Abstract
Background
Patellofemoral pain is a prevalent disorder among female adolescents. Overuse is frequently cited as the etiology of pain for this population. What is currently unclear, however, is if the patella demonstrates abnormal tracking patterns relative to the femoral trochlear groove in adolescent females with patellofemoral pain.
Purpose
The aim of this case-control study is to determine if abnormal patellar tracking patterns are present in adolescent females with patellofemoral pain. The secondary aim is to identify if an increased distance between the tibial tuberosity and trochlear groove (TT_TG) is associated with the observed kinematic patterns.
Study Design
Case Control
Methods
Twenty female adolescent knees from 12 subjects with patellofemoral pain and 20 age-matched female knees from 13 healthy controls were recruited for this study. Patellofemoral kinematics (e.g., lateral patellar displacement) during a repetitive knee extension-flexion maneuver were quantified from dynamic cine-phase-contrast magnetic resonance imaging techniques. Static magnetic resonance images were used to determine the TT-TG distance.
Results
Relative to the control cohort, female adolescents with patellofemoral pain demonstrated significantly greater lateral displacement at 10° (3.2mm, p<0.001), 20° (2.3mm, p<0.001), and 30° (1.7mm, p=0.014) of knee flexion. A subgroup within this cohort (7 knees from 5 subjects) demonstrated extreme lateral maltracking >2 standard deviations beyond the average control. This subgroup also demonstrated a greater distance between the tibial tuberosity and trochlear grove relative to controls (Δ=4.2mm, p=0.001).
Conclusions
This study demonstrates that abnormal patellar tracking patterns are present in adolescent females with patellofemoral pain. Since all subjects from both cohorts participated in impact sports, it appears that rigorous athletic training alone is inadequate to produce symptoms in this population. Rather, patellofemoral pain may derive from a combination of physical activity in the context of pathologic kinematics.
Introduction
As one of the most common causes of joint pain encountered in sports medicine clinics, patellofemoral pain (PFP) reduces quality of life for thousands of individuals worldwide.1, 3, 11, 31 This is particularly true among adolescent females (10 – 19 years old), where PFP often prevents involvement in youth sports and other forms of physical activity.4, 30, 34, 42 Since an active lifestyle is required for maintaining physical health and many adolescents rely on sports for social acceptance and as a pathway to higher education, PFP may affect a child developmentally, emotionally, socially, economically, and physically. Further, persistent PFP was recently found to be the norm and not the exception in an adolescent cohort with PFP at two year follow-up; and evidence suggests that PFP in young patients may predispose them to long-term sequelae such as osteoarthritis.20, 25, 30, 44, 49 Thus, correctly understanding the potential factors leading to PFP in this population is becoming increasingly urgent.
Despite a reported prevalence of PFP among female adolescents (14.3% - 20.8%) that is approximately equal to or greater than the prevalence in female adults (15.3%), less than 5% of published studies in the field are devoted to the adolescent population.7, 32, 43, 45 This paucity of published data specific to PFP experienced by adolescents limits our understanding of the underlying pathology in these patients. In contrast to adults, for whom PFP is often assumed to be a kinematic problem, overuse is most often cited as the etiology of pain for adolescent patients.28, 44, 46, 47, 52 There are a plethora of analyses6, 9, 12, 24, 37, 50 on patellar tracking and alignment patterns in adults with PFP. Yet, an extensive search of the literature revealed no studies on patellar tracking and just two studies17, 33 on patellar alignment in adolescents with PFP. In addition, both of these analyses used static imaging techniques and included or focused exclusively on adolescents with PFP secondary to patellar dislocation. Two other studies,2, 10 also focused on adolescent cohorts with patellar instability, reported higher rates of dislocation in adolescent patients with increased distance between the tibial tuberosity and trochlear groove (TT-TG). Finally, studies19, 26, 27 have identified increased hip and knee abduction moments as risk factors for the development of PFP in adolescents. While the implied consequence of these abnormalities is altered patellofemoral tracking patterns and increased patellofemoral contact pressures, confirmation of these fundamental findings in adolescent females with PFP is currently lacking.
To alleviate this knowledge gap, this study sets out to determine if abnormal patellar tracking patterns are associated with PFP in adolescents by comparing patellofemoral joint kinematics in a cohort comprised exclusively of female pubescent subjects (12 – 15 years old) with PFP to age-matched female controls. The null hypothesis is that subjects with PFP and healthy controls demonstrate similar patellofemoral kinematics during dynamic knee extension. To further explore this novel subject matter, two additional areas of study are investigated: 1) the potential contribution of TT-TG to the patellofemoral kinematics in adolescents with PFP; and 2) the potential presence of kinematic subgroups within the cohort of adolescents with PFP.36, 38
Methods
Subject Recruitment
Female patients with PFP between 12 and 15 years of age were referred to this IRB-approved study from local orthopaedic sports medicine clinics. For a knee to be included within the cohort with PFP, the knee had to have a clinical diagnosis of PFP that existed for at least six months prior to participation. A knee was excluded from this cohort if it had a prior patellar dislocation; traumatic onset of PFP; ligament, meniscus, iliotibial band, cartilage, or other lower extremity injury; prior knee surgery. Asymptomatic females, age-matched (within six months), with no prior history of PFP or lower leg pathology/injury (for both legs) were recruited from the greater Washington, DC region via advertisement for the control cohort. A subject was excluded from the either cohort if they had contraindications to magnetic resonance (MR) imaging, were premenarchal, had a Beighton score41 of ≥ 5 or clinically diagnosed hypermobility syndrome (e.g., Ehlers-Danlos syndrome).
