Abstract
Background:
Very few data have been reported for ST-segment elevation myocardial infarction (STEMI) caused by unprotected left main coronary artery (ULMCA) occlusion, and very little is known about the results of this subgroup of patients who underwent primary percutaneous coronary intervention (PCI). The aim of this study was to determine the clinical features and outcomes of patients with STEMI who underwent primary PCI for acute ULMCA occlusion.
Methods:
From January 2000 to February 2014, 372 patients with STEMI caused by ULMCA acute occlusion (ULMCA-STEMI) who underwent primary PCI at one of two centers were enrolled. The 230 patients with non-ST-segment elevation MI (NSTEMI) caused by ULMCA lesion (ULMCA-NSTEMI) who underwent emergency PCI were designated the control group. The main indexes were the major adverse cardiac events (MACEs) in-hospital, at 1 month, and at 1 year.
Results:
Compared to the NSTEMI patients, the patients with STEMI had significantly higher rates of Killip class≥III (21.2% vs. 3.5%, χ2 = 36.253, P < 0.001) and cardiac arrest (8.3% vs. 3.5%, χ2 = 5.529, P = 0.019). For both groups, the proportions of one-year cardiac death in the patients with a post-procedure thrombolysis in myocardial infarction (TIMI) flow grade<3 were significantly higher than those in the patients with a TIMI flow grade of 3 (STEMI group: 51.7% [15/29] vs. 4.1% [14/343], P < 0.001; NSTEMI group: 33.3% [3/9] vs. 13.6% [3/221], P = 0.001; respectively]. Landmark analysis showed that the patients in STEMI group were associated with higher risks of MACE (16.7% vs. 9.1%, P = 0.009) and cardiac death (5.4% vs. 1.3%, P = 0.011) compared with NSTEMI patients at 1 month. Meanwhile, in patients with ULMCA, the landmark analysis for incidences of MACE and cardiac death was similar between the STEMI and NSTEMI (all P = 0.72) in the intervals of 1–12 months. However, patients who were diagnosed with STEMI or NSTEMI had no significant difference in reinfarction (all P > 0.05) and TVR (all P > 0.05) in the intervals of 0–1 month as well as 1 month to 1 year. The results of Cox regression analysis showed that the differences in the independent predictors for MACE included the variables of Killip class ≥ III and intra-aortic balloon pump support for the STEMI patients and the variables of previous MI, ULMCA distal bifurcation, and 2-stent for distal ULMCA lesions for the NSTEMI patients.
Conclusions:
Compared to the NSTEMI patients, the patients with STEMI and ULMCA lesions still remain at a much higher risk for adverse events at 1 year, especially on 1 month. If a successful PCI procedure is performed, the 1-year outcomes in those patients might improve.
Keywords: Left Main Coronary Artery, Myocardial Infarction, Percutaneous Coronary Intervention
摘要
背景:
目前关于直接经皮冠状动脉介入(PCI)治疗无保护左主干(ULMCA)闭塞所致ST段抬高型心肌梗死(STEMI)患者 疗效的相关研究报道非常少。本文旨在观察直接PCI治疗ULMCA为罪犯病变STEMI患者的临床特点及预后。
方法:
在2000.1~2014.2期间,沈阳军区总医院和南京第一医院心脏中心共有372例ULMCA闭塞导致的STEMI患者(ULMCA-STEMI) 接受了直接PCI治疗。另有230例ULMCA病变导致非ST段抬高型心肌梗死患者(ULMCA-NSTEMI)接受了急诊PCI, 此部分患者设为对照组。主要观察终点为患者住院期间、1个月及1年的主要心脏不良事件[MACE,包括心性死亡、心肌梗死 (MI)及靶血管重建(TVR)]。
结果:
分析提示,Killip=?级和有心脏复苏史的患者在STEMI组的比例明显高于NSTEMI组(分别是21.2% vs. 3.5%, χ2 = 36.253, P<0.001和8.3% vs. 3.5%, χ2 = 5.529, P=0.019)。亚组分析结果提示,两组术后血流TIMI>3级患者的1年心性死亡率均明显高于术 后血流TIMI 3级的患者(分别是STEMI组: 51.7% [15/29] vs. 4.1% [14/343], P<0.001; NSTEMI组: 33.3% [3/9] vs. 13.6% [3/221], P=0.001)。Landmark分析显示与NSTEMI患者相比,STEMI组患者术后1个月内具有更高的MACE和心性死亡风险(分别是 P=0.009;P=0.011),但在术后1个月至12个月期间,两组MACE和心性死亡的风险无明显差异(均P=0.72)。无论在术后1个 月内还是在术后1个月至12个月期间,两组再发MI和TVR的风险无明显差异(均P>0.05)。Cox回归分析显示,两组患者发生 MACE的独立危险因素存在不同,其中Killip=≥级和置入主动脉内囊反搏是STEMI组患者发生MACE的独立危险因素, 而既 往MI、分叉病变及双支架术是NSTEMI组患者发生MACE的独立危险因素。
结论:
与NSTEMI患者相比,因ULMCA急性闭塞的STEMI患者术后仍然面临较高的1年心脏事件风险,尤其是在术后1个月内 更甚。无论STMEI还是NSTEMI患者,若PCI手术成功实施,均将改善其1年的临床疗效。
INTRODUCTION
Patients who present with acute myocardial infarction (AMI), including those with ST-segment elevation MI (STEMI) and those with non-ST-segment elevation MI (NSTEMI) caused by acute unprotected left main coronary artery (ULMCA) occlusion, represent a very high-risk group of patients who may be susceptible to associated cardiogenic shock, malignant ventricular arrhythmias, and sudden death.[1,2,3,4,5,6] In patients presenting with AMI, primary percutaneous coronary intervention (PCI) is considered the optimal revascularization strategy. However, the current guidelines consider that the standard revascularization strategy for ULMCA disease is still coronary artery bypass graft.[7,8] However, this strategy was also confronted with a very high mortality and morbidity in patients presenting with AMI due to ULMCA occlusion, especially in hemodynamically unstable or malignant ventricular arrhythmias. Recently, some published results have produced acceptable results in primary PCI in patients with ULMCA-STEMI. However, most of those results were often from small sample size, single-arm, or single-center studies.[9,10,11,12] To distinctively describe the clinical characteristics and follow-up outcomes for patients with ULMCA-STEMI, the patients with ULMCA-NSTEMI in this study were designed as the control group and also had emergency PCI performed. The main purpose of this study was to observe the characteristics of patients with ULMCA-STEMI as described above and to identify the differences in the clinical, angiographic, and procedural features and in-hospital, 1-month, and 1-year outcomes of patients with ULMCA-STEMI or NSTEMI who underwent emergency PCI.
