Abstract
Cholangiocarcinoma (CCA) remains to be a major health problem in several Asian countries including Thailand. The molecular mechanism of CCA is poorly understood. Early diagnosis is difficult, and at present, no effective therapeutic drug is available. The present study aimed to identify the molecular mechanism of CCA by gene expression profile analysis and to search for current approved drugs which may interact with the upregulated genes in CCA. Gene Expression Omnibus (GEO) was used to analyze the gene expression profiles of CCA patients and normal subjects. Using the Kyoto Encyclopedia of Genes and Genomes (KEGG), gene ontology enrichment analysis was also performed, with the KEGG pathway analysis indicating that pancreatic secretion, protein digestion and absorption, fat digestion and absorption, and glycerolipid metabolism may serve important roles in CCA oncogenesis. The drug signature database (DsigDB) was used to search for US Food and Drug Administration (FDA)-approved drugs potentially capable of reversing the effects of the upregulated gene expression in CCA. A total of 61 antineoplastic and 86 non-antineoplastic drugs were identified. Checkpoint kinase 1 was the most interacting with drug signatures. Many of the targeted protein inhibitors that were identified have been approved by the US-FDA as therapeutic agents for non-antineoplastic diseases, including cimetidine, valproic acid and lovastatin. The current study demonstrated an application for bioinformatics analysis in assessing the potential efficacy of currently approved drugs for novel use. The present results suggest novel indications regarding existing drugs useful for CCA treatment. However, further in vitro and in vivo studies are required to support the current predictions.
Keywords: cholangiocarcinoma, gene expression analysis, pathway analysis, non-antineoplastic drug, gene-drug interaction
Introduction
Cholangiocarcinoma (CCA) is the second most common hepatobiliary cancer after hepatocellular carcinoma and accounts for 10–15% of all liver carcinomas (1,2). It arises in the biliary tract epithelium (cholangiocyte) and is categorized into three groups: Intrahepatic, perihilar and distal hepatic carcinoma. Previous studies in the US and worldwide have demonstrated that the associated mortality and incidence rates have increased since 2002 (3,4). Clinically, CCA is a challenge to treat as patients often do not exhibit clear symptoms, making early diagnose difficult (5). At present, there is no specific molecular targeting treatment for CCA. Conventional chemotherapy is still used but is generally ineffective in cases of CCA associated with different genetic variants (6). A greater understanding of the biology of CCA may improve treatment and diagnosis.
Recent research has focused on target identification and selective inhibitors of several molecular signaling pathways (7). In earlier reports, genetic alterations were identified to be involved in CCA carcinogenesis, including point mutations in p53, B-Raf proto-oncogene serine/threonine kinase and V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog (8,9). Liver-specific downregulation of Smad family member 4 and phosphatase and tensin homolog, as established tumor suppressor genes, may also induce CCA (10,11). In addition, increased expression of cyclooxygenase-2, receptor tyrosine-protein kinase c-erbB-2 and interleukin 6 are considered to be involved in early carcinogenesis in the biliary tract epithelium (12,13).
Although a variety of anticancer protein inhibitors, including Notch, Wnt, growth factor receptor and histone deacetylase inhibitors, are being developed to suppress oncoproteins, an average time of 7 years is typically required for drug approval following clinical trial evaluation (14). However, it has been demonstrated that certain drugs already approved by the US Food and Drug Administration (FDA) may be used to suppress cancer. For example, inhibitors of 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase, including lovastatin, atorvastatin and simvastatin, and of cyclooxygenase-2 (COX-2), including celecoxib, have potential preventative effects on CCA carcinogenesis (15,16). Identifying novel uses for the approved drugs also minimizes the need for toxicity studies, particularly with regard to non-antineoplastic drugs.
The study of cancer genomes, and CCA mechanisms in particular, is still in its infancy. Single gene studies are no longer feasible for this complex disease. Improved and more powerful tools for analysis by high-throughput array are required to provide greater accuracy, precision and cost-effectiveness. Gene Expression Omnibus (GEO) is a public functional genomics data repository created to aid the identification and analysis of gene regulatory and cancer signaling pathways. By also serving as a gene-drug interaction database, this may further be used to determine novel therapeutic drugs and targets that may be crucial to the identification of novel protein inhibitors.
In the present study, gene expression profiles from the GSE26566 dataset were collected to analyze differential gene expression, and currently approved drugs associated with the upregulated genes were searched in drug interaction databases. The greater availability of gene expression analytical tools and improved access to information on currently approved treatments may be useful in developing novel indications for CCA drug treatment.
