Abstract
Atrial fibrillation is common in hypertrophic cardiomyopathy with a prevalence of 22-32 %. The impact of atrial fibrillation on overall survival, left ventricular function, thromboembolic stroke and quality of life is crucial. This review enlightens incidence, pathophysiology, and clinical symptoms. Early recognition of atrial fibrillation is essential. Monitoring methods for early detection are described. Finally effective therapy options are discussed including oral anticoagulation and the role of interventional catheter-based ablation in the treatment of atrial fibrillation in HCM patients.
Keywords: Hypertrophic Cardiomyopathy, Atrial Fibrillation, Device Therapy, Implantable Cardioverter Defibrillator, Epidemiology
Introduction
It is well known, that rhythm disorders play a pivotal role in patients with hypertrophic cardiomyopathy (HCM) and that ventricular arrhythmias are the major course of sudden cardiac death especially in young HCM patients[1]–[5]. Nevertheless, up to date the impact of atrial fibrillation (AF) in these patients is not well understood and in most cases detected by chance as a cause of heart failure or stroke[6]–[7]. Early recognition and treatment of AF is essential to improve both, quality of life and clinical outcome. This review article gives an update about incidence, implication, diagnosis and therapy of atrial fibrillation in HCM.
Incidence of AF in HCM
HCM is the most frequent monogenetic cardiomyopathy with a prevalence of 1:500[8] Depending on the localization and degree of hypertrophy, HCM patients may present with various pathoanatomic and pathophysiologic anomalies, such as left ventricular outflow tract obstruction, mitral regurgitation, diastolic dysfunction and/or myocardial ischemia and fibrosis [Figure 1] and [Figure 2]. AF is the most frequent arrhythmia in HCM. Its prevalence depends on the severity of the disease with 22 % in a general cohort[7] and up to 32% in a cohort prior to ICD and pacemaker implantation[9] [Table 1]. The incidence for de-novo AF in a general HCM cohort is about 2% per year[7]–[10].
Figure 1. Left atrial enlargement in Hypertrophic Cardiomyopathy.
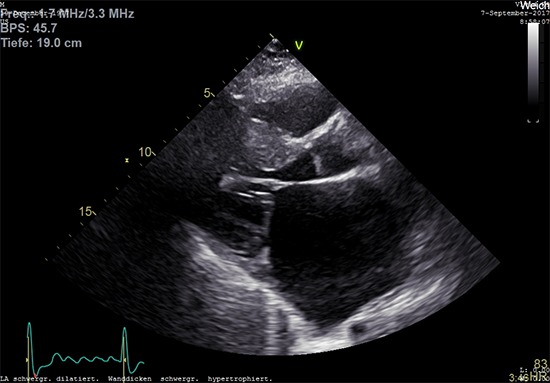
Two-dimensional transthoracic echocardiography in a 40-year-old male patient with HCM and persistent atrial fibrillation showing an enlarged left atrium with LVOT hypertrophy (IVS 20mm).
Figure 2. Mitral regurgitation in Hypertrophic cardiomyopathy.
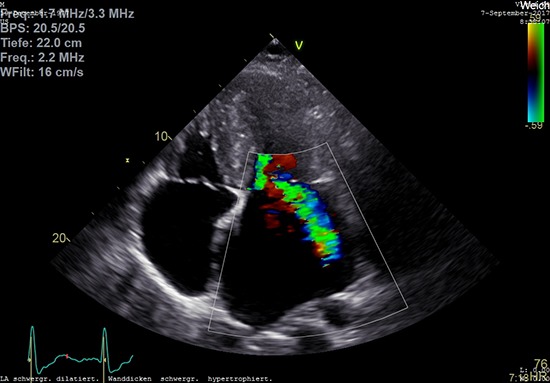
Two-dimensional transthoracic echocardiography in the same 40-year-old male patient with HCM and persistent atrial fibrillation showing an enlarged left atrium and significant eccentric mitral regurgitation
Table 1. Prevalence of Atrial fibrillation and stroke in non-referral bias HCM cohorts.
| Author | Year | Number | Prevalence | Prevalence of |
|---|---|---|---|---|
| of patients | of AF | Stroke or TIA | ||
| Masri et al[18] | 2015 | 1005 | 19% | 3% |
| Guttmann[58] | 2015 | 4815 | 12.5% | 3.6% |
| Siontis[26] | 2014 | 3673 | 18% | n.a. |
| Tian[6] | 2013 | 654 | 24% | n.a. |
| Maron[33] | 2009 | 900 | 21% | 6% |
| Olivotto[7] | 2001 | 480 | 22% | 21% for patients with AF , |
| 2.6% for patients without AF |
Although the majority of HCM patients are asymptomatic, some develop heart failure, present with palpitations or suffer from stroke[10]–[13] [Table 1]. In all these devastating conditions, AF plays a key role[6].
Pathophysiology
Regular atrial contraction is necessary for left ventricular filling and function especially in HCM patients with impaired diastolic function[14]. In this context, the presence of atrial arrhythmia impairs left ventricular outflow obstruction, mitral regurgitation, diastolic dysfunction and myocardial ischemia[14].
The interaction between AF and the pathophysiological and -anatomical changes in HCM is complex. It is known that atrial fibrillation reflects both, the trigger and the result of morphological and physiological changes in cardiac anatomy[5]. In HCM multiple changes may trigger atrial fibrillation [Figure 3]. As demonstrated in MRI scans, myocardial fibrosis disturbs a regular electrical activity leading to enhanced ectopy in atrial and ventricular myocardium[15]. Thick myocardium with reduced diastolic relaxation leads to higher left ventricular pressure resulting in elevated left atrial pressure. This process may induce atrial stress ultimately leading to atrial enlargement and the development of AF. In some HCM patients with LVOT obstruction, mitral valve anatomy and function are altered leading to valve insufficiency that further enhances the left atrial volume[16]. Mitral regurgitation is present in up to 30% in HCM patients[16].