In total, 12 patients with PFP (20 knees) and 13 controls (20 knees) were enrolled in this study (Table 1). If both knees, from either cohort, fit the study criteria and time permitted, both knees were scanned. Prior to data collection, subjects provided signed assent (with a legal guardian or parent providing signed consent); verified past medical history; and underwent a physical exam with a focused evaluation of the knee. Patellofemoral pain levels were assessed using a visual analog scale (VAS) and anterior knee pain (AKP) scale, also known as a Kujala Score (Table 2).22, 29
Table 1.
Characteristics of participants. Where appropriate, the average value is given with one standard deviation in parentheses.
| Characteristic | PFP | Controls | p-value |
|---|---|---|---|
| Number of knees | 20 | 20 | NA |
| Number of subjects | 12 | 13 | NA |
| Age range (years) | 12.2 – 15.7 | 12.4 – 15.9 | NA |
| Mean age (years) | 14.1 (1.1) | 14.2 (1.0) | 0.88 |
| Weight (kg) | 51.1 (7.4) | 53.4 (9.6) | 0.40 |
| Height (cm) | 160.0 (5.2) | 156.9 (7.6) | 0.68 |
| BMI (kg/m2) | 20.4 (3.1) | 21.6 (3.1) | 0.23 |
| Age at menarche (years) | 11.9 (1.4) | 12.6 (0.5) | 0.06 |
| Hours/week in impact physical activities* | 7.75 (6.8) | 5.4 (4.4) | 0.21 |
| Hours/week in non-impact physical activities† | 4.4 (4.5) | 3.3 (6.0) | 0.20 |
Activities that required the lower extremities to repeatedly absorb a ground reactive force that exceeded body weight (e.g., running, soccer, basketball, field hockey, volleyball, and gymnastics)
Activities that required the lowered extremities to repeatedly absorb a ground reactive force less than body weight (e.g., swimming, biking, elliptical training)
Table 2.
Subjective measures of PFP severity in PFP subjects and controls. The average value is listed with one standard deviation in parentheses.
| Measure | PFP | Controls |
|---|---|---|
| Knee pain score (out of 100)†† | 61.1 (16.5) | 100 (0) |
| Visual analog score, pain on an average day (out of 10) ‡ | 3.5 (2.6) | 0 (0) |
| Visual analog score, pain at the end of the day (out of 10) ‡ | 4.7 (3.2) | 0 (0) |
| Visual analog score, pain during provocative activities (out of 10) ‡ | 7.0 (2.6) | 0 (0) |
Lower scores correspond to increased severity of PFP and decreased functionality
Higher scores correspond to increased severity of PFP
MR imaging
As described elsewhere,35 patellofemoral dynamic tracking patterns were quantified for all subjects using cine-phase contrast (CPC) MR imaging in a 3-Tesla MR scanner (Philips Electronics, Eindhoven, The Netherlands). This technique captures three-dimensional patellofemoral and tibiofemoral joint kinematics to an accuracy of <0.3mm.5 Subjects were situated supine in the MR scanner with the knee flexed and supported by a cushioned block (Figure 1). A custom-built coil holder supported a pair of large flex-coils medial and lateral to the knee and a pair of medium flex-coils directly anterior to the patella. These coils enhanced image quality, whereas the coil holder, with its rigid fixation to the MR plinth, provided medial-lateral stabilization of the knee during extension-flexion.
Figure 1.
Patient positioning in the MR scanner for image acquisition.
For dynamic MR data capture, subjects extended their knee, touching the top of the inner MR bore with their toe, and then flexed their knee until their heel made contact with a small cushion that rested on the MR plinth during each series at 30 cycles/minute. Repeatability of the motion was optimized by an auditory metronome (2 beats per cycle, indicating the end ranges of motion) and by providing medial-lateral stabilization of the knee within the coil holder. Each CPC acquisition required the patient to sustain this exercise for approximately 1.5 minutes with a typical cycle ranging from 5° - 45° of flexion. Dynamic CPC MR images (x, y, z velocity and anatomic image frames) were obtained in a single sagittal scan plane (TR = 5.1msec, TE = 2.8msec, spatial resolution = 0.7×0.7×8mm, flip angle = 12°, temporal resolution = 85.6msec) during knee motion. In a similar manner, dynamic, cine, anatomic, MR images in four axial planes were obtained to construct an anatomical coordinate system (Figure 2B&C).35 The knee angle was calculated using the anterior border of the proximal tibia and the long axis of the distal femur (Figure 2A). This method tends to overestimate the knee angle, as compared to the clinical knee angle (measured using the hip, knee, and ankle centers). Thus, a 10° knee angle, measured in the MR images, corresponds to a 0° clinical knee angle.14
Figure 2.