Materials and methods
Data collection
The gene expression dataset of normal subjects and intrahepatic CCA (iHCCA) patients [Gene Expression Omnibus (GEO) accession no. GSE26566 (17)] were obtained from the National Center for Biotechnology Information GEO database (https://www.ncbi.nlm.nih.gov/geo/). A total of 104 cholangiocarcinoma and 6 normal intrahepatic bile duct gene expression data profiles were collected. This microarray platform (GLP6104) was collected from one type of platform: Illumina humanRef-8 v2.0 expression beadchip.
Gene expression analysis
The microarray database GLP6104 platform was analyzed using GEO2R (version 2.14.1) for the collected datasets. The data was normalized by log 2 transformation in GEO2R along with the Benjamini-Hochberg procedure for false discovery rate correction. Samples were assigned to normal and cholangiocarcinoma subject groups. Following analysis by GEO2R, the dataset was displayed in terms of adjusted P-values, P-values, log fold changes, gene symbols and gene names. The top 15 most up- and downregulated genes according to most adjusted P-value (from Student's t-test, P<0.05) were selected as differentially expressed genes (DEGs).
Gene ontology (GO) analysis
To investigate the DEGs at a functional level, the Database for Annotation, Visualization and Integrated Discovery (DAVID; https://david.ncifcrf.gov/) was used to establish gene clustering following GO analysis, as described previously (18). The GO was categorized into cellular component, biological process and molecular function following standard GO analysis as detailed previously (19).
Pathway analysis
The Kyoto Encyclopedia of Genes and Genomes (KEGG; http://www.genome.jp/kegg/) was accessed for assistance in investigating the dysregulated signaling pathways in cholangiocarcinoma as detailed previously (20). The DEGs were searched in the database for investigation of biochemistry pathways that may be involved in the tumorigenesis and development of cholangiocarcinoma. The up- and downregulated genes were analyzed by DAVID. The significant categories were predicted by an Expression Analysis Systematic Explorer score <0.01 and the minimum number of genes for the corresponding term >2 were considered.
Protein-protein interaction (PPI) analysis
PPI network analysis was conducted by using the search tool for the retrieval of interacting genes/proteins (STRING; http://string-db.org/) as in previous study (21). The threshold protein interaction reliability score was 0.400, which represents a medium level of confidence (22).
Validation by The Cancer Genome Atlas (TCGA) Kaplan-Meier-plotter analysis
To confirm the analysis, an overall survival (OS) Kaplan-Meier computation was performed by using the top 30 DEGs (15 most upregulated and 15 most downregulated). Expression and OS data of the iHCCA cohort in the TCGA database was assessed and P-values obtained by log-rank test using the cBioPortal for Cancer Genomics (http://www.cbioportal.org/) (23–25).
Gene-drug interaction analysis
The drug signatures of upregulated genes and their interacting genes were identified by searching the drug signatures database for gene set analysis (DSigDB) (26). The signatures of the database are grouped into four categories: i) 1,202 FDA-approved drugs retrieved for bioactivity assay results from PubChem and ChEMBL; ii) 1,220 kinase inhibitors from human kinome profiling databases (Medical Research Council Kinase Inhibitor database and Harvard Medical School Library of Integrated Network-based Cellular Signatures database); iii) 1,309 perturbagens identified from DEGs in the three cell lines PC3 (prostate cancer), HL60 (leukemia) and SKMEL5 (melanoma) (with >2-fold change compared with controls); and iv) drug candidates identified by manual curation and text mining from the Therapeutics Targets Database and the Comparative Toxicogenomics Database (27–29). The drugs were further categorized according to the US-FDA database (https://www.accessdata.fda.gov/scripts/cder/daf/) as FDA-approved non-antineoplastic and neoplastic drugs.
Results
Gene expression analysis
The dataset retrieved from GEO26566 included 104 iHCCA and 6 normal profiles. The top 15 most significantly up- and downregulated genes, respectively, determined by integrative analysis in GEOR2, are listed in Table I. FYVE, RhoGEF and PH domain-containing 6 (FGD6) and chymotrypsinogen B2 (CTRB2) were the most significantly up- and downregulated genes, respectively (Table I).
Table I.
