Abstract
Methotrexate-related lymphoproliferative disorder (MTX-LPD) is a rare disorder caused by long-term MTX therapy for autoimmune diseases. There has been no report of the dermoscopic features of MTX-LPD to date. A 64-year-old female presented with a slightly elevated indurated erythematous plaque with scales on her right thigh. The patient had been treated for rheumatic arthritis with MTX and prednisolone for more than 15 years, and 18 mg/week MTX without prednisolone had been administered in the last year. Dermoscopy revealed dotted vessels and glomerular vessels on pink homogeneous areas and multiple surface scales. Enhanced computed tomography showed multiple nodules and lymphadenopathies at the mediastinum and axillae. Histopathological examination revealed telangiectasia in the superficial dermis. Atypical lymphoid cells were scattered in the whole dermis and subcutaneous tissue. A perivascular infiltrate of atypical lymphocytes and histiocytoid cells partially destroyed the vessel walls. Epstein-Barr virus in situ hybridization showed a positive result. The cessation of MTX reduced the erythematous plaque, and lymphadenopathies at the neck, mediastinum, and axillae were not palpable. We discuss the relevance of these dermoscopic and histopathological features. The accumulation of such cases will reveal the dermoscopic features of MTX-LPD and the utility of dermoscopy for the diagnosis of MTX-LPD.
Keywords: Methotrexate, Lymphoproliferative disorder, Dermoscopy, Epstein-Barr virus
Introduction
Methotrexate-related lymphoproliferative disorder (MTX-LPD) is a rare disorder caused by long-term MTX therapy for autoimmune diseases [1, 2]. Although a careful examination of skin lesions is critical for an accurate diagnosis of MTX-LPD, no report of dermoscopic features has been published. Here, we report a case of MTX-LPD and, for the first time, present its dermoscopic features.
Case Report
A 64-year-old female presented with an erythematous plaque on her right thigh. The patient had received prednisolone, JAK inhibitor, certolizumab, and infliximab 8 mg/kg for rheumatoid arthritis over a span of 15 years and had started 18 mg/week of MTX 4 years before presentation, which persisted with the infliximab at presentation. A subcutaneous, tender, erythematous tumor had appeared on her right thigh 1 month after the cessation of prednisolone. The patient consulted the Department of Dermatology due to no remission 1 month after the cessation of infliximab. Physical examination revealed a slightly elevated indurated erythematous plaque with scales on her right thigh (Fig. 1a). Dermoscopy revealed ambiguous dotted/glomerular vessels on pink homogeneous areas (Fig. 1b), which were clearly visible with contrast enhancement (Fig. 1c), and multiple surface scales (Fig. 1b, c). Enhanced computed tomography showed multiple nodules and lymphadenopathies at the mediastinum and axillae. A bone marrow biopsy revealed a negative result. Histopathological examination revealed perivascular infiltrates of atypical lymphocytes and histiocytoid cells in the dermis and subcutaneous tissues (Fig. 2a, b). Atypical lymphocytes with halos infiltrated the small vessels (Fig. 2c). Partial destruction of vessels compensatively expanded vessels in the superficial dermis (Fig. 2d). Immunohistochemistry showed positive reactions for CD15, CD20 (Fig. 2e), CD30, CD79a, and Bcl-2 and negative reactions for CD3, CD5, CD7, CD10, CD56, granzyme B, TIA-1, and ALK. Positivity of atypical lymphoid cells was 80%. Epstein-Barr virus-encoded RNA in situ hybridization showed a positive result (Fig. 2f). Immunohistochemistry for CD34 and α-SMA highlighted dilated vessels in the superficial dermis (Fig. 2g). Both histopathological and immunohistochemical findings did not imply Epstein-Barr virus-positive Hodgkin lymphoma. The erythematous plaques disappeared 1 month after the cessation of MTX. The diagnosis of MTX-LPD was made. Lymphadenopathies at the neck, mediastinum, and axillae were reduced 4 months after the cessation of MTX.
Fig. 1.

a Slightly elevated indurated erythematous plaque with scales on the patient's right thigh. b Dermoscopy showing multiple surface scales and pink homogeneous areas. c Contrast-enhanced image of the dermoscopic features; dotted/glomerular vessels were noted at the center of the lesion.
Fig. 2.
