To the Editor: Submucosal nasopharyngeal carcinoma (NPC) is very uncommon, comprising only 8.8% of all tumors in the nasopharynx.[1] However, given difficulties in tissue sampling, the pathological diagnosis of a submucosal growth pattern in NPC is not easy to obtain. Here, we describe the successful clinical application of endonasopharyngeal ultrasound-guided transnasopharyngeal needle aspiration (ENUS-TNNA) with a real-time ultrasonic bronchoscope for the diagnosis of a submucosal growth type of nasopharyngeal neoplasms.
A 50-year-old man with an unexplained cervical mass was referred to our hospital for further treatment. Magnetic resonance imaging showed different degrees of soft-tissue thickness of the bilateral wall, especially the right sidewall, and top and posterior wall of the nasopharynx as well as enlarged cervical nodes were identified [Figure 1a and 1b]. Nasopharyngoscopy only revealed thickening of the right torus [Figure 1c]. To achieve a definite diagnosis, we attempted to perform ENUS-TNNA with a real-time ultrasonic bronchoscope to obtain specimens from submucosal lesions of the nasopharynx for histopathological examination.
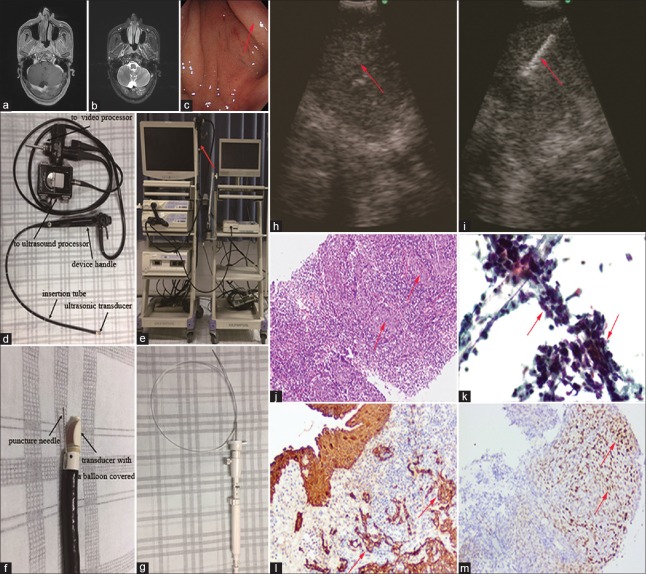
Figure 1.
Representative images of the patient and apparatuses used for the procedure of ENUS-TNNA. (a and b) Magnetic resonance imaging of the submucosal nasopharyngeal neoplasms ([a] T1-weighted image, [b] T2-weighted image). (c) Nasopharyngoscopy revealed no remarkable abnormalities with the exception of thickening of the right torus (arrow). (d) Parts of an ultrasonic bronchoscope. (e) An ultrasonic bronchoscope (arrow) was linked to the video processor (left) and ultrasound processor (right). (f) Distal end of the ultrasonic bronchoscope with an electronic convex array ultrasonic transducer covered by a water-inflatable balloon and a 21-gauge needle introduced through the biopsy channel. (g) A dedicated 21-gauge puncture needle used during the procedure. (h) An abnormally heterogeneous low echo next to the right sidewall of the nasopharynx was detected (arrow). (i) A 21-gauge needle penetrating into the targeted submucosal lesion (arrow). (j) Histological findings indicate clusters of epithelial cells with slightly stained vesicular nuclei among small lymphocytes (arrows, Hematoxylin and eosin staining, ×100). (k) Cytological findings depicting atypical epithelial cells with large irregular nuclei and minimal cytoplasm (arrows, Papanicolaou staining, ×200). (l and m) Immunohistochemistry showed positive staining for CK (arrows, ×200) and EBER (arrows, ×200). ENUS-TNNA: Endonasopharyngeal ultrasound-guided transnasopharyngeal needle aspiration. CK: Cytokeratin; EBER: Epstein-Barr virus-encoded small RNAs.
