Abstract
Background
Insufficient training in infection control and occupational health among healthcare workers (HCWs) in countries with high human immunodeficiency virus (HIV) and tuberculosis (TB) burdens requires attention. We examined the effectiveness of a 1-year Certificate Program in Occupational Health and Infection Control conducted in Free State Province, South Africa in an international partnership to empower HCWs to become change agents to promote workplace-based HIV and TB prevention.
Methods
Questionnaires assessing reactions to the program and Knowledge, Attitudes, Skills, and Practices were collected pre-, mid-, and postprogram. Individual interviews, group project evaluations, and participant observation were also conducted. Quantitative data were analyzed using Wilcoxon signed-rank test. Qualitative data were thematically coded and analyzed using the Kirkpatrick framework.
Results
Participants recruited (n = 32) were mostly female (81%) and nurses (56%). Pre-to-post-program mean scores improved in knowledge (+12%, p = 0.002) and skills/practices (+14%, p = 0.002). Pre-program attitude scores were high but did not change. Participants felt empowered and demonstrated attitudinal improvements regarding HIV, TB, infection control, and occupational health. Successful projects were indeed implemented. However, participants encountered considerable difficulties in trying to sustain improvement, due largely to lack of pre-existing knowledge and experience, combined with inadequate staffing and insufficient management support.
Conclusion
Training is essential to strengthen HCWs' occupational health and infection control knowledge, attitudes, skills, and practices, and workplace-based training programs such as this can yield impressive results. However, the considerable mentorship resources required for such programs and the substantial infrastructural supports needed for implementation and sustainability of improvements in settings without pre-existing experience in such endeavors should not be underestimated.
Keywords: capacity building, healthcare workers, HIV infection control, occupational health, tuberculosis
1. Introduction
The global commitment to the Sustainable Development Goals (SDGs) in 2015 highlighted the need for “recruitment, development, training and retention of the health workforce in developing countries” [1]. Low-and-middle-income countries are faced with particularly severe healthcare worker (HCW) shortages caused by emigration and by the limited capacity to train. As fear of hospital-acquired infections, specifically serious ones such as tuberculosis (TB), is an important contributor to job dissatisfaction [2], one way to contribute to the retention of HCWs and encourage new recruits is to strengthen occupational health (OH) and infection control (IC) practices. Universally recognized guidelines and codes of practice for IC have been articulated by various organizations [3], including guidelines to improve access to human immunodeficiency virus (HIV) and TB prevention, care, and support [4]. However, such measures are not implemented in many settings in low income countries [5], [6], including in South Africa [7], [8] where there is a high population prevalence of TB, with some studies suggesting that HCWs are three times more likely to acquire TB than the general population [9].
The need to build capacity in OH and IC in low-and-middle-income countries is undeniable, yet there are few interventions described in the literature addressing either of these, let alone the two combined. Most training interventions are brief, cover only basic content, and are not reinforced over time, resulting in an inability to retain and translate knowledge to the workplace in a sustainable manner [10], [11], [12]. Nursing education in IC practices has also been found to be lacking due to limited teaching time dedicated to IC and the persistence of out-of-date IC policies used in teaching; furthermore, severe staff shortages and quick staff turnovers have led to groups of staff who have been practicing but without ever receiving designated IC training [13]. A literature review of IC education/interventions by Ward in 2011 examined 39 studies from around the world (over half in the United States, United Kingdom, and Canada), and found limited strong evidence on the efficacy of training programs for improving IC practices and reducing infection [10]. Evidence is also lacking on the effectiveness of various training approaches. The results from this study also point toward a need for capacity-building programs that include robust evaluation components. A review of the literature for more ambitious interventions reveals that many IC [10] and OH [12] training intervention studies have been conducted, but that the majority of these are restricted to brief, surface-level, and narrowly focused knowledge and skills training, and result in effects that are too often short-lasting [10], [12]. Diminishing retention of knowledge, attitudes, and practices with time was observed by Suchitra and Devi in a 2007 paper [11], in which they described an IC training program and the immediate subsequent improvement in knowledge, attitudes, and practices among HCWs. The evaluative measure was repeated at 6 months, 12 months, and 24 months, and the authors concluded that the degree of improvement declined as time progressed. These findings highlight the need for OH and IC interventions that have impacts long after would-be trainees have forgotten the information imparted to them. To reach such a goal, it is argued that HCWs need to be empowered to care for and protect themselves and their community of HCWs. The process of empowerment not only requires that HCWs acquire a sense of agency but that contextual factors allow this agency to be implemented [14], as in the case of IC practices, for which knowledge, without corresponding environmental factors supporting them, does not translate into practice [15].
To enable effective, long-term IC and OH interventions, the process of empowering HCWs to protect themselves not only requires that HCWs acquire a sense of agency, and the ability to consider and deliberately choose a course of action, but that contextual factors must allow this agency to be implemented. There is an urgent need to understand how to best develop and deliver an effective capacity building program for HCWs that addresses their unique occupational and infection prevention hazards with respect to HIV and TB control, while taking into consideration resource constraints. The objective of this study was to examine the effectiveness of a 1-year Certificate Program in Infection Control and Occupational Health in Free State Province, South Africa aimed at empowering HCWs to act as change agents for improving workplace-based HIV and TB prevention. Specifically, we aimed to determine if this Certificate Program was a viable model for: (1) acquiring and improving knowledge, attitudes skills and practices (KASPs) of participants; (2) applying KASPs in their workplace interventions; and (3) effecting meaningful impacts in their workplace through their workplace interventions. In addition, our team tried to determine the extent to which the capacity built among the health workforce was sustainable as well as to document lessons learned in implementing the program.
