Abstract
Background
Fatigue and sleepiness are inter-related and common among road transport drivers. In this study, sleep deprivation and fatigue among chemical transportation drivers were examined.
Methods
A cross-sectional study surveying 107 drivers from three hazardous types of chemical production and transportation industries (nonflammable gases, flammable gases, and flammable liquids) was conducted. Data on sleep deprivation were collected using questionnaires of the Stanford Sleeping Scale and the Groningen Sleep Quality Scale. Fatigue was assessed using an interview questionnaire and a flicker fusion instrument.
Results
Chemical drivers had a mean sleeping scale (Stanford Sleeping Scale) of 1.98 (standard deviation 1.00) and had a mean score of 1.89 (standard deviation 2.06) on the Groningen Sleep Quality Scale. High-risk drivers had higher scores in both the Stanford Sleeping Scale and the Groningen Sleep Quality Scale with a mean score of 2.59 and 4.62, respectively, and those differences reached statistical significance (p < 0.05). The prevalence of fatigue, as assessed through a critical flicker fusion analyzer, subjective fatigue question, and either of the instruments, was 32.32%, 16.16%, and 43.43%, respectively. Drivers who slept <7 hours and had poor sleep quality were found to have more fatigue than those who slept enough and well. Drivers who had a more sleepiness score resulted in significantly more objective fatigue than those who had a less sleepiness score.
Conclusion
Sleep quality and sleeping hour can affect a driver's fatigue. Optimization of work–rest model should be considered to improve productivity, driver retention, and road safety.
Keywords: chemical transportation, drivers, fatigue, road safety, sleep deprivation
1. Introduction
In Thailand, road transport is the predominant form of chemical transportation, and causes the most severe safety and environmental health, social, and economic consequences [1]. Chonburi, the center of industrial enterprises, tourism, and logistics, connects to other provinces including Bangkok through an eight-lane motorway. Statistically, 20% of road accidents occurred on main roads and motorways [1]. Owing to heavy traffic, driving a vehicle carrying chemicals has become increasingly difficult, especially in the metropolitan and suburban areas of Chonburi. The public has become more aware of and concerned about the dangers involved in the road transportation of hazardous chemicals.
Fatigue and sleepiness are inter-related and common among the population of truck drivers. Despite their different implications in terms of diagnosis and treatment, these two terms are often used interchangeably, or merged under the general term “tired, sleepy, or exhausted” [2], [3]. In many countries including Thailand, fatigue is not fully defined as an offence under traffic law and hence remains a form of driver's behavior that cannot be effectively targeted. The effects of fatigue can vary but are best viewed as a continuum, ranging from mild, infrequent complaints to severe, disabling manifestations including burnout, overstrain, or chronic fatigue syndrome [4]. Fatigue is a construct that links factors such as time of day, time since waking, task duration, and monotony, with safety-related outcomes [5]. It causes significant effects in different countries. For instance, fatigue caused 15%, 20%, and 40% of accidents in China, UK, and North America, respectively [6], [7]. In the United States, fatigue driving causes >1,500 deaths every year [8]. Late-sleeping drivers are involved in motor vehicle accidents more frequently, which may be related to personality traits [9]. Other factors involved in driver fatigue and road accidents included age, body mass index (BMI), work experience, smoking, alcohol, and vision [10], [11]. These factors have been identified as major causes of road accidents due to reduced driving performance, increasing the risk of accidents [12], [13], [14]. A number of studies had been conducted on fatigue driving [12], [15], [16], [17], [18], [19], but not on chemical transportation in particular. Thailand is among the top five countries with the worst road safety record in the world [20]. In view of road safety, we were interested in the assessment of sleep deprivation and fatigue among drivers working in the chemical production and transportation industries. The results of this study are important for the development of safety and health surveillance and promotion policies and programs, as well as evaluation of measures to be taken to improve hazardous chemical transportation on the road.
2. Materials and methods
2.1. Sampling sites
This cross-sectional study was performed during January 2015 and April 2015 in three types of chemical industries that had accidents frequently, including the transportation of gas and flammable liquid [21]. Selection criteria of sampling location were based on industry location, type of industry, and other factors including the consent of plant manager and workers to conduct the research. All study sites located in Chonburi were prioritized to be high-risk chemical industries according to the attachment in the notification of Ministry of Industry (No. 3/2542) under Hazard Substances Act B.E. 2535. These factories are briefly introduced below.