METHODS
Ethical approval
This study was approved by the Medical Ethics Committee of General Hospital of Shenyang Military Region, China (No.(2015) 67). As a retrospective study, this study was exempt from obtaining the informed consent of patients.
Patients
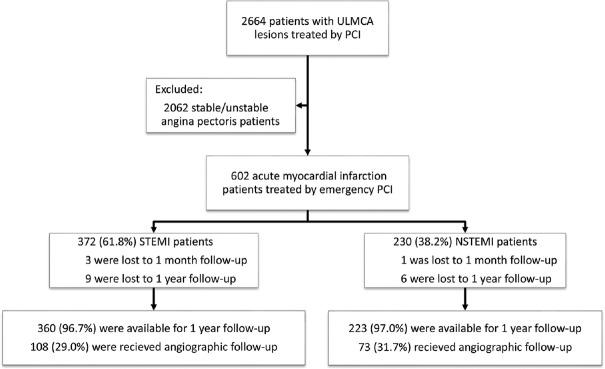
Between January 27, 2000, and February 1, 2014, 2664 consecutive patients with ULMCA who underwent PCI were enrolled and retrospectively studied at two centers (General Hospital of Shenyang Military Region and Nanjing First Hospital). Of these patients, 602 consecutive patients were diagnosed with AMI and subsequently underwent emergency PCI, including primary PCI, PCI after thrombolysis for STEMI patients, and emergency PCI for NSTEMI patients. ULMCA was identified as being the culprit of the lesions by angiography. Of these patients, 372 patients were diagnosed with STEMI (STEMI group) and 230 patients were diagnosed with NSTEMI (NSTEMI group). STEMI was defined as chest pain persisting for over 30 min and ST-segment elevation of the avR lead with ST-segment depression of the anterior and lower wall leads on the electrocardiogram. NSTEMI without ST-segment elevation in the electrocardiogram was defined as ischemic symptoms and either an increase in the creatine kinase level, with an isoenzyme-MB level that was three times that of the upper limit of the normal level, or abnormal troponin levels [Figure 1]. The patients were treated with aspirin and clopidogrel for at least 1 year after the PCI procedure. Prasugrel and ticagrelor were not available for use. Other cardiovascular medications were given as per their current guidelines. The left main coronary artery was considered to be unprotected if there were no patent coronary artery bypass grafts or the right coronary artery (RCA) to the left anterior descending artery or left circumflex artery. The procedural strategy (thrombus aspiration, balloon dilatation, stent selection, use of an intra-aortic balloon pump [IABP], and anticoagulation regimen) was left to the discretion of the operator.
Figure 1.
Study flow diagram. Comparison between the 1-year outcomes in patients with STEMI and those in patients with NSTEMI who received emergency PCI in ULMCA lesions. ULMCA: Unprotected left main coronary artery; PCI: Percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction.
Definitions and endpoints
PCI procedural success was defined as mean lesion diameter stenosis <30% in 2 near-orthogonal projections with thrombolysis in MI (TIMI) flow grade of 3 after emergency procedures, as visually assessed by the physician. The primary endpoint was the composite of major adverse cardiac events (MACEs: cardiac death, MI, or target vessel revascularization [TVR]) in-hospital, at 1 month, and at 1 year. Additional endpoints included definite stent thrombosis according to the ARC criteria.[13] Detailed procedural and event data were monitored at two centers by an independent contract research organization. All of the MACE and definite/probable stent thrombosis events were adjudicated by an independent clinical event committee.
Follow-up
All of the surviving patients with no clinical contraindications were scheduled for angiographic evaluation at a 9-month mean follow-up time. The clinical follow-up data were obtained from an outpatient clinic visit or by direct telephone contact. The follow-up period began at the moment of hospital discharge. The data of the follow-up were retrospectively collected in a dedicated database.