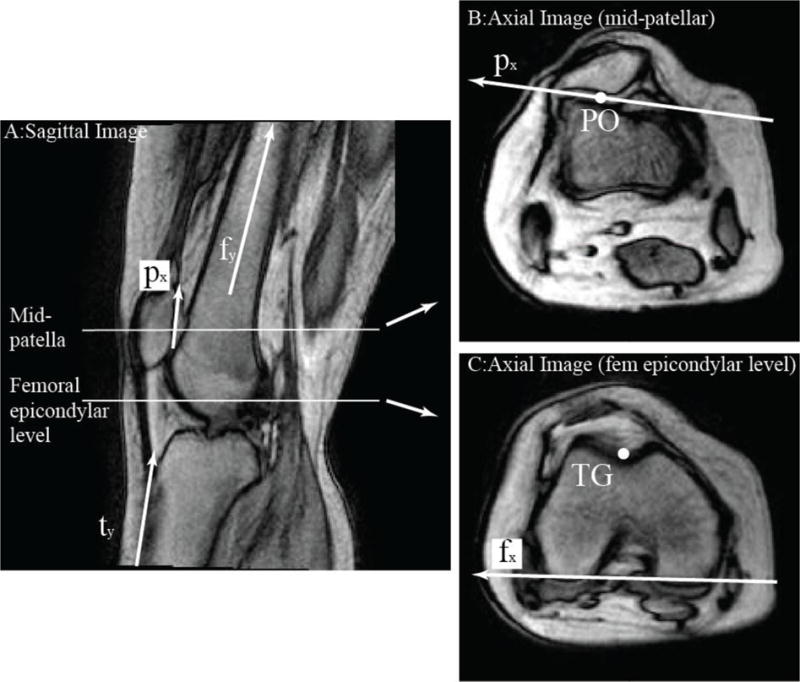
A: Sagittal CPC MR image, representing maximum knee extension (6°) for this subject. The knee angle was defined by the angle between the long axis of the femur (fy) and the anterior border of the tibia (ty). Based on this sagittal image, the dynamic cine axial image planes were selected. B: The mid-patellar axial image was defined by bisecting the posterior edge of the patella (py). The patellar origin (PO) was defined as the most posterior point of the posterior patellar ridge. The vector perpendicular to the lateral patellar facet was defined as the patellar medial-lateral direction) (px). C: The axial femoral image was defined at the level of the mid-femoral epicondyles. The femoral origin (trochlear groove, TG) was defined as the deepest point in the femoral groove. The femoral medial-lateral direction (fx) was defined tangent to the posterior femoral condyles. The subject-specific coordinate system was creating using px, py, fx, and fy, as described previously.35 Note, the distance from TG to PO defined the displacement of the patella. Patellar tilt is a three-dimensional angle, but can be approximated by the angle between px and fx.35
After the dynamic imaging, three-dimensional gradient recalled echo (GRE), GRE with fat-saturation, and proton density weighted (PDW) static images in all three cardinal planes were acquired with the lower limb in an anatomically neutral position and the knee within an 8-channel knee coil. A radiologist read all images to rule out undiagnosed knee disorders. Static axial PDW images (spatial resolution = 0.27 ×0.27×1.0mm, 512×512pixels) at full extension were used to measure the TT-TG distance for all subjects using the current gold standard methodology.8
Patellar displacements and rotations were measured relative to the femur using the coordinate system constructed for each bone (Figure 2). Three-dimensional velocity data enabled accurate tracking of bone throughout the movement cycle using integration, thus the construction of the coordinate system was only required for a single time frame. Medial, superior, and anterior were the positive displacement directions. Flexion, medial tilt, and varus were the positive rotation directions.39 Data were collected in even temporal increments (80msec), therefore all kinematic data were linearly interpolated to single knee angle increments for data averaging and statistical analysis.
Statistical Analysis
An a priori power analysis revealed that 19 knees were required to obtain an alpha of 0.05 and a beta of 0.2 for medial-lateral displacement at full extension. This was based on the following assumptions: a difference of >2.9mm in medial-lateral displacement would exist between cohorts; the control cohort and the cohort of individuals with PFP would demonstrate a standard deviation in this measure of ≤ 2.0mm and ≤ 4.5mm.37
Normality of all variables was determined using the Kolmogorov-Smirnov test. A two-tailed Student’s t-test provided the statistical comparison between cohorts for the normally distributed demographic factors (BMI, weight, age at menarche, hours per week engaged in impact physical activities). A Mann-Whitney U test provided the statistical comparison between cohorts for the non-normally distributed demographic factors (height and hours per week engaged in non-impact physical activities). Generalized estimating equations (SPSS, ver 22, IBM Corporation, Somers, NY), were used to assess main and interaction effects of cohort (PFPS and control) and knee angle (10°, 20°, and 30°) on the six normally distributed kinematic variables. The generalized estimating equations can be used to run an ANOVA (2×2) type analysis that first models the correlation between data derived from the same subject (e.g., kinematics data from the left and right knee) and then statistically compensates for these correlations.18 The post-hoc analyses were done within the generalized estimating equations framework. Generalized estimating equations also provided the statistical comparison for TT-TG across cohorts.