2. Materials and methods
2.1. Certificate Program description
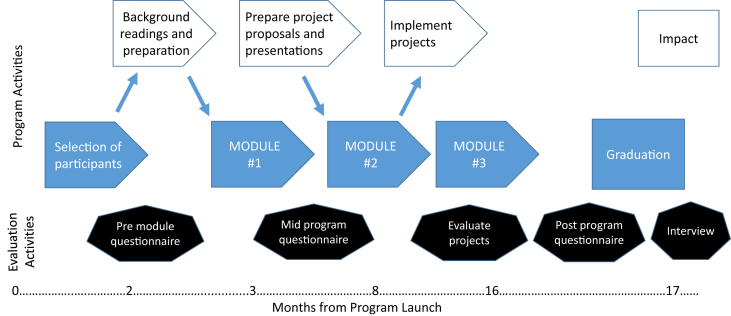
The Certificate Program was launched within an already established collaboration between Canadian and South African researchers focused on building capacity in OH and IC in the Free State Province of South Africa [16], [17]. Within this context, the Global Health Research Program of the University of British Columbia and the Centre for Health Systems Research & Development at the University of the Free State (South Africa) received funding from Canada's Global Health Research Initiative (GHRI) to pursue this initiative. Beginning in March 2011, the Certificate Program recruited OH and IC practitioners as well as participants who had responsibility in OH and IC such as health and safety committee members, managers, health program coordinators, and health students [18]. The recruitment of participants was facilitated by the Free State Department of Health, who contacted health facility managers across the province to gain support and to recommend participants for the program. A recruitment brochure was also distributed across local facilities. An overview of the Program design and timeline is provided in Fig. 1. Prospective participants were required to send a letter of interest, provide their curriculum vitae as well as an employer's letter of support. The Certificate Program consisted of three 4-day, face-to-face modules and workplace-based group projects expected to address identified gaps in OH and IC, environmental arrangements, and/or policies/procedures. The program was intended to impart OH and IC knowledge, skills, and practices, including the basics of HIV and TB prevention, diagnosis, treatment, care, and support. It also provided an overview of healthcare workplace HIV and TB programs, the ethical and sociocultural issues related to workplace research, and relevant legislation, policies, and guidelines. Additionally, research methods involving program planning, implementation, and evaluation were taught. These included data collection methods such as survey design and administration, and focus group and key informant interview methods, along with data analysis methods. Attitudes and stigma related issues were also targeted, although less time was dedicated to this aspect.
Fig 1.
Timeline of evaluation activities.
Prior to the first module, participants were sent background documentation and readings that included an overview of OH and IC guidelines, as well as other relevant materials. The first module focused on knowledge and skill building using a combination of didactic presentations and problem-based learning. At the end of the first module, participants were separated into eight groups, based on workplaces or positions, and were asked to prepare a project proposal to address a program-relevant issue that they identified so that it could be developed further at the second module. The resulting project proposals were each reviewed by several of the Canadian and South African mentors. The second module was project specific, and groups worked directly with their topic expert mentors to refine their proposals and present them to their classmates for feedback. Mentors attempted to keep group proposals close to the original goals and objectives, in line with Free State Department of Health overall needs, and conforming to the program mandate. During the rest of the second module, guest lecturers filled gaps in KASPs that were identified as weaknesses during program monitoring. The project teams then returned to their facilities to implement their proposals and collect data. Locally based mentors and graduate students followed up with participants at their facilities to assess their progress and provide support where needed. The final module focused on completing the data analysis and interpretation for the group projects and presenting the results. On the last day a graduation ceremony was held, during which the participants presented their projects to a larger audience of stakeholders from the provincial and national levels, as well as their friends and family.
2.2. Conceptual framework for evaluation
The program evaluation was guided by an adapted Kirkpatrick framework [19] for assessing training programs. This assessed: (1) reactions to the content and teaching methods of the module and reactions to the projects; (2) learning of KASPs regarding HIV and TB transmission and prevention, OH and IC policies and guidelines, research methods, program implementation and evaluation methods, as well as ethics; (3) behavior changes in work practices, application of knowledge, skills, and practices; and (4) outcomes that originated both from the participants' reactions, learning, behavior and attitude changes, as well as their projects. The adapted framework considered these elements within the context of the processes and dynamics of the program, projects, and the wider context of the partnership and institutional frame. This mixed methods study was approved under University of British Columbia Ethics Certificate number H10-01879.
2.3. Questionnaires
Quantitative data were obtained from participant self-administered questionnaires and analyzed pre-, mid-, and postprogram. Reactions to the program as well as KASPs were measured using a five-point Likert-style scale and true/false questions. Questionnaire items were summed into composite scores based on thematic similarity and congruency. Wilcoxon signed-rank test identified any significant differences between questionnaire results and background (preprogram questionnaire) characteristics. The same method was used to analyze the significance between the pre-, mid-, and postprogram results for the categories (KASPs) and subcategories of composite scores. In the case of multiple comparisons, a Bonferroni correction was applied according to the number of comparisons that were made.