Statistical analysis
Continuous variables were presented as mean ± standard deviation (SD) and were compared with Student's t-test or one-way analysis of variance (ANOVA). Categorical variables were presented as frequency (%) and were compared with the Chi-square or Fisher's exact test. Survival curves were generated by the Kaplan-Meier method. Landmark analysis was performed with a landmark of 1 month among patients who were event free at this time. Multivariate analysis of the 1-year MACE in STEMI and NSTEMI patients was performed using Cox regression analysis. Performed with the STEMI and NSTEMI groups separately, the candidate variables entered into regression equation were described by previous reports about the procedure for patients with ULMCA lesions.[1,2,3,4,5,6,9,10,11,12,14] The variables were removed if they produced P > 0.10. The results were presented as the hazard ratio (HR) and relative risk with the 95% confidence interval (CI). A value of P < 0.05 was considered statistically significant. All statistical analyses were two sided and were performed with SPSS Statistics version 19.0 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
Baseline clinical data
The baseline demographic data are presented in Table 1. Compared with the NSTEMI group, the STEMI group had a significantly lower proportions of patients with histories of hypertension, previous MI and PCI (51.3% vs. 64.3%, P = 0.002; 4.8% vs. 13.0%, P < 0.001; and 8.3% vs. 17.0% P = 0.001, respectively). However, the patients with STEMI and ULMCA lesions had significantly higher proportions of Killip class ≥III (21.2% vs. 3.5%, P < 0.001), cardiac arrest (8.3% vs. 3.5%, P = 0.019), and worse heart function (left ventricular ejection fraction [LVEF] <35%, 21.7% vs. 12.4%, P = 0.007) than the patients in the NSTEMI group.
Table 1.
Summary of the demographic and clinical characteristics between the two groups
| Characteristic | STEMI (n = 372) | NSTEMI (n = 230) | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 63.4 ± 11.5 | 65.2 ± 11.0 | −1.896* | 0.058 |
| Male gender, n (%) | 313 (84.1) | 173 (75.2) | 7.273† | 0.007 |
| Current smoke, n (%) | 207 (55.6) | 104 (45.2) | 6.189† | 0.013 |
| Hypercholesterolemia, n (%) | 163 (43.8) | 97 (42.2) | 0.156† | 0.692 |
| Diabetes mellitus, n (%) | 117 (31.5) | 69 (30.0) | 0.140† | 0.708 |
| Hypertension, n (%) | 191 (51.3) | 148 (64.3) | 9.769† | 0.002 |
| Chronic pulmonary disease, n (%) | 29 (7.8) | 20 (8.7) | 0.154† | 0.695 |
| Previous stroke, n (%) | 53 (14.2) | 26 (11.3) | 1.080† | 0.299 |
| Renal insufficiency, n (%) | 29 (7.8) | 23 (10.0) | 0.944† | 0.350 |
| Previous MI, n (%) | 18 (4.8) | 30 (13.0) | 12.527† | <0.001 |
| Previous PCI, n (%) | 31 (8.3) | 39 (17.0) | 10.285† | 0.001 |
| Systolic blood pressure (mmHg) | 105.2 ± 7.4 | 113.4 ± 12.3 | −10.341* | <0.001 |
| Total ischemic time, n (%) | ||||
| 0<Time (h)≤6 | 149 (40.1) | 13 (5.7) | 85.518† | <0.001 |
| 6<Time (h)≤12 | 183 (49.2) | 26 (11.3) | 90.024† | 0.001 |
| 12<Time (h)≤24 | 33 (8.9) | 117 (50.9) | 134.001† | <0.001 |
| 24<Time (h)≤72 | 7 (1.9) | 74 (32.1) | 111.997† | <0.001 |
| Cardiac arrest, n (%) | 31 (8.3) | 8 (3.5) | 5.529† | 0.019 |
| Killip class ≥III, n (%) | 79 (21.2) | 8 (3.5) | 36.253† | <0.001 |
| LVEF <35%, n (%) | 75 (21.7) | 24 (12.4) | 7.189† | 0.007 |
*t values; †χ2 values. Total ischemic time indicates that the time is from symptom onset to reperfusion. 1 mmHg=0.133 kPa. STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; MI: Myocardial infarction; PCI: Percutaneous coronary intervention; LVEF: Left ventricular ejection fraction.
Angiographic and procedural data
The angiographic and procedural data are presented in Table 2. The patients in the STEMI group had significantly lower proportions of left main artery distal bifurcation and RCA chronic occlusion lesion (19.1% vs. 27.8%, P = 0.012 and 1.1% vs. 9.1%, P < 0.001, respectively) than those in the NSTEMI group. However, 96 (25.8%) of 372 STEMI patients received thrombolytic therapy before the emergency PCI procedure. The STEMI patients still had significantly higher emergency procedure risk profiles, such as lower TIMI flow grade before PCI (pre-PCI TIMI flow grade 0/1: 66.9% vs. 19.6%, P < 0.001) and IABP support (20.7% vs. 13.5%, P = 0.025).
Table 2.