Figure 3. Pathophysiology of Atrial Fibrillation in Hypertrophic Cardiomyopathy.
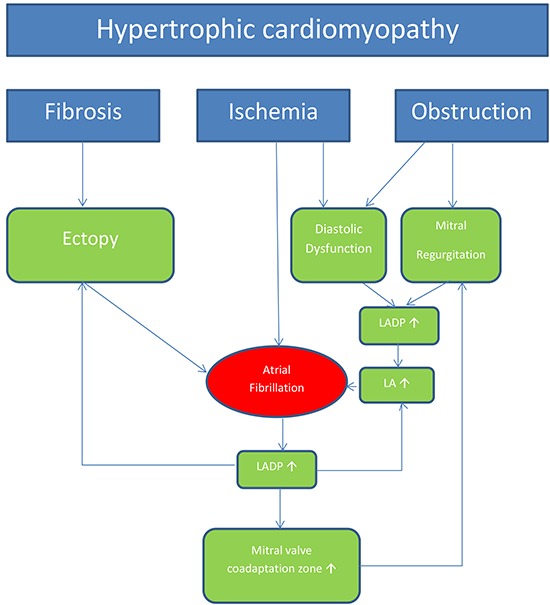
LA: left atrial diameter, LADP: left atrial diastolic pressure 10
For many years, a high LVOT gradient was the key determinant in the diagnostic and therapeutic approach in HCM. However, recent studies have shown that additional parameter should be used to predict patient´s outcome: On a stepwise multivariate survival analysis, exercise capacity during stress echocardiography, abnormal heart rate recovery, and atrial fibrillation independently predicted patient´s outcome, whereas the LVOT gradient was not associated with atrial fibrillation and had no impact on the outcome[17]-[19].
Clinical Symptoms and Implications
Maron et al. defined three distinctive modes of death in HCM: sudden and unexpected death (51%), progressive heart failure (36%), and HCM-related stroke associated with AF (13%)[20]. Sudden cardiac death is most common in young patients, whereas heart failure and stroke-related death occur more frequently in midlife and beyond[10].
The clinical presentation of HCM patients with AF is unspecific: some patients present with signs of heart failure (dyspnoea, hypotension, pulmonary edema, chest pain), arrhythmia (palpitations, presyncope, syncope) and/or stroke. However, many patients with AF do not have any symptoms and the AF is classified as subclinical.In our own experience, the majority of HCM patients with a cardiacrhythm management device and de-novo AF were free from clinical symptoms (88%)[9]. The incidence of subclinical AF was higher in this HCM cohort compared to other patients treated with cardiacrhythm management (CRM) devices such as patients with sick sinussyndrome[21], atrioventricular block[22],[23] or stroke[23],[24]. Only patients with ischemic cardiomyopathy and an ICD had an equivalent high incidence of de-novo AF[25].
The impact of AF on survival of HCM patients is discussed controversially[6],[26]. Olivotto et al. reported a HCM-related mortality of 1.7% per year and confirmed AF as an independent risk factor for cardiovascular death, heart failure, and stroke[6],[22]. Siontiset al. demonstrated that AF is associated with a nearly 50% increased relative risk for overall mortality[26]. However, in this study AF didnot affect cardiac mortality[26]. One trial identified just paroxysmal AF but not permanent AF as an independent determinant of outcome, including the risk of HCM-related death[27], which was explained by the fact that paroxysmal AF in HCM patients may be frequently subclinical and therefore untreated. Of note, HCM patients with paroxysmal AF demonstrate exercise intolerance despite being in sinus rhythm at the time of exercise testing[28].
Interestingly, in a few case reports atrial fibrillation was anticipated to trigger sustained ventricular tachycardia and sudden cardiac death in HCM patients[29],[30]. Nevertheless, as valid data are missing atrial fibrillation is not classified as a major risk factor for sudden death in the current guidelines[5].
Stroke and HCM
Patients with HCM have a high risk for stroke or thromboembolic events. Stroke is an important determinant of mortality, especially in older patients. Since symptomatic and subclinical AF is the main cause of thromboembolic stroke, early detection of AF is crucial for further therapy, particularly with regard to a required oral anticoagulation. Recently published reports have suspected the left ventricular apex as an alternative source of thromboembolic complications in HCM patients[31],[32]. In unselected HCM patients, stroke and peripheral embolism occur with a prevalence rate of 6% and an incidence of 0.8% per year[7],[33] [Table 1]. However, in our own cohort of HCM patients who received a CRM device a much higher incidence of thromboembolic stroke could be detected (18%)[9].
Echocardiography and magnetic resonance tomography
Echocardiography is the method of choice for HCM diagnosis. However, so far, no specific echocardiographic risk factor for the development of AF has been identified in these patients. A variety of pathologic alterations associated with HCM, such as diastolic dysfunction, left atrial enlargement, myocardial fibrosis, and myocardial ischemia, may promote the development of AF[17],[35],[36] [Figure 1] and [Figure 2]. Some studies reported that left atrial dilation was related to an adverse outcome[6],[37]. Magnetic resonance tomography can add optional information, especially regarding the fibrotic burden[38]. Nevertheless, the extent of late gadolinium enhancement was inferior to the left atrial size as the strongest determinant for predicting AF prevalence[38]. Diastolic dysfunction was also confirmed as a predictor for AF in this MR study[38].
Treatment
Therapeutic options for HCM patients with AF do not differ from those without HCM. Early detection and therapy of AF are essential in the management of a timely oral anticoagulation even after one single episode of AF and an appropriate rhythm or rate control using medical and interventional options[39],[40].
Rhythm control strategy
We strongly suggest attempting a rhythm control strategy for every symptomatic patient with newly detected AF. Even though no data are available comparing a rhythm control versus rate control strategy in HCM, maintaining sinus rhythm as long as possible and restoring sinus rhythm as soon as possible is beneficial for both: control of symptoms and improvement of hemodynamics[40].
