Abstract
Patient-perceived stress and avoidance-oriented coping strategies are mental health risk factors well documented within the infertility literature. Relatedly, these factors are associated with maladaptive eating behaviours known to influence reproductive functioning. This study aims to investigate the interconnection between perceived stress, avoidant coping style and eating pathology in infertile women, and to determine whether avoidant coping style mediates the relationship between stress and eating pathology. A multicentre cross-sectional study of 416 women (aged 20–47 years) was completed. Women were assessed on the Eating Disorder Examination Questionnaire, the Perceived Stress Scale and the Brief COPE. Correlational matrices, principal components analysis and structural equation modelling were used to develop a measurement model to test the avoidant coping style mediation hypothesis. Results showed that perceived stress had a direct effect on maladaptive eating behaviours [β = 0.21; 95% confidence interval (CI) 0.065–0.346; P = 0.005]. Furthermore, a statistically significant indirect effect between perceived stress and maladaptive eating via avoidant coping style was also observed (β = 0.14; 95% CI = 0.017–0.267; P = 0.018), indicating partial mediation. These findings highlight that both perceived stress and avoidant coping style are important psychotherapy targets to consider in infertile women presenting with eating pathology.
Keywords: avoidant coping style, eating pathology, infertility, perceived stress, preconception counselling
Introduction
In studies of human reactions to stress, stressful life events characterized by socio-evaluative elements are generally associated with greater physiological, psychosocial and behavioural sequelae (Gruenewald et al., 2004, Miller et al., 2007). The inability to conceive children is considered to be one of the greatest sources of perceived stress in a person's life, akin to a diagnosis of a major illness (Domar et al., 1993). The impact of perceived stress and psychological distress secondary to the experience of infertility has been widely investigated with respect to fertility treatment burden and outcomes, mood, coping style and quality of relationship (Boivin et al., 2011, Ebbesen et al., 2009, Gameiro et al., 2012, Schmidt et al., 2005, Van den Broeck et al., 2010, Verhaak et al., 2007). Some studies report that stress is associated with increased rates of anxiety and depression, marital dissatisfaction and a greater perception of treatment burden, increasing the potential for fertility treatment drop-out (Cousineau and Domar, 2007, Domar, 2004, Gameiro et al., 2012, Gana and Jakubowska, 2016, Pasch et al., 2016). Stress can further pre-empt engagement in maladaptive health attitudes and lifestyle behaviours, including disordered eating attitudes and behaviours (Keyes et al., 2011, Klatzkin et al., 2016, Kouvonen et al., 2005). Thus, exploration of stress and the way it is manifested, appraised and managed among women presenting for fertility treatment represent important objectives for research and intervention.
The Transactional Model of Stress and Coping (Glanz et al., 2008, Lazarus and Folkman, 1984) provides a framework to evaluate appraisal and coping with situational and chronic stressful events. Lazarus and Folkman (1984) defined coping as a response to a perceived stressor, involving cognitive and behavioural strategies aimed at reducing the psychosocial and physical burdens of an event viewed as taxing or exceeding the resources of that person. It recognizes that the stress response is influenced by the perceived significance placed upon a stressful situation, with the coping style endorsed being dependent upon whether the stressor is appraised as personally meaningful and/or whether it is viewed as something that is unchangeable (Lazarus and Folkman, 1984).
Individuals deal with stress through a diversity of coping styles. For example, problem-focused versus emotion-focused strategies, and active versus avoidant-oriented coping are common distinctions in the coping literature (Aldao et al., 2010, Endler and Parker, 1990, Lazarus and Folkman, 1984). Generally, problem-focused coping efforts are seen as adaptive. In contrast, avoidance-oriented coping strategies are deemed maladaptive and are strongly related to psychopathology and poorer behavioural health outcomes (Aldao et al., 2010). Psychosocial studies in the area of fertility coincide with the broader literature. For example, avoidant-oriented coping strategies are shown to be associated with poorer adjustment both during and after in-vitro fertilization (IVF) treatment (Benyamini et al., 2008, Gourounti et al., 2012, Lancastle and Boivin, 2005, Terry and Hynes, 1998, Van den Broeck et al., 2010).
How an individual perceives and copes with a major life stressor such as infertility may have direct bearings upon the manifestation of negative health behaviours known to compromise reproduction (e.g. alcohol and drug consumption, smoking, poor sleep and weight status) (Gormack et al., 2015, Homan et al., 2007, Rooney and Domar, 2014). In the context of preconception care, particularly for women with forms of an ovulatory disorder, healthy reproductive function is related to a woman's optimal body weight range and weight stability (Loucks, 2007, Mircea et al., 2007, Schneider, 2004). In times of stress, weight status can fluctuate, being directionally influenced by symptoms of eating pathology such as binge eating or dietary restraint (Ball and Lee, 2000, Kupeli et al., 2017, Razzoli et al., 2017). Therefore, it is important to investigate factors that either exacerbate or ameliorate eating pathology.
The antecedents to eating pathology are multifactorial (Striegel-Moore and Bulik, 2007). Some studies propose that higher levels of perceived stress and daily life hassles are associated with greater eating pathology (Ball and Lee, 2000, Crowther et al., 2001, Greeno and Wing, 1994, Klatzkin et al., 2016). Other studies emphasize the role of coping style, and particularly avoidance-oriented coping, in disordered eating attitudes and behaviours (Davies et al., 2011, Freeman and Gil, 2004, MacNeil et al., 2012, Sulkowski et al., 2011, Troop et al., 1994). Consequently, when faced with a life stressor such as fertility-related stress, women may have a greater propensity to engage in maladaptive eating behaviours such as binge eating, or alternatively employ unhealthy weight control practices such as skipping meals, fasting and purging, or use of laxatives and diuretics (Fairburn and Beglin, 2008, Freeman and Gil, 2004, Klatzkin et al., 2016), especially when coupled with poor coping styles. Endorsement of such maladaptive eating behaviours may be expected to influence energy availability and body mass index (Mircea et al., 2007), having implications for reproductive outcomes. These include increased time to pregnancy (Gesink Law et al., 2007, Norman et al., 2008), increased incidence of cancelled treatment cycles, and reduced fertility treatment success rates (ESHRE Capri Workshop Group, 2006, Landres et al., 2010, Norman et al., 2008). Moreover, the emotional and physical burdens of ovarian stimulation as part of the fertility treatment protocol can lead to weight gain (Toftager et al., 2018), with fear of weight gain, in turn, being a potential trigger to eating pathology in women who are susceptible to body image dissatisfaction and eating disorders (American Psychiatric Association, 2013, Pearson et al., 2010).