2.4. Interviews, qualitative project evaluation, and participant observations
Semistructured interview guides were used to provide a richer analysis of participants and local mentors' experiences. The midterm interviews were conducted with 27 of the remaining 28 participants (1 participant being unavailable at the time of interviews, and the remaining 4 having exited the program). Final interviews included 19 of the 28 participants (at which point data saturation was judged to have been reached); all of whom had also been interviewed in the midterm evaluation. Additionally, five of the 12 mentors, all South African, were conveniently sampled and interviewed at completion of the program. Participant observations complemented the data acquired from questionnaires and interviews, providing insight into the projects completed by participants, including understanding the dynamics of the program and shedding light on the challenges and barriers within the program. The interview data were transcribed verbatim into QSR International Nvivo 10 Software. Open coding was utilized for the initial inductive coding in Nvivo to generate a coding tree. The first 10 transcripts (random order) were split and coded with a second researcher. Codes from each were then compared, and differences were reconciled through discussion and reference to the literature. Themes were categorized to reflect the interview guides. Thematic analysis was used to identify and combine key emerging themes [20]. These were then applied to the Kirkpatrick framework to reflect the four thematic areas: learning, behavior, outcomes, and reactions. Detailed field notes were collected daily and analyzed using a wide and narrow perspective to understand viewpoints of individual participants and the context of the program and its institutional and environmental context [21]. A descriptive approach was used to evaluate the group projects at their distinct phases: planning, implementation, and evaluation.
3. Results
3.1. Background characteristics and KASPs
Participants were mainly female (81%), and 44% were aged 40–49 years (Table 1). While participants were expected to predominantly be OH or IC professionals, only 56% reported being nurses that could hold these roles. Pre- to postprogram, significant changes in scores were observed among females (+10%, p = 0.002) but not among males; among healthcare professionals (+12%, p = 0.003); and among those who reported having had some training in three of the five training items (+7%, p = 0.007) (Table 1). The increase in scores from pre- to midquestionnaires was greater than from pre- to postquestionnaires. In some categories, a statistically significant decrease in scores was observed from mid- to postquestionnaires. Knowledge, skills, and practices item scores statistically increased from pre- to postquestionnaire results, peaking at the midprogram questionnaire (Table 2). From pre- to postprogram, mean scores for knowledge items increased from 67.8% to 79.7% (p = 0.002). The mean score for skills and practices items also increased significantly from pre- to postprogram, from 57.0% to 71.4% (p ≤ 0.001). Among the six subcategories assessed, five showed a significant improvement from pre- to postprogram. Among these, the OH policies, procedures, and guidelines, and research/program implementation improved the most.
Table 1.
Pre-, mid-, and postquestionnaire results (all KASPs Likert-style items combined)
| Characteristics | Total |
Pre–Post |
Pre (n = 32) |
Mid (n = 30) |
Post (n = 24) |
Pre–Mid |
Mid–Post |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Z (p)∗ | n | μ (SD) (%) | n | μ (SD) (%) | n | μ (SD) (%) | Z Score(p) | Z Score (p) | |
| Age (y) | ||||||||||
| 20–39 | 9 (28) | 2.2 (0.030) | 9 | 60.9 (9.6) | 9 | 80.9 (10.2) | 8 | 78.1 (10.7) | 2.5 (0.110) | −0.6 (0.575) |
| 40–49 | 14 (44) | 1.4 (0.161) | 14 | 72.0 (10.7) | 12 | 83.2 (7.6) | 8 | 77.0 (8.0) | 2.6 (0.009) | −2.1 (0.035) |
| 50–59 | 9 (28) | 2.3 (0.021) | 9 | 65.7 (5.5) | 9 | 84.8 (6.4) | 8 | 76.5 (8.9) | 2.7 (0.008) | −2.4 (0.017) |
| Sex | ||||||||||
| Male | 6 (19) | 1.6 (0.109) | 6 | 69.4 (9.2) | 5 | 83.2 (6.9) | 3 | 79.4 (8.4) | 2.0 (0.043) | −0.5 (0.593) |
| Female | 26 (81) | 3.0 (0.002) | 26 | 66.5 (10.4) | 25 | 82.9 (8.4) | 21 | 76.9 (10.5) | 4.1 (<0.001) | −2.9 (0.004) |
| Workplace | ||||||||||
| Department of Health | 6 (19) | — | 6 | 77.0 (11.6) | 4 | 87.1 (2.5) | 1 | 83.8 (0) | 1.1 (0.273) | — |
| Pelonomi Hospital | 8 (25) | 2.4 (0.180) | 8 | 64.8 (6.4) | 8 | 86.5 (6.4) | 7 | 83.1 (4.5) | 2.5 (0.012) | −2.2 (0.027) |
| Universitas Hospital | 13 (41) | 2.6 (0.009) | 13 | 65.1 (8.4) | 13 | 81.4 (8.9) | 13 | 73.6 (9.2) | 3.1 (0.002) | −2.6 (0.009) |
| Other | 5 (16) | 1.1 (0.285) | 5 | 63.8 (12.5) | 5 | 78.1 (8.4) | 3 | 76.9 (10.8) | 1.8 (0.080) | −0.5 (0.593) |
| Occupation | ||||||||||
| Healthcare professional | 18 (56) | 3.0 (0.003) | 18 | 65.1 (8.3) | 18 | 81.4 (8.3) | 17 | 76.3 (9.0) | 3.6 (<0.001) | −2.6 (0.009) |
| Community level | 3 (9) | — | 3 | 68.2 (8.5) | 2 | 84.0 (11.5) | 0 | — | 1.3 (0.180) | — |
| Hospital admin/tier 1 management | 6 (19) | 1.2 (0.248) | 6 | 70.7 (12.4) | 6 | 87.4 (6.6) | 6 | 78.1 (9.1) | 2.0 (0.046) | −2.2 (0.026) |
| District/provincial/academic | 5 (16) | — | 5 | 69.1 (15.2) | 4 | 82.9 (7.9) | 1 | 87.5 (0) | 1.8 (0.068) | — |
| Training | ||||||||||
| Yes | 8 (25) | 2.7 (0.007) | 16 | 70.0 (10.9) | 15 | 83.2 (8.3) | 12 | 76.8 (9.6) | 3.4 (0.001) | −1.7 (0.099) |
| No | 24 (75) | 2.0 (0.410) | 16 | 64.2 (8.7) | 15 | 82.8 (8.0) | 12 | 77.7 (8.6) | 3.1 (0.002) | −2.7 (0.007) |
— denotes values that were not available due to a limited or absent population size.