Top 30 most significantly up- and downregulated differentially expressed genes.
| A, Upregulated genes | ||||
|---|---|---|---|---|
| Gene probe ID | Gene symbol | Description | P-value | Log fold change |
| 154240685 | FGD6 | FYVE, RhoGEF and PH domain-containing 6 | 9.58E-09 | 3.86 |
| 349501059 | CHEK1 | Checkpoint kinase 1 | 3.22E-07 | 4.34 |
| 61743966 | CTBP1 | C-terminal-binding protein 1 | 3.29E-07 | 3.63 |
| 168229167 | BUB1B | BUB1 mitotic checkpoint serine/threonine kinase B | 6.76E-07 | 5.38 |
| 154800452 | TROAP | Trophinin-associated protein | 7.45E-07 | 5.41 |
| 157419137 | LAMC2 | Laminin subunit gamma 2 | 1.57E-06 | 4.8 |
| 19882252 | CST2 | Cystatin-SA | 1.77E-06 | 4.71 |
| 748821156 | CKAP2L | Cytoskeleton-associated protein 2-like | 2.44E-06 | 3.93 |
| 300794717 | WDHD1 | WD repeat and HMG-box DNA-binding protein 1 | 4.42E-06 | 4.05 |
| 938148819 | MMP11 | Matrix metallopeptidase 11 | 1.23E-05 | 6.10 |
| 444189305 | FAM83B | Family with sequence similarity 83 member B | 3.77E-05 | 5.82 |
| 54607054 | GJB3 | Gap junction protein beta 3 | 1.36E-04 | 4.90 |
| 148806907 | FNDC1 | Fibronectin type III-domain containing 1 | 1.45E-04 | 4.41 |
| 379056370 | CDCA8 | Cell division cycle-associated 8 | 1.66E-04 | 4.01 |
| 748983174 | CNBD2 | Cyclic nucleotide-binding domain-containing 2 | 2.68E-04 | 6.61 |
| B, Downregulated genes | ||||
| Gene probe ID | Gene symbol | Description | P-value | Log fold change |
| 118498349 | CTRB2 | Chymotrypsinogen B2 | 8.80E-34 | −10.15 |
| 236459772 | CELA2A | Chymotrypsin-like elastase family member 2A | 3.21E-29 | −9.71 |
| 54607079 | CPB1 | Carboxypeptidase B1 | 9.23E-29 | −10.98 |
| 38016927 | PLA2G1B | Phospholipase A2 group IB | 8.53E-25 | −10.78 |
| 747165370 | CPA1 | Carboxypeptidase A1 | 1.09E-21 | −11.95 |
| 58331210 | CELA2B | Chymotrypsin-like elastase family member 2B | 3.17E-20 | −8.90 |
| 440309868 | CEL | Carboxyl ester lipase | 5.85E-18 | −9.68 |
| 734703929 | PNLIPRP1 | Pancreatic lipase-related protein 1 | 1.14E-14 | −8.37 |
| 236460049 | CELA3A | Chymotrypsin-like elastase family member 3A | 2.42E-14 | −10.80 |
| 357588512 | CLPS | Colipase | 1.88E-12 | −12.09 |
| 310923201 | PRSS1 | Protease, serine 1 | 2.48E-10 | −11.52 |
| 217416389 | CPA2 | Carboxypeptidase A2 | 3.24E-10 | −11.27 |
| 62526042 | CTRC | Chymotrypsin 2 | 7.93E-09 | −10.82 |
| 1010226556 | CELA3B | Chymotrypsin-like elastase family member 3B | 8.45E-07 | −11.10 |
| 1042779786 | PNLIP | Pancreatic lipase | 1.22E-06 | −12.04 |
Functional enrichment analysis
GO enrichment analysis of DEGs was performed for the top 30 most significant DEG signatures (15 most upregulated and 15 most downregulated). The DEGs were classified into the three GO categories of biological process, cellular component and molecular function. It was identified that the significantly enriched GO terms for biological process included proteolysis and lipid catabolic processes, while those for cellular component included extracellular space and extracellular region; the significantly enriched GO terms for molecular function included serine-type endopeptidase activity and triglyceride lipase activity (Table II).
Table II.
Enriched GO categories of differentially expressed genes.