In light of the above, the over-arching aim of this study was to investigate a model of perceived stress, avoidant coping style and eating pathology amongst infertile women attending an IVF clinic. Drawing from the extant literature, it was first hypothesized that the level of perceived stress would be positively associated with avoidant coping style and severity of eating pathology (disordered eating attitudes and behaviours). Second, consistent with reports that avoidant-oriented coping strategies are positively associated with eating pathology, it was hypothesized that avoidant coping style would be positively associated with eating pathology, and that avoidant coping style would mediate, either partially or fully, the relationship between stress and eating pathology symptoms. Third, should partial mediation be observed, this study aimed to determine whether the direct effect or the indirect effect (via avoidant coping) between perceived stress and maladaptive eating had a larger influence on the maladaptive eating scores. From a clinical perspective, research exploring the relationship between stress and coping style is important and may help orientate treatment goals for fertility patients experiencing stress-related eating pathology.
Materials and methods
Participants
Participants were 416 partnered women recruited from three fertility clinics located in Perth, Western Australia. Patients undergoing donor conception, undertaking oncology treatment or referred for genetic testing were excluded from participation. All participants spoke English, were aged between 20 and 47 years, and had commenced a treatment cycle.
Measures
The Demographics Questionnaire is an investigator-developed sociodemographic protocol gauging background information (e.g. age, educational level, occupation, employment status, marital status, living arrangements, etc.), anthropometric measures (e.g. height, weight), treatment-related information (e.g. cause of infertility, type of fertility treatment) and physical health status.
The Eating Disorder Examination Questionnaire (EDE-Q; Fairburn and Beglin, 2008) is a self-report version of the Eating Disorder Examination Interview. It is used to assess core attitudinal and behavioural components of eating psychopathology over the last 28 days. The EDE-Q produces four subscales (restraint, eating concern, weight concern and shape concern) and an overall global score. Scores range from 0 to 6, with a higher score on either the subscales or global score indicating a greater severity of eating disorder pathology. The EDE-Q also assesses frequencies of maladaptive eating behaviour items (e.g. binge eating and bulimic weight control compensatory behaviours). These maladaptive compensatory eating behaviour items are assessed in terms of the number of episodes and/or days that these behaviours have occurred over a 4-week time frame. In this study, a disordered eating behaviour composite was generated from these items: the presence of restrained eating for greater than an 8-h period (Item 2), binge eating days with sense of loss of control (Item 15), purging behaviour (Item 16), laxative use (Item 17) and engagement in obligatory excessive exercise (Item 18). These five behavioural items were dichotomized for any occurrence (i.e. ≥ 1 episode versus 0 episodes over the past 28 days) and summed to form the disordered eating behaviour composite, with a higher score representing greater use of diverse disordered eating behaviours (range 0–5).
The Perceived Stress Scale (PSS; Cohen et al., 1983) is a 14-item scale that measures the degree to which an individual assesses the situations in their life as being stressful. The scale focuses on three aspects of stress – uncontrollability, unpredictability and overload – and is sensitive to various sources of chronic stress. Ratings are given using a five-point Likert scale (0 = never, 4 = very often). A higher score indicates a higher level of perceived stress. The PSS has good construct validity due to its close correlation with measures of depression and inventories of life events (Cohen et al., 1983). In this study, the PSS was used to gauge a participant's perceived level of stress over the last 28 days.
The Brief COPE (Carver, 1997) is a 28-item self-report scale that is used to gauge the coping reactions to stress used by participants. The Brief COPE consists of 14 subscales comprising of two items each, rated on a four-point Likert scale ranging from 1 to 4. Each subscale measures a conceptually different aspect of coping (active coping, planning, positive reframing, acceptance, humour, religion, emotional support, instrumental support, self-distraction, denial, venting, substance use, behavioural disengagement and self-blame). Participants were asked to respond according to their habitual response style to stressful situations. A higher score on any subscale indicates a higher frequency of use for that particular coping mechanism.
Procedure
Between June 2011 and May 2012, partnered women attending three fertility centres in Western Australia were invited to participate in this research project. Following an introduction by a fertility nurse co-ordinator, patients waiting to have fertility-related blood tests were approached by the chief investigator regarding inclusion in a questionnaire-based study. Participants were given a research pack inclusive of a participant information form, study questionnaires, a debriefing sheet and a pre-paid envelope for anonymous questionnaire submission. Participants were instructed to complete the questionnaire within a 2-week time frame and were also advised that study participation was entirely voluntary. Returning the anonymously completed survey served as informed consent to proceed. Approval for completion of this study and the research protocol was granted by the Human Research Ethics Committee of The University of Western Australia (Reference RA/4/1/4642), Joondalup Health Campus (Reference JHC1111) and Hollywood Private Hospital (Reference HPH334), covering each of the respective data collection sites.
Data management
From 1000 test protocols issued, 445 participant protocols were returned; 16 were subsequently excluded as the participant indicated that she was pregnant. All psychological scales and subscales were examined for excessive missing test responses and values exceeding test norms. This resulted in an additional 13 response protocols being deleted, yielding a final sample size for analysis of 416 participants. For remaining participants, if less than 5% of data points were missing, omitted values on these variables were replaced with the test mean for the specific factor on which that item loaded (Tabachnick and Fidell, 2001).
Data analytic approach
Percentages were computed for all demographic data. To determine the indicators of avoidant coping style for use in the structural equation model, principal component analysis using promax rotation was initially performed on the subscales of the Brief COPE with four factors converging (Kaiser–Meyer–Olkin Index = 0.71). Only the six subscales loading on the avoidant coping style factor (i.e. denial, disengagement, venting, self-blame, substance use and self-distraction) were parcelled as indicators for use in the structural equation model. An avoidant cope composite was derived from the summed scores on these six subscales that served the basis of the bivariate analyses. Eating pathology indicators were represented by the four subscales of the EDE-Q and the disordered eating behaviours composite.