SD, standard deviation.
Z scores and p values are the result of the Wilcoxon-signed rank test.
Table 2.
Pre-, mid-, and postquestionnaire results by category of items
| Category of items | Pre–Post |
Pre (n = 32) |
Mid (n = 30) |
Post (n = 24) |
Pre–mid |
Mid–post |
|---|---|---|---|---|---|---|
| Z score (p)∗ | μ (SD) (%) | μ (SD) (%) | μ (SD) (%) | Z score(p) | Z score (p) | |
| Main categories | ||||||
| Knowledge | 3.1 (0.002) | 67.8 (14.6) | 86.5 (9.5) | 79.7 (9.6) | 4.5 (<0.001) | −3.2 (0.002) |
| Skills/practice | 3.6 (<0.001) | 57.0 (2.3) | 76.3 (11.6) | 71.4 (12.4) | 4.6 (<0.001) | −2.6 (0.008) |
| Attitudes | 0.1 (0.930) | 84.9 (1.6) | 85.8 (8.9) | 81.5 (12.3) | 1.2 (0.240) | −1.8 (0.079) |
| True/False | 1.9 (0.054) | 68.0 (18.2) | 85.4 (18.9) | 74.5 (17.9) | 3.7 (<0.001) | −2.2 (0.028) |
| Subcategories | ||||||
| Occupational health/infection control | 2.0 (0.050) | 72.8 (17.9) | 87.2 (12.1) | 81.7 (9.3) | 4.0 (<0.001) | −2.9 (0.004) |
| HIV | 2.5 (0.013) | 82.3 (14.6) | 93.3 (9.3) | 91.1 (12.4) | 3.4 (0.001) | −1.1 (0.270) |
| Tuberculosis | 2.9 (0.004) | 68.9 (19.4) | 90.5 (10.2) | 82.7 (15.3) | 4.4 (<0.001) | −2.6 (0.010) |
| HIV/TB Co-infection | 2.7 (0.007) | 67.5 (23.7) | 92.7 (9.8) | 81.7 (18.6) | 4.1 (<0.001) | −2.7 (0.007) |
| Occupational policies, procedures and guidelines | 3.2 (0.002) | 59.2 (18.6) | 81.5 (13.7) | 71.3 (13.2) | 4.5 (<0.001) | −3.0 (0.002) |
| Research/program implementation | 3.8 (<0.001) | 52.5 (14.9) | 73.7 (13.1) | 69.4 (13.2) | 4.7 (<0.001) | −1.9 (0.063) |
HIV, human immunodeficiency virus; SD, standard deviation; TB, tuberculosis.
Z scores and p values are the result of the Wilcoxon-signed rank test.
3.2. Group projects and practice outcomes
An important feature of this certification program was the undertaking of practical research projects in the workplace, providing an opportunity to apply the knowledge being gained and learn from the challenges being encountered. The eight group projects took place in six distinct settings, where 544 participants (participants of program participants) were surveyed or directly received an intervention. In other cases, groups focused on OH and IC needs assessments or studying the feasibility of implementing a cough registry program and developing associated tools and procedures (Table 3). The projects yielded results affecting positive improvement in individual and organizational IC and OH awareness and practices but these positive results were not achieved without substantial mentor support. Group project documentations showed that participants had considerable difficulties in each distinct phase of their projects (planning, implementing, and evaluating) and that great mentor support was required at all project stages. Nonetheless, excellent projects were conducted. One of the projects resulted in a publication that highlighted approaches to blood and body fluid exposure in a small rural hospital [22], and all generated impacts in their facilities.
Table 3.
Group project descriptions, results, and key findings
| Groups | Topics/objectives | Interventions | Results and key findings |
|---|---|---|---|
| 1 | Improving utilization of workplace HIV/AIDS program for HCWs at Pelonomi Hospital |
Assess HCWs views on the OH services and HIV stigma (n = 344) | HCWs underutilized the OH services because of stigma, potential breaches of confidentiality and lack of awareness |
| 2 & 3 | Reducing the risk of DOTS supporters acquiring TB during home visits in Bloemfontein and Welkom | Two-day training (informed by baseline questionnaires) (n = 23) | Training recommended for OH services staff |
| 4 | Creating a safe environment for patients and staff in the Bronchoscopy theatre at Universitas Hospital | Training session (informed by baseline questionnaires) (n = 14) Information pamphlet produced and distributed Environmental risk assessment |
Awareness campaign among HCW to promote the OH services and reduce workplace stigma |
| 5 | Investigating TB infection control knowledge, practices, and environment in the medical outpatient department at Pelonomi Hospital | Assess TB IC practices (n = 21) | Low baseline knowledge on IC, use of PPE, and hand hygiene practices |
| 6 | Blood and body fluid exposure in the workplace | Assess BBF exposures knowledge and HCWs knowledge and attitudes towards OH and IC services (n = 74) | Administrative controls and use of PPE were lacking |
| 7 | Strengthening the occupational health clinic for the management of TB and HIV in the healthcare workplace at Universitas Hospital | Assess the feasibility of implementing a cough registry (n not available) | Training successfully improved TB knowledge, attitudes, and beliefs regarding TB IC |
| 8 | Infection control and workplace safety: knowledge and practices in a large laundry facility | Assess the IC, safety, and OH service knowledge and practice of workers (n = 68) | Recommended regular refresher in-service training and improved access to PPE |
BBF, blood body fluids; DOTS, directly observed treatment, short-course; HCW, healthcare worker; HIV, human immunodeficiency virus; OH, occupational health; IC, infection control; PPE, personal protective equipment; TB, tuberculosis.