In symptomatic patients, we prefer a rapid electrical cardioversion to restore sinus rhythm according to the 2014 AHA/ACC/HRS and the 2016 ESC guidelines[5],[41]. Although, medical cardioversion is an alternative to electrical cardioversion, no controlled trials exist investigating different drugs in this regard. Suggested drugs to restore and maintain sinus rhythm are amiodarone, sotalol, disopyramide and dofetilide[5].
Amiodarone is considered as the best option for rhythm control because it is safe and effective in HCM patients[40]. For other antiarrhythmic drugs, there are no valid data available. We do not recommend class I antiarrhythmic agents (flecainide, disopyramide), sotalol, or dronedarone in HCM, because of their possible side effects like ventricular arrhythmia, atrioventricular conduction delay, QTc prolongation (sotalol) or anticholinergic syndromes (disopyramide) [40]. Dofetilide as a class III antiarrhythmic agent and an alternative for amiodarone is not available in Europe and Australia.
In all cases of HCM with AF a Beta-blocker is the basis of therapy[5]. Beta-blockers modulate sympathetic activity and improve ventricular contractility, so LVOT gradient lowers, diastolic dysfunction is improved, and the incidence of supraventricular and ventricular arrhythmia is reduced[40].
Patients with recurrent AF may benefit from interventional catheterbased radiofrequency ablation, but randomized controlled trials are missing.
Many studies confirmed that catheter ablation is safe and effective for patients with HCM. However, the overall success rate is lower and usually more ablation procedures are required to achieve sinus rhythm compared with patients without HCM[42] [Table 2]. Santangeli et al. investigated the role of pulmonal vein isolation in patients with AF and HCM (28% paroxysmal AF). In this study, the success rate was low and additional procedures were needed. After a median followup of 42 months, only 49% of the patients remained free from AF/atrial tachycardia. All patients needed an additional procedure, in which pulmonal vein antrum and posterior wall remained isolated in 82% of the cases, but extra-PV triggers were documented in all patients[43].
Table 2. Trials investigating Catheter Ablation in HCM patients with AF.
In a recent metaanalysis including 15 studies, single-procedure freedom from atrial arrhythmia at the latest follow-up was 45 %[44]. With multiple procedures, the final overall success rate was calculated with 66 %[44]. The final success rate was much higher in patients with paroxysmal AF with 72 % compared with only 47 % in persistent AF[44]. In many cases, even after successful ablation, antiarrhythmic therapy is required to maintain sinus rhythm[44]. Without antiarrhythmic drugs, the single-procedure success rate at latest followup was 32.9% and after multiple procedures 50.4%[44]. The risk for HCM patients to experience a relapse after a single catheter ablation therapy is about 2 times higher compared to patients without HCM[42],[45],[46]. Left atrial dilation, mitral regurgitation, atrial fibrosis, left outflow tract obstruction, and persistent AF are linked to lower success rates of catheter ablation[42],[47],[48]. The best strategy for the ablation procedure (pulmonal vein isolation vs. pulmonal vein isolation combined with atrial modification) and the optimal energy force (radiofrequency ablation vs. cryoablation) is under discussion. Adding left atrial linear ablation to pulmonal vein isolation increased the success rate in one single center study[49]. Kuck et al. demonstrated that cryoablation is as safe and as effective as radiofrequency ablation in a general AF cohort[50]. In contrast to this observation, the success rate of cryoablation in HCM was low, but this trial observed only four HCM patients with AF[51].
Considering the present data, we do not recommend surgical ablation as first line or stand-alone ablation strategy. Compared to surgical ablation strategies the observed complication rate for catheter ablation procedures in HCM was low[42] with a higher success rate[52]. However, the Maze procedure, with concomitant septal myectomy or mitral valve replacement if indicated, appears to be feasible in patients with hypertrophic cardiomyopathy and refractory atrial fibrillation[53],[54].
Rate Control Strategy
Until now, no data exist investigating a rate control strategy in patients with permanent AF in HCM. In line with other studies investigating a rate control strategy, we suggest beta-blockers or calcium antagonists for rate control, if a rhythm control strategy fails. Positive inotropic drugs such as digitalis are contraindicated[55]. AVnodal ablation is a final option to avoid high heart rate in patients without sufficient rate control[56].
Oral Anticoagulation
Maron et al. proved in a large cohort analysis of 900 HCM patients, that the cumulative incidence of stroke and peripheral embolism among patients with atrial fibrillation was significantly higher in non-anticoagulated patients compared with patients receiving warfarin[33]. New data are in line with these observations and show a 1.0% yearly risk for stroke and embolic events[12].
In contrast to patients without HCM, we do not have a validated risk score to define patients who benefit from oral anticoagulation. Even if the CHA₂DS₂-VASc Score is zero, patients with HCM are at high risk for embolic events. Parameters, such as left atrial size, mitral regurgitation, and left ventricular outflow gradient may contribute to a higher stroke risk, but do not contribute to the CHA₂DS₂-VASc Score[12].
Patients with HCM suffering from stroke need careful screening for AF because 7.4 % of these patients have newly documented at AF the time of the event and 14.7 % present AF during evaluation after stroke[12]. Repetitive ECG monitoring is mandatory. However, implantable loop recorders are superior to conventional follow-up and can detect atrial fibrillation in so-called cryptogenic stroke[24].
Although long-term studies with novel oral anticoagulants are missing to date, few case reports exist showing direct oral anticoagulants to be as effective and save in HCM patients[31],[57].
In conclusion, we recommend lifelong oral anticoagulation for every HCM patient with documented atrial fibrillation independent of individual CHA₂DS₂-VASc Score to reduce the risk of stroke[33].