| A, Biological process clustering | ||||
|---|---|---|---|---|
| GO term | Biological process | Gene count | Genes | P-value |
| GO:0006508 | Proteolysis | 11 | CPA1, CPA2, CPB1, CTRC, CELA2A, CELA2B, CELA3A, CELA3B, CTRB2, MMP11, PRSS1 | 1.7E-09 |
| GO:0007586 | Digestion | 4 | CELA3A, CTRB2, CLPS, PRSS1 | 1.2E-04 |
| GO:0044241 | Lipid digestion | 3 | CEL, CLPS, PNLIP | 1.8E-04 |
| GO:0022617 | Extracellular matrix | 4 | CTRB2, LAMC2, MMP11, PRSS1 | 2.1E-04 |
| GO:0016042 | Lipid catabolic process | 4 | CLPS, PNLIPRP1, PNLIP, PLA2G1B | 3.0E-04 |
| GO:0009235 | Cobalamin metabolic process | 3 | CTRC, CTRB2, PRSS1 | 4.8E-04 |
| GO:0030299 | Intestinal cholesterol absorption | 2 | CEL, PNLIP | 1.4E-02 |
| GO:0006629 | Lipid metabolic process | 3 | CEL, CLPS, PNLIPRP1 | 2.4E-02 |
| GO:0007093 | Mitotic cell cycle checkpoint | 2 | BUB1B, CHEK1 | 4.8E-02 |
| GO:0001523 | Retinoid metabolic process | 2 | CLPS, PNLIP | 9.0E-02 |
| B, Cellular component | ||||
| GO term | Biological process | Gene count | Genes | P-value |
| GO:0005615 | Extracellular space | 14 | CEL, CPA1, CPA2, CPB1, CHEK1, CELA2A, CELA2B, CELA3A, CELA3B, CTRB2, CST2, LAMC2, PNLIPRP1, PLA2G1B | 4.1E-08 |
| GO:0005576 | Extracellular region | 13 | CEL, CPA2, CTRC, CELA2B, CTRB2, CLPS, FNDC1, LAMC2, MMP11, PNLIPRP1, PNLIP, PLA2G1B, PRSS1 | 2.7E-06 |
| GO:0051233 | Spindle midzone | 2 | BUB1B, CDCA8 | 3.0E-02 |
| C, Molecular function | ||||
| GO term | Biological process | Gene count | Genes | P-value |
| GO:0004252 | Serine-type endopeptidase activity | 8 | CTRC, CELA2A, CELA2B, CELA3A, CELA3B, CTRB2, MMP11, PRSS1 | 1.1E-07 |
| GO:0004806 | Triglyceride lipase activity | 3 | CEL, PNLIPRP1, PNLIP | 3.3E-04 |
| GO:0004181 | Metal carboxypeptidase activity | 3 | CPA1, CPA2, CPB1 | 8.4E-04 |
| GO:0016298 | Lipase activity | 2 | CEL, PNLIPRP1 | 1.4E-02 |
| GO:0004180 | Carboxypeptidase activity | 2 | CPA2, CPB1 | 2.7E-02 |
| GO:0008236 | Serine-type peptidase activity | 2 | CTRB2, PRSS1 | 9.6E-02 |
GO, gene ontology.
Pathway enrichment analysis based on the KEGG database demonstrated that the DEGs were significantly enriched in 4 terms (Table III). The most significant pathway was pancreatic secretion (P=1.6E-17).
Table III.
Enriched Kyoto Encyclopedia of Genes and Genomes pathways of differentially expressed genes.
| Term | Pathway | P-value | Gene count | Genes |
|---|---|---|---|---|
| Hsa:04972 | Pancreatic secretion | 1.6E-17 | 12 | CEL, CPA1, CPA2, CPB1, CELA2A, CELA2B, CELA3A, CELA3B, PNLIPRP1, PNLIP, PLA2G1B, PRSS1 |
| Hsa:04972 | Protein digestion and absorption | 7.5E-10 | 8 | CPA1, CPA2, CPB1, CELA2A, CELA2B, CELA3A, CELA3B, PRSS1 |
| Hsa:04975 | Fat digestion and absorption | 2.0E-06 | 5 | CEL, CLPS, PNLIPRP1, PNLIP, PLA2G1B |
| Hsa:00561 | Glycerolipid metabolism | 8.7E-03 | 3 | CEL, PNLIPRP1, PNLIP |
Hsa, Homo sapiens.