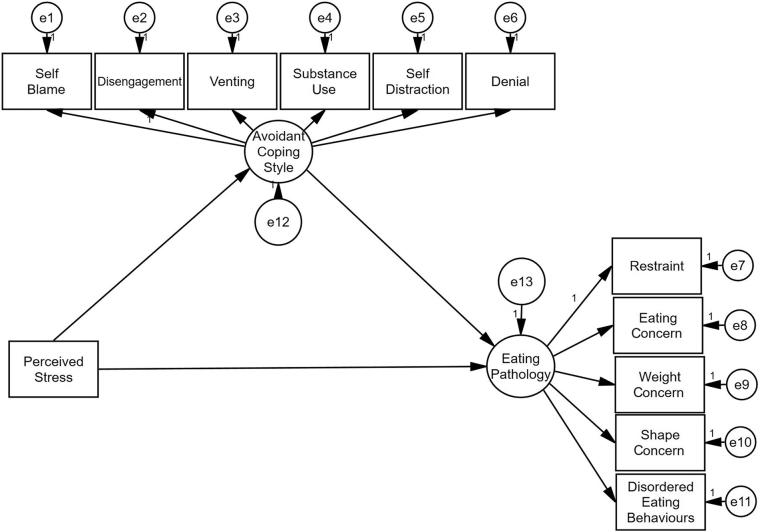
Fig. 1 shows a schematic model of the variables that were investigated. Two latent variables were represented in the structural equation model: (i) avoidant coping style and (ii) eating pathology. The full fit of the mediation model was estimated using maximum likelihood estimation. Adequacy of the model fit was evaluated based on several close-fit indices: the comparative fit index (CFI), the Tucker-Lewis Index (TLI), the Incremental Fit Index (IFI), the root mean squared error of approximation (RMSEA) and the standardized root mean squared residual (SRMSR). The following guidelines were used: CFI, TLI and IFI > 0.95 and RMSEA and SRMR < 0.08 as indicative of a well-fitting model (Hair et al., 2010, Hu and Bentler, 1999, Marsh et al., 2004).
Fig. 1.
Schematic representation of proposed model relationships between perceived stress, mediator avoidant coping style and eating pathology (disordered eating attitudes and behaviours). Perceived stress is an observed measured variable, and avoidant coping style and eating pathology are unobserved latent variables comprised of measurement indicators and associated error terms (e1–e13). The observed variables in the model are outcome scores from the Perceived Stress Scale (PSS), the Brief COPE and the Eating Disorder Examination Questionnaire (EDE-Q).
In this study, the mediation model intended to evaluate the direct and indirect effects of perceived stress on eating pathology via the intermediary variable of avoidant coping style. All standardized point estimates associated with the model were tested for statistical significance via 2000 bootstrapped re-samples. According to Preacher and Hayes (2004), mediation (whether partial or complete) is observed when a statistically significant indirect effect is estimated from a bootstrapped solution, i.e. when the 95% confidence intervals (CI) associated with the point estimate do not intersect with zero. Complete mediation was considered to be observed in the event that the direct effect between perceived stress and maladaptive eating was no longer found to be statistically significant. Partial mediation was considered to be observed in the event that the direct effect of perceived stress on maladaptive eating remained statistically significant in the presence of avoidant coping.
The numerical difference between the direct and indirect standardized beta weights was tested for statistical significance via 2000 bootstrapped re-samples through the Amos user-estimand utility. SPSS for Windows, Version 24 (SPSS, Chicago, IL, USA) and AMOS, Version 24 (Arbuckle, 2016) were used for all statistical analyses. In all cases, a two-tailed P-value of < 0.05 was considered to indicate statistical significance.
Results
Sample characteristics
On average, the study participants were 34.4 years of age [standard deviation (SD = 4.8 years] and had been trying to conceive for approximately 31 months (SD = 24.8 months). Participant body mass index (BMI) derived from self-reported height and weight ranged from 16.33 to 45.25 kg/m2, with the mean BMI being 24.78 kg/m2 (SD = 5.12 kg/m2). Whilst BMI was correlated positively with all eating pathology measures (all P < 0.001), BMI was not correlated with the independent variable perceived stress (r = 0.07; P = 0.176) or mediator avoidant coping style (r = 0.03; P = 0.536). Approximately 64% of patients were actively undergoing IVF or intracytoplasmic sperm injection fertility treatment, with the remainder being monitored for cycle tracking and/or ovulation induction treatments. Thirty-nine percent of participants were undergoing their first fertility treatment cycle, 56% were undergoing a repeat treatment cycle and 5% did not respond. Perceived level of stress (PSS) did not vary between those completing their first and repeat treatment cycles [t (392) = − 0.357; P = 0.722]. Eighty-six percent of the sample consisted of participants who self-identified as Caucasian, 53% reported working full-time in paid employment and 61% reported attaining tertiary education.
Preliminary bivariate analyses
Descriptive statistics and bivariate correlation analyses associated with the the Perceived Stress Scale, the Eating Disorder Examination Questionnaire and the Brief COPE are presented in Table 1. As can be seen in Table 1, the correlations between the indicators included in the structural equation model were all statistically significant and in the expected direction. For example, higher levels of perceived stress were associated with greater levels of eating pathology on all four EDE-Q subscales and the disordered eating behaviour composite (r = 0.11–0.36; all P < 0.05). A higher level of perceived stress was likewise positively correlated with higher use of avoidant coping strategies (r = 0.55; P < 0.001). Similarly, avoidant coping style was positively correlated with all measures of the EDE-Q subscales and the disordered eating behaviour composite (r = 0.16–0.27; all P < 0.001).
Table 1.