Conclusion:
Atrial fibrillation is a major complication and reason for worse outcome in patients with HCM. Close and thorough investigations using ECG, Holter- ECG and implantable loop recorders, are extremely important to recognize and treat AF in a timely manner. If AF is detected, oral anticoagulation is indicated independently of the CHA₂DS₂-VASc Score. Rapid electrical cardioversion should be attempted to restore sinus rhythm. Beta-blockers and Amiodarone and in some cases interventional catheter-based radio frequency ablation are options to maintain the patient in sinus rhythm.
References
- 1.Monserrat Lorenzo, Elliott Perry M, Gimeno Juan R, Sharma Sanjay, Penas-Lado Manuel, McKenna William J. Non-sustained ventricular tachycardia in hypertrophic cardiomyopathy: an independent marker of sudden death risk in young patients. J. Am. Coll. Cardiol. 2003 Sep 03;42 (5):873–9. doi: 10.1016/s0735-1097(03)00827-1. [DOI] [PubMed] [Google Scholar]
- 2.Elliott P M, Poloniecki J, Dickie S, Sharma S, Monserrat L, Varnava A, Mahon N G, McKenna W J. Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J. Am. Coll. Cardiol. 2000 Dec;36 (7):2212–8. doi: 10.1016/s0735-1097(00)01003-2. [DOI] [PubMed] [Google Scholar]
- 3.O'Mahony Constantinos, Jichi Fatima, Pavlou Menelaos, Monserrat Lorenzo, Anastasakis Aristides, Rapezzi Claudio, Biagini Elena, Gimeno Juan Ramon, Limongelli Giuseppe, McKenna William J, Omar Rumana Z, Elliott Perry M. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur. Heart J. 2014 Aug 07;35 (30):2010–20. doi: 10.1093/eurheartj/eht439. [DOI] [PubMed] [Google Scholar]
- 4.Adabag A Selcuk, Casey Susan A, Kuskowski Michael A, Zenovich Andrey G, Maron Barry J. Spectrum and prognostic significance of arrhythmias on ambulatory Holter electrocardiogram in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2005 Mar 01;45 (5):697–704. doi: 10.1016/j.jacc.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 5.Elliott Perry M, Anastasakis Aris, Borger Michael A, Borggrefe Martin, Cecchi Franco, Charron Philippe, Hagege Albert Alain, Lafont Antoine, Limongelli Giuseppe, Mahrholdt Heiko, McKenna William J, Mogensen Jens, Nihoyannopoulos Petros, Nistri Stefano, Pieper Petronella G, Pieske Burkert, Rapezzi Claudio, Rutten Frans H, Tillmanns Christoph, Watkins Hugh. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014 Oct 14;35 (39):2733–79. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- 6.Elliott Perry M, Anastasakis Aris, Borger Michael A, Borggrefe Martin, Cecchi Franco, Charron Philippe, Hagege Albert Alain, Lafont Antoine, Limongelli Giuseppe, Mahrholdt Heiko, McKenna William J, Mogensen Jens, Nihoyannopoulos Petros, Nistri Stefano, Pieper Petronella G, Pieske Burkert, Rapezzi Claudio, Rutten Frans H, Tillmanns Christoph, Watkins Hugh. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014 Oct 14;35 (39):2733–79. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- 7.Olivotto I, Cecchi F, Casey S A, Dolara A, Traverse J H, Maron B J. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001 Nov 20;104 (21):2517–24. doi: 10.1161/hc4601.097997. [DOI] [PubMed] [Google Scholar]
- 8.Maron B J, Gardin J M, Flack J M, Gidding S S, Kurosaki T T, Bild D E. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995 Aug 15;92 (4):785–9. doi: 10.1161/01.cir.92.4.785. [DOI] [PubMed] [Google Scholar]
- 9.Wilke Iris, Witzel Katrin, Münch Julia, Pecha Simon, Blankenberg Stephan, Reichenspurner Hermann, Willems Stephan, Patten Monica, Aydin Ali. High Incidence of De Novo and Subclinical Atrial Fibrillation in Patients With Hypertrophic Cardiomyopathy and Cardiac Rhythm Management Device. J. Cardiovasc. Electrophysiol. 2016 Jul;27 (7):779–84. doi: 10.1111/jce.12982. [DOI] [PubMed] [Google Scholar]
- 10.Maron B J, Olivotto I, Spirito P, Casey S A, Bellone P, Gohman T E, Graham K J, Burton D A, Cecchi F. Epidemiology of hypertrophic cardiomyopathy-related death: revisited in a large non-referral-based patient population. Circulation. 2000 Aug 22;102 (8):858–64. doi: 10.1161/01.cir.102.8.858. [DOI] [PubMed] [Google Scholar]
- 11.Noseworthy Peter A, Yao Xiaoxi, Shah Nilay D, Gersh Bernard J. Stroke and Bleeding Risks in NOAC- and Warfarin-Treated Patients With Hypertrophic Cardiomyopathy and Atrial Fibrillation. J. Am. Coll. Cardiol. 2016 Jun 28;67 (25):3020–1. doi: 10.1016/j.jacc.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Haruki Shintaro, Minami Yuichiro, Hagiwara Nobuhisa. Stroke and Embolic Events in Hypertrophic Cardiomyopathy: Risk Stratification in Patients Without Atrial Fibrillation. Stroke. 2016 Apr;47 (4):936–42. doi: 10.1161/STROKEAHA.115.012130. [DOI] [PubMed] [Google Scholar]