In line with a previous study,38 the PFP cohort was evaluated for the potential presence of distinct kinematic subgroups. If more than 85% of the individual PFP subjects demonstrated a lateral or medial maltracking pattern, then the potential for an extreme subgroup classification was explored. In such a case, a lateral or medial displacement greater than two standard deviations (SD) from the control average was designated an “extreme” case.
Results
The demographics were not significantly different between cohorts (Table 1). All subjects in both cohorts reported involvement in impact physical activities. Each subject with PFP reported values on the AKP and VAS consistent with PFP (Table 2). The kinematic data for all subjects were represented at 10°, 20°, and 30°, except for one control subject who only reached 12° in full extension. The kinematic data for this one subject was extrapolated to 10°, using a 2nd or 3rd order fit to the data (r2 ≥ 0.96).
Relative to the control cohort, the patellae in the cohort with PFP tracked laterally at all knee angles tested (p<0.001, Figure 3). The difference from the control average was 3.2mm (p<0.001), 2.3mm (p<0.001), and 1.7mm (p=0.014) at 10°, 20°, and 30°, respectively. Varus-valgus rotation was significantly different between cohorts (p=0.009). However, significant differences were not found at any single knee angle. Differences between cohorts were not found for superior-inferior displacement, anterior-posterior displacement, flexion-extension, or medial-lateral tilt. All kinematic variables, except for varus-valgus, significantly changed as the knee extended. Specifically, all knee angle pairs were significant different except the 20°-30° pair for medial-lateral displacement, anterior-posterior displacement, and medial-lateral tilt. There were no interaction effects.
Figure 3.
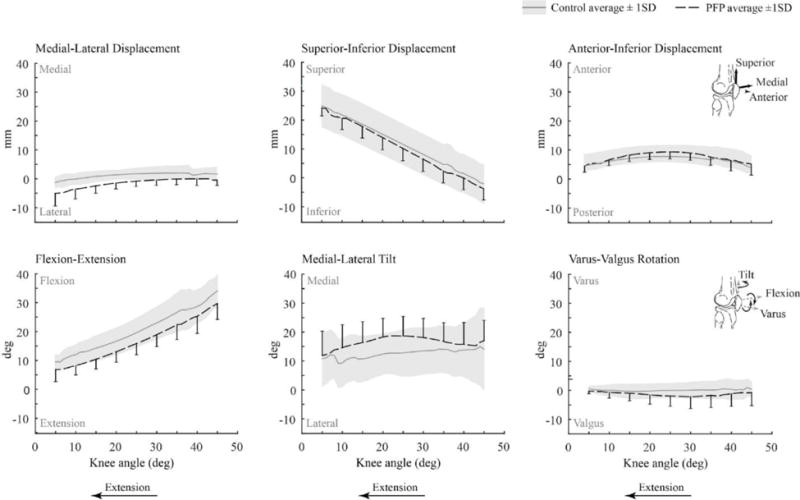
Average patellofemoral kinematics for healthy controls (grey) with ±1 SD shown in grey shading and PFP subjects (black) with ±1 SD shown every 5° of knee angle using bars. Kinematic data from all subjects are represented from 10° – 35°, whereas data from 22/40 (55%) and 20/40 (50%) of subjects are represented at 5° and 45°, respectively.
Within the adolescent PFP cohort, 19/20 (95%) of the knees were classified as lateral maltrackers, defined as lateral patellar displacement relative to the average of healthy controls.38 Of these, 7/19 (35% overall) of knees demonstrated extreme lateral maltracking, defined as >2SD of lateral displacement relative to the average of healthy controls (Figure 4). These 7 knees came from 5 subjects; 2 subjects had lateral maltracking bilaterally with only one knee being categorized as “extreme”. The average value of medial-lateral displacement for the extreme lateral maltracking subgroup was 7.0 ± 1.6mm and the highest value observed was 8.6mm.
Figure 4.