Summary of the angiographic and procedural characteristics of the two groups
| Characteristics | STEMI (n = 372) | NSTEMI (n = 230) | t/χ2 | P |
|---|---|---|---|---|
| Right dominance, n (%) | 207 (55.6) | 141 (61.3) | 1.866* | 0.172 |
| Left main, n (%) | ||||
| Ostial/body | 239 (64.2) | 152 (66.0) | 0.211* | 0.646 |
| Distal bifurcation | 71 (19.1) | 64 (27.8) | 6.241* | 0.012 |
| 2/3-vessel disease, n (%) | ||||
| Long lesions in RCA or LCX | 136 (36.6) | 98 (42.6) | 2.189* | 0.139 |
| Long lesions in LAD | 36 (9.7) | 20 (8.7) | 0.162* | 0.687 |
| CTO in RCA, n (%) | 4 (1.1) | 21 (9.1) | 23.169* | <0.001 |
| Pre-PCI TIMI flow, n (%) | ||||
| Grade 0/1 | 249 (66.9) | 45 (19.6) | 127.638* | <0.001 |
| Grade 2 | 117 (31.5) | 93 (40.4) | 5.049* | 0.025 |
| Grade 3 | 6 (1.6) | 92 (40.0) | 153.667* | <0.001 |
| Post-PCI TIMI flow, n (%) | ||||
| Grade 0–2 | 29 (7.8) | 9 (4.0) | 3.617* | 0.062 |
| Grade 3 | 343 (92.8) | 221 (96.0) | ||
| Balloon only, n (%) | 4 (1.1) | 0 (0) | ||
| Bare metal stent, n (%) | 45 (12.2) | 10 (4.3) | 10.531* | 0.001 |
| 2-stent for distal LM lesions, n (%) | 31 (8.3) | 50 (21.7) | 21.935* | <0.001 |
| Stent in LM per patient | ||||
| Diameter (mm) | 3.43 ± 0.59 | 3.42 ± 0.37 | 0.189† | 0.850 |
| Length (mm) | 28.0 ± 12.6 | 30.0 ± 12.6 | –1.892† | 0.059 |
| IVUS guidance, n (%) | 13 (3.5) | 17 (7.4) | 4.588* | 0.033 |
| IABP support, n (%) | 77 (20.7) | 31 (13.5) | 5.034* | 0.025 |
| Thrombectomy, n (%) | 67 (18.0) | 19 (8.3) | 11.033* | <0.001 |
| Glycoprotein IIb/IIIa inhibitor, n (%) | 109 (29.3) | 59 (25.7) | 0.941* | 0.332 |
*χ2 values; †t values. STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; RCA: Right coronary artery; LCX: Left circumflex artery; LAD: Left anterior descending coronary artery; CTO: Chronic total occlusion; PCI: Percutaneous coronary intervention; TIMI: Thrombolysis in myocardial infarction; LM: Left main artery; IVUS: Intravenous ultrasound; IABP: Intra-aortic balloon pump.
In-hospital, 1-month, and 1-year outcomes
The results of the in-hospital, 1-month, and 1-year outcomes are presented in Table 3. For the higher proportions of in-hospital and 1-month cardiac death in the STEMI patients, the total MACE of them at 1 month was significantly increased compared to that of the NSTEMI patients (22.0% vs. 14.3%, P = 0.020). Similarly, the proportions of 1-year cardiac death were significantly different between the two groups (7.0% vs. 2.6%, P = 0.020). After excluding in-hospital and 1-month cardiac death, the proportions of 1-year cardiac death and MACE were almost equal between the two groups (1-year cardiac death: 1.3% [5/372] vs. 1.3% [3/230], P = 0.967; and 1-year MACE: 5.4% [20/372] vs. 4.3% [10/230], P = 0.318).
Table 3.
Medication and outcomes of in-hospital, 1-month, and 1-year follow-up between two groups
| Characteristics | STEMI (n = 372) | NSTEMI (n = 230) | χ2 | P |
|---|---|---|---|---|
| Medications in hospital, n (%) | ||||
| DAPT | 370 (99.5) | 229 (99.6) | 0.030 | 1.000 |
| Statins | 309 (83.1) | 181 (78.7) | 1.791 | 0.181 |
| Medications at 1 month, n | 353 | 228 | ||
| DAPT, n (%) | 351 (99.4) | 224 (98.2) | 1.912 | 0.217 |
| Statins, n (%) | 294 (83.3) | 185 (81.1) | 0.441 | 0.507 |
| Medications at 1 year, n | 349 | 226 | ||
| DAPT, n (%) | 327 (93.7) | 208 (92.0) | 0.585 | 0.445 |
| Statins, n (%) | 278 (79.7) | 177 (78.3) | 0.149 | 0.700 |
| In-hospital MACE, n (%) | 44 (11.8) | 16 (7.0) | 3.759 | 0.053 |
| Cardiac death | 17 (4.6) | 2 (0.9) | 6.367 | 0.014 |
| MI | 15 (4.0) | 8 (3.5) | 0.119 | 0.730 |
| TVR | 12 (3.2) | 6 (2.7) | 1.172 | 0.279 |
| All-cause death, n (%) | 19 (5.1) | 2 (0.9) | 7.582 | 0.006 |
| Definite/probable ST, n (%) | 7 (1.9) | 4 (1.8) | 0.016 | 1.000 |
| 1-month MACE, n (%) | 55 (14.7) | 19 (8.3) | 5.611 | 0.018 |
| Cardiac death | 21 (5.6) | 3 (1.3) | 6.996 | 0.008 |
| MI | 16 (4.3) | 8 (3.5) | 0.251 | 0.616 |
| TVR | 18 (4.8) | 8 (3.5) | 0.637 | 0.425 |
| All-cause death, n (%) | 23 (6.2) | 4 (1.7) | 6.551 | 0.010 |
| Definite/probable ST, n (%) | 7 (1.9) | 4 (1.7) | 0.016 | 0.899 |
| 1-year MACE, n (%) | 82 (22.0) | 33 (14.3) | 5.446 | 0.020 |
| Cardiac death | 26 (7.0) | 6 (2.6) | 5.419 | 0.020 |
| MI | 17 (4.6) | 8 (3.5) | 0.426 | 0.514 |
| TVR | 39 (10.5) | 19 (8.3) | 0.807 | 0.369 |
| All-cause death, n (%) | 30 (8.1) | 8 (3.5) | 5.055 | 0.025 |
| Definite/probable ST, n (%) | 8 (2.3) | 5 (2.6) | 0.000 | 1.000 |
STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; DAPT: Dual antiplatelet therapy; MACE: Major adverse cardiac events; MI: Myocardial infarction; TVR: Target vessel revascularization; ST: Stent thrombosis.