Pearson product moment correlations, means and standard deviations.
| Variables | Mean | SD | PSS | REST | EC | SC | WC | DEB | COPE |
|---|---|---|---|---|---|---|---|---|---|
| PSS | 25.75 | 7.84 | 1 | 0.11a | 0.31b | 0.36b | 0.32b | 0.18b | 0.55b |
| REST | 1.11 | 1.22 | 1 | 0.41b | 0.52b | 0.53b | 0.39b | 0.16b | |
| EC | 0.47 | 0.79 | 1 | 0.65b | 0.66b | 0.52b | 0.20b | ||
| SC | 1.88 | 1.51 | 1 | 0.92b | 0.46b | 0.27b | |||
| WC | 1.54 | 1.39 | 1 | 0.45b | 0.26b | ||||
| DEB | 0.47 | 0.76 | 1 | 0.16b | |||||
| COPE | 26.29 | 5.38 | 1 |
Note: n = 416.
PSS, Perceived Stress Scale; REST, Eating Disorder Examination Questionnaire (EDE-Q) restraint subscale; EC, EDE-Q eating concern subscale; SC, EDE-Q shape concern subscale; WC, EDE-Q weight concern subscale; DEB, disordered eating behaviours; COPE, composite of six avoidant cope indicators.
Correlation is significant at the 0.05 level (two-tailed).
Correlation is significant at the 0.001 level (two-tailed).
Mediating the effects of avoidant coping style on eating pathology
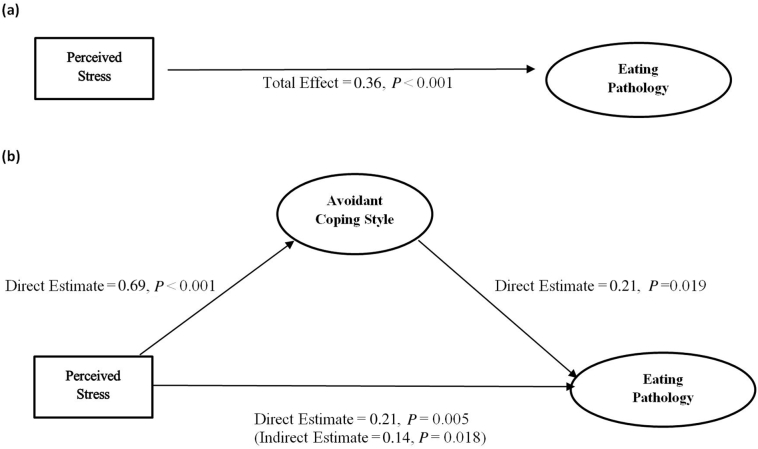
As can be seen in Fig. 2a, the standardized total effect of perceived stress on eating pathology was estimated at β = 0.36 (P < 0.001). As can be seen in Fig. 2(b), all direct effects were statistically significant (P < 0.05). The direct effect of perceived stress on eating pathology was estimated at β = 0.21 (95% CI 0.065–0.346; P = 0.005). Furthermore, the indirect effect of perceived stress on eating pathology via the mediator avoidant coping was estimated at β = 0.14 (95% CI 0.017–0.267; P = 0.018). As the strength of the relationship between perceived stress and eating pathology was reduced but remained significant when avoidant coping was incorporated into the model, the pattern of results was consistent with partial mediation. The close-fit indices suggested an adequately fitting model: χ2(52) = 147.84; P < 0.001; CFI = 0.950; TLI = 0.937; IFI = 0.951; RMSEA = 0.067; SRMR = 0.048. The model R2 was estimated at 0.150, thus 15% of the variance in maladaptive eating was accounted for by perceived stress and avoidant coping style. To determine which pathway, direct or indirect via the mediator, provided a better explanation for the variance in eating pathology, the numerical difference between the standardized direct and indirect effects was tested for statistical significance. No statistical significance was observed between the pathways (∆ β = − 0.065; 95% CI -0.318–0.189; P = 0.593).
Fig. 2.
(a) Base model establishing the standardized total effect between perceived stress and eating pathology (n = 416). (b) Demonstrating path relationships between perceived stress and eating pathology once avoidant coping style has been included as an intermediary variable. Avoidant coping style and eating pathology are latent variables. Perceived stress is an observed variable. Standardized coefficients of relevant paths are shown. The value in the parentheses is the standardized coefficient for the stress to eating pathology path following the inclusion of avoidant coping style in the model (i.e. indirect effect).
Discussion
Psychological stress is an established risk factor for negative lifestyle aspects, including disordered eating behaviours (Ball and Lee, 2000). The objectives of this study were to examine the direct and indirect effects of perceived stress on eating pathology via the intermediary variable of avoidant coping style. With respect to perceived stress, the results of this study parallel the findings of previous research in community samples, supporting the perspective that higher levels of perceived stress are directly associated with higher levels of eating pathology symptoms (Ball and Lee, 2000, Kupeli et al., 2017). However, to the authors' knowledge, the positive association between perceived stress and eating pathology reported in this study is unique in its context of women actively undergoing fertility treatment. That is, whilst previous studies in reproductive medicine have reported a higher incidence of disordered eating attitudes and behaviours amongst patients with forms of ovulatory disorders frequenting fertility clinics (Abraham et al., 1990, Coker et al., 2016, Cousins et al., 2015, Freizinger et al., 2010, Stewart et al., 1990), these studies do not specifically investigate the interconnection between measures of stress and eating pathology. Consequently, in light of the present findings, it is clinically important to assess and monitor perceived stress and eating pathology in these diagnostic groups during preconception counselling, with a view to referral for psychosocial care, particularly cognitive behavioural therapy programmes applicable to both symptoms of infertility-related stress and eating pathology (Fairburn and Beglin, 2008, Gameiro et al., 2015, Rooney and Domar, 2014). Assessing and screening patients for eating pathology is important as studies emphasize the benefit of early intervention in terms of prognostic outcomes, including a reduction in the severity of symptoms and duration of the eating disorder (Rodino et al., 2017, Rowe, 2017). Moreover, psychological interventions in patients undergoing fertility treatment have shown a positive effect on patient psychological well-being, fertility treatment retention rates and subsequent pregnancy rates, highlighting the beneficial effects of addressing patient vulnerabilities with adjunct psychological care (Domar, 2004, Domar et al., 2011, Frederiksen et al., 2015, Kraaij et al., 2010).