3.3. Reactions and challenges
Participant reactions to the program and its various components were mixed but predominantly conveyed satisfaction with the program. Reaction item scores from the questionnaires showed that seven of the eight sets of items were given scores > 75%. One of the reactions most often mentioned was “eye-opening”, and its ambitiousness often recognized as seen in this quote by a hospital nurse: “I've never been involved in such a constructive research programme, because the ones we did at university or the ones that I was involved in were not this huge, this project is really huge for the future.”
Barriers to implementing workplace interventions could be categorized into those related to: (1) time, resources, and logistics, and (2) institutional capacity. The most often cited challenge was limited time availability.
3.4. Program-wide learning
The two major themes that emerged under the learning domain were: (1) OH and IC knowledge and skills; and (2) research and workplace intervention knowledge and skills. Responses indicated that OH and IC knowledge, skills, and practices were practical and easy to apply in the workplace. Participants reported being better able to identify workplace hazards, and stated that the Program reinforced their existing knowledge. Some participants discussed a new appreciation for and the realization of the interconnectedness of OH and IC. An IC nurse described this realization in this way: “Now, if I identify a hazard, I involve both the patient and the HCW. [Before,] I had a demarcation that [it] does not involve me if it [concerns] a HCW, it is [an] occupational health problem […]. I only identify now with this programme; that it’s very important for IC and OH [to work together].”
Many participants also highlighted the value of the program for demystifying the research process and giving them confidence to conduct research. Furthermore, the benefit of the practical component of the program was also apparent, as described by an assistant nurse manager in the following quote: “I learned about research before but when put in practice, it becomes real. There is no replacement for real world experience.”
3.5. Behaviour and workplace practices
Under the behaviour domain, respondents expressed improved collaboration between their peers and mentors, and engagement with managers and unions. The following quote from a nongovernmental organization project manager describes this improvement: “this project has made me come closer to my manager, especially the deputy director. [Management is] so supportive and so interested in what I am doing.” Participants also reported improved IC behaviours among themselves and their colleagues by using correct personal hygiene and personal protective equipment procedures and by advising and promoting these to their colleagues. Participants also reported a heightened awareness for environmental and procedural IC hazards. An assistant nursing manager described such changes in this way: “when we cough, we follow the [cough] etiquette now and [we are] also opening the windows when we sit in an office.”
3.6. Program-wide outcomes
The outcome domain highlighted improvements beyond the individual level changes reported. Participants often reported that they were able to make changes in their workplaces themselves or that subsequent to recommendations to management, corrective measures were applied. The most reported changes in the application of knowledge were with regards to IC measures and practices. Participants noted improvements in the safe collection of sputum samples; appropriate use of personal protective equipment; and use of environmental controls and application of algorithms to identify and segregate high-risk patients (e.g., identification and spatial separation of the coughing patient, offering testing to all patients for HIV on admission). An example of such changes is described in the following quote from a geriatrics nurse: “Normally, we didn't isolate the patients that were coughing. [Since] the [program], now we are isolating them and we take the sputum. If they are positive, they will start treatment and remain in isolation. We didn't isolate until this course and we would also sometimes discharge patients that have a cough without testing. Now if there is a cough, they get tested.”
Another outcome that was often raised by participants was the role of the Program in changing their attitudes by: (1) empowering them and elevating their morale, improving confidence and motivation; and (2) increasing their awareness. Participants reported that their knowledge and skills had: empowered them to voice their opinions and take actions; built their confidence to discuss and present their findings from the projects; and built their confidence to engage in further research, project design and implementation.
In some cases, program participants were also able to change the attitude of their colleagues. In the following quote by an OH nurse, fellow employees are described as being comfortable using the OH services at their hospital rather than going to an HIV-dedicated center outside the hospital (Centre for Excellence): “[the] project has some positive impact for the hospital, people with HIV are now able to go to the OHS here, while before they would have to go to the Center for Excellence [specialist care for persons with HIV]”.
3.7. Mentor perspective
Many mentors discussed the value in training participants who were working “on the ground”, using words such as motivated, committed, and energetic to describe the participants. The mentors generally expressed the view that participants' weaknesses were mostly related to not having sufficient baseline knowledge in research methods, writing and computer skills to implement projects without considerable assistance.
3.8. Participant observations
The lack of basic computer skills left many participants unable to easily implement the practical component of the Program. The limited baseline knowledge and skills in designing and implementing workplace interventions negatively affected the ability of some participants to grasp some of the topics and materials related to research and workplace intervention methods. Participants often deferred decisions to mentors and researchers, not seeming to trust that they would meet expectations on their own, and preferring to follow instructions. As such, participants and groups required a large amount of mentor time and resources to assist them in implementing their workplace-based intervention projects.
4. Discussion
The study responds to the call for more evaluative studies on how to improve OH and IC [23], [24]. This training program resulted in improving KASPs in OH and IC, which is consistent with findings of other researchers [25], [26]. More specifically, Gammon and colleagues [27] found that compliance with IC measures does improve following a structured intervention, but their review of the literature concluded that research fails to indicate the duration of the impact. Another key factor in the uptake of IC measures is management commitment to health and safety [28]. Our findings support the importance of a high level of management support when undertaking such initiatives in order for them to be successful.