To further subanalyze both the groups, the proportions of 1-year cardiac death in the patients with a postprocedure TIMI flow grade <3 were significantly higher than those of the patients with a TIMI flow grade of 3 (STEMI group: 51.7% [15/29] vs. 4.1% [14/343], P < 0.001; NSTEMI group: 33.3% [3/9] vs 13.6% [3/221], P = 0.001). The results are presented in Figure 2.
Figure 2.
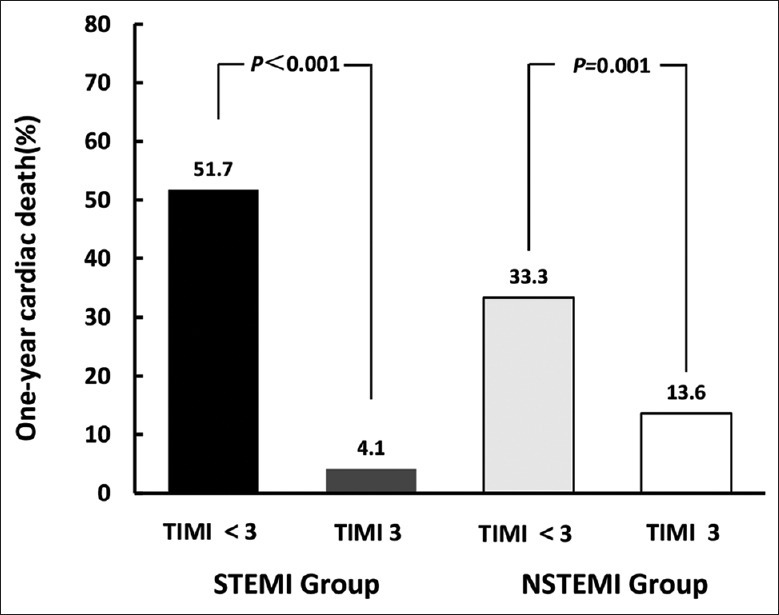
The results of subanalyze in STEMI and NSTEMI groups showed that the proportions of 1-year cardiac death in patients with post procedure TIMI flow grade <3 were significantly higher than that in the patients with post procedure TIMI flow grade of 3. STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; TIMI: Thrombolysis in myocardial infarction.
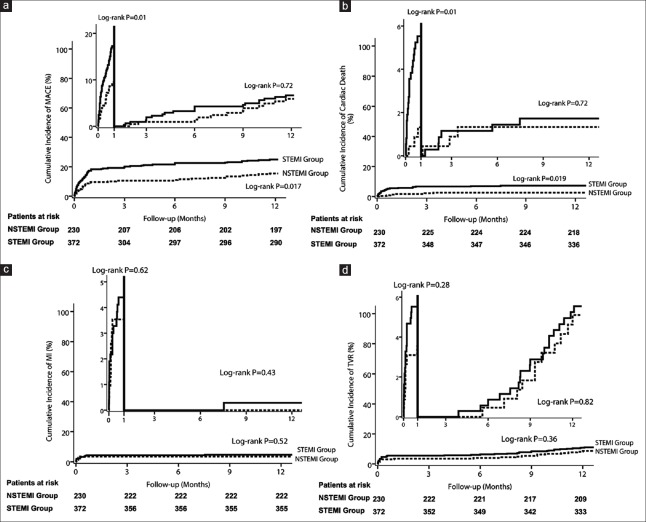
From the Kaplan-Meier analysis, there were significantly different proportions in the cardiac mortality (P = 0.017) and MACE (P = 0.019) between the STEMI and NSTEMI patients for 1 year, but no difference in MI and TVR (P = 0.52 and P = 0.36, respectively). Obviously, the landmark analysis clearly showed that the patients in STEMI group were associated with higher risks of MACE (16.7% vs. 9.1%, P = 0.009) and cardiac death (5.4% vs. 1.3%, P = 0.011) compared with NSTEMI patients at 1 month. Meanwhile, in patients with LM, the landmark analysis for incidences of MACE and cardiac death was similar between the STEMI and NSTEMI (5.4% vs. 5.2%, P = 0.720 and 1.6% vs. 1.3%, P = 0.720, respectively) in the intervals of 1–12 months. However, patients who were diagnosed with STEMI or NSTEMI had no significant difference in reinfarction (4.3% vs. 3.5%, P = 0.62 and 0.3% vs. 0.0%, P = 0.43, respectively) and TVR (5.4% vs. 3.5%, P = 0.28 and 5.1% vs. 4.8%, P = 0.82, respectively) in the intervals of 0–30 days as well as 30 days to 1 year. These results are presented in Figure 3.
Figure 3.
Kaplan-Meier curves showing the risks for MACE, including MACE (a), cardiac death (b), myocardial infarction (c) and TVR (d) for patients with STEMI and those with NSTEMI. Landmark analysis was further performed with a landmark of 1-month among patients in both groups who were events free at this time. MACE: Major adverse cardiac events; MI: Myocardial infarction; TVR: Target vessel revascularization; STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction.