This study further investigated whether avoidant coping strategies mediated the relationship between perceived stress and eating pathology. Consistent with the hypothesis, avoidant coping style was shown to partially mediate the relationship between stress and eating pathology. This result suggests that avoidant coping style plays a role in eating pathology symptoms, beyond that explained purely by the direct effect of perceived stress on maladaptive eating. This mediational relationship between perceived stress, avoidant coping and eating pathology can be interpreted as consistent with an “escape theory” of eating pathology. According to this theory, perceived stress and subsequent distress arising from external life stressors may be managed through a reduced level of self-awareness and engagement in avoidance-oriented behaviours (Heatherton and Baumeister, 1991). Whilst in the short term, these avoidance strategies may be adaptive by providing emotional distance to the problem, longitudinally, they are less instrumental in resolving the distress and can impact upon psychological well-being (Holahan et al., 2005). Accordingly, clinical interventions that focus on guiding patients with alternative forms of adaptive coping skills, such as problem-focused strategies, acceptance and distress tolerance techniques, may be of greater benefit for patient well-being. This suggestion is supported empirically by others who have found that engagement in positive appraisal or cognitive-oriented coping therapies aimed at direct problem management and emotional regulation are associated with improved patient emotional responses in fertility, including perceived burden of fertility treatment (Gameiro et al., 2015, Kraaij et al., 2010, Lancastle and Boivin, 2005, Ockhuijsen et al., 2014, Rooney and Domar, 2014, Terry and Hynes, 1998).
Understanding the differential paths of perceived stress on eating pathology is important in terms of staging targets for clinical intervention. This study found that neither the direct effects of perceived stress on eating pathology nor the indirect effect via the intermediary variable of avoidant coping style provided a superior explanation of eating pathology symptoms. Therefore, this study highlights that both perceived stress levels and avoidant coping style should be considered important targets in psychotherapeutic interventions for infertile women presenting with forms of eating pathology.
Admittedly, the relationship between stress and eating pathology is complex. In this study, only 15% of the variance in eating pathology was explained by perceived stress and avoidant coping style. Thus, it is clear that there are other unmeasured factors in our mediation model which may better account for the presence of eating pathology. For instance, it has been recognized that concomitant biological changes can occur in the body when an individual is under stress. Specifically, individual differences in levels of neuroendocrine hormones such as cortisol, insulin and ghrelin may influence appetite regulation, alterations to eating behaviours (e.g. binging) and food choice (Culbert et al., 2016, Hilterschield and Laessle, 2015, Newman et al., 2007, Roberts et al., 2014). Similarly, researchers have further speculated that the level of social support available can assist a woman in her capacity to cope adaptively by influencing the stress appraisal process or the emotional and behavioural responses to a stressful event (Aime et al., 2006, Cohen and Willis, 1985, Schwarzer and Knoll, 2007). Future investigations should explore the direct and stress-buffering effects of partner support on eating pathology and other negative lifestyle behaviours relevant to fertility (Kwan and Gordon, 2016, Limbert, 2010).
Limitations and strengths
Whilst this research provides a number of important insights, it is not without limitations. In this study, women had been attempting to conceive for an average of 31 months. One-off measures involved in a cross-sectional design may not fully capture the likely complex relationship of how stress and avoidant coping style act to influence eating pathology longitudinally. Therefore, future research examining coping style and eating pathology across the course of a patient's treatment journey using latent growth curve modelling would be valuable in understanding the causal and temporal aspects of these variables. Second, this study relied upon participants completing sensitive self-report measures with a potential for social desirability response bias. The anonymous completion of the study questionnaire may have served to reduce this bias. Third, whilst the response rate of 44.5% is acknowledged as a further limitation of this study, the sample size requirements for the purposes of structural equation modelling were readily met (Kline, 2011, Preacher and Hayes, 2004).
Limitations notwithstanding, the strengths of the present study include the use of a large, representative cohort drawn from multiple assisted reproductive technology clinics, thereby reducing potential sampling bias. Second, some studies investigating the relationship between stress and eating pathology – such as those carried out in a laboratory – can lack ecological validity, failing to mimic real-life stress and coping experiences (Greeno and Wing, 1994). However, the sampling of patients who were receiving fertility treatment has permitted an investigation of authentic life experiences, with the findings not reliant on an artificial experimental design. Third, the large sample size allowed for use of structural equation modelling providing a methodological advantage over other eating pathology and stress-related fertility studies that use univariate or path analysis statistical designs. Structural equation modelling is the only data analytic strategy that allows simultaneous analysis of multiple relationships between variables measured without error, as the error has been estimated and removed (Tabachnick and Fidell, 2001). Moreover, from a theoretical perspective, it uses a confirmatory approach to data analysis by specifying the relationship among study variables a priori. These empirical findings provide a methodological framework for the investigation of other stress-specific maladaptive health behaviours detrimental to fertility.
Conclusions
Disordered eating attitudes and behaviours have clinical consequences for women undergoing fertility treatment. Stress and coping style have been identified as important variables impacting upon the well-being of fertility patients. The results of this study are in accordance with the existing literature in that a relationship was found between perceived stress and eating pathology, via the intermediary factor avoidant coping style. The results from this study further support the importance of both perceived stress and avoidant coping style as relevant variables to consider in preconception counselling of eating pathology symptoms in infertile patients, with recommendations for referral for adjunct psychological interventions relevant to stress management and coping. Finally, perceived stress and its health outcome response are best viewed as a process of complex intervening factors. As such, this study highlights the advantages of using structural equation modelling, with its advanced statistical capabilities, over traditional univariate analysis, and recommends continued exploration of other fertility-compromising negative health behaviours or lifestyle behaviours within this framework.
Acknowledgements
We are grateful to the women who participated in the study. We thank the nurses of Concept Fertility Centre, Fertility North and Hollywood Fertility Centre who assisted with advertising of the study and participant recruitment.
Biography

Iolanda Rodino is a clinical psychologist in private practice in Perth, Western Australia. She has extensive counselling experience working in the fields of infertility, antenatal and postnatal services. In addition to counselling, she is currently completing a PhD at The University of Western Australia. Her research interests are diverse, and include the areas of third party reproduction and the emotional impact of disordered eating attitudes and behaviours in women undergoing fertility treatment.