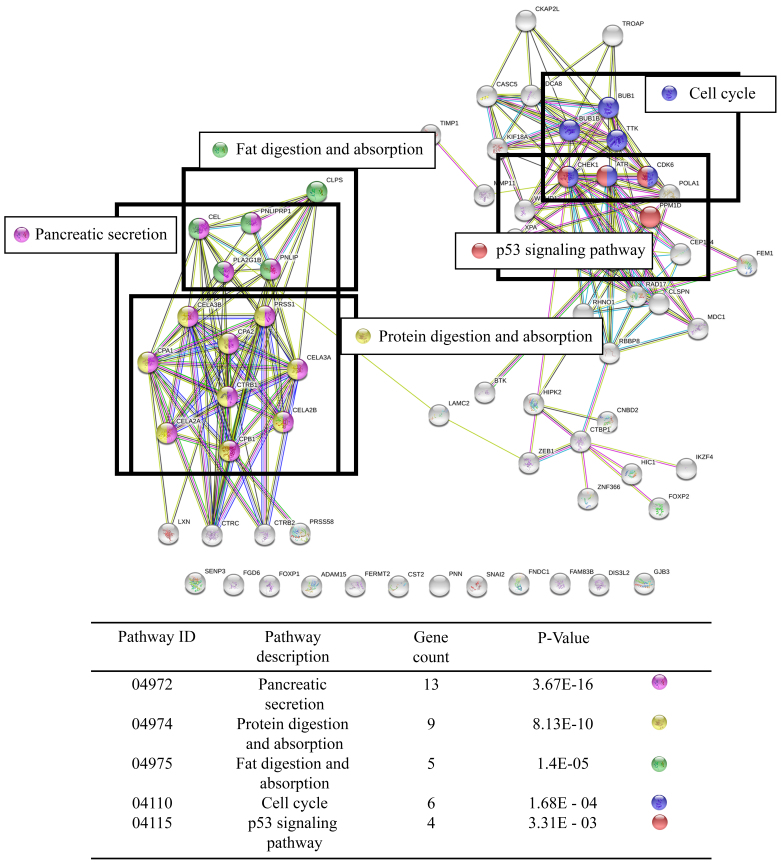
PPI network analysis
To investigate the associations between the DEGs and signaling pathways, a comprehensive analysis of protein interactions of the top 15 up- and downregulated genes, respectively, was conducted using the STRING database. As illustrated in Fig. 1, direct or indirect interactions were identified with the exception of 12 genes [Forkhead box p1, ADAM metallopeptidase domain 15, FGD6, sentrin-specific-peptidase 3, fermitin family member 2, cystatin-SA, pinin, Snail family transcriptional repressor 2, fibronectin type III domain containing 1 (FNDC1), family with sequence similarity 83 member B (FAM83B), DIS3-like 3′-5′ exoribonuclease 2 and gap junction protein beta 3 (GJB3)]. The associations between pathways and gene expression were categorized into 5 pathways, namely pancreatic secretion, protein digestion and absorption, lipid digestion and absorption, cell cycle and p53 signaling pathway.
Figure 1.
Protein-protein interaction network for differentially expressed genes. The genes with no direct interaction with any other partner are the co-expression genes of the genes of interest.
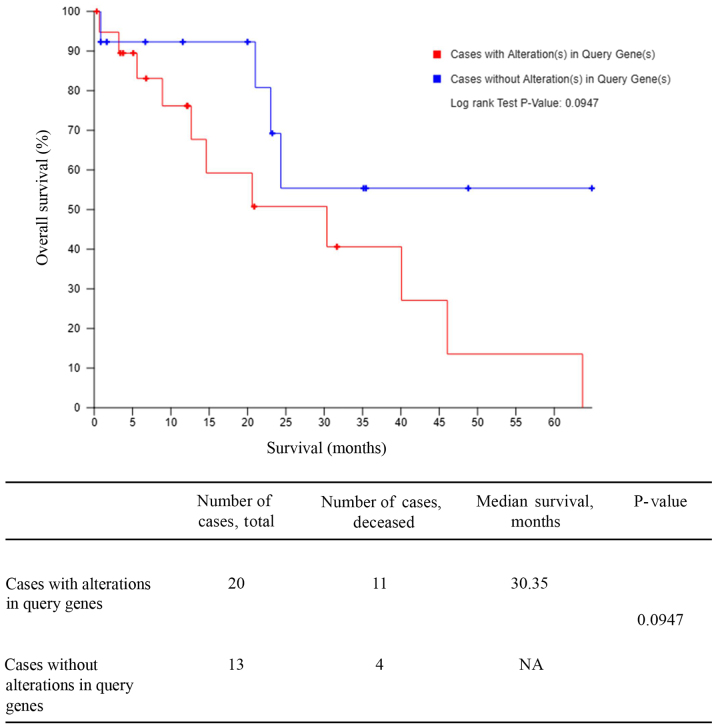
Validation by TCGA Kaplan-Meier-plotter analysis
For validation of altered gene signatures using clinical data, CCA data was retrieved from the TCGA database (n=36). Cases were divided into those with alterations in the previously identified DEGs (n=20) and those without (13). The Kaplan-Meier curve demonstrated that the altered genes group was associated with a significantly lower survival rate (P=0.0947; Fig. 2).
Figure 2.
Kaplan-Meier survival curves for the association between the gene alteration of differentially expressed genes and the overall survival time of patients with cholangiocarcinoma.