Participants in our program were able to successfully apply their KASPs through workplace interventions, although this varied, as did the extent to which meaningful and sustained changes seemed likely. Although a decline was found between mid- and postprogram questionnaire scores, pre- to postprogram questionnaire scores significantly increased. The decrease from mid- to postprogram questionnaire scores is thought to be attributable to participants' initially rating themselves high, but after experiencing difficulties during the project implementation phase of the program and after receiving feedback from mentors, they may have realized the more accurate extent of their knowledge, skills, and practices. Similar changes in perceived learning have also been observed elsewhere [29]. Another potential factor in this effect is the long time that elapsed between the first module and final module. While the first module was dominated by didactic teaching that focused on most of the subjects assessed in the questionnaires, the final module came after a period in the Program that focused largely on project implementation, for which there were fewer assessment items in the questionnaires. The evaluation extended to 2 months after completion of the Program, and, as such, long-lasting changes could only be inferred from participants' reports on their intentions to continue to use their capacity to affect further change.
Some workplace projects set simple measurable objectives, while others had more complex objectives, sometimes moulded by mentors to fit into larger collaborative projects between the Canadian and South African researchers [15], [30], [31], [32], [33]. Despite the good intentions on the part of the mentors, those groups with simple, measurable objectives that were not part of larger endeavours, were most confident, had the least difficulty with their projects, and seemed to learn the most.
It is well established that the successful implementation of IC practices by HCWs is influenced by individual, organizational, and environmental factors [34]. Others have emphasized the importance of social environments, peer group pressure, their own experiences, modeling [35], as well as management support [35]. While improvements in interpersonal skills, teamwork, and group dynamics were identified as important outcomes of this Certificate Program, power relations and institutional challenges remained. While many OH and IC trainings have been described in the literature [9], [10], [11], they have tended to focus on specific KASPs that are necessary to follow OH and IC guidelines, and have often neglected the upstream factors that lead HCWs to falling back to inappropriate OH and IC practices.
A lesson learned here is that a capacity-building program such as this one must be based on a realistic appraisal of the baseline knowledge and skills of participants. This is critical if what is being taught is to be implemented and the learning sustained. It is noteworthy that those who reported to have previously had relevant training showed a statistically significant increase in KASP questionnaire items pre- to postprogram when compared with those who did not report relevant training. These results point to the importance of considering participants' baseline capacities in the development of such programs. Questionnaire results further showed that while participants were found, for example, to have significantly increased their knowledge and skills in the category of research and program implementation, postprogram results still found that participants still rated themselves at a low absolute level of 69%. The apparent difference between women in comparison to the small number of men in the course disappeared in a gendered analysis of the results that recognized that men and women had different occupations in the health sector, and observed no male–female differences among those who had previously received training or were health professionals, which were the characteristics rather than sex that were associated with the differences observed.
The challenge of this capacity building program was further complicated by impacts of the legacy of apartheid and neoliberalism [36], [37] that intensified the weaknesses being addressed. During the apartheid period, the country experienced extreme racial discrimination, high income inequalities, devastation of families, contrived labor migrations, and substantial violence [38]. The educational and health systems, which provided the focus of this study, were particularly affected and were left with deep scars that have persisted into the present-day post-apartheid period. These sectors were expressly segregated by race, with nonwhite health and education services systematically underfunded and undermined, resulting in systematic disempowerment of the majority people and their institutions [38].
This legacy has greatly affected the education levels of workers in the healthcare system and throughout society, rendering in “most individuals emerging from secondary (and often tertiary) education with limited numeracy, literacy, and problem solving skills [37]” – considerably limiting worker capacities [37], [39]. These factors shaped the persistent maldistribution of HCWs, their poor skill level, their disenfranchisement, and their substandard, inadequately staffed and inadequately resourced work environment [37].
Furthermore, the post-Apartheid South African government commitment to austerity policies that accompanied South Africa's integration into the global economy severely limited any increases in public spending [36]. This led to further intensification of social and economic disparities in post-Apartheid South Africa [40]. In the context of a health system meeting unprecedented challenges but with restricted budgets, concerns over issues such as senior management inexperience and lack of proper training combined with the general problems of understaffing have been noted as reasons for some of the difficulties that the health systems is undergoing [37].
The results in this study suggest that while such collaborative educational programs are indeed worth offering, however, more attention is also needed to consider the upstream socioeconomic factors driving inadequate staffing, poor education, and insufficient resources if such educational efforts are to have a profound and long-lasting impact.
Nonetheless, many important advances were made with respect to new policies and programs; for example, the process of conducting needs assessments and identification of OH and IC deficiencies in various workplaces to provide recommendations and inform policy decisions; and a feasibility study for a cough registry program and the subsequent development of tools and procedures for the detection of TB among HCWs and concomitant training of operational managers in the use of these tools and procedures. While further research is necessary to determine whether the considerable resources invested justify the outputs, the magnitude of the problem of HIV and TB in HCWs is such that efforts such as this one need to continue. The complexity of issues involved in successful implementation suggests the desirability of North–South–South collaborations [15] with a strong southern partner that not only can provide technical support during the capacity-building program but also help sustain gains made. The strong southern partner, working with the northern partner can facilitate adoption in the weaker southern setting of effective strategies drawn from broader knowledge and experience. However, adequate resources need to be planned to facilitate such collaborations, if they are to be effective.