The independent predictors for the 1-year MACE showed by multivariate analysis were different between the two groups, except for the variable of LVEF <35% and postprocedure TIMI flow grade of 3. For the STEMI patients, the independent predictors for the 1-year MACE included the variable of Killip class ≥III and IABP support. However, for the NSTEMI patients, the independent predictors were previous MI, ULMCA distal bifurcation, and 2-stent for distal ULMCA lesions (all of the variables had P < 0.05 [Table 4]).
Table 4.
Multivariable analysis showing independent predictors of the 1-year MACE for the two groups
| Variables | STEMI (n = 372) | NSTEMI (n = 230) | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Renal insufficiency | 1.24 (0.43–3.54) | 0.691 | 1.91 (0.94–3.85) | 0.068 |
| Previous MI | 1.73 (0.68–4.40) | 0.250 | 2.35 (1.02–5.42) | 0.045 |
| LVEF <35% | 3.06 (1.95–4.82) | <0.001 | 2.71 (1.16–6.36) | 0.016 |
| Killip class ≥III | 2.76 (1.39–5.49) | 0.004 | 1.09 (0.13–9.01) | 0.940 |
| LM distal bifurcation | 0.82 (0.45–1.50) | 0.516 | 2.25 (1.13–4.46) | 0.024 |
| Two-stent for distal LM lesions | 0.97 (0.55–1.69) | 0.914 | 2.41 (1.06–5.49) | 0.037 |
| Post-PCI TIMI flow grade >2 | 0.02 (0.01–0.04) | 0.018 | 0.03 (0.01–0.06) | <0.001 |
| IABP support | 1.79 (1.07–3.01) | 0.027 | 2.24 (0.94–5.35) | 0.071 |
HR: Hazard ratio; CI: Confidence interval; MACE: Major adverse cardiac events; STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; MI: Myocardial infarction; LVEF: Left ventricular ejection fraction; LM: Left main artery; PCI: Percutaneous coronary intervention; TIMI: Thrombolysis in myocardial infarction; IABP: Intra-aortic balloon pump.
DISCUSSION
The principal findings from this study are that the patients who underwent emergency PCI for ULMCA-STEMI still remained at a higher risk for in-hospital cardiac events than the NSTEMI patients. Moreover, this high-profile tendency was sustained over 1 month in the patients with ULMCA-STEMI. A successful PCI procedure and a culprit vessel with a TIMI flow grade of 3 might improve the 1-year outcomes in the STEMI and NSTEMI patients.
In previously published studies, NSTEMI patients with non-ULMCA lesions were more likely to have a higher prevalence of coronary artery disease risk factors than STEMI patients.[15,16] Compared to the NSTEMI patients in this study, the patients with ULMCA-STEMI who underwent primary PCI had significantly lower clinical risk factors, such as lower proportions of female patients, hypertension, and previous MI and PCI (all P < 0.05). Being a current smoker was related to the STEMI patients, whereas the mean age tended to be older among the NSTEMI patients. Those findings were similar to the results of the CADILLAC trial and Opera registry.[15,16,17] In addition, severe atherosclerotic changes, including distal bifurcation disease of the left main artery and chronic total occlusions in RCA, were more frequently observed in the NSTEMI patients than those in the patients with ULMCA-STEMI in this study. Meanwhile, 96 (25.8%) of 372 patients with ULMCA-STEMI in our study received thrombolytic therapy before the emergency PCI procedure. Similar to previous reports, patients with ULMCA-STEMI received more early invasive therapy and a shorter total ischemic time than that of the NSTEMI patients.[16,17] However, among the STEMI patients in this study, most of the patients had thrombus-occluded ULMCA lesions that were regarded as being in the infarct-related artery (TIMI flow grade of 0/1 flow in 66.9%), whereas in the NSTEMI patients, most of the ULMCA lesions were usually patent with a nonocclusive thrombus (TIMI grade flow of 2/3 in over 80%) at the baseline coronary angiography. There have been prominent and fatal changes in patients with ULMCA-STEMI after symptom onset. Consequently, the 1-year outcome in patients with ULMCA-STEMI was significantly worse than that of the NSTEMI patients in the study, especially regarding cardiac death at 1 year. This different result may be associated with the larger amount of damaged cardiac muscle in STEMI patients with ULMCA lesions after symptom onset. Therefore, there were significantly higher proportions of Killip class ≥III, cardiac arrest, and worse heart function in the patients with ULMCA-STEMI than those in the patients ULMCA-NSTEMI. The previous studies proved that the high mortality rate was caused by cardiogenic shock/pulmonary edema (amount to Killip class III or IV) and cardiac arrest. Cardiogenic shock or pulmonary edema and cardiac arrest are closely related to the extent and location of coronary lesions and are more common in patients with extensive coronary artery disease, ULMCA lesions, or a depressed LVEF.[3,4,5,6,9,10,11,12]
Upon further analysis for MACE, an obvious change was observed by our study and other registries.[3,4,10,11,12,13,14] For the patients with ULMCA-STEMI, a significantly high mortality rate was sustained in-hospital and at 1 month. However, the mortality rate tended to stabilize after 1 month, so excluding in-hospital and 1-month cardiac death, the proportions of the cardiac death and MACE were almost equal between the two groups by landmark analysis in this study (MACE: 5.4% vs. 5.2%, P = 0.72 and cardiac death: 1.6% vs. 1.3%, P = 0.72). On the other hand, to further subanalyze the cardiac death in both of the groups, the proportions of the 1-year cardiac death in the patients with a postprocedure TIMI flow grade <3 were significantly higher than those of patients with a TIMI flow grade of 3, particularly in the patients with ULMCA-STEMI (STEMI group: 51.7% vs. 4.1%, P < 0.001; NSTEMI group: 33.3% vs 13.6%, P = 0.001). Indirectly, a successful procedure might considerably reduce the MACE for patients with STEMI or NSTEMI.