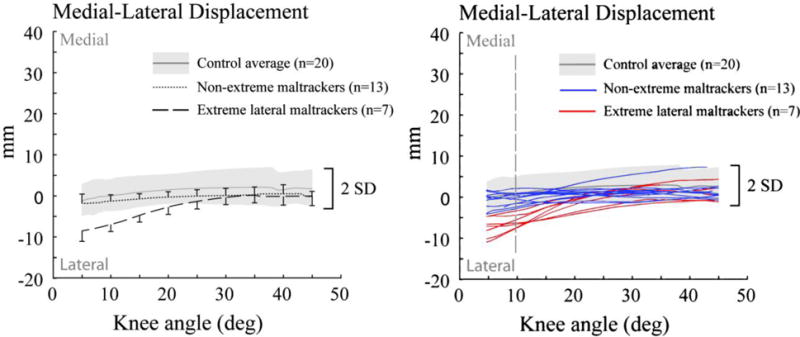
Average patellofemoral kinematics for healthy controls (grey) ± 2 SDs. Left: PFP subgroups with extreme (dashed) and non-extreme (dotted) lateral maltracking patterns. For both groups, 1 SD is provided every 5° of knee angle using bars. Right: The individual patellofemoral kinematics for subjects with PFP demonstrating extreme (red) and non-extreme (blue) lateral tracking patterns.
The cohort with PFP demonstrated greater TT-TG distances (12.2 ± 3.9mm) relative to the control cohort (10.0 ± 2.7mm, p=0.03). The extreme maltracking subgroup also demonstrated greater TT-TG distances (14.2 ± 3.5mm, p=0.001) relative to controls.
Discussion
As the first study to investigate dynamic, in vivo, patellar tracking patterns in adolescent females with PFP, this study demonstrates that abnormal kinematics are associated with PFP. The leading model for this association is that the altered kinematics change contact patterns, contact pressures, or both, which leads to pathological forces on the subchondral bone and ultimately pain.28 Since all subjects from both cohorts participated in impact sports, rigorous athletic training might not be adequate to produce PFP in the adolescent female. Rather, PFP may be due to a combination of physical activity in the context of pathologic kinematics. This directly translates into clinical practice in that the common prescription for adolescent females with PFP (activity reduction with the potential addition of physical therapy) may alleviate the overuse component of the disorder; however, it may fail to address the underlying kinematic pathology. This may explain why nearly two-thirds of adolescents with PFP report persistent symptoms at two-year follow-up.30 Further research is necessary to elucidate the most effective treatment for adolescent patients with PFP.
Despite many prior studies investigating the prevalence of PFP in adolescents, the patellar maltracking patterns associated with adolescent PFP is relatively unexplored in the literature. The work of Guzzanti and colleagues17 provides the closest parallel. This study used static CT imaging to compare patellofemoral alignment for a cohort of adolescent females with PFP against age- and sex-matched controls during isometric quadriceps muscles contraction. In contrast to the current results, this study found that at 30° of static knee flexion, lateral tilt was significantly greater in adolescents with PFP. The discrepancy between this and the current study result is partially explained by the fact that the previous study included patients with patellar instability and possibly joint hypermobility. In addition, Guzzanti and colleagues measured the patellar tilt angle in the axial slice at the mid-patellar level. Since patella alta was likely present in the cohort, the femoral reference line was likely taken at a more superior level, which would bias this group towards a larger lateral patellar tilt.40 The only other comparable study33 to evaluate adolescent females with patellofemoral pathology focused exclusively on patients with a history of recurrent patellar dislocations. This population exhibits severe patellar instability, and is not representative of the vast majority of PFP cases.31
The average lateral displacement (3.4mm) demonstrated in the cohort with PFP, as compared to controls, was equivalent to the difference seen in a previous study37 focused on adults with PFP. This was unexpected because the previous adult study included individuals with generalized joint laxity, which has been shown to cause more extreme maltracking problems, whereas the current study excluded individuals with generalized joint laxity. In addition, adults with PFP demonstrated significant abnormalities in multiple kinematic parameters whereas adolescents with PFP only demonstrated significant lateral displacement. Thus, for both adult and adolescent populations, altered kinematics may contribute to the etiology of PFP. However, this finding does not imply that the same underlying kinematic pathology is present in adults and adolescents. Future studies are needed to explore the potentially unique profiles of adolescent and adult kinematics for the development of age-specific interventions.
The unique pattern of isolated lateral displacement found in the present adolescent cohort can be explained by evaluating the kinematic pattern in the context of the functional anatomy of the patellofemoral joint. The femoral trochlea widens and angles laterally at its superior aspect. With extension, the patella progresses higher in the groove, placing it in the wider and more lateral aspect of the trochlea. An increased TT-TG distance, which represents a lateralization of the patellar tendon force, would tend to pull the patella to the most lateral location within the sulcus. This force, in combination with increased hip and knee abduction moments, provide explanation for the observed kinematic patterns.26, 27 However, excessive lateral tilt was not seen in this study. Thus, alterations in patellofemoral bone shape, ligament laxity, and/or muscle force balance likely play a role. For example, unique anatomy of the trochlea in adolescents may allow for lateral displacement while restricting excessive lateral tilt. Further, the degree of lateral displacement across the cohort of adolescents with PFP occurred along a spectrum (Figure 4). Thus, the interplay of various biomechanical factors likely explains the individual maltracking patterns observed in this population. It is also likely that for subjects with more normative kinematic patterns, overuse played a more prominent role in the etiology of PFP.