Assessment of gene-drug interaction
Drug signatures from drug-upregulated gene interactions in DsigDB were classified, based on known FDA-approved targeted agents including neoplastic and non-neoplastic drugs. A total of 86 non-neoplastic and 61 neoplastic drugs were identified. Among the top upregulated genes, CHEK1 was the most interacting with drug signatures. No drug signatures were identified for CST2, MMP11 or cyclic nucleotide binding domain-containing 2 (Table IV). The interacting anticancer drugs belonged to 6 categories in the FDA database, namely alkylating agent, hormone agent, cytotoxic alkaloid, antitumor antibiotic, antimetabolite and protein inhibitor (Table V).
Table IV.
Non-neoplastic and neoplastic drugs relating to upregulated genes in cholangiocarcinoma.
| Gene symbol | Total drugs | Non-neoplastic drugs | Neoplastic drugs |
|---|---|---|---|
| FGD6 | 8 | Zalcitabine, digoxin, raloxifene, retinoic acid | Vorinostat, tamoxifen, 5-fluorouracil, melphalan |
| CHEK1 | 44 | Chlorzoxazone, dirithromycin, medrysone, latamoxef, clindamycin, ipratropium bromide, danazol, thymidine, caffeine, mucosolvan, lovastatin, troglitazone, rimonabant hydrochloride, menadione, retinoic acid, diclofenac, carbamazepine, valproic acid, folic acid, auraptan, zidovudine | Etoposide, bosutinib, sunitinib, daunorubicin, irinotecan, bortezomib, melphalan, mitomycin vorinostat, hydroxyurea, olaparib, 5-fluorouracil gemcitabine, temozolomide, doxorubicin, decitabine, carmustine, bortezomib, fludarabine, irinotecan, clofarabine, busalfan |
| CTBP1 | 18 | Nifedipine, clofazimine, chlortetracycline, chlozoxazone, baclofen, levonorgestrel, cimetidine, ambroxol, medrysone, valproic acid, dorzolamide, clindamycin, ipratropium bromide, danazole, niclozamide, vitamin E, acetaminophen | Vorinostat |
| BUB1B | 20 | Ciclopirox, trifluridine, pyrvinium, clindamycin, colchicine, piroxicam, acetaminophen, valproic acid | Daunorubicin, etoposide, azacitidine, irinotecan, fulvestrant, docetaxel, dasatinib, decitabine, doxorubicin, 5-fluorouracil, paclitaxel, bicalutamide |
| TROAP | 11 | Ciclopirox, trifluridine, pergolide, acetaminophen, valproic acid | Etoposide, azacitidine, methotrexate, doxorubicin, irinotecan, 5-fluorouracil |
| LAMC2 | 4 | Valproic acid, mifepristone | Mechlorethamine, cyclophosphamide |
| CST2 | 0 | – | – |
| CKAP2L | 3 | Retinoic acid, acetaminophen | Dasatinib |
| WDHD1 | 10 | Zalcitabine, primaquine, doxycycline, latamoxef, cianidanol, retinoic acid, acetaminophen, valproic acid | Dasatinib, vorinostat |
| MMP11 | 0 | – | – |
| FAM83B | 1 | Valproic acid | – |
| JGB3 | 5 | Retigabine | Vorinostat, azacitidine, doxorubicin, decitabine |
| FNDC1 | 1 | Valproic acid | – |
| CDCA8 | 22 | Chlortetracycline, chlorzoxazone, ciclopirox, trifluridine, cimetidine, medrysone, pyrvinium, latamoxef, glibenclamide, metronidazole, monobenzone, piroxicam, retinoic acid, acetaminophen, zidovudine | Azacitidine, methotrexate, doxorubicin, irinotecan, 5-fluorouracil, vinblastine, cytarabine |
| CNBD2 | 0 | – | – |
| Total | 147 | 86 | 61 |
Table V.
Categories of the US Food and Drug Administration-approved drugs associated with upregulated genes.
| Category | Drug name |
|---|---|
| Alkylating agent | Melphalan, temozolomide, busalfan, carmustine, mechlorethamine, cyclophosphamide, busalfan |
| Hormone agent | Tamoxifen, fulvestrant, bicalutamide |
| Cytotoxic alkaloid | Etoposide, irinotecan, vinblastine, docetaxel, paclitaxel |
| Antitumor antibiotic | Doxorubicin, daunorubicin, mitomycin |
| Antimetabolite | Methotrexate, 5-fluorouracil, clofarabine, gemcitabine, cytarabine, azacitidine, fludarabine, decitabine, hydroxyurea |
| Protein inhibitor | Vorinostat, bosutinib, sunitinib, bortezomib, olaparib |
Discussion
Although previous study has suggested numerous biomarkers and therapeutic targets for CCA (30), there remains to be few treatments and drugs available to overcome the disease. In addition, the molecular mechanisms of CCA are not fully understood. In the present study, gene expression profiles and dysregulated pathways of CCA were analyzed, along with gene-drug interactions for drug repositioning.