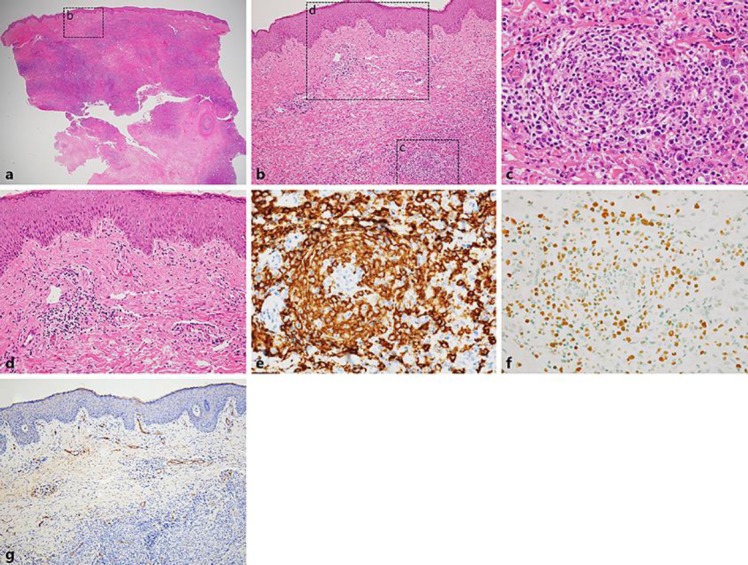
a Histopathology showing perivascular infiltrates of lymphoid cells in the dermis and subcutaneous tissues; the dotted box labelled “b” indicates an area shown in b (HE stain; original magnification, ×12.5). b Dilated vessels were found in the superficial dermis, and a perivascular infiltrate of atypical lymphocytes and histiocytoid cells partially destroyed the vessel walls; dotted boxes labelled “c” and “d” indicate areas shown in c and d, respectively (HE stain; original magnification, ×100). c Atypical lymphocytes with halos infiltrated the vessels; some atypical lymphocytes with halos had convoluted and enlarged nuclei (HE stain; original magnification, ×400). d Partial destruction of vessels compensatively expanded vessels in the superficial dermis (HE stain; original magnification, ×200). e Immunohistochemistry for CD20 showing a positive reaction in atypical lymphocytes; the area shown is the same as in c (original magnification, ×400). f Epstein-Barr virus-encoded RNA in situ hybridization and a positive result in atypical lymphocytes; the area shown is the same as in e (original magnification, ×400). g Immunohistochemistry for CD34 revealing dilated vessels in the superficial dermis (original magnification, ×100).
Discussion
MTX-LPD is an LPD caused by MTX and is categorized under iatrogenic immunodeficiency-associated LPD. Cutaneous manifestations of MTX-LPD are nodules and/or erythematous plaques [3]. Although vascular findings of dermoscopy are difficult to be specified in the differential diagnosis between amelanotic melanomas, nonpigmented Bowen disease, and other cutaneous lymphomas, the lack of both apparent polymorphous vessels and dermoscopic findings of the epidermal structures may not imply the diagnosis of amelanotic melanomas and nonpigmented Bowen disease. In cutaneous lymphomas, serpentine vessels and fine short linear vessels are frequent in primary B-cell lymphoma and mycosis fungoides, respectively [4, 5]. In our case, dotted/glomerular vessels on pinkish backgrounds are the main dermoscopic features. Those dermoscopic features of vascular structures may partially reflect histopathological features of vascular damages by atypical lymphocytes. Although it is difficult to specify a particular subset of cutaneous lymphomas by dermoscopy, accumulation of such cases may reveal frequent dermoscopic features of MTX-LPD.
Statement of Ethics
Informed consent has been obtained and no ethics approval was required for reporting of a single case.
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Kamel OW, van de Rijn M, Weiss LM, Del Zoppo GJ, Hench PK, Robbins BA, et al. Brief report reversible lymphomas associated with Epstein-Barr virus occurring during methotrexate therapy for rheumatoid arthritis and dermatomyositis. N Engl J Med. 1993 May;328((18)):1317–21. doi: 10.1056/NEJM199305063281806. [DOI] [PubMed] [Google Scholar]
- 2.Shimura C, Satoh T, Takayama K, Yokozeki H. Methotrexate-related lymphoproliferative disorder with extensive vascular involvement in a patient with rheumatoid arthritis. J Am Acad Dermatol. 2009 Jul;61((1)):126–9. doi: 10.1016/j.jaad.2008.10.051. [DOI] [PubMed] [Google Scholar]
- 3.Shimizu S, Inokuma D, Murata J, Kikuchi K, Ito T, Fukasawa Y, et al. Cutaneous manifestations of methotrexate-associated lymphoproliferative disorders report of two cases and a review of the literature. Acta Derm Venereol. 2015 Mar;95((3)):366–7. doi: 10.2340/00015555-1951. [DOI] [PubMed] [Google Scholar]
- 4.Lallas A, Apalla Z, Lefaki I, Tzellos T, Karatolias A, Sotiriou E, et al. Dermoscopy of early stage mycosis fungoides. J Eur Acad Dermatol Venereol. 2013 May;27((5)):617–21. doi: 10.1111/j.1468-3083.2012.04499.x. [DOI] [PubMed] [Google Scholar]
- 5.Geller S, Marghoob AA, Scope A, Braun RP, Myskowski PL. Dermoscopy and the diagnosis of primary cutaneous B-cell lymphoma. J Eur Acad Dermatol Venereol. 2018 Jan;32((1)):53–6. doi: 10.1111/jdv.14549. [DOI] [PMC free article] [PubMed] [Google Scholar]