While future work is needed to determine the temporal relationship between maltracking and symptom onset, it appears that isolated lateral patellar displacement is a prominent kinematic abnormality in this population. This information can aid clinicians in developing new conservative therapies for adolescent females with PFP. It also supports tailoring of currently available therapies (e.g., targeted strengthening of the vastus medialis, neuromuscular reeducation, and patellar bracing) to the adolescent population. In addition, the kinematic abnormalities found in this study provide a basis for future clinical trials aiming to optimize outcomes for adolescent females that fail conservative therapy. Given that tibial tubercle osteotomy aims to correct lateral patellar displacement while lateral release targets patellar tilt, pre-operative identification of the patient-specific kinematic abnormality may advance surgical planning.15, 48
Currently, one method of identifying patients with patellar instability that may benefit from a tibial tubercle osteotomy is the TT-TG measurement.8 This is the first study to investigate TT-TG in an adolescent PFP cohort with no history of dislocation. The average TT-TG distances for the PFP (12.2mm) and control (10.0mm) cohorts in this study closely matched the average values found in adolescents with patellar instability (12.1mm)10 and healthy adolescent controls (9.4 mm).51 The average TT-TG of extreme maltrackers (14.2mm) in the current study exceeded that of adolescent subjects with patellar instability.
A potential limitation of this study is sample size. While powered to identify differences in the kinematic patterns of PFP subjects and healthy controls, it is likely that the sample of convenience obtained in this study does not represent all adolescents with PFP. Other kinematic alterations (e.g., tilt, varus, flexion) may be associated with PFP in certain subgroups of adolescents. Regardless of this potential, the present study found a homogenous group of adolescent subjects with PFP, indicating a strong likelihood that this kinematic pattern is a prominent pathological profile in adolescents with pain. Although the study was not designed to evaluate factors outside of kinematics, hormonal abnormalities, such as early exposure to estrogen, may also be present in the adolescent cohort with PFP given the trend towards younger menarche (Table 1).
Extension of the knee against the weight of the lower leg without axial loading of the tibiofemoral joint is not a typical activity of daily living. However, it does serve as a diagnostic tool. Specifically, a strong quadriceps contraction in terminal extension pulls the patella to the superior aspect of the femoral groove, or out of the groove, limiting the boney constraint on the patella. In this setting, any soft tissue imbalances around the patella present as maltracking. In contrast, during an activity such as walking or squatting <60°, the patella likely remains in the femoral groove and the boney constraints limit maltracking. Yet, the soft tissue imbalance remains, likely causing increased or misaligned contact forces. Similar to the design of the current study, a prior cadaveric study16 demonstrated significant lateral displacement with quadriceps muscles loading representative of a free extension exercise. Another previous study50 evaluating patellofemoral patterns in adults with PFP during squatting found that maltracking only occurred at deep flexion (>60°). This coincided with high intensity quadriceps contraction at a range of motion where the patella was situated at or near the wider distal terminal aspect of the sulcus. The authors concluded that identification of patellar maltracking requires reduced bony constraint. Thus, the methodology of the current study was accurately designed to identify subtle force imbalances presenting as kinematic abnormalities.
The primary strength of this study is the specificity of the patient inclusion criteria. All subjects were post-menarche, between 12 – 15 years of age, and demonstrated clinical and radiologic findings that were consistent with the strict definition of PFP. One of the problems in understanding PFP concerns the lack of a consistent definition for knee pain. Across studies, the pathologies that are contained within the definitions for knee pain (PFP, anterior knee pain, patellofemoral dysfunction, patellofemoral maltracking, chondromalacia patellae, patellar instability) varies greatly. Often, these terms are used without clear specification of the pathologies that are being referred to. Further, the majority of studies evaluating the epidemiology or risk factors for PFP in this population include pubescent, post-pubescent, and even pre-pubescent individuals.3, 21, 23, 25 PFP may be unique in each of these groups based purely on developmental status. Specifically, open physes, incongruent increases in limb mass relative to limb length, hormonal fluctuations, and underdeveloped neuromuscular control patterns likely expose adolescents to various pathologies and injuries that are not typically seen in adult patients with PFP.13 To begin to discover the true etiology of PFP in adolescents, studies need to investigate cohorts comprised exclusively of subjects with defined pathology at specific pubescent stages. This study focused on PFP in the strict definition of peripatellar pain in the absence of other structural pathologies (e.g., tendinitis, ligament injury, Osgood-Schlatter’s syndrome, etc.) or history of prior dislocation/trauma among post-menarche adolescent females.
Finally, while significant differences in the average kinematics of the adolescent group with PFP were identified, this study moved beyond averages by investigating the patterns for individual subjects. For these subjects, rigorous training regimens may have played a more dominant role in the etiology of pain. To provide optimal therapy for this complex patient population, identification of subject-specific tracking patterns should be the goal of future clinical trials.