In the present study, gene expression analysis was performed on a CCA patient dataset. The analysis firstly determined the top 30 DEGs that may be important for CCA carcinogenesis. Checkpoint kinase 1 (CHEK1) is required for DNA replication and cell survival in cancer (31). BUB1 mitotic checkpoint serine/threonine kinase B (BUB1B) and cell division cycle-associated 8 (CDCA8) have been identified to be involved in cell division and the cell spindle check-point. Increased expression in progressive cholangiocarcinoma has also been identified (32–34). A previous study observed that matrix metalloproteinase 11 (MMP11) was upregulated in CCA patients with poor prognosis. Therefore, MMP11 may be useful as a prognostic marker in CCA (35–36).
GO and KEGG pathway analysis demonstrated that the main biological processes involved in CCA were extracellular matrix and protein and lipid metabolism. A previous study of bile acid identified downregulated genes including CTRB, colipase, chymotrypsin-like elastase family member 3A (CELA3A) and CELA3B, phospholipase A2, chymotrypsin 2, carboxypeptidase B (CPB) and CPA, similar to the present gene expression analysis. The profiles of these genes also differ markedly between CCA patients and normal subjects, and they may be protein markers for differentiating malignant from benign tumors (37). Integrative analysis of five microarrays in the GSE26566 dataset indicated that MMP11 and FGD6 were upregulated while CELA2A and CTRB2 were downregulated. These genes were associated with the extracellular matrix, cell division processes, bile acid secretion and protein and lipid metabolism, with these biological processes implicated in various pathways in CCA progression (38). These results of DEG pathway analysis may be used to investigate and target the mechanism of disease initiation, to ultimately treat CCA, and to clarify the association between metabolic dysregulation and CCA progression.
Previous PPI analysis revealed an association of ataxia telangiectasia with Rad3-related protein/casein kinase 1 signaling in p53 activation, which serves an important role in DNA repair, cell division and the cell cycle (39–40). CTRB, a member of a family of serine proteases, is secreted into the gastrointestinal tract and activated through proteolytic cleavage by protease, serine 1. A previous study observed low-level expression of CTRB in pancreatic cancer (41). The current analysis of CCA patient profiles revealed similar results. As concluded previously (41), this suggests that CTRB may be a genetic marker for CCA. Furthermore, since genes including carboxyl ester lipase, pancreatic lipase-related protein 1, pancreatic lipase and phospholipase A2 group IB associated with pancreatic secretion and fat digestion and absorption exhibited significant interaction, the tumorigenesis and progression of CCA may lead to the dysfunction of liver metabolism and disruption of pancreatic function.
According to the survival analysis, patients with CCA in the altered gene group had a lower rate of OS compared with those patients with no alterations in the DEGs of interest. Genetic alterations in cell metabolism may contribute to poor prognosis in human cancers (42). Lipid metabolism is now considered to have a key role in cancer progression; it has been proposed that increased metabolic flux may serve as substrate source for phospholipid synthesis in the rapid growth stages of cancer (43).
The use of molecular signatures in cancer to determine potential drug therapies is a widespread technique (44). Potential drugs that target molecular aberrations in various CCA pathways have been proposed (45). In the present study, the genetic signatures of upregulated genes from microarray datasets were analyzed for gene-drug interactions, and US-FDA-approved drugs were grouped according to their FDA classification as antineoplastic and non-antineoplastic agents. The present study demonstrated the potential of various FDA approved antineoplastic drugs for use in CCA treatment. For example, vorinostat is a histone deacetylase inhibitor which has been approved by the FDA for the treatment of cutaneous manifestations of cutaneous T-cell lymphoma; olaparib is a poly-ADP-ribose polymerase inhibitor approved for ovarian and breast cancer treatment; and sunitinib, a multitargeted receptor tyrosine kinase inhibitor, has been approved by the FDA for the treatment of renal cell carcinoma (46–48). Also dasatinib, a kinase inhibitor approved for use in patients with chronic myelogenous leukemia, may be used to treat CCA by targeting the FGD6, CHEK1, C-terminal binding protein 1 (CTBP1), cytoskeleton-associated protein 2-like and WD repeat and HMG-box DNA-binding protein 1 (WDHD1) genes. Sunitinib has been reported to have possible use in iHCCA chemotherapies, where resistance is an issue in advanced stage patients (49–51).
