Highlights
-
•
We report 2 patients with pontine infarcts showing transient conjugate eye deviation.
-
•
Conjugate eye deviation resolved within a few days in both patients.
-
•
Small restricted dorsomedial pontine lesions can produce conjugate eye deviation.
Keywords: Conjugate eye deviation, Dorsal pontine infarction, Gaze palsy
1. Introduction
Conjugate eye deviation (CED) typically results from a hemispheric stroke involving the frontal eye field [1,2]. Although brainstem lesions can produce conjugate eye deviation, few studies have correlated the characteristics of conjugate eye deviation with the localization of brainstem lesions. Herein, we report 2 patients with pontine infarction who present with transient CED followed by contralateral gaze palsy.
2. Case 1
A 91-year-old woman with hypertension and dyslipidemia suddenly developed nausea, vomiting and unsteadiness after lunch. She was soon taken to our hospital by ambulance. Her blood pressure was 136/54 mmHg, her body temperature was 36.0 °C and her pulse was 67/min and regular. Neurological findings were unremarkable except for conjugate deviation of the eyes to the left and horizontal gaze palsy to the right. Diffusion-weighted magnetic resonance images (DWI) showed the high-intensity areas in the right paramedian pontine region extending from the dorsal to ventral regions (Fig. 1A, B). The patient was treated with argatroban and clopidogrel. On day 4, the CED disappeared but the horizontal gaze palsy to the right remained. The horizontal gaze palsy completely improved 8 days after the onset of symptoms.
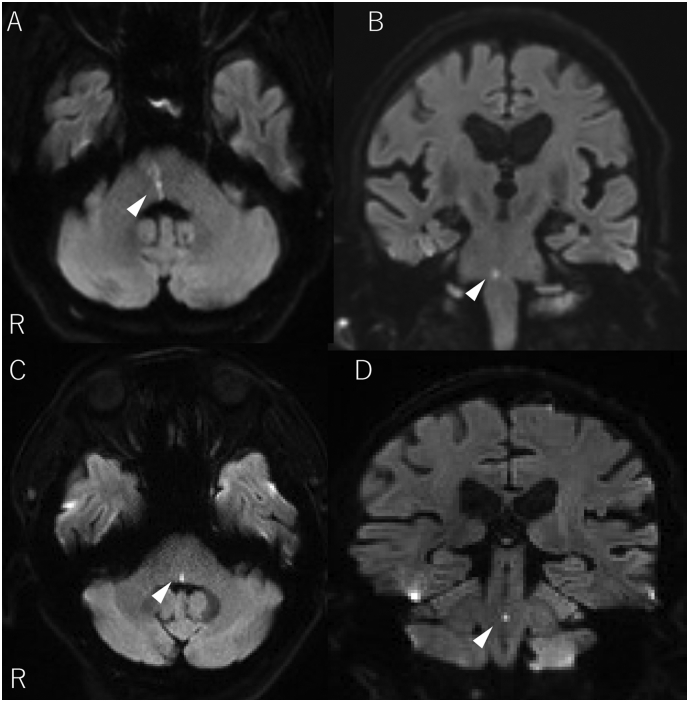
Fig. 1.
Diffusion-weighted MRI findings of the patients.
High signal intensities are observed in the right paramedian pontine region extending from the ventral to dorsal parts in Case 1 (A, B, arrowheads) and the left dorsomedial pontine tegmentum in Case 2 (C, D, arrowheads).
3. Case 2
A 77-year-old man with diabetes mellitus and hypertension developed an unsteady gait upon awakening, followed by diplopia 3 days later. The next day, he presented to our hospital. Initial examinations showed a blood pressure of 164/84 mmHg, a body temperature of 36.3 °C and a pulse rate of 73 /min with a regular rhythm. Neurological findings showed a conjugate deviation to the right, a horizontal gaze palsy to the left (Supplementary video 1) and truncal ataxia. DWI showed a small, high-intensity area restricted to the left dorsomedial pontine tegmentum (Fig. 1C, D). The patient received argatroban and clopidogrel. Four days after starting treatment, the CED disappeared. Two weeks after the onset of symptoms, the horizontal gaze palsy resolved.