A workplace-based capacity building Certificate Program can impart improvements in the KASPs needed by HCWs in the areas of OH and IC. Additionally, such a program is able to affect meaningful change within workplaces through the agency of empowered participants leading workplace interventions. Such improvements on a personal and organizational level contribute to increasing HCW health and well-being through improved recognition, job satisfaction, morale, and safety in their workplaces. By improving OH and IC practices, such a program could also help reduce nosocomial infection, and increase HIV and TB care, leading to a healthier, more resilient healthcare workforce. While this study provides evidence to support OH and IC training programs in high-risk, low-resource settings, a set of basic requirements is needed to increase the likelihood of sustainable success. These include, first, ensuring that participants chosen for such programs have a strong enough knowledge and skill foundation to be able to meet the objectives of the program, or be prepared to provide the extensive mentorship needed. Second, appropriate organizational resources and equipment in place, including commitment from management to spend the needed time to implement the interventions. Third, clear national and regional policies and guidelines must be in place to support implementation of OH and IC interventions. Last, the overall context, with its unique historical, political and economic realities, must figure prominently in the planning of such programs.
Acknowledgments
We thank the participants of the Program, mentors, and researchers who aided in the Program, the Global Health Research Initiative (GHRI) for their funding, and the Free State Provincial Department of Health. Particular thanks are due to Karen Lockhart for her contributions throughout this study.
Conflicts of interest
All authors have no conflicts of interest to declare.
References
- 1.United Nations Development Program (UNDP) UNDP; Geneva: 2015. The 2030 Agenda for Sustainable Development. [Google Scholar]
- 2.Yami A., Hamza L., Hassen A., Jira C., Sudhakar M. Job satisfaction and its determinants among health workers in jimma university specialized hospital, southwest ethiopia. Ethiopian J Health Sci. 2011;21:19–27. [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) WHO; Geneva: 2009. WHO Policy on TB infection control in health-care facilities. [PubMed] [Google Scholar]
- 4.World Health Organization (WHO), International Labor Organization, Joint United Nations Programme on HIV/AIDS . WHO; Geneva: 2010. Joint WHO-ILO-UNAIDS policy guidelines on improving health workers’ access to HIV and tuberculosis prevention, treatment, care and support services. [Google Scholar]
- 5.Jahangiri M., Rostamabadi A., Hoboubi N., Tadayon N., Soleimani A. Needle stick injuries and their related safety measures among nurses in a university hospital, Shiraz, Iran. Saf Health Work. 2016;7:72–77. doi: 10.1016/j.shaw.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yenesew M.A., Fekadu G.A. Occupational exposure to blood and body fluids among health care professionals in bahir dar town, northwest ethiopia. Saf Health Work. 2014;5:17–22. doi: 10.1016/j.shaw.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sissolak D., Marais F., Mehtar S. TB infection prevention and control experiences of South African nurses – a phenomenological study. BMC Public Health. 2011;11:262. doi: 10.1186/1471-2458-11-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehtar S. Lowbury Lecture 2007: infection prevention and control strategies for tuberculosis in developing countries - lessons learnt from Africa. J Hosp Infect. 2008;69:321–327. doi: 10.1016/j.jhin.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 9.University Research Co., Tuberculosis in healthcare workers: findings from South Africa; University Research Co. [Internet]. 2008 [cited 2016 Sep 15]. Available from: http://www.urc-chs.com/resources/tuberculosis-healthcare-workers-findings-south-africa
- 10.Ward D. The role of education in the prevention and control of infection: a review of the literature. Nurse Educ Today. 2011;31:9–17. doi: 10.1016/j.nedt.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Suchitra J., Devi N. Impact of education on knowledge, attitudes and practices among various categories of health care workers on nosocomial infections. Ind J Med Microbiol. 2007;25:181–187. doi: 10.4103/0255-0857.34757. [DOI] [PubMed] [Google Scholar]
- 12.Robson L.S., Stephenson C.M., Schulte P.A., Amick B.C. A systematic review of the effectiveness of occupational health and safety training. Scand J Work Environ Health. 2012;38:193–208. doi: 10.5271/sjweh.3259. [DOI] [PubMed] [Google Scholar]
- 13.Mehtar S, Marais F, Aucamp M. From policy to practice – education in infection prevention and control. Int J Infect Control [Internet]. 2011 [cited 2017 Aug 26];7(i2). Available from: http://www.ijic.info/article/viewFile/7235/5818. [date accessed: 2016 Feb 21].