Factory #1
This is a painting factory located in an industrial estate. It is of moderate size and employs 51 drivers. Most vehicles used for chemical transportation are four- and six-wheel vehicles. Transportation of hazardous chemical products is under the operation of a contractor. Less than 10% of the vehicles have the Global Positioning System installed. Driving times are between 5:00 am and 8:00 pm.
Factory #2
This factory manufactures industrial gas (nonflammable and nontoxic gas, i.e., oxygen, nitrogen, and argon) and is located in an industrial estate. It is a small plant that employs just 24 drivers. Vehicles used for gas transportation are 10-wheel trucks, all of which have the Global Positioning System installed. Drivers work in three shifts: 6:00 am–2:00 pm, 9:00 am–5:00 pm, and 2:00 pm–10:00 pm.
Factory #3
This factory manufactures flammable gas (liquefied petroleum gas) and is located outside the industrial estate. It is a small industry employing 32 drivers. Vehicles used for flammable gas transportation are trucks and trailers. All vehicles have the Global Positioning System installed. Drivers work in two shifts: 4:00 am–12:00 pm and 12:00 pm–8:00 pm.
2.2. Participants
A total of 107 drivers participated in this study. All participants were day-shift chemical drivers, who started work in the morning (5:00–9:00 am) and stopped the routine in the evening (4:00–8:00 pm). Inclusion criteria were having experience for driving vehicles in industries mentioned above for at least 4 months and willingness to give written informed consent. Participants who could not participate in all activities were excluded from the study. This research was approved by the Ethics Review Committees for Research on Human Subjects of Burapha University.
2.3. Study design and tools
The general questionnaire comprised three parts: demographic factors (age and BMI), work history (working experience, and driving distances and hours), and health status (vision, tobacco and alcohol consumption, and use of somnolent medication). The questionnaire was sent to three experts to verify its structural and content validity. Consistency was examined using Cronbach α coefficient, which was calculated to be 0.788. Drivers also were assessed for fatigue and sleep deprivation using quantitative and qualitative scales.
2.4. Measurement of fatigue
All drivers were assessed for both objective and subjective fatigue using the flicker fusion instrument and Piper scale, respectively. The objective fatigue was assessed by the flicker fusion instrument model 12021A. Measurements of the critical flicker frequency (CFF) threshold were done by intrafoveal stimulation with a luminous diode. It was measured in a quiet and semidark room. When the eyes were not fatigued, they would be perceived to wink well at a high frequency, and thus the CFF value would be high. The results of testing showed decreased values when visual fatigue occurred. CFFs were measured before (5:00–9:00 am) and after driving (4:00–8:00 pm) three times for each individual, after which the mean value was calculated. The unit of CFF was cycle per second or hertz. It was considered to have fatigue symptom when (CFFafter – CFFbefore) > 1 standard deviation (SD) of individual CFFbefore.
The subjective fatigue was also assessed using the Piper fatigue scale [22], which is a 22-item scale that measures four subscales: behavior (6 items), affective (5 items), sensory (5 items), and cognition/mood (6 items). Each item had 11 response categories on a 0–10 metric, with verbal descriptors anchoring the end points. Each subscale was scored individually and then aggregated together for an overall score, with higher scores reflecting more fatigue. The subjective fatigue was classified into three categories on a response scale (0–3 = mild; 4–6 = moderate; 7–10 = severe fatigue).
2.5. Assessment of sleep deprivation
Each participant was asked to complete two questionnaires of the Stanford Sleeping Scale (SSS) and the Groningen Sleep Quality Scale (GSQS) before driving. The SSS [23], a measure of self-reported feeling of the immediate state of sleepiness on a seven-point scale, ranging from “alert” (1) to “almost asleep” (7), was administered. The test scores of drivers who graded their feeling as equivalent to a score of ≥3 were defined as “high-risk” scores.
The instrument for measuring subjective sleep quality was the GSQS, which is widely used [19], [24], [25]. The scale rates from 0 to 14, with a higher score indicating disturbed sleep. Originally, this scale was created for studying the sleep problem in depressed inpatients. In a validation study of 80 patients with depression, the mean score was 6.0 (SD = 4.2) and Cronbach α for internal consistency was 0.88 [26]. This validated scale consists of 14 questions relating to sleep quality, to be answered with yes or no. Generally, under normal conditions of an unrestricted and undisturbed night's sleep, participants scored between 0 and 2. Test scores of participants who scored their sleep quality as ≥3 were defined as “high-risk” scores.