- 13.Spirito Paolo, Autore Camillo, Formisano Francesco, Assenza Gabriele Egidy, Biagini Elena, Haas Tammy S, Bongioanni Sergio, Semsarian Christopher, Devoto Emmanuela, Musumeci Beatrice, Lai Francesco, Yeates Laura, Conte Maria Rosa, Rapezzi Claudio, Boni Luca, Maron Barry J. Risk of sudden death and outcome in patients with hypertrophic cardiomyopathy with benign presentation and without risk factors. Am. J. Cardiol. 2014 May 01;113 (9):1550–5. doi: 10.1016/j.amjcard.2014.01.435. [DOI] [PubMed] [Google Scholar]
- 14.Bonow R O, Frederick T M, Bacharach S L, Green M V, Goose P W, Maron B J, Rosing D R. Atrial systole and left ventricular filling in hypertrophic cardiomyopathy: effect of verapamil. Am. J. Cardiol. 1983 May 01;51 (8):1386–91. doi: 10.1016/0002-9149(83)90317-x. [DOI] [PubMed] [Google Scholar]
- 15.Chan Raymond H, Maron Barry J, Olivotto Iacopo, Pencina Michael J, Assenza Gabriele Egidy, Haas Tammy, Lesser John R, Gruner Christiane, Crean Andrew M, Rakowski Harry, Udelson James E, Rowin Ethan, Lombardi Massimo, Cecchi Franco, Tomberli Benedetta, Spirito Paolo, Formisano Francesco, Biagini Elena, Rapezzi Claudio, De Cecco Carlo Nicola, Autore Camillo, Cook E Francis, Hong Susie N, Gibson C Michael, Manning Warren J, Appelbaum Evan, Maron Martin S. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation. 2014 Aug 05;130 (6):484–95. doi: 10.1161/CIRCULATIONAHA.113.007094. [DOI] [PubMed] [Google Scholar]
- 16.Opfermann U T, Doll N, Walther T, Mohr F W. Combined mitral valve repair, LVOT myectomy and left atrial cryoablation therapy. Interact Cardiovasc Thorac Surg. 2003 Dec;2 (4):501–2. doi: 10.1016/S1569-9293(03)00129-4. [DOI] [PubMed] [Google Scholar]
- 17.Desai Milind Y, Bhonsale Aditya, Patel Parag, Naji Peyman, Smedira Nicholas G, Thamilarasan Maran, Lytle Bruce W, Lever Harry M. Exercise echocardiography in asymptomatic HCM: exercise capacity, and not LV outflow tract gradient predicts long-term outcomes. JACC Cardiovasc Imaging. 2014 Jan;7 (1):26–36. doi: 10.1016/j.jcmg.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Masri Ahmad, Pierson Lee M, Smedira Nicholas G, Agarwal Shikhar, Lytle Bruce W, Naji Peyman, Thamilarasan Maran, Lever Harry M, Cho Leslie S, Desai Milind Y. Predictors of long-term outcomes in patients with hypertrophic cardiomyopathy undergoing cardiopulmonary stress testing and echocardiography. Am. Heart J. 2015 May;169 (5):684–692.e1. doi: 10.1016/j.ahj.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Peteiro Jesús, Bouzas-Mosquera Alberto, Fernandez Xusto, Monserrat Lorenzo, Pazos Pablo, Estevez-Loureiro Rodrigo, Castro-Beiras Alfonso. Prognostic value of exercise echocardiography in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2012 Feb;25 (2):182–9. doi: 10.1016/j.echo.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Maron Barry J, Maron Martin S. Hypertrophic cardiomyopathy. Lancet. 2013 Jan 19;381 (9862):242–55. doi: 10.1016/S0140-6736(12)60397-3. [DOI] [PubMed] [Google Scholar]
- 21.Nielsen Jens Cosedis, Thomsen Poul Erik B, Højberg Søren, Møller Mogens, Riahi Sam, Dalsgaard Dorthe, Mortensen Leif S, Nielsen Tonny, Asklund Mogens, Friis Elsebeth V, Christensen Per D, Simonsen Erik H, Eriksen Ulrik H, Jensen Gunnar V H, Svendsen Jesper H, Toff William D, Healey Jeffrey S, Andersen Henning R. Atrial fibrillation in patients with sick sinus syndrome: the association with PQ-interval and percentage of ventricular pacing. Europace. 2012 May;14 (5):682–9. doi: 10.1093/europace/eur365. [DOI] [PubMed] [Google Scholar]
- 22.Mittal Suneet, Stein Kenneth, Gilliam F Roosevelt, Kraus Stacia Merkel, Meyer Timothy Edward, Christman Shelly Ann. Frequency, duration, and predictors of newly-diagnosed atrial fibrillation following dual-chamber pacemaker implantation in patients without a previous history of atrial fibrillation. Am. J. Cardiol. 2008 Aug 15;102 (4):450–3. doi: 10.1016/j.amjcard.2008.03.080. [DOI] [PubMed] [Google Scholar]
- 23.Healey Jeff S, Connolly Stuart J, Gold Michael R, Israel Carsten W, Van Gelder Isabelle C, Capucci Alessandro, Lau C P, Fain Eric, Yang Sean, Bailleul Christophe, Morillo Carlos A, Carlson Mark, Themeles Ellison, Kaufman Elizabeth S, Hohnloser Stefan H. Subclinical atrial fibrillation and the risk of stroke. N. Engl. J. Med. 2012 Jan 12;366 (2):120–9. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 24.Sanna Tommaso, Diener Hans-Christoph, Passman Rod S, Di Lazzaro Vincenzo, Bernstein Richard A, Morillo Carlos A, Rymer Marilyn Mollman, Thijs Vincent, Rogers Tyson, Beckers Frank, Lindborg Kate, Brachmann Johannes. Cryptogenic stroke and underlying atrial fibrillation. N. Engl. J. Med. 2014 Jun 26;370 (26):2478–86. doi: 10.1056/NEJMoa1313600. [DOI] [PubMed] [Google Scholar]