- 14.World Bank . World Bank; Washington DC: 2007. Empowerment in practice: analysis and implementation. [Google Scholar]
- 15.Mortell M. Hand hygiene compliance: is there a theory-practice-ethics gap? Br J Nurs. 2012;21:1011–1014. doi: 10.12968/bjon.2012.21.17.1011. [DOI] [PubMed] [Google Scholar]
- 16.Yassi A., Zungu M., Kistnasamy B., Spiegel J., Lockhart K., Jones D. Protecting health workers from infectious disease transmission: an exploration of a Canadian–South African partnership of partnerships. Global Health. 2016;12:10. doi: 10.1186/s12992-016-0145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yassi A., Nophale L.E., Dybka L., Bryce E., Kruger W., Spiegel J. Building capacity to secure healthier and safer working conditions for healthcare workers: a South African–Canadian collaboration. Int J Occup Environ Health. 2009;15:360–369. doi: 10.1179/oeh.2009.15.4.360. [DOI] [PubMed] [Google Scholar]
- 18.Liautaud A., Yassi A., Engelbrecht M.C., O'Hara L.M., Rau A., Bryce E.A., Nophale L.E. Building capacity to design, implement and evaluate participatory action research projects to decrease the burden of HIV and promote and protect the health and safety of the healthcare workforce: a South African–Canadian Collaboration. Open Med. 2013;7:S33. [Google Scholar]
- 19.Bullock A., Morris Z.S., Atwell C. Collaboration between health services managers and researchers: making a difference? J Health Services Res Policy. 2012;17(Suppl 2):2–10. doi: 10.1258/jhsrp.2011.011099. [DOI] [PubMed] [Google Scholar]
- 20.Kvale S. Sage Publications; Thousand Oaks, California: 1996. Interviews: an introduction to qualitative research interviewing. [Google Scholar]
- 21.Merriam S.B. Sage Publications; Thousand Oaks, California: 1998. Qualitative research and case study applications in education. Epub 2nd. [Google Scholar]
- 22.Nkoko L., Spiegel J., Rau A., Parent S., Yassi A. Reducing the risks to health care workers from blood and body fluid exposure in a small rural hospital in Thabo-Mofutsanyana, South Africa. Workplace Health Saf. 2014;62:382–388. doi: 10.3928/21650799-20140815-03. [DOI] [PubMed] [Google Scholar]
- 23.Verbeek J., Husman K., van Dijk F., Jauhiainen M., Pasternack I., Vainio H. Building an evidence base for occupational health interventions. Scand J Work Environ Health. 2004;30:164–170. [PubMed] [Google Scholar]
- 24.Hulshof C., Hoenen J. Evidence-based practice guidelines in OHS: are they agree-able? Industrial Health. 2007;45:26–31. doi: 10.2486/indhealth.45.26. PubMed PMID: 17284870. [DOI] [PubMed] [Google Scholar]
- 25.Valim M.D., Marziale M.H.P., Richart-Martínez M., Sanjuan-Quiles Á. Instruments for evaluating compliance with infection control practices and factors that affect it: an integrative review. J Clin Nurs. 2014;23:1502–1519. doi: 10.1111/jocn.12316. [DOI] [PubMed] [Google Scholar]
- 26.Singh A., Purohit B., Bhambal A., Saxena S., Singh A., Gupta A. Knowledge, attitudes, and practice regarding infection control measures among dental students in Central India. J Dental Educ. 2011;75:421–427. [PubMed] [Google Scholar]
- 27.Gammon J., Morgan-Samuel H., Gould D. A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. J Clin Nurs. 2008;17:157–167. doi: 10.1111/j.1365-2702.2006.01852.x. [DOI] [PubMed] [Google Scholar]
- 28.Amponsah-Tawaih K., Adu M.A. Work pressure and safety behaviors among health workers in Ghana: the moderating role of management commitment to safety. Saf Health Work. 2016;7:340–346. doi: 10.1016/j.shaw.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sitzmann T., Ely K., Brown K., Bauer K. Self-assessment of knowledge: a cognitive learning or affective measure? Acad Manage Learn Educ. 2010;9:169–191. [Google Scholar]
- 30.Engelbrecht M., Yassi A., Spiegel J., van Rensburg A., O’Hara L., Bryce E., Nophale L. Tuberculosis and blood-borne infectious diseases: Workplace conditions and practices of healthcare workers at three public hospitals in the Free State. South Afr J Epidemiol Infect Dis. 2015;30:23–28. [Google Scholar]
- 31.Siegel J., Yassi A., Rau A., Buxton J., Wouters E., Engelbrecht M., Uebel K.E., Nophale L.E. Workplace Interventions to Reduce HIV and TB Stigma among Healthcare Workers - where do we go from here? Global Public Health. 2015;13:1–13. doi: 10.1080/17441692.2015.1021365. [DOI] [PubMed] [Google Scholar]
- 32.Khan R., Yassi A., Engelbrecht M., Nophale L., van Rensburg A., Spiegel J. Barriers to HIV counselling and testing uptake by health workers in three public hospitals in Free State Province, South Africa. AIDS Care. 2014;30:1–8. doi: 10.1080/09540121.2014.951308. [DOI] [PubMed] [Google Scholar]
- 33.Yassi A., O'Hara L., Engelbrecht M., Uebel K., Nophale L., Bryce E. Considerations and dilemmas in preparing a randomized population health intervention trial: lessons from a South African–Canadian partnership to improve HIV and tuberculosis prevention and care for health workers. Global Health Action. 2014;7(1):23594. doi: 10.3402/gha.v7.23594. https://doi.org/10.3402/gha.v7.23594 [date accessed: 2016 Feb 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore D., Gamage B., Bryce E., Copes R., Yassi A., British Columbia Interdisciplinary Respiratory Protection StudyGroup Protecting health care workers from SARS and other respiratory pathogens: organizational and individual factors that affect adherence to infection control guidelines. Am J Infect Control. 2005;33:88–96. doi: 10.1016/j.ajic.2004.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pittet D. Infection control and quality health care in the new millennium. Am J Infect Control. 2005;33:258–267. doi: 10.1016/j.ajic.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 36.Baker P.A. From apartheid to neoliberalism: health equity in post-apartheid South Africa. Int J Health Serv. 2010;40:79–95. doi: 10.2190/HS.40.1.e. [DOI] [PubMed] [Google Scholar]
- 37.Coovadia H., Jewkes R., Barron P., Sanders D., McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374:817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 38.van Rensburg D. Van Schaik; 2004. Health and healthcare in South Africa.http://www.takealot.com/health-and-healthcare-in-south-africa/PLID35557641 Available from: [date accessed: 2017 Feb 21] [Google Scholar]
- 39.Jansen J., Herman C., Matenjie T., Morake R., Pillay V., Sehoole C., Weber E. Council on Higher Education; Pretoria: 2007. Tracing and explaining change in higher education: the South African case. Review of higher education in South Africa. [Google Scholar]
- 40.Marais H. Zed Books; South Africa: 2011. South Africa pushed to the limit: the political economy of change. [Google Scholar]