2.6. Statistical analysis
Statistical analyses were performed using SPSS, version 17.0 (IBM Singapore Pte Ltd, Singapore). The general data were analyzed by descriptive statistics. The difference between high- and low-risk test scores with quantitative variables (sleepiness, sleep quality, and average sleep time) was analyzed by independent t test. Qualitative variables (alcohol drinking, vision impairment, accidental history, and fatigue) were analyzed by z test of proportion difference between high- and low-risk test groups with two-tailed testing. The p level of significance was 0.05.
3. Results
3.1. General characteristics of participants
A total of 99 of 107 drivers (92.52%) in the three chemical industries were examined. The other eight drivers were excluded due to being new employees or not completing the flicker fusion testing after their work. Majority of the drivers (63.6%) used 10-wheel trucks. All drivers were men with a mean age of 38.2 years (range, 21–64 years). Nearly one-third of the sample (62.6%) was overweight, as indicated by their BMI. They had an average of 5.37 years of working experience (range, 0.3–32 years). The mean numbers of driving hours and driving distances were 6.13 hours and 156.45 km/d, respectively. Approximately 30% of workers slept <7 hours/night on average, and up to 54.5% of them had been involved in road traffic accidents. Approximately half of the drivers (53.5%) had good vision, while 27 (27.3%) had impaired vision. Characteristics of the drivers are shown in Table 1.
Table 1.
Demographic factors of chemical transportation drivers (N = 99)
| Variables | Mean (SD) |
|---|---|
| Age (y) | 38.20 (7.91) |
| BMI (kg/m2) | 25.63 (5.02) |
| Working experience (y) Driving distance (km/d) |
5.37 (6.47) |
| 156.45 (110.83) | |
| Driving (h/d) Sleep (h/d) |
7.34 (1.75) 6.13 (2.23) |
| n (%) | |
| Smoking | |
| Yes | 43 (43.40) |
| No | 56 (56.60) |
| Accident history 1 y past (time) | |
| Yes | 54 (54.50) |
| No | 45 (45.50) |
| Vision | |
| Normal | 53 (53.50) |
| Abnormal | 27 (27.30) |
| Unknown | 19 (19.20) |
BMI, body mass index; SD, standard deviation.
3.2. Assessment of sleepiness and fatigue
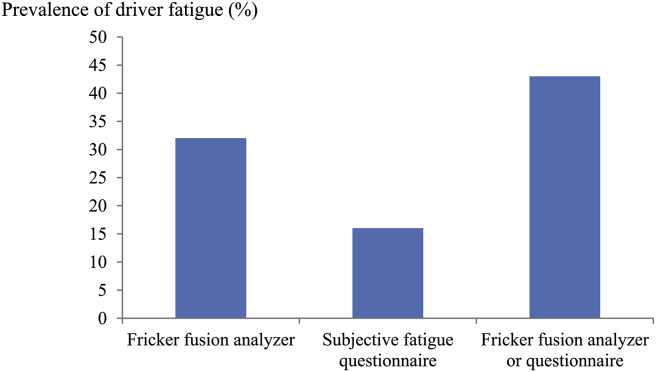
The results revealed that the prevalence of fatigue as assessed through the critical flicker fusion analyzer, subjective fatigue question, and either of the instruments were 32.32%, 16.16%, and 43.43%, respectively (Fig. 1). The mean value of objective fatigue before driving (CFFbefore) was 39.12 Hz (SD = 3.20, range, 29.33–48.03) and that after driving (CFFafter) was 37.76 Hz (SD: 4.29, range, 23.23–44.30), whereas the mean value of subjective fatigue was 3.13 (SD: 0.99, range, 1.09–6.45).
Fig. 1.
Prevalence of fatigue from flicker fusion test and questionnaire.
Of the 39 examination sets that were labeled “high risk”, on 13 occasions drivers slept <7 hours the night before the test, with an average sleep time of 6.7 hours. The results of the SSS and GSQS of the high- and low-risk groups of chemical transportation drivers are presented in Table 2. The high-risk group had higher scores in both scales; the difference between the groups reached statistical significance. Findings show that drivers had a mean score of 1.89 (SD: 2.06, range, 0–11) on the GSQS and had a mean sleeping scale (SSS) score of 1.98 (SD: 1.00, range, 1–6). High-risk drivers had a higher level of objective and subjective fatigue than those in the low-risk group, but not statistically significant.