- 25.Mandal Saroj, Pande Arindam, Mandal Debosmita, Kumar Asutosh, Sarkar Achyut, Kahali Dhiman, Mazumdar Biswakesh, Panja Manotosh. Permanent pacemaker-related upper extremity deep vein thrombosis: a series of 20 cases. Pacing Clin Electrophysiol. 2012 Oct;35 (10):1194–8. doi: 10.1111/j.1540-8159.2012.03467.x. [DOI] [PubMed] [Google Scholar]
- 26.Siontis Konstantinos C, Geske Jeffrey B, Ong Kevin, Nishimura Rick A, Ommen Steve R, Gersh Bernard J. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high-risk population. J Am Heart Assoc. 2014 Jun 25;3 (3) doi: 10.1161/JAHA.114.001002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yashiro Bun, Minami Yuichiro, Terajima Yutaka, Hagiwara Nobuhisa. Prognostic difference between paroxysmal and non-paroxysmal atrial fibrillation in patients with hypertrophic cardiomyopathy. J Cardiol. 2014 Jun;63 (6):432–7. doi: 10.1016/j.jjcc.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 28.Azarbal Farnaz, Singh Maneesh, Finocchiaro Gherardo, Le Vy-Van, Schnittger Ingela, Wang Paul, Myers Jonathan, Ashley Euan, Perez Marco. Exercise capacity and paroxysmal atrial fibrillation in patients with hypertrophic cardiomyopathy. Heart. 2014 Apr;100 (8):624–30. doi: 10.1136/heartjnl-2013-304908. [DOI] [PubMed] [Google Scholar]
- 29.Boriani Giuseppe, Rapezzi Claudio, Biffi Mauro, Branzi Angelo, Spirito Paolo. Atrial fibrillation precipitating sustained ventricular tachycardia in hypertrophic cardiomyopathy. J. Cardiovasc. Electrophysiol. 2002 Sep;13 (9) doi: 10.1046/j.1540-8167.2002.00954.x. [DOI] [PubMed] [Google Scholar]
- 30.Doi Y, Kitaoka H. Hypertrophic cardiomyopathy in the elderly: significance of atrial fibrillation. J Cardiol. 2001;37 Suppl 1 ():133–8. [PubMed] [Google Scholar]
- 31.Ma Ji-Fang, Fu Hai-Xia. Apical aneurysm, apical thrombus, ventricular tachycardia and cerebral hemorrhagic infarction in a patient of mid-ventricular non-obstructive hypertrophic cardiomyopathy: A case report. Int. J. Cardiol. 2016 Oct 01;220 ():828–32. doi: 10.1016/j.ijcard.2016.06.282. [DOI] [PubMed] [Google Scholar]
- 32.Xiao Yan, Wang Lin-Ping, Yang Yan-Kun, Tian Tao, Yang Kun-Qi, Sun Xin, Jiang Yong, Liu Ya-Xin, Zhou Xian-Liang, Li Jian-Jun. Clinical Profile and Prognosis of Left Ventricular Apical Aneurysm in Hypertrophic Cardiomyopathy. Am. J. Med. Sci. 2016 Jan;351 (1):101–10. doi: 10.1016/j.amjms.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 33.Maron Barry J, Olivotto Iacopo, Bellone Pietro, Conte Maria Rosa, Cecchi Franco, Flygenring Björn P, Casey Susan A, Gohman Thomas E, Bongioanni Sergio, Spirito Paolo. Clinical profile of stroke in 900 patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2002 Jan 16;39 (2):301–7. doi: 10.1016/s0735-1097(01)01727-2. [DOI] [PubMed] [Google Scholar]
- 34.Weidemann Frank, Maier Sebastian K G, Störk Stefan, Brunner Thomas, Liu Dan, Hu Kai, Seydelmann Nora, Schneider Andreas, Becher Jan, Canan-Kühl Sima, Blaschke Daniela, Bijnens Bart, Ertl Georg, Wanner Christoph, Nordbeck Peter. Usefulness of an Implantable Loop Recorder to Detect Clinically Relevant Arrhythmias in Patients With Advanced Fabry Cardiomyopathy. Am. J. Cardiol. 2016 Jul 15;118 (2):264–74. doi: 10.1016/j.amjcard.2016.04.033. [DOI] [PubMed] [Google Scholar]
- 35.Michels Michelle, Soliman Osama I I, Kofflard Marcel J, Hoedemaekers Yvonne M, Dooijes Dennis, Majoor-Krakauer Danielle, ten Cate Folkert J. Diastolic abnormalities as the first feature of hypertrophic cardiomyopathy in Dutch myosin-binding protein C founder mutations. JACC Cardiovasc Imaging. 2009 Jan;2 (1):58–64. doi: 10.1016/j.jcmg.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Yang Hua, Woo Anna, Monakier Daniel, Jamorski Michal, Fedwick Katie, Wigle E Douglas, Rakowski Harry. Enlarged left atrial volume in hypertrophic cardiomyopathy: a marker for disease severity. J Am Soc Echocardiogr. 2005 Oct;18 (10):1074–82. doi: 10.1016/j.echo.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 37.Spirito P, Lakatos E, Maron B J. Degree of left ventricular hypertrophy in patients with hypertrophic cardiomyopathy and chronic atrial fibrillation. Am. J. Cardiol. 1992 May 01;69 (14):1217–22. doi: 10.1016/0002-9149(92)90939-v. [DOI] [PubMed] [Google Scholar]