Several chemotherapeutic drugs may be used to treat bile duct cancer, for example, 5-fluorouracil, gemcitabine, cisplatin, capecitabine and oxaliplatin. The current standard treatment drugs for CCA are 5-fluorouracil, gemcitabine, or their combinations with cisplatin. In certain cases, two or more of these drugs may be combined. However, their treatment efficacy is unsatisfactory with low clinical response rate (52). A previous study observed survival of patients treated with cisplatin plus gemcitabine, there may be little benefit to patients because of the debilitating side effects, depending on the amount and frequency of the dosage (53,54). Nonetheless, CCA is a heterogeneous cancer involving multifactorial risks (55,56). The present results demonstrate that the other antineoplastic drugs, including protein inhibitors such as vorinostat, sunitinib and olaparib, and standard chemotherapy drugs such as melphalan, etoposide, and mitomycin, may be suitable candidates for drug repositioning for CCA and should be studied further.
The approach of the current study was to investigate established drugs to identify novel indications for cancer treatment. The results indicated that non-antineoplastic agents interacted with certain genes implicated in CCA. Cimetidine, a histamine type 2 antagonist, is used to treat heartburn and peptic ulcer; however, data also indicates that cimetidine may contribute to growth inhibition and apoptosis induction in CCA in vitro and in vivo (57). Valproic acid is used to treat bipolar disorders and prevent migraine headaches; previous study identified that it may inhibit the growth of CCA cell lines (TFK-1, QBC939 and CCLP1) by inducing cell cycle arrest and promoting cell differentiation via induction of dendrite-like structures (58). The effects of each drug may be mediated by several molecular mechanisms. For example, valproic acid, an anti-epileptic drug, appears to act primarily by histone deacetylase inhibition, and not solely by inhibition of CHEK1, CTBP1, BUB1B, trophinin-associated protein, laminin subunit gamma 2, WDHD1, FAM83B and FNDC1. For each of these drugs, further extensive studies, both in vitro and in vivo, are needed to confirm their effectiveness, molecular mechanisms and toxicity in the treatment of CCA.
Previous study (59) and the present data have demonstrated that lipid metabolism pathways may be significantly altered, and that lovastatin interacts with the dysregulated gene signatures. The lipid metabolism pathway may serve important roles in CCA growth and progression by downregulating the farnesoid × receptor and lipid metabolism pathways (59). Lovastatin is a medication used for lipid metabolic disorder, and blocks HMG-CoA reductase enzyme in cholesterol synthesis. This drug has been studied in vitro and in vivo and has been demonstrated to exert anticancer effects in CCA and enhancement of gefitinib-induced antiproliferation in resistant CCA (60–62).
Clofazimine is a drug used in the treatment of leprosy. It also has an anticancer effect and may be used for hepatocellular carcinoma (63). Certain antimalarial primaquines have been shown to block amino acid uptake in in vivo studies (64). From the present gene-drug interaction results, these drugs may have certain therapeutic roles in the context of CCA treatment; however further study is required.
COX-2 also serves an important role in CCA carcinogenesis, and is expressed at high levels in CCA tissue compared with non-tumorous adjacent tissue (65). Inhibition of COX-2 by nonsteroidal anti-inflammatory drugs, including peroxicam in combination with cisplatin, may trigger cell cycle regulation and apoptosis in different mesothelioma cell lines (MSTO-211H and NCI-H2452) (66).
The present results also revealed retinoic acid and caffeine to interact with gene signatures of the top most DEGs. Retinoic acid is categorized as a retinoid and has been studied for its therapeutic efficacy in numerous cancers. In CCA, cell migration and tumor invasion may be blocked by all trans-retinoic acid-incorporated glycol chitosan nanoparticles (67). Caffeine is a methylxanthine alkaloid related to the adenine and guanine bases. Previous reports demonstrated that caffeinated coffee consumption was associated with reduced risk of HCC and CCA (68,69). However, since a molecular mechanism underlying the potential anticancer activity of caffeine is yet to be elucidated, it is probably best utilized as a supplement in daily diet. The present research is limited as the application of molecular data based on bioinformatics analysis may not be sufficient to predict the efficacy of potential targeted agents or protein inhibitors. Therefore, validation of the current data with case studies and additional functional downstream approach experiments is necessary.
In conclusion, the present study performed gene expression analysis, and based on the findings, assessed molecular pathways and drug interactions