Table 2.
Comparison between high and low risk test score of chemical transportation drivers
| Variables | Test score∗ |
p-value | |
|---|---|---|---|
| High risk | Low risk | ||
| Slept <7 h | 13/39 (33.30%) | 17/60 (28.30%) | 0.597 |
| Average sleep time (h) | 6.7 ± 1.65 7 (3–9) |
7.56 ± 1.75 7.4 (3–13) |
0.031† |
| Sleepiness score | 2.59 ± 1.21 3 (1–6) |
1.75 ± 0.80 2 (1–4) |
<0.001† |
| Sleep Quality Scale | 4.62 ± 1.88 4 (3–11) |
0.87 ± 0.82 1 (0–2) |
<0.001† |
| Consumed alcohol or somnolent medication | 3/39 (7.69%) | 0/60 (0%) | — |
| Objective fatigue (CFFbefore–CFFafter) | 13/32 (40.63%) | 19/56 (33.93%) | 0.530 |
| Subjective fatigue | 7/39 (17.95%) | 9/60 (15%) | 0.697 |
| Visual impairment | 12/39 (30.77%) | 15/60 (25%) | 0.529 |
| Accident history | 20/39 (51.20%) | 34/60 (56.67%) | 0.599 |
CFFbefore–CFFafter, difference in flicker frequency value before and after driving; GSQS, Groningen Sleep Quality Scale; SSS, Stanford Sleeping Scale.
Test scores of SSS and GSQS equivalent to ≥3 were defined as a high-risk group.
Significant difference between high- and low-risk test scores at p < 0.05 with two-tailed testing.
Three drivers in the high-risk score group admitted to using alcohol or somnolent pills. None of the low-risk drivers reported consumption of any medications or chemical substances. Regarding accident history, 20 high-risk drivers (including those having an accident at least once) were involved in 50 accidents, and 34 low-risk drivers were involved in 46 accidents.
The relationship between sleeping patterns and fatigue is shown in Table 3. Drivers sleeping <7 hours and reporting poor sleep quality had more fatigue than those who slept enough and well. About alertness test, drivers who had a higher score on the sleepiness scale were also measured to have a significantly higher level of objective fatigue than those who had a lower sleepiness score.
Table 3.
Relationship between sleeping and fatigue
| Driver fatigue |
||
|---|---|---|
| Critical flicker fusion (CFFbef–aft) | Questionnaire | |
| Sleep hour | ||
| <7 | –3.59 ± 2.44 (–9.03 to 0.00) |
3.25 ± 0.99 (2.00–5.99) |
| ≥7 | –2.90 ± 3.39 (–15.85 to 2.53) |
3.08 ± 1.00 (1.09–6.45) |
| Sleepiness score | ||
| ≤2 | –2.97 ± 3.17 (–15.83 to 1.53) |
3.00 ± 1.03 (1.09–6.45) |
| >2 | –3.44 ± 3.22∗ (–13.20 to 2.53) |
3.53 ± 0.79 (2.14–5.32) |
| Sleep Quality Scale | ||
| ≤2 | –3.36 ± 3.39 (–15.83 to 1.53) |
3.03 ± 1.02 (1.09–6.45) |
| >2 | –2.16 ± 2.08 (–6.17 to 2.53) |
3.35 ± 0.93 (1.59–5.23) |
Values are expressed as mean ± SD, min–max.
CFFbef–aft, difference in flicker frequency value before and after driving; min, minimum; max, maximum; SD, standard deviation.
Significant difference from a sleep quality score of ≤2 (control) at p < 0.05 with two-tailed testing.
4. Discussion
Sleep deprivation affects the prefrontal cortex of the cerebrum, the area of the brain responsible for most decisions and judgments, and significantly reduces executive function and reaction time [27], [28]. The mean score of GSQS and SSS in the participants was 1.89 and 1.98, respectively, both not indicating sleep debt and impaired sleep quality. However, about 30% of drivers slept <7 hours and had a score of >2.0 on the GSQS. Individuals with fatigue and sleep disorders seem vulnerable to additional negative consequences due to a possible interplay between amplified fatigue and psychological distress [29]. People who wake frequently and have unpleasant dreams do not feel refreshed in the morning. With increasing duration of wakefulness, the propensity for sleep increases and alertness becomes impaired. Another study showed that individuals who had been awake for 18.5 hours, 21 hours, and 24 hours of wakefulness produced performance decrements equivalent to those observed at blood alcohol concentrations of 0.05%, 0.08%, and 0.10%, respectively [13], [30]. A comparison of how long drivers had slept before an accident and the time of the accident showed that they had slept less than usual. In addition, when they sleep significantly less than usual, the risk of a critical event increases. This suggested that fatigue could play a major role [31].
