaining strong evidence are understandable considering the relatively small target population, highlighting the need for larger scale, collaborative approaches to research in this area.
Open synovectomy for patients suffering from JIA affecting the wrist has been reported in a few case series with small sample sizes (level IV evidence), with results suggesting that synovectomy has a role in disease treatment through relieving pain and improving function. 18 20 However, open procedures are associated with disruption of the joint capsule and ligaments and can lead to joint stiffness and decreased mobility.
The safety and efficacy of AS for knee, hip, shoulder, and elbow joints affected by JIA have been well documented in the literature, noting improvement in clinical and radiological scoring systems. 27 28 29 Toledo et al evaluated the long-term safety and efficacy of AS in patients suffering from oligoarticular forms of JIA. They found AS to be safe but only partially effective, with best results achieved by early intervention for children with persistent monoarticular involvement showing no evidence of systemic inflammation. 30 Various studies described the efficacy of open synovectomy in patients with JIA affecting the wrist. 18 20
In adults with RA, wrist arthroscopy and AS are associated with pain relief, increased ROM, and improvement in general function. 16 17 21 23 25 26 In addition, studies evaluating long-term follow-up found that AS induced sustained remission and slowed radiological progression of disease when antirheumatic medications alone failed to control the inflammation. 16 21 23 25 26 Lee et al noted that AS afforded a significant reduction in pain and controlled synovitis in 75% of adult patients with RA not responding to medication. 17 Kim and Jung were of the opinion that AS may delay the need for complex surgery, such as wrist arthrodesis or total wrist arthroplasty. 21
A recent study using synovial biopsies identified synovial protein expression patterns that discriminate between clinical subgroups of early JIA. 31 Synovial biopsies are relatively easy to obtain using AS in JIA and may contribute to understanding the early pathological changes and disease process in JIA. 31 Such studies may identify patients who are at high risk of disease progression. Protein modification has been found to be a surrogate marker of uncontrolled inflammation in JIA, and synovial protein analysis could identify patients who are at high risk of disease progression. 32
Our anecdotal experience is that 35 to 40% of adult patients with RA progress to remission, and 20 to 30% do not respond despite drug treatment. Additionally, we are monitoring several children who have uncontrolled JIA and extensive joint destruction with very few clinical symptoms to indicate the progression of their disease. It is possible that early identification of these “silent destructors” and early use of AS could delay joint destruction and preserve function.
Conclusion
There is currently a paucity of evidence for the use of arthroscopy and AS in the wrists of patients with JIA ( Table 1 ), and there is clearly a need for better outcome studies regarding the usefulness of wrist arthroscopy in JIA.
Based on a systematic review and 20 years of clinical experience in adult RA, we postulate that children with JIA will respond in a similar fashion when treated with AS and that silent destructors will show slowing of the progression of disease and destruction of their wrist joints. Studies suggest that AS is likely to be a safe and effective intervention, which could be used judiciously in patients with refractory JIA. There clearly is a need for well-designed prospective studies to assess the role of wrist arthroscopy and AS in JIA.
Future Implications
Early identification and subsequent early AS of patients with JIA affecting the wrist could delay joint destruction, preserve function, and defer more invasive procedures. A multidisciplinary team approach (MDT, e.g., involving colleagues from rheumatology, radiology, hand surgery, and hand therapy) 33 is likely to be an effective means of identifying candidates for arthroscopy and AS. We postulate that JIA patients with any wrist involvement should be monitored regularly in this type of MDT, regardless of whether they are clinically symptomatic or not. A treatment algorithm that allows early identification of those at risk would encourage early consideration for AS, which may improve long-term outcome.
Funding Statement
Funding None.
Conflict of Interest None.
Note
This study was presented at the 10th World Symposium on Congenital Malformations of the Hand and Upper Limb 2015, May 7–9, Rotterdam, The Netherlands.