There have been 6 case reports of CED resulting from a brainstem infarction (5 paramedian pons, 1; lateral medulla). The CED was temporary (4–20 days) in all patients (Table 1) [1,[3], [4], [5]]. Except for Patient 2 (the medulla lesion) [1], the horizontal gaze palsy opposite to the CED was observed in all patients. The CED or horizontal gaze palsy occurs due to a lesion in either the contralateral hemisphere including the frontal eye field, the frontopontine pathways or the ipsilateral pons [6]. Disruption of the olivary projections to the contralateral vestibulocerebellum was suggested to produce CED ipsilateral to the dorsolateral medulla lesion [1]. There is controversy regarding the responsible lesion for CED in the pons, but the involvement of the abducens nucleus and the paramedian pontine reticular formation (PPRF) have been implicated. In our two patients, the horizontal gaze palsy to the opposite side improved after the improvement of the CED. Although the lesion in Case 1, which extended from the paramedian dorsal to ventral pons, was larger than that in Case 2, which was restricted to the dorsal pons, we think a small dorsomedial tegmentum pontine lesion disrupted the tracts of the horizontal eye movement including the PPRF, causing CED. In hemispheric stroke patients, CED, especially CED to the left, indicated poor short-term mortality and disability [2]. This is in contrast with a favorable outcome for patients showing CED due to brainstem lesions, in whom CED recovered within a few days to three weeks (Table 1).
Table 1.
Characteristics of patients with conjugate eye deviation due to brainstem infarction.
| Author | Patient No. | Age (y)/sex | Risk factors | Clinical presentation | Duration of CED (d) | MRI lesions |
|---|---|---|---|---|---|---|
| Hashiguchi et al. [4] | 1 | 80/M | HT | Vertigo, CED to R, L HGP | 15 | L paramedian pontine tegmentum |
| Solomon et al. [1] | 2 | 40/F | HT | Vertigo, headache, CED to L without HGP, postural instability | 6 | L upper dorsolateral medulla |
| Hamasaki et al. [3] | 3 | 76/M | – | CED to R, L HGP | 14 | L paramedian pontine tegmentum |
| Uemura et al. [5] | 4 | 75/M | HT, OCI, smoking | CED to R, L HGP | 20 | L paramedian pontine tegmentum |
| Case 1a | 5 | 91/F | HT, dyslipidemia | CED to L, R HGP | 4 | R paramedian dorsal to ventral pontine tegmentum |
| Case 2a | 6 | 77/M | HT, DM | CED to R, L HGP, truncal ataxia | 4 | L dorsomedial pontine tegmentum |
2 patients from the present study CED = conjugate eye deviation; HGP = horizontal gaze palsy; HT = hypertension; OCI = old cerebral infarction; DM = diabetes mellitus.
We showed that dorsomedial tegmentum pontine lesions produced transient CED followed by contralateral gaze palsy. We should consider the possibility that brainstem lesions can cause CED, especially when accompanied by symptoms suggesting brainstem involvement, such as vomiting, vertigo and truncal ataxia, without a disturbance in consciousness.
Conflict of interest
The authors declare that they have no potential conflicts of interest in relation to this article.
Financial disclosures
None.
The following are the supplementary data related to this article.
The patient (Case 2) showed conjugate eye deviation to the right on admission.
References
- 1.Solomon D., Galetta S.L., Liu G.T. Possible mechanisms for horizontal gaze deviation and lateropulsion in the lateral medullary syndrome. J. Neuroophthalmol. 1995;15 [PubMed] [Google Scholar]
- 2.Tijssen C.C., Schulte B.P., Leyten A.C. Prognostic significance of conjugate eye deviation in stroke patients. Stroke. 1991;22(2):200. doi: 10.1161/01.str.22.2.200. [DOI] [PubMed] [Google Scholar]
- 3.Hamasaki S., Motomura M., Koga H. Persistent lateral gaze palsy and abducens nerve palsy due to pontine infarction. Rinsho Shinkeigaku. 1998;38:344–346. [PubMed] [Google Scholar]
- 4.Hashiguchi S., Ogasawara N., Igaki T. Persistent isolated abducens nerve palsy from pontine infarction confirmed by gadolinium-DTPA enhanced MRI. Rinsho Shinkeigaku. 1994;34:72–76. [PubMed] [Google Scholar]
- 5.Uemura J., Shibazaki K., Inoue T. A case of pontine infarction presenting with conjugate deviation and unilateral conjugate gaze palsy. Rinsho Shinkeigaku. 2007;47:231–233. [PubMed] [Google Scholar]
- 6.Karatas M. Internuclear and supranuclear disorders of eye movements: clinical features and causes. Eur. J. Neurol. 2009;16:1265–1277. doi: 10.1111/j.1468-1331.2009.02779.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient (Case 2) showed conjugate eye deviation to the right on admission.