Conclusion
This study demonstrates that abnormal patellar tracking patterns are present in adolescent females with PFP. Rigorous athletic training alone might not be adequate to produce patellofemoral pain in this population. Rather, patellofemoral pain may result from the combination of physical activity in the context of pathologic kinematics. Accurate evaluation of patellofemoral kinematics in adolescent females with PFP is encouraged for clinical decision making.
What is known about the subject
Patellofemoral pain is a common disorder with a high prevalence among adolescent females. Abnormal patellar tracking patterns and abnormal static alignment have been shown to contribute to the etiology of patellofemoral pain in adults.
What this study adds to existing knowledge
This study demonstrates that pathologic patellar tracking patterns are present in adolescent females with patellofemoral pain.
Acknowledgments
The authors thank A.J. Behnam and J.N. Jackson for assisting in data collection. The authors also thank informationist Judith Welsh, NIH Library, for editing this article.
References
- 1.Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33(1):75–81. doi: 10.2165/00007256-200333010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Balcarek P, Jung K, Frosch KH, Sturmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–1761. doi: 10.1177/0363546511404883. [DOI] [PubMed] [Google Scholar]
- 3.Barber Foss KD, Myer GD, Chen SS, Hewett TE. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train. 2012;47(5):519–524. doi: 10.4085/1062-6050-47.5.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beasley MA, Stracciolini A, Tyson KD, Stein CJ. Knee injury patterns in young irish dancers. Med Probl Perform Art. 2014;29(2):70–73. doi: 10.21091/mppa.2014.2016. [DOI] [PubMed] [Google Scholar]
- 5.Behnam AJ, Herzka DA, Sheehan FT. Assessing the accuracy and precision of musculoskeletal motion tracking using cine-PC MRI on a 3.0T platform. J Biomech. 2011;44(1):193–197. doi: 10.1016/j.jbiomech.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biedert RM, Gruhl C. Axial computed tomography of the patellofemoral joint with and without quadriceps contraction. Arch Orthop Trauma Surg. 1997;116(1-2):77–82. doi: 10.1007/BF00434106. [DOI] [PubMed] [Google Scholar]
- 7.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 9.Derasari A, Brindle TJ, Alter KE, Sheehan FT. McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010;90(3):411–419. doi: 10.2522/ptj.20080365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G. Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014;96(4):318–324. doi: 10.2106/JBJS.M.00688. [DOI] [PubMed] [Google Scholar]
- 11.Earl JE, Vetter CS. Patellofemoral pain. Phys Med Rehabil Clin N Am. 2007;18(3):439–458, viii. doi: 10.1016/j.pmr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Erkocak OF, Altan E, Altintas M, Turkmen F, Aydin BK, Bayar A. Lower extremity rotational deformities and patellofemoral alignment parameters in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3611-y. [DOI] [PubMed] [Google Scholar]
- 13.Frank JB, Jarit GJ, Bravman JT, Rosen JE. Lower extremity injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2007;15(6):356–366. doi: 10.5435/00124635-200706000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Freedman BR, Sheehan FT. Predicting three-dimensional patellofemoral kinematics from static imaging-based alignment measures. J Orthop Res. 2013;31(3):441–447. doi: 10.1002/jor.22246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 16.Goudakos IG, Konig C, Schottle PB, et al. Stair climbing results in more challenging patellofemoral contact mechanics and kinematics than walking at early knee flexion under physiological-like quadriceps loading. J Biomech. 2009;42(15):2590–2596. doi: 10.1016/j.jbiomech.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Guzzanti V, Gigante A, Di Lazzaro A, Fabbriciani C. Patellofemoral malalignment in adolescents. Computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med. 1994;22(1):55–60. doi: 10.1177/036354659402200110. [DOI] [PubMed] [Google Scholar]
- 18.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 19.Herbst KA, Barber Foss KD, Fader L, et al. Hip Strength Is Greater in Athletes Who Subsequently Develop Patellofemoral Pain. Am J Sports Med. 2015;43(11):2747–2752. doi: 10.1177/0363546515599628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hunter DJ, Zhang YQ, Niu JB, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthri Cartil. 2007;15(10):1120–1127. doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson RP. Anterior knee pain in adolescents and young adults. Curr Opin Rheumatol. 1997;9(2):159–164. doi: 10.1097/00002281-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 23.Luhmann SJ, Schoenecker PL, Dobbs MB, Eric Gordon J. Adolescent patellofemoral pain: implicating the medial patellofemoral ligament as the main pain generator. J Child Orthop. 2008;2(4):269–277. doi: 10.1007/s11832-008-0104-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88(12):2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 25.Moretz JA, 3rd, Harlan SD, Goodrich J, Walters R. Long-term followup of knee injuries in high school football players. Am J Sports Med. 1984;12(4):298–300. doi: 10.1177/036354658401200410. [DOI] [PubMed] [Google Scholar]