References
- 1.Prakken B, Albani S, Martini A.Juvenile idiopathic arthritis Lancet 2011377(9783):2138–2149. [DOI] [PubMed] [Google Scholar]
- 2.Ravelli A, Martini A.Juvenile idiopathic arthritis Lancet 2007369(9563):767–778. [DOI] [PubMed] [Google Scholar]
- 3.Petty R E, Southwood T R, Manners P et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(02):390–392. [PubMed] [Google Scholar]
- 4.Espinosa M, Gottlieb B S. Juvenile idiopathic arthritis. Pediatr Rev. 2012;33(07):303–313. doi: 10.1542/pir.33-7-303. [DOI] [PubMed] [Google Scholar]
- 5.Hemke R, Nusman C M, van der Heijde D MFM et al. Frequency of joint involvement in juvenile idiopathic arthritis during a 5-year follow-up of newly diagnosed patients: implications for MR imaging as outcome measure. Rheumatol Int. 2015;35(02):351–357. doi: 10.1007/s00296-014-3108-x. [DOI] [PubMed] [Google Scholar]
- 6.Ravelli A, Martini A. Early predictors of outcome in juvenile idiopathic arthritis. Clin Exp Rheumatol. 2003;21(05) 31:S89–S93. [PubMed] [Google Scholar]
- 7.Miller E, Uleryk E, Doria A S. Evidence-based outcomes of studies addressing diagnostic accuracy of MRI of juvenile idiopathic arthritis. AJR Am J Roentgenol. 2009;192(05):1209–1218. doi: 10.2214/AJR.08.2304. [DOI] [PubMed] [Google Scholar]
- 8.Magni-Manzoni S, Malattia C, Lanni S, Ravelli A. Advances and challenges in imaging in juvenile idiopathic arthritis. Nat Rev Rheumatol. 2012;8(06):329–336. doi: 10.1038/nrrheum.2012.30. [DOI] [PubMed] [Google Scholar]
- 9.Østergaard M, Peterfy C, Conaghan P et al. OMERACT Rheumatoid Arthritis Magnetic Resonance Imaging Studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol. 2003;30(06):1385–1386. [PubMed] [Google Scholar]
- 10.Malattia C, Damasio M B, Pistorio A et al. Development and preliminary validation of a paediatric-targeted MRI scoring system for the assessment of disease activity and damage in juvenile idiopathic arthritis. Ann Rheum Dis. 2011;70(03):440–446. doi: 10.1136/ard.2009.126862. [DOI] [PubMed] [Google Scholar]
- 11.Hemke R, van Rossum M A, van Veenendaal M et al. Reliability and responsiveness of the Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee. Eur Radiol. 2013;23(04):1075–1083. doi: 10.1007/s00330-012-2684-y. [DOI] [PubMed] [Google Scholar]
- 12.Nusman C M, Hemke R K, Kuijpers T W, Deurloo E E, Schoneberg D, Van den Berg J. A novel MRI scoring system for the evaluation of early-stage disease activity of the wrist in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2012 10:2019. [Google Scholar]
- 13.Ording Muller L S, Boavida P, Avenarius D et al. MRI of the wrist in juvenile idiopathic arthritis: erosions or normal variants? A prospective case-control study. Pediatr Radiol. 2013;43(07):785–795. doi: 10.1007/s00247-012-2575-z. [DOI] [PubMed] [Google Scholar]
- 14.Müller L-SO, Avenarius D, Damasio B et al. The paediatric wrist revisited: redefining MR findings in healthy children. Ann Rheum Dis. 2011;70(04):605–610. doi: 10.1136/ard.2010.135244. [DOI] [PubMed] [Google Scholar]
- 15.Lanni S, Wood M, Ravelli A, Magni Manzoni S, Emery P, Wakefield R J. Towards a role of ultrasound in children with juvenile idiopathic arthritis. Rheumatology (Oxford) 2013;52(03):413–420. doi: 10.1093/rheumatology/kes287. [DOI] [PubMed] [Google Scholar]