- 38.Papavassiliu Theano, Germans Tjeerd, Flüchter Stephan, Doesch Christina, Suriyakamar Anton, Haghi Dariusch, Süselbeck Tim, Wolpert Christian, Dinter Dietmar, Schoenberg Stefan O, van Rossum Albert C, Borggrefe Martin. CMR findings in patients with hypertrophic cardiomyopathy and atrial fibrillation. J Cardiovasc Magn Reson. 2009 Sep 09;11 () doi: 10.1186/1532-429X-11-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gersh Bernard J, Maron Barry J, Bonow Robert O, Dearani Joseph A, Fifer Michael A, Link Mark S, Naidu Srihari S, Nishimura Rick A, Ommen Steve R, Rakowski Harry, Seidman Christine E, Towbin Jeffrey A, Udelson James E, Yancy Clyde W. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 2011 Dec 13;58 (25):e212–60. doi: 10.1016/j.jacc.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 40.Spoladore Roberto, Maron Martin S, D'Amato Rossella, Camici Paolo G, Olivotto Iacopo. Pharmacological treatment options for hypertrophic cardiomyopathy: high time for evidence. Eur. Heart J. 2012 Jul;33 (14):1724–33. doi: 10.1093/eurheartj/ehs150. [DOI] [PubMed] [Google Scholar]
- 41.January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 02;130 (23):e199–267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Providencia Rui, Elliott Perry, Patel Kiran, McCready Jack, Babu Girish, Srinivasan Neil, Bronis Kostantinos, Papageorgiou Nikolaos, Chow Anthony, Rowland Edward, Lowe Martin, Segal Oliver R, Lambiase Pier D. Catheter ablation for atrial fibrillation in hypertrophic cardiomyopathy: a systematic review and meta-analysis. Heart. 2016 Oct 01;102 (19):1533–43. doi: 10.1136/heartjnl-2016-309406. [DOI] [PubMed] [Google Scholar]
- 43.Santangeli Pasquale, Di Biase Luigi, Themistoclakis Sakis, Raviele Antonio, Schweikert Robert A, Lakkireddy Dhanunjaya, Mohanty Prasant, Bai Rong, Mohanty Sanghamitra, Pump Agnes, Beheiry Salwa, Hongo Richard, Sanchez Javier E, Gallinghouse G Joseph, Horton Rodney, Dello Russo Antonio, Casella Michela, Fassini Gaetano, Elayi Claude S, Burkhardt J David, Tondo Claudio, Natale Andrea. Catheter ablation of atrial fibrillation in hypertrophic cardiomyopathy: long-term outcomes and mechanisms of arrhythmia recurrence. Circ Arrhythm Electrophysiol. 2013 Dec;6 (6):1089–94. doi: 10.1161/CIRCEP.113.000339. [DOI] [PubMed] [Google Scholar]
- 44.Zhao Dong-Sheng, Shen Yi, Zhang Qing, Lin Gang, Lu Yi-Hua, Chen Bang-Tao, Shi Lin-Sheng, Huang Jian-Fei, Lu Hui-He. Outcomes of catheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy: a systematic review and meta-analysis. Europace. 2016 Apr;18 (4):508–20. doi: 10.1093/europace/euv339. [DOI] [PubMed] [Google Scholar]
- 45.Rahimi Kazem, Otto Catherine M. Heartbeat: Is atrial fibrillation ablation effective in patients with hypertrophic cardiomyopathy? Heart. 2016 Oct 01;102 (19):1511–2. doi: 10.1136/heartjnl-2016-310468. [DOI] [PubMed] [Google Scholar]
- 46.Prutkin Jordan M, Owens David S. Catheter ablation for atrial fibrillation in patients with hypertrophic cardiomyopathy. Heart. 2016 Oct 01;102 (19):1513–4. doi: 10.1136/heartjnl-2016-309761. [DOI] [PubMed] [Google Scholar]
- 47.Contreras-Valdes Fernando M, Buxton Alfred E, Josephson Mark E, Anter Elad. Atrial fibrillation ablation in patients with hypertrophic cardiomyopathy: long-term outcomes and clinical predictors. J. Am. Coll. Cardiol. 2015 Apr 14;65 (14):1485–7. doi: 10.1016/j.jacc.2014.12.063. [DOI] [PubMed] [Google Scholar]
- 48.Hayashi Hiroshi, Hayashi Meiso, Miyauchi Yasushi, Takahashi Kenta, Uetake Shunsuke, Tsuboi Ippei, Yodogawa Kenji, Iwasaki Yu-Ki, Shimizu Wataru. Left atrial wall thickness and outcomes of catheter ablation for atrial fibrillation in patients with hypertrophic cardiomyopathy. J Interv Card Electrophysiol. 2014 Aug;40 (2):153–60. doi: 10.1007/s10840-014-9894-y. [DOI] [PubMed] [Google Scholar]
- 49.Assasi Nazila, Xie Feng, Blackhouse Gord, Gaebel Kathryn, Robertson Diana, Hopkins Rob, Healey Jeff S, Goeree Ron. Comparative effectiveness of catheter ablation strategies for rhythm control in patients with atrial fibrillation: a meta-analysis. J Interv Card Electrophysiol. 2012 Dec;35 (3):259–75. doi: 10.1007/s10840-012-9723-0. [DOI] [PubMed] [Google Scholar]
- 50.Kuck Karl-Heinz, Fürnkranz Alexander, Chun K R Julian, Metzner Andreas, Ouyang Feifan, Schlüter Michael, Elvan Arif, Lim Hae W, Kueffer Fred J, Arentz Thomas, Albenque Jean-Paul, Tondo Claudio, Kühne Michael, Sticherling Christian, Brugada Josep. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur. Heart J. 2016 Oct 07;37 (38):2858–2865. doi: 10.1093/eurheartj/ehw285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maagh Petra, Plehn Gunnar, Christoph Arnd, Oernek Ahmet, Meissner Axel. Impact of Cryoballoon Ablation in Hypertrophic Cardiomyopathy-related Heart Failure due to Paroxysmal Atrial Fibrillation. A Comparative Case Series. Int J Med Sci. 2016;13 (9):664–72. doi: 10.7150/ijms.16181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bassiouny Mohamed, Lindsay Bruce D, Lever Harry, Saliba Walid, Klein Allan, Banna Moustafa, Abraham JoEllyn, Shao Mingyuan, Rickard John, Kanj Mohamed, Tchou Patrick, Dresing Thomas, Baranowski Bryan, Bhargava Mandeep, Callahan Thomas, Tarakji Khaldoun, Cantillon Daniel, Hussein Ayman, Marc Gillinov A, Smedira Nicholas G, Wazni Oussama. Outcomes of nonpharmacologic treatment of atrial fibrillation in patients with hypertrophic cardiomyopathy. Heart Rhythm. 