Declaration: The authors report no financial or commercial conflicts of interest.
References
- Abraham S., Mira M., Llewellyn-Jones D. Should ovulation be induced in women recovering from an eating disorder or who are compulsive exercisers? Fertil. Steril. 1990;53:566–568. doi: 10.1016/s0015-0282(16)53359-7. [DOI] [PubMed] [Google Scholar]
- Aime A., Sabourin S., Ratte C. The eating disturbed spectrum in relation with coping and interpersonal functioning. Eat. Weight Disord. 2006;11:66–72. doi: 10.1007/BF03327753. [DOI] [PubMed] [Google Scholar]
- Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Arbuckle J.L. IBM SPSS Corp.; Chicago: 2016. AMOS (Version 24.0) [Computer Program] [Google Scholar]
- Ball K., Lee C. Relationships between psychological stress, coping and disordered eating: A review. Psychol. Health. 2000;14:1007–1035. doi: 10.1080/08870440008407364. [DOI] [PubMed] [Google Scholar]
- Benyamini Y., Gefen-Bardarian Y., Gozlan M., Tabiv G., Shiloh S., Kokia E. Coping specificity: the case of women coping with infertility. Psychol. Health. 2008;23:221–241. doi: 10.1080/14768320601154706. [DOI] [PubMed] [Google Scholar]
- Boivin J., Griffiths E., Venetis C.A. Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol's too long: Consider the Brief COPE. Int. J. Behav. Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- Coker E., Lahoud R., Abraham S. Polycystic Ovarian Syndrome and Eating Disorder Quality of Life: A Pilot Study. JFIV Reprod. Med. Genet. 2016;4(171) [Google Scholar]
- Cousineau T., Domar A.D. Psychological impact of infertility. Best Pract. Res. Clin. Obstet. Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Cousins A., Freizinger M., Duffy M.E., Gregas M., Wolfe B.E. Self-report of eating disorder symptoms among women with and without infertility. JOGNN. 2015;44:380–388. doi: 10.1111/1552-6909.12573. [DOI] [PubMed] [Google Scholar]
- Crowther J.H., Sanftner J., Bonifazi D.Z., Shepherd K.L. The role of daily hassles in binge eating. Int. J. Eat. Disord. 2001;29:449–454. doi: 10.1002/eat.1041. [DOI] [PubMed] [Google Scholar]
- Culbert K.M., Racine S.E., Klump K.L. Hormonal factors and disturbances in eating disorders. Curr. Psychiatry Rep. 2016;18 doi: 10.1007/s11920-016-0701-6. [DOI] [PubMed] [Google Scholar]
- Davies M.M., Bekker M.H., Roosen M.A. The role of coping and general psychopathology in the prediction of treatment outcome in eating disorders. Eat. Disord. 2011;19:246–258. doi: 10.1080/10640266.2011.566147. [DOI] [PubMed] [Google Scholar]
- Domar A.D. Impact of psychological factors on dropout rates in insured infertility patients. Fertil. Steril. 2004;81:271–273. doi: 10.1016/j.fertnstert.2003.08.013. [DOI] [PubMed] [Google Scholar]
- Domar A.D., Rooney K.L., Wiegand B., Orav E.J., Alper M.M., Berger B.M., Nikolovski J. Impact of a group mind/body intervention on pregnancy rates in IVF patients. Fertil. Steril. 2011;95:2269–2273. doi: 10.1016/j.fertnstert.2011.03.046. [DOI] [PubMed] [Google Scholar]
- Domar A.D., Zuttermeister P.C., Freidman R. The psychological impact of infertility: a comparison with patients with other medical conditions. J. Psychosom. Obstet. Gynaecol. 1993;14:45–52. [PubMed] [Google Scholar]
- Ebbesen S.M.S., Zachariae R., Mehlsen M.Y., Thomsen D., Hojgaard A., Ottosen L., Petersen T., Ingerslev H.J. Stressful life events are associated with a poor in-vitro fertilization (IVF) outcome: a prospective study. Hum. Reprod. 2009;24:2173–2182. doi: 10.1093/humrep/dep185. [DOI] [PubMed] [Google Scholar]
- Endler N.S., Parker J.D. Multidimensional assessment of coping: A critical evaluation. J. Pers. Soc. Psychol. 1990;58:844–854. doi: 10.1037//0022-3514.58.5.844. [DOI] [PubMed] [Google Scholar]
- ESHRE Capri Workshop Group Nutrition and reproduction in women. Hum. Reprod. Update. 2006;12:193–207. doi: 10.1093/humupd/dmk003. [DOI] [PubMed] [Google Scholar]
- Fairburn C.G., Beglin S.J. Eating Disorder Examination Questionnaire (EDE-Q 6.0) In: Fairburn C.G., editor. Cognitive Behaviour Therapy and Eating Disorders. Guildford Press; New York: 2008. [Google Scholar]
- Frederiksen Y., Farver-Vestergaard I., Skovgard N.G., Ingerslev H.J., Zachariae R. Efficacy of psychosocial interventions for psychological and pregnancy outcomes in infertile women and men: a systematic review and meta-analysis. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-006592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman L.M., Gil K.M. Daily stress, coping, and dietary restraint in binge eating. Int. J. Eat. Disord. 2004;36:204–212. doi: 10.1002/eat.20012. [DOI] [PubMed] [Google Scholar]
- Freizinger M., Franko D.L., Dacey M., Okun B., Domar A.D. The prevalence of eating disorders in infertile women. Fertil. Steril. 2010;93:72–78. doi: 10.1016/j.fertnstert.2008.09.055. [DOI] [PubMed] [Google Scholar]
- Gameiro S., Boivin J., Dancet E., de Klerk C., Emery M., Lewis-Jones C., Thorn P., Van den Broeck U., Venetis C., Verhaak C.M., Wischman T., Vermeulen N. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction – a guide for fertility staff. Hum. Reprod. 2015;30:2476–2485. doi: 10.1093/humrep/dev177. [DOI] [PubMed] [Google Scholar]
- Gameiro S., Boivin J., Peronace L., Verhaak C.M. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum. Reprod. Update. 2012;18:652–669. doi: 10.1093/humupd/dms031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gana K., Jakubowska S. Relationship between infertility-related stress and emotional distress and marital satisfaction. J. Health Psychol. 2016;21:1043–1054. doi: 10.1177/1359105314544990. [DOI] [PubMed] [Google Scholar]