In terms of methodology for conducting research on fatigue, subjective measures of sleepiness are important because objective measurements (such as electrocardiogram, electroencephalogram, etc.) are not feasible to implement in most population research [32]. The GSQS is a short and simple, self-administered, and detailed questionnaire survey that is easy to score and enables the examination of drivers. It has been confirmed to be valid and reliable [24], [33]. Such a subjective screening tool can also be important if it could be applied to identify drivers who are too sleepy to drive or who are incapable of driving due to drug or alcohol use. A range of approaches can be used to enhance alertness including screening and short naps during day time. Ocular parameters can be served as fatigue screening of truck drivers [19]. Evidence-based management strategies require consideration of the work–rest model optimization.
Testing of CFF value is a simple, affordable test, which is easy to perform, although there are some limitations [34]. CFF threshold is known to be affected by several factors including target luminance, target color, and target size [35]. However, this study has been done in a quiet and semidark room, and the result showed a higher prevalence of driver fatigue than the results from subjective fatigue questionnaire. A previous study disclosed that subjective fatigue did not reflect the objective physiological status of the tired person because of a bias in motivation and personal factors such as experience, training, etc. [36]. However, in the review of long workdays and health, van der Hulst [37] summarized that subjective, rather than objective, measures are more commonly linked to fatigue. In contrast, this study revealed that there was an agreement of testing assessed through flicker fusion instrument and subjective fatigue questionnaire at 59.1%.
Other factors including age, BMI, work experience, smoking, alcohol, and vision were involved in sleepiness related to fatigue and road accidents [2], [11], [12]. This study found that six drivers had age >50 years, 62 drivers were overweight (BMI ≥ 23), and 20 drivers worked >8 hours/d and drove >200 km/d. These were more frequently involved in sleepiness-related road accidents, especially at night. Nightshift workers, compared with dayshift workers, are likely to be at a greater risk of sleepiness [13], [38]. Smoking is not good behavior for safety, especially in chemical transportation drivers. Our results showed that 43 out of 99 were smokers and 16% of them smoked while driving. Alcohol levels in the blood of chemical transportation drivers were measured randomly by safety personnel in all three study locations. A half of the drivers always took energy drink to control fatigue while on duty (data not shown). Periodic eye examinations should be carried out for all commercial drivers before issuing or renewing licenses to drive. Although eye examinations were carried out in the three study sites every year, 19 drivers (19.2%) did not participate in this activity since they were on the road at the time of the eye test event. Our results also showed that visual impairment, fatigue, and accident history between persons with sleep deprivation (high-risk test score group) and low-risk test score group were not significantly different. Pepple and Adio [11] also found that visual impairment was not significantly associated with the occurrence of road traffic accidents.
There are some limitations of the study, including its small sample size and no data on the night shift chemical drivers. In terms of public health implications of the study, it is recommended that more effort is invested in raising public awareness about the dangers of fatigued driving, and on educating drivers about how to recognize and deal with fatigue and sleepiness when these occur. More studies about the work–rest model, evaluation, and management are needed. These will lead to a set of safety measures and ultimately result in improved productivity, driver retention, and road safety. Nonetheless, more studies on drivers involved in hazardous chemical transportation (i.e., crane, forklift, reach stacker, and sideloader) should be conducted for more accurate generalization of the results.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgments
This research was funded by the National Research Council of Thailand (103318). The authors would like to thank Mr Jedsadanon Ratanaumpornkoon for coordinating the study sites. We also thank the individuals who participated in the study and acknowledge the contributions of the field team.
References
- 1.Department of Land Transport, Ministry of Transport (MOT). Traffic statistics [Internet]. 2015 [cited 2015 Sept 10]. Available from: http://www.mot.go.th/statmot.html.
- 2.Jamroz K., Smolarek L. Driver fatigue and road safety on Poland’s national roads. Int J Occup Saf Ergon. 2013;19(2):297–309. doi: 10.1080/10803548.2013.11076987. [DOI] [PubMed] [Google Scholar]
- 3.Workplace Safety and Health Guidelines. Fatigue management [Internet]. 2010 [cited 2016 Dec 31]. Available from: https://www.wshc.sg/files/wshc/upload/cms/file/2014/Fatigue Management.pdf.