A linear array ultrasonic bronchoscope (BF-UC260F-OL8, Olympus Ltd., Tokyo, Japan) was employed for the puncture procedure [Figure 1d]. The ultrasonic bronchoscope was linked to an ultrasound processor (EU-C2000, Olympus Ltd., Tokyo, Japan) and video processor (CV-260SL, Olympus Ltd., Tokyo, Japan) [Figure 1e]. A water-inflatable balloon (MAJ-1351, Olympus Ltd., Tokyo, Japan) was mounted around the transducer for better ultrasonic coupling with the nasopharyngeal wall [Figure 1f].
The ultrasonic bronchoscope was then inserted to the nasopharyngeal cavity through the right nasal cavity, and target lesions were then examined by endonasopharyngeal ultrasound. Transnasopharyngeal needle biopsies were performed with a dedicated 21-gauge needle (NA-201SX-4021, Olympus Ltd., Tokyo, Japan) introduced through the biopsy channel of the endoscope [Figure 1g]. Before puncturing, color power Doppler ultrasound was used to exclude the presence of vessels within the planned puncture area. Under guidance of real-time ultrasound, an abnormally heterogeneous low echo next to the right sidewall of the nasopharynx was detected, and the puncture needle was then placed into the target lesion [Figure 1h and 1i]. Suction was added with a syringe, and the needle was moved back and forth inside the lesion. The obtained tissue samples were sent for pathological and cytological examination. Finally, pathological examination revealed nonkeratinizing squamous cell carcinoma [Figure 1j–1m].
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), using a linear array ultrasonic bronchoscope, is a safe, effective, and less invasive tool for the diagnosis and staging of lung cancer. Inspired by the great success of EBUS-TBNA in lung cancer, we innovatively and successfully performed ENUS-TNNA with an ultrasonic bronchoscope in a patient with the clinical diagnosis of NPC under the normal nasopharyngeal mucosa. Through careful literature review, the technique of endoscopic ultrasonography-guided fine-needle aspiration through the nasopharynx has been previously reported in 2015.[2] In that report, the authors successfully performed fine-needle aspiration of a retropharyngeal lymph node guided by endoscopic ultrasonography in a patient with suspected recurrence of NPC. Unlike that report, we here describe the successful and unique application of ENUS-TNNA for the diagnosis of a primary submucosal nasopharyngeal lesion. We provided a new method of targeted biopsy for the diagnosis of NPC under the normal mucosa.
Compared with traditional biopsy methods, the advantages of the ENUS-TNNA procedure are as follows. First, ENUS-TNNA provides better outcomes in terms of reduced trauma and blood loss due to its tiny biopsy site with the use of a dedicated needle, and the function of integrated color power Doppler ultrasound also avoids unintended punctures of vessels between the wall of the nasopharynx and lesions. In addition, under real-time ultrasound guidance, it is easier to accurately target a biopsy compared with conventional methods, and the operator could choose the best puncture sites and puncture direction at any time if necessary. Finally, specimens obtained during the procedure are suitable for histological examination with the use of a 21-gauge needle, and liquid-based cytology also assists in the identification of tumor cells.
ENUS-TNNA is a novel and minimally invasive technique to provide a diagnosis of a submucosal growth type of nasopharyngeal neoplasms. More experience and further studies are needed to evaluate the validity of this technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yuan-Yuan Ji
REFERENCES
- 1.Loh KS, Petersson F. Nonexophytic nasopharyngeal carcinoma: High frequency of advanced lymph node and distant metastasis. Otolaryngol Head Neck Surg. 2011;145:594–8. doi: 10.1177/0194599811411141. doi: 10.1177/0194599811411141. [DOI] [PubMed] [Google Scholar]
- 2.Li JJ, He LJ, Luo GY, Liu LZ, Huang XX, Pan K, et al. Fine-needle aspiration of a retropharyngeal lymph node guided by endoscopic ultrasonography. Endoscopy. 2015;47(Suppl 1 UCTN):E449–50. doi: 10.1055/s-0034-1392652. doi: 10.1055/s-0034-1392652. [DOI] [PubMed] [Google Scholar]