- Gesink Law D.C., Maclehose R.F., Longnecker M.P. Obesity and time to pregnancy. Hum. Reprod. 2007;22:414–420. doi: 10.1093/humrep/del400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K., Rimer B., Viswanath K. fourth edition. John Wiley & Sons; San Francisco, CA: 2008. Health Behavior and Health Education: Theory, Research and Practice. [Google Scholar]
- Gormack A.A., Peek J.C., Jose G.B., Derraik J.G.B., Gluckman P.D., Young N.L., Cutfield W.S. Many women undergoing fertility treatment make poor lifestyle choices that may affect their treatment outcome. Hum. Reprod. 2015;30:1617–1624. doi: 10.1093/humrep/dev094. [DOI] [PubMed] [Google Scholar]
- Gourounti K., Anagnostopoulos F., Potamianos G., Lykeridou K., Schmidt L., Vaslamatzis G. Perception of control, coping, and psychological stress of infertile women undergoing IVF. Reprod. BioMed. Online. 2012;24:670–679. doi: 10.1016/j.rbmo.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Greeno C.G., Wing R.R. Stress-induced eating. Psychol. Bull. 1994;115:444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- Gruenewald T.L., Kemeny M.E., Aziz N., Fahey J.L. Acute threat to the social self: Shame, social self-esteem, and cortisol activity. Psychosom. Med. 2004;66:915–924. doi: 10.1097/01.psy.0000143639.61693.ef. [DOI] [PubMed] [Google Scholar]
- Hair J.F., Black W.C., Babin B.J., Anderson R.E. 7th edn. Pearson Prentice Hall; Upper Saddle River, NJ: 2010. Multivariate Data Analysis. [Google Scholar]
- Heatherton T.F., Baumeister R.F. Binge eating as escape from self-awareness. Psychol. Bull. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hilterschield E., Laessle R. Stress-induced release of GUT peptides in young women classified as restrained and unrestrained eaters. Eat. Weight Disord. 2015;20:435–439. doi: 10.1007/s40519-015-0185-0. [DOI] [PubMed] [Google Scholar]
- Holahan C.J., Moos R.H., Holahan C.K., Brennan P.L., Schutte K.K. Stress generation, avoidance coping, and depressive symptoms: A 10-year model. J. Consult. Clin. Psychol. 2005;73:658–666. doi: 10.1037/0022-006X.73.4.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan G.F., Davies M., Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum. Reprod. Update. 2007;13:209–223. doi: 10.1093/humupd/dml056. [DOI] [PubMed] [Google Scholar]
- Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis. Conventional criteria versus alternatives. Struct. Equ. Model. 1999;6:1–55. [Google Scholar]
- Keyes K.M., Hatzenbuehler M.L., Hasin D.S. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011;218:1–17. doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatzkin R.R., Gaffney S., Cyrus K., Bigus E., Brownley K.A. Stress-induced eating in women with binge-eating disorder and obesity. Biol. Psychiatry. 2016 doi: 10.1016/j.biopsycho.2016.11.002. [DOI] [PubMed] [Google Scholar]
- Kline R.B. Guilford; New York, NY: 2011. Principles and practice of structural equation modeling. [Google Scholar]
- Kouvonen A., Kivimaki M., Virtanen M., Pentti J., Vahtera J. Work stress, smoking status, and smoking intensity: an observational study of 46 190 employees. J. Epidemiol. Community Health. 2005;59:63–69. doi: 10.1136/jech.2004.019752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraaij V., Garnefski N., Schroevers M.J., Weijmer J., Helmerhorst F. Cognitive coping, goal adjustment, and depressive and anxiety symptoms in people undergoing infertility treatment. J. Health Psychol. 2010;15:876–886. doi: 10.1177/1359105309357251. [DOI] [PubMed] [Google Scholar]
- Kupeli N., Norton S., Chilcot J., Campbell C., Schmidt U.H., Troop N.A. Affect systems, changes in body mass index, disordered eating and stress: an 18 month longitudinal study in women. Health Psychol. Behav. Med. 2017;5:214–228. doi: 10.1080/21642850.2017.1316667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan M.Y., Gordon K.H. The effects of social support and stress perception on bulimic behaviors and unhealthy food consumption. Eat. Behav. 2016;22:34–39. doi: 10.1016/j.eatbeh.2016.03.024. [DOI] [PubMed] [Google Scholar]
- Lancastle D., Boivin J. Dispositional optimism, trait anxiety, and coping: unique or shared effects on biological response to fertility treatment? Health Psychol. 2005;24:171–178. doi: 10.1037/0278-6133.24.2.171. [DOI] [PubMed] [Google Scholar]
- Landres I.V., Milki A.A., Lathi R.B. Karyotype of miscarriages in relation to maternal weight. Hum. Reprod. 2010;25:1123–1126. doi: 10.1093/humrep/deq025. [DOI] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer; New York: 1984. Stress, Appraisal and Coping. [Google Scholar]
- Limbert C. Perceptions of social support and eating disorder characteristics. Health Care Women Int. 2010;31:170–178. doi: 10.1080/07399330902893846. [DOI] [PubMed] [Google Scholar]
- Loucks A.B. Energy availability. Curr. Opin. Endocrinol. Diabetes Obes. 2007;14:470–474. doi: 10.1097/MED.0b013e3282f1cb6a. [DOI] [PubMed] [Google Scholar]
- MacNeil L., Esposito-Smythers C., Mehlenbeck R., Weismoore J. The effects of avoidance coping and coping self-efficacy on eating disorder attitudes and behaviors: A stress-diathesis model. Eat. Behav. 2012;13:293–296. doi: 10.1016/j.eatbeh.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Marsh H.W., Hau K.-T., Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indices and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct. Equ. Model. 2004;11:320–341. [Google Scholar]