- 4.Shen J., Barbera J., Shapiro C.M. Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev. 2006;10:63–76. doi: 10.1016/j.smrv.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Mohren D., Jansen N., van Amelsvoort L., Kant I.J. Wilco Publishers; Amersfoort: 2007. An epidemiological approach of fatigue and work. Experiences from the Maastricht Cohort Study. [Google Scholar]
- 6.Williamson A., Lombardi D., Folkard S., Stutts J., Courtney T., Connor J. The links between fatigue, safety and performance. Accid Anal Prev. 2011;43:498–515. doi: 10.1016/j.aap.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher A., McCulloch K., Baulk S.D., Dawson D. Countermeasures to driver fatigue: a review of public awareness campaigns and legal approaches. Aust NZ J Public Health. 2005;29(5):471–476. doi: 10.1111/j.1467-842x.2005.tb00229.x. [DOI] [PubMed] [Google Scholar]
- 8.Dan M., Hongting L., Wenshu L. A review study of driving fatigue detection methods based on physiological signal. Chin J Ergon. 2012;18(1):67–69. [Google Scholar]
- 9.Drobnich D.A. A National Sleep Foundation’s conference summary: the National Summit to prevent drowsy driving and a new call to action. Ind Health. 2005;43:197–200. doi: 10.2486/indhealth.43.197. [DOI] [PubMed] [Google Scholar]
- 10.Schwebel D.C., Severson J., Ball K.K., Rizzo M. Individual difference factors in risky driving: the roles of anger/hostility, conscientiousness, and sensation-seeking. Accid Anal Prev. 2006;38(4):801–810. doi: 10.1016/j.aap.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Pepple G., Adio A. Visual function of drivers and its relationship to road traffic accidents in Urban Africa. Springerplus. 2014;3:47–53. doi: 10.1186/2193-1801-3-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duke J., Guest M., Boggess M. Age-related safety in professional heavy vehicle drivers: a literature review. Accid Anal Prev. 2010;42:364–371. doi: 10.1016/j.aap.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 13.Rajaratnam S.M.W., Howard M.E., Grunstein R.R. Sleep loss and circadian disruption in shift work: health burden and management. Med J Aust. 2013;199(8):S11–S15. doi: 10.5694/mja13.10561. [DOI] [PubMed] [Google Scholar]
- 14.Sze S.K., Tamrin S.B.M., Goh Y.M. Driving fatigue and performance among occupational drivers in simulated prolonged driving. Global J Health Sci. 2010;2(1):167–177. [Google Scholar]
- 15.Boonpa P., Lormpong M., Pusapukdeepob J. Factors related to fatigue among bus drivers in zone of Bangkok Mass Transit Authority, Bangkok. Public Health J Burapha Univ. 2013;8(2):46–58. [Google Scholar]
- 16.Milia L.D., Smolensky M.H., Costa G., Howarth H.D., Ohayon M.M., Philip P. Demographic factors, fatigue and driving accidents: an examination of the published literature. Accid Anal Prev. 2011;43(2):516–532. doi: 10.1016/j.aap.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 17.Singh H, Bhatia JS, Kaur J. Eye tracking based driver fatigue monitoring and warning system. India International Conference on Power Electronics, IICPE 2010, January 28, 2011–January 30, IEEE Computer Society, New Delhi, India.
- 18.Smolensky M.D., Milia L., Ohyayon M., Philip P. Demographic factors and fatigue: chronic medical conditions and sleep disorders. Accid Anal Prev. 2011;43:516–532. doi: 10.1016/j.aap.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 19.Morad Y., Barkana Y., Zadok D., Hartstein M., Pras E., Bar-Dayan Y. Ocular parameters as an objective tool for the assessment of truck. Accid Anal Prev. 2009;41:856–860. doi: 10.1016/j.aap.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 20.Fox News Travel. Top 10 countries with deadliest roads for travelers [Internet]. 2016 [cited 2016 Apr 10]. Available from: http://www.foxnews.com/travel/2014/02/21/top-10-deadliest-countries-for-drivers.html.
- 21.Center of Excellence on Hazardous Substance Management, Chulalongkorn University. Knowledge platform on chemical safety [Internet]. 2006 [cited 2015 Dec 25]. Available from: http://www.chemtrack.org/BoardFile/F3-4-1.pdf.