Multivariate analysis provided definite results in an attempt to identify the differences between the two groups and intended to find which factors have the most important effect on the in-hospital and 1-year MACE. For the STEMI patients with ULMCA lesion, the independent predictors were almost associated with the amount of the infarcted muscle tissue after infarction attack, such as Killip class ≥III and IABP support. In the past decades, almost all of the studies about patients with ULMCA lesions confirm that the high incidence or mortality rate is attributed to cardiogenic shock/pulmonary edema and low left ventricular ejection. Commonly, IABP support was more likely to be used for patients who presented with hemodynamic instability.[4,6,10,14] Therefore, in the study, the IABP support was the predictor for the 1-year MACE for patients with STEMI (P = 0.03). Among the NSTEMI patients, the more independent predictors were related to the baseline risk factors, such as previous MI and ULMCA distal bifurcation lesions. Distal bifurcation lesions of the ULCMA appear to be associated with an increased risk for adverse events, such as side branch occlusion or restenosis. Obviously, low left ventricular ejection (LVEF <35%) was contributed to the high MACE for STEMI as well as NSTEMI patients. However, the successful revascularization (post-PCI TIMI flow grade of 3), which was an independent predictor for the two groups in this study, can decrease the rate of adverse events for patients with ULMCA and acute MI after emergency PCI. Likewise, the independent predictor of a post-PCI TIMI flow grade of 3 was more influential on the outcomes of patients with ULMCA-STEMI (STEMI: HR: 0.02, 95% CI: 0.01–0.04, P = 0.018; NSTEMI: HR: 0.03, 95% CI: 0.01–0.06, P < 0.001). The previous studies confirmed that a TIMI flow grade of 3 resulted in a 5-fold decrease in the annual mortality of these patients.[18,19]
Limitations
This was a retrospective nonrandomized study with a relatively small sample size and only the results of 1-year follow-up. Like all observational studies, the present study is prone to biases from its nonrandom assignment of exposures. The time span of the 602 patients who were analyzed in this article is almost 13 years. However, the PCI procedures of these 602 patients are different but had the same changes for the two groups in the corresponding period, thus having little effect on the result analysis. Follow-up angiography was not performed in all of the patients. Therefore, the true restenosis rate is unknown. We report a lower mortality rate, which is difficult to use to make meaningful comparisons with other studies because the observation index in the study is Killip class ≥III (included cardiogenic shock and pulmonary edema). Furthermore, some patients with ULMCA and AMI suffered cardiac death before admission and were not included in this study. Among the STEMI patients in this study, 96 (25.8%) of 372 patients received thrombolytic therapy before the PCI procedure. There was an important reason to explain the lower mortality rate in the present study because of the 33% patients with a pre-PCI TIMI flow grade 2/3 in the STEMI group. Despite these, the study of consecutive unselected patients from two experienced centers provides insight into emergency PCI for this high-risk group of patients.
In conclusion, emergency PCI appears to be technically feasible and a reasonable alternative to surgical revascularization for AMI patients with ULMCA disease. In our results, many differences in the characteristics of the patients with STEMI and NSTEMI distinctly affected the outcomes. The patients with ULMCA-STEMI still remained at a much higher risk for adverse events compared with the NSTEMI patients. If a successful PCI procedure was performed, the 1-year outcomes in those patients with acute MI and ULMCA lesions might improve. Ultimately, randomized controlled trials are needed to further elucidate the optimal treatment strategy.
Financial support and sponsorship
This work was supported by a grant from the Construction Program of National Clinical Priority Specialty.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Qiang Shi
REFERENCES
- 1.Gagnor A, Tomassini F, Romagnoli E, Infantino V, Rosa Brusin MC, Maria C, et al. Percutaneous left main coronary disease treatment without on-site surgery back-up in patients with acute coronary syndromes. Catheter Cardiovasc Interv. 2011;79:979–87. doi: 10.1002/ccd.23225. doi: 10.1002/ccd.23225. [DOI] [PubMed] [Google Scholar]
- 2.Lee MS, Bokhoor P, Park SJ, Kim YH, Stone GW, Sheiban I, et al. Unprotected left main coronary disease and ST-segment elevation myocardial infarction: A contemporary review and argument for percutaneous coronary intervention. JACC Cardiovasc Interv. 2010;3:791–5. doi: 10.1016/j.jcin.2010.06.005. doi: 10.1016/j.jcin.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Pedrazzini GB, Radovanovic D, Vassalli G, Sürder D, Moccetti T, Eberli F, et al. Primary percutaneous coronary intervention for unprotected left main disease in patients with acute ST-segment elevation myocardial infarction the AMIS (Acute myocardial infarction in Switzerland) plus registry experience. JACC Cardiovasc Interv. 2011;4:627–33. doi: 10.1016/j.jcin.2011.04.004. doi: 10.1016/j.jcin.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Pappalardo A, Mamas MA, Imola F, Ramazzotti V, Manzoli A, Prati F, et al. Percutaneous coronary intervention of unprotected left main coronary artery disease as culprit lesion in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2011;4:618–26. doi: 10.1016/j.jcin.2011.02.016. doi: 10.1016/j.jcin.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Izumikawa T, Sakamoto S, Takeshita S, Takahashi A, Saito S. Outcomes of primary percutaneous coronary intervention for acute myocardial infarction with unprotected left main coronary artery occlusion. Catheter Cardiovasc Interv. 2012;79:1111–6. doi: 10.1002/ccd.23396. doi: 10.1002/ccd.23396. [DOI] [PubMed] [Google Scholar]