- Miller G.E., Chen E., Zhou E.S. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol. Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Mircea C.N., Lujan M.E., Pierson R.A. Metabolic fuel and clinical implications for female reproduction. J. Obstet. Gynaecol. Can. 2007;29:887–902. doi: 10.1016/S1701-2163(16)32661-5. [DOI] [PubMed] [Google Scholar]
- Newman E., O'Connor D.B., Conner M. Daily hassles and eating behaviour: The role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32:125–132. doi: 10.1016/j.psyneuen.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Norman R., Chura L., Robker R.L. Effects of obesity on assisted reproductive technology outcomes. Fertil. Steril. 2008;89:1611–1612. doi: 10.1016/j.fertnstert.2007.02.065. [DOI] [PubMed] [Google Scholar]
- Ockhuijsen H., van den Hoogen A., Eijkemans M., Macklon N., Boivin J. The impact of a self-administered coping intervention on emotional well-being in women awaiting the outcome of IVF treatment: a randomized controlled trial. Hum. Reprod. 2014;29:1459–1470. doi: 10.1093/humrep/deu093. [DOI] [PubMed] [Google Scholar]
- Pasch L.A., Holley S.R., Bleil M.E., Shehab D., Katz P.P., Adler N.E. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil. Steril. 2016;106:209–215. doi: 10.1016/j.fertnstert.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Pearson A.N., Heffner M., Follette V.M. New Harbinger Publications Inc.; Oakland, California: 2010. Acceptance & Commitment Therapy for Body Image Dissatisfaction: A Practitioner's Guide to Using Mindfulness, Acceptance & Values-Based Behavior Change Strategies. [Google Scholar]
- Preacher K.J., Hayes A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Razzoli M., Pearson C., Crow S., Bartolomucci A. Stress, overeating, and obesity: Insights from human studies and preclinical models. Neurosci. Biobehav. Rev. 2017;76:154–162. doi: 10.1016/j.neubiorev.2017.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts C.J., Campbell I.C., Troop N. Increases in weight during chronic stress are partially associated with a switch in food choice towards increased carbohydrate and saturated fat intake. Eur. Eat. Disord. Rev. 2014;22:77–82. doi: 10.1002/erv.2264. [DOI] [PubMed] [Google Scholar]
- Rodino I.S., Byrne S., Sanders K.A. Eating disorders in the context of preconception care: fertility specialists' knowledge, attitudes, and clinical practices. Fertil. Steril. 2017;107:494–501. doi: 10.1016/j.fertnstert.2016.10.036. [DOI] [PubMed] [Google Scholar]
- Rooney K.L., Domar A.D. The impact of lifestyle behaviors on infertility treatment outcome. Curr. Opin. Obstet. Gynecol. 2014;26:181–185. doi: 10.1097/GCO.0000000000000069. [DOI] [PubMed] [Google Scholar]
- Rowe E. Early detection of eating disorders in general practice. Aust. Fam. Physician. 2017;46:833–838. [PubMed] [Google Scholar]
- Schmidt L., Holstein B.E., Christensen U., Boivin J. Communication and coping as predictors of fertility problem stress: cohort of 816 participants who did not achieve a delivery after 12 months of fertility treatment. Hum. Reprod. 2005;20:3248–3256. doi: 10.1093/humrep/dei193. [DOI] [PubMed] [Google Scholar]
- Schneider J.E. Energy balance and reproduction. Physiol. Behav. 2004;81:289–317. doi: 10.1016/j.physbeh.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Schwarzer R., Knoll N. Functional roles of social support within the stress and coping process: A theoretical and empirical overview. Int. J. Psychol. 2007;42:243–252. [Google Scholar]
- Stewart D.E., Robinson G.E., Goldbloom D.S., Wright C. Infertility and eating disorders. Am. J. Obstet. Gynecol. 1990;163:1196–1199. doi: 10.1016/0002-9378(90)90688-4. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore R.H., Bulik C.M. Risk factors for eating disorders. Am. Psychol. 2007;62:181–198. doi: 10.1037/0003-066X.62.3.181. [DOI] [PubMed] [Google Scholar]
- Sulkowski M.L., Dempsey J., Dempsey A.G. Effects of stress and coping on binge eating in female college students. Eat. Behav. 2011;12:188–191. doi: 10.1016/j.eatbeh.2011.04.006. [DOI] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S. Allyn and Bacon; Needham Heights: 2001. Using Multivariate Statistics. [Google Scholar]
- Terry D.J., Hynes G.J. Adjustment to a low-control situation: Reexamining the role of coping responses. J. Pers. Soc. Psychol. 1998;74:1078–1092. [Google Scholar]
- Toftager M., Sylvest R., Schmidt L., Bogstad J., Lossl K., Praetorius L., Zedeler A., Bryndorf T., Pinborg A. Quality of life and psychosocial and physical well-being among 1,023 women during their first assisted reproductive technology treatment: secondary outcome to a randomized controlled trial comparing gonadotropin-releasing hormone (GnRH) antagonist and GnRH agonist protocols. Fertil. Steril. 2018;109:154–164. doi: 10.1016/j.fertnstert.2017.09.020. [DOI] [PubMed] [Google Scholar]
- Troop N.A., Holbrey A., Trowler R., Treasure J.L. Ways of coping in women with eating disorders. J. Nerv. Ment. Dis. 1994;182:535–540. doi: 10.1097/00005053-199410000-00001. [DOI] [PubMed] [Google Scholar]
- Van den Broeck U., D'Hooghe T., Enzlin P., Demyttenaere K. Predictors of psychological stress in patients starting IVF treatment: infertility-specific versus general psychological characteristics. Hum. Reprod. 2010;25:1471–1480. doi: 10.1093/humrep/deq030. [DOI] [PubMed] [Google Scholar]
- Verhaak C.M., Smeenk J.M.J., Evers A.W.M., Kremer J.A.M., Kraaimaat F.W., Braat D.D.M. Women's emotional adjustment to IVF: A systematic review of 25 years of research. Hum. Reprod. Update. 2007;13:27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]