2015 Jul;12 (7):1438–47. doi: 10.1016/j.hrthm.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 53.Chen Michael S, McCarthy Patrick M, Lever Harry M, Smedira Nicholas G, Lytle Bruce L. Effectiveness of atrial fibrillation surgery in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 2004 Feb 01;93 (3):373–5. doi: 10.1016/j.amjcard.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 54.Matsui Yoshiro, Fukada Yasuhisa, Imai Takahiro, Naito Yuji, Sasaki Shigeyuki. Combined cox maze procedure, septal myectomy, and mitral valve replacement for severe hypertrophic obstructive cardiomyopathy complicated by chronic atrial fibrillation. Ann Thorac Cardiovasc Surg. 2003 Oct;9 (5):323–5. [PubMed] [Google Scholar]
- 55.Groenveld Hessel F, Crijns Harry J G M, Rienstra Michiel, Van den Berg Maarten P, Van Veldhuisen Dirk J, Van Gelder Isabelle C. Does intensity of rate control influence outcome in persistent atrial fibrillation? Data of the RACE study. Am. Heart J. 2009 Nov;158 (5):785–91. doi: 10.1016/j.ahj.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 56.Takahashi Yoshihide, Yoshito Iesaka, Takahashi Atsushi, Harada Tomoo, Mitsuhashi Takeshi, Shirota Kinya, Kumagai Koichiro, Nuruki Norihito, Shiraishi Takayoshi, Nitta Junichi, Ito Hiroshi. AV nodal ablation and pacemaker implantation improves hemodynamic function in atrial fibrillation. Pacing Clin Electrophysiol. 2003 May;26 (5):1212–7. doi: 10.1046/j.1460-9592.2003.t01-1-00171.x. [DOI] [PubMed] [Google Scholar]
- 57.Kaya Adnan, Hayıroğlu Mert İlker, Keskin Muhammed, Tekkeşin Ahmet İlker, Alper Ahmet Taha. Resolution of left ventricular thrombus with apixaban in a patient with hypertrophic cardiomyopathy. Turk Kardiyol Dern Ars. 2016 Jun;44 (4):335–7. doi: 10.5543/tkda.2015.68054. [DOI] [PubMed] [Google Scholar]
- 58.Guttmann Oliver P, Pavlou Menelaos, O'Mahony Constantinos, Monserrat Lorenzo, Anastasakis Aristides, Rapezzi Claudio, Biagini Elena, Gimeno Juan Ramon, Limongelli Giuseppe, Garcia-Pavia Pablo, McKenna William J, Omar Rumana Z, Elliott Perry M. Prediction of thrombo-embolic risk in patients with hypertrophic cardiomyopathy (HCM Risk-CVA). Eur. J. Heart Fail. 2015 Aug;17 (8):837–45. doi: 10.1002/ejhf.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Derejko Paweł, Polańska Magdalena, Chojnowska Lidia, Michałowska Ilona, Wójcik Anna, Piotrowicz Ewa, Lech Agnieszka, Kłopotowski Mariusz, Baranowski Rafał, Przybylski Andrzej, Bilińska Maria, Sierpiński Radosław, Walczak Franciszek, Szumowski Lukasz. Catheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy: atrial fibrillation type determines the success rate. Kardiol Pol. 2013;71 (1):17–24. [PubMed] [Google Scholar]
- 60.Di Donna Paolo, Olivotto Iacopo, Delcrè Sara Dalila Luisella, Caponi Domenico, Scaglione Marco, Nault Isabelle, Montefusco Antonio, Girolami Francesca, Cecchi Franco, Haissaguerre Michel, Gaita Fiorenzo. Efficacy of catheter ablation for atrial fibrillation in hypertrophic cardiomyopathy: impact of age, atrial remodelling, and disease progression. Europace. 2010 Mar;12 (3):347–55. doi: 10.1093/europace/euq013. [DOI] [PubMed] [Google Scholar]
- 61.Bunch T Jared, Munger Thomas M, Friedman Paul A, Asirvatham Samuel J, Brady Peter A, Cha Yong-Mei, Rea Robert F, Shen Win-Kuang, Powell Brian D, Ommen Steve R, Monahan Kristi H, Haroldson Janis M, Packer Douglas L. Substrate and procedural predictors of outcomes after catheter ablation for atrial fibrillation in patients with hypertrophic cardiomyopathy. J. Cardiovasc. Electrophysiol. 2008 Oct;19 (10):1009–14. doi: 10.1111/j.1540-8167.2008.01192.x. [DOI] [PubMed] [Google Scholar]
- 62.Gaita Fiorenzo, Di Donna Paolo, Olivotto Iacopo, Scaglione Marco, Ferrero Ivana, Montefusco Antonio, Caponi Domenico, Conte Maria Rosa, Nistri Stefano, Cecchi Franco. Usefulness and safety of transcatheter ablation of atrial fibrillation in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 2007 Jun 01;99 (11):1575–81. doi: 10.1016/j.amjcard.2006.12.087. [DOI] [PubMed] [Google Scholar]
- 63.Kilicaslan Fethi, Verma Atul, Saad Eduardo, Themistoclakis Sakis, Bonso Aldo, Raviele Antonio, Bozbas Huseyin, Andrews Michelle Williams, Beheiry Salwa, Hao Steven, Cummings Jennifer E, Marrouche Nassir F, Lakkireddy Dhannunjaya, Wazni Oussama, Yamaji Hirosuke, Saenz Luis C, Saliba Walid, Schweikert Robert A, Natale Andrea. Efficacy of catheter ablation of atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy. Heart Rhythm. 2006 Mar;3 (3):275–80. doi: 10.1016/j.hrthm.2005.11.013. [DOI] [PubMed] [Google Scholar]