- 6.Lee MS, Dahodwala MQ. Percutaneous coronary intervention for acute myocardial infarction due to unprotected left main coronary artery occlusion: Status update 2014. Catheter Cardiovasc Interv. 2015;85:416–20. doi: 10.1002/ccd.25704. doi: 10.1002/ccd.25704. [DOI] [PubMed] [Google Scholar]
- 7.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2 011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–122. doi: 10.1016/j.jacc.2011.08.007. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Section of Interventional Cardiology of Chinese Society of Cardiology of Chinese Medical Association, Specialty Committee on Prevention and Treatment of Thrombosis of Chinese College of Cardiovascular Physicians, Editorial Board of Chinese Journal of Cardiology. Chinese guideline for percutaneous coronary intervention (2016) (in Chinese) Chin J Cardiol. 2016;44:382–400. doi: 10.3760/cma.j.issn.0253-3758.2016.05.006. doi: 10.3760/cma.j.issn.0253.3758.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 9.De Luca G, Suryapranata H, Thomas K, van 't Hof AW, de Boer MJ, Hoorntje JC, et al. Outcome in patients treated with primary angioplasty for acute myocardial infarction due to left main coronary artery occlusion. Am J Cardiol. 2003;91:235–8. doi: 10.1016/s0002-9149(02)03115-6. doi: 10.1016/S0002-9149(02)03115-6. [DOI] [PubMed] [Google Scholar]
- 10.Hurtado J, Pinar Bermúdez E, Redondo B, Lacunza Ruiz J, Gimeno Blanes JR, García de Lara J, et al. Emergency percutaneous coronary intervention in unprotected left main coronary arteries. Predictors of mortality and impact of cardiogenic shock. Rev Esp Cardiol. 2009;62:1118–24. doi: 10.1016/s1885-5857(09)73326-2. doi: 10.1016/S1885-5857(09)73326-2. [DOI] [PubMed] [Google Scholar]
- 11.Bonello L, Com O, Gil JM, Curjol J, Gelisse R, Sbragia P, et al. Emergency percutaneous angioplasty of unprotected left main coronary artery in the setting of myocardial infarction: Experience of a low volume center without surgical back up. Int J Cardiol. 2006;112:406–8. doi: 10.1016/j.ijcard.2006.07.007. doi: 10.1016/j.ijcard.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Pepe M, Napodano M, Tarantini G, Fraccaro C, Cutolo A, Peluso D, et al. Percutaneous coronary intervention for unprotected left main disease in very high risk patients: Safety of drug-eluting stents. Heart Vessels. 2011;26:17–24. doi: 10.1007/s00380-010-0027-y. doi: 10.1007/s00380-010-0027-y. [DOI] [PubMed] [Google Scholar]
- 13.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation. 2007;115:2344–51. doi: 10.1161/CIRCULATIONAHA.106.685313. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 14.Vis MM, Beijk MA, Grundeken MJ, Baan J, Jr, Koch KT, Wykrzykowska JJ. A systematic review and meta-analysis on primary percutaneous coronary intervention of an unprotected left main coronary artery culprit lesion in the setting of acute myocardial infarction. JACC Cardiovasc Interv. 2013;6:317–24. doi: 10.1016/j.jcin.2012.10.020. doi: 10.1016/j.jcin.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 15.Montalescot G, Dallongeville J, Van Belle E, Rouanet S, Baulac C, Degrandsart A, et al. STEMI and NSTEMI: Are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry) Eur Heart J. 2007;28:1409–17. doi: 10.1093/eurheartj/ehm031. doi: 10.1093/eurheartj/ehm031. [DOI] [PubMed] [Google Scholar]
- 16.Steg PG, Goldberg RJ, Gore JM, Fox KA, Eagle KA, Flather MD, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the global registry of acute coronary events (GRACE) Am J Cardiol. 2002;90:358–63. doi: 10.1016/s0002-9149(02)02489-x. doi: 10.1016/S0002-9149(02)02489-X. [DOI] [PubMed] [Google Scholar]
- 17.Cox DA, Stone GW, Grines CL, Stuckey T, Zimetbaum PJ, Tcheng JE, et al. Comparative early and late outcomes after primary percutaneous coronary intervention in ST-segment elevation and non-ST-segment elevation acute myocardial infarction (from the CADILLAC trial) Am J Cardiol. 2006;98:331–7. doi: 10.1016/j.amjcard.2006.01.102. doi: 10.1016/j.amjcard.2006.01.102. [DOI] [PubMed] [Google Scholar]
- 18.Sadowski M, Gutkowski W, Janion-Sadowska A, Gąsior M, Gierlotka M, Janion M, et al. Acute myocardial infarction due to left main coronary artery disease: A large multicenter national registry. Cardiol J. 2013;20:190–6. doi: 10.5603/CJ.2013.0033. doi: 10.5603/CJ.2013.0033. [DOI] [PubMed] [Google Scholar]
- 19.Baek JY, Seo SM, Park HJ, Kim PJ, Park MW, Koh YS, et al. Clinical outcomes and predictors of unprotected left main stem culprit lesions in patients with acute ST segment elevation myocardial infarction. Catheter Cardiovasc Interv. 2014;83:E243–50. doi: 10.1002/ccd.23420. doi: 10.1002/ccd.23420. [DOI] [PubMed] [Google Scholar]