- 16.Adolfsson L. Arthroscopic synovectomy of the wrist. Hand Clin. 2011;27(03):395–399. doi: 10.1016/j.hcl.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Lee H I, Lee K H, Koh K H, Park M J. Long-term results of arthroscopic wrist synovectomy in rheumatoid arthritis. J Hand Surg Am. 2014;39(07):1295–1300. doi: 10.1016/j.jhsa.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 18.Hanff G, Sollerman C, Elborgh R, Pettersson H. Wrist synovectomy in juvenile chronic arthritis (JCA) Scand J Rheumatol. 1990;19(04):280–284. doi: 10.3109/03009749009102534. [DOI] [PubMed] [Google Scholar]
- 19.Slutsky D J. The role of arthroscopy in wrist arthritis. Curr Rheumatol Rev. 2012;8:245–252. [Google Scholar]
- 20.Evans D M, Ansell B M, Hall M A. The wrist in juvenile arthritis. J Hand Surg Br. 1991;16(03):293–304. doi: 10.1016/0266-7681(91)90057-u. [DOI] [PubMed] [Google Scholar]
- 21.Kim S-J, Jung K-A. Arthroscopic synovectomy in rheumatoid arthritis of wrist. Clin Med Res. 2007;5(04):244–250. doi: 10.3121/cmr.2007.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farr S, Grill F, Girsch W. Wrist arthroscopy in children and adolescents: a single surgeon experience of thirty-four cases. Int Orthop. 2012;36(06):1215–1220. doi: 10.1007/s00264-011-1428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adolfsson L, Frisén M. Arthroscopic synovectomy of the rheumatoid wrist. A 3.8 year follow-up. J Hand Surg Br. 1997;22(06):711–713. doi: 10.1016/s0266-7681(97)80430-5. [DOI] [PubMed] [Google Scholar]
- 24.Wei N, Delauter S K, Beard S, Erlichman M S, Henry D. Office-based arthroscopic synovectomy of the wrist in rheumatoid arthritis. Arthroscopy. 2001;17(08):884–887. doi: 10.1016/s0749-8063(01)90014-3. [DOI] [PubMed] [Google Scholar]
- 25.Kim S M, Park M J, Kang H J, Choi Y L, Lee J J. The role of arthroscopic synovectomy in patients with undifferentiated chronic monoarthritis of the wrist. J Bone Joint Surg Br. 2012;94(03):353–358. doi: 10.1302/0301-620X.94B3.28354. [DOI] [PubMed] [Google Scholar]
- 26.Park M J, Ahn J H, Kang J S. Arthroscopic synovectomy of the wrist in rheumatoid arthritis. J Bone Joint Surg Br. 2003;85(07):1011–1015. doi: 10.1302/0301-620x.85b7.14195. [DOI] [PubMed] [Google Scholar]
- 27.Guszczyn T, Sierakowski S, Popko J. AB1208 Arthroscopic synovectomy of the knee in patients with juvenile idiopathic arthritis (JIA) Ann Rheum Dis. 2013;71 03:706. [Google Scholar]
- 28.Nwachukwu B U, McFeely E D, Nasreddine A Y, Krcik J A, Frank J, Kocher M S. Complications of hip arthroscopy in children and adolescents. J Pediatr Orthop. 2011;31(03):227–231. doi: 10.1097/BPO.0b013e31820cadc5. [DOI] [PubMed] [Google Scholar]
- 29.Mäenpää H, Kuusela P, Lehtinen J, Savolainen A, Kautiainen H, Belt E. Elbow synovectomy on patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2003;(412):65–70. doi: 10.1097/01.blo.0000072463.53786.df. [DOI] [PubMed] [Google Scholar]
- 30.Toledo M MM, Martini G, Gigante C, Da Dalt L, Tregnaghi A, Zulian F. Is there a role for arthroscopic synovectomy in oligoarticular juvenile idiopathic arthritis? J Rheumatol. 2006;33(09):1868–1872. [PubMed] [Google Scholar]
- 31.Finnegan S, Robson J, Scaife C et al. Synovial membrane protein expression differs between juvenile idiopathic arthritis subtypes in early disease. Arthritis Res Ther. 2014;16(01):R8. doi: 10.1186/ar4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gibson D S, Newell K, Evans A N et al. Vitamin D binding protein isoforms as candidate predictors of disease extension in childhood arthritis. J Proteomics. 2012;75(17):5479–5492. doi: 10.1016/j.jprot.2012.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farr S, Girsch W. The hand and wrist in juvenile rheumatoid arthritis. J Hand Surg Am. 2015;40(11):2289–2292. doi: 10.1016/j.jhsa.2015.06.111. [DOI] [PubMed] [Google Scholar]