- 26.Myer GD, Ford KR, Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25(7):700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Di Stasi SL, Foss KD, Micheli LJ, Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49(2):118–122. doi: 10.1136/bjsports-2013-092536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. doi: 10.2519/jospt.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 30.Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is Knee Pain During Adolescence a Self-limiting Condition? Prognosis of Patellofemoral Pain and Other Types of Knee Pain. Am J Sports Med. 2016 doi: 10.1177/0363546515622456. [DOI] [PubMed] [Google Scholar]
- 31.Rathleff MS, Roos EM, Olesen JL, Rasmussen S. High prevalence of daily and multi-site pain–a cross-sectional population-based study among 3000 Danish adolescents. BMC Pediatr. 2013;13:191. doi: 10.1186/1471-2431-13-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rathleff MS, Vicenzino B, Middelkoop M, et al. Patellofemoral Pain in Adolescence and Adulthood: Same Same, but Different? Sports Med. 2015;45(11):1489–1495. doi: 10.1007/s40279-015-0364-1. [DOI] [PubMed] [Google Scholar]
- 33.Regalado G, Lintula H, Eskelinen M, et al. Dynamic KINE-MRI in patellofemoral instability in adolescents. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2795–2802. doi: 10.1007/s00167-013-2679-5. [DOI] [PubMed] [Google Scholar]
- 34.Sacks D. Age limits and adolescents. Paediatr Child Health. 2003;8(9):577. doi: 10.1093/pch/8.9.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seisler AR, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng. 2007;54(7):1333–1341. doi: 10.1109/TBME.2007.890735. [DOI] [PubMed] [Google Scholar]
- 36.Selfe J, Sutton C, Hardaker NJ, Greenhalgh S, Karki A, Dey P. Anterior knee pain and cold knees: a possible association in women. Knee. 2010;17(5):319–323. doi: 10.1016/j.knee.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res. 2009;27(5):561–570. doi: 10.1002/jor.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468(1):266–275. doi: 10.1007/s11999-009-0880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sheehan FT, Mitiguy P. In regards to the “ISB recommendations for standardization in the reporting of kinematic data”. J Biomech. 1999;32(10):1135–1136. doi: 10.1016/s0021-9290(99)00077-9. [DOI] [PubMed] [Google Scholar]
- 40.Shibanuma N, Sheehan FT, Stanhope SJ. Limb positioning is critical for defining patellofemoral alignment and femoral shape. Clin Orthop Relat Res. 2005;(434):198–206. doi: 10.1097/01.blo.0000155078.52475.63. [DOI] [PubMed] [Google Scholar]
- 41.Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. J Pediatr. 2011;158(1):119–123. 123.e111–114. doi: 10.1016/j.jpeds.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 42.Soderman K, Adolphson J, Lorentzon R, Alfredson H. Injuries in adolescent female players in European football: a prospective study over one outdoor soccer season. Scand J Med Sci Sports. 2001;11(5):299–304. doi: 10.1034/j.1600-0838.2001.110508.x. [DOI] [PubMed] [Google Scholar]
- 43.Stracciolini A, Casciano R, Levey Friedman H, Stein CJ, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med. 2014;42(4):965–972. doi: 10.1177/0363546514522393. [DOI] [PubMed] [Google Scholar]
- 44.Suzue N, Matsuura T, Iwame T, et al. Prevalence of childhood and adolescent soccer-related overuse injuries. J Med Invest. 2014;61(3-4):369–373. doi: 10.2152/jmi.61.369. [DOI] [PubMed] [Google Scholar]
- 45.Tallay A, Kynsburg A, Toth S, et al. Prevalence of patellofemoral pain syndrome. Evaluation of the role of biomechanical malalignments and the role of sport activity. Orv Hetil. 2004;145(41):2093–2101. [PubMed] [Google Scholar]
- 46.Tenforde AS, Sayres LC, McCurdy ML, Collado H, Sainani KL, Fredericson M. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. Pm r. 2011;3(2):125–131. doi: 10.1016/j.pmrj.2010.09.009. quiz 131. [DOI] [PubMed] [Google Scholar]
- 47.Thomee R, Renstrom P, Karlsson J, Grimby G. Patellofemoral pain syndrome in young women. I. A clinical analysis of alignment, pain parameters, common symptoms and functional activity level. Scand J Med Sci Sports. 1995;5(4):237–244. [PubMed] [Google Scholar]
- 48.Tigchelaar S, van Essen P, Benard M, Koeter S, Wymenga A. A self-centring osteotomy of the tibial tubercle for patellar maltracking or instability: results with ten-years’ follow-up. Bone Joint J. 2015;97-b(3):329–336. doi: 10.1302/0301-620X.97B3.34515. [DOI] [PubMed] [Google Scholar]
- 49.Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12(5):362–365. doi: 10.1016/j.knee.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 50.Wilson NA, Press JM, Koh JL, Hendrix RW, Zhang LQ. In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am. 2009;91(3):558–566. doi: 10.2106/JBJS.G.00572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wittstein JR, Bartlett EC, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy. 2006;22(6):643–649. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 52.Yen YM. Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin North Am. 2014;61(6):1155–1173. doi: 10.1016/j.pcl.2014.08.003. [DOI] [PubMed] [Google Scholar]