- 22.Piper B.F., Dibble S.L., Dodd M.J., Weiss M.C., Slaughter R.E. The revise Piper fatigue scale: psychometric evaluation in women with breast cancer. Oncol Nurs Forum. 1998;25:677–684. [PubMed] [Google Scholar]
- 23.Hoddes E., Zarcone V., Smythe H., Phillips R., Dement W.C. Quantification of sleepiness: a new approach. Psychophysiology. 1973;10(4):431–436. doi: 10.1111/j.1469-8986.1973.tb00801.x. [DOI] [PubMed] [Google Scholar]
- 24.Mulder-Hajonides van der Meulen W.R.E.H., Wijnberg J.R., Hollanders J.J., DeDiana I., Hoofdakker R. Measurement of subjective sleep quality. Eur Sleep Res Soc Abstracts. 1980;5:98. [Google Scholar]
- 25.Jafarian S., Gorouhi F., Taghva A., Lotfi J. High altitude sleep disturbance: results of the Groningen Sleep Quality Questionnaire survey. Sleep Med. 2008;994:446–449. doi: 10.1016/j.sleep.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 26.Williams T.M., Aderanti R.A. Sleep as a determinant of academic performance of university students in Ogun state, South west, Nigeria. Eur Sci J. 2014;10(13):657–664. [Google Scholar]
- 27.Killgore W.D.S., Balkin T.J., Wesensten N.J. Impaired decision-making following 49 hours of sleep deprivation. J Sleep Res. 2006;15:7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- 28.Crowley S., Acebo C., Carskadon M.A. Circadian rhythms and circadian rhythm disorders in adolescents. Sleep Med Rev. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 29.Hossain J.L., Ahmad P., Reinish L.W., Kayumov L., Hossain N.K., Shapiro C.M. Subjective fatigue and subjective sleepiness: two independent consequences of sleep disorders? J Sleep Res. 2005;14(3):245–253. doi: 10.1111/j.1365-2869.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- 30.Arnedt J.T., Wilde G.J.S., Munt P.W., MacLean A.W. How do prolonged wakefulness and alcohol compare in the decrements they produce on a simulated driving task? Accid Anal Prev. 2001;33:337–344. doi: 10.1016/s0001-4575(00)00047-6. [DOI] [PubMed] [Google Scholar]
- 31.Hanowski R.J., Hickman J., Fumero M.C., Olson R.L., Dingus T.A. The sleep of commercial vehicle drivers under the 2003 hours-of-service regulations. Accid Anal Prev. 2007;39(6):1140–1145. doi: 10.1016/j.aap.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 32.Kim H., Young T. Subjective daytime sleepiness: dimensions and correlates in the general population. Sleep. 2005;28(5):625–634. doi: 10.1093/sleep/28.5.625. [DOI] [PubMed] [Google Scholar]
- 33.Weil J.V. Sleep at high altitude. High Alt Med Biol. 2004;5:180–189. doi: 10.1089/1527029041352162. [DOI] [PubMed] [Google Scholar]
- 34.Torlot F.J., McPhail M.J.W., Taylor-Robinson S.D. Meta-analysis: the diagnostic accuracy of critical flicker frequency in minimal hepatic encephalopathy. Aliment Pharmacol Ther. 2013;37(5):527–536. doi: 10.1111/apt.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shankar H., Pesudovs K. Critical flicker fusion test of potential vision. J Cataract Refract Surg. 2007;33:232–239. doi: 10.1016/j.jcrs.2006.10.042. [DOI] [PubMed] [Google Scholar]
- 36.Krueger G.P. June 2004. Technologies and methods for monitoring driver alertness and detecting driver fatigue: a review applicable to long haul truck driving: Technical report for American Transportation Research Institute and Federal Motor Carrier Safety Administration. [Google Scholar]
- 37.van der Hulst M. Long workdays and health. Scand J Work Environ Health. 2003;29:171–188. doi: 10.5271/sjweh.720. [DOI] [PubMed] [Google Scholar]
- 38.Akerstedt T. Shift work and sleep disturbance. Scientific symposium: the health effects of shift work. Toronto [Internet]. 2010 [cited 2015 Dec 18]. Available from: http://www.iwh.on.ca/system/files/documents/shift_work_2010_akerstedt_abstract.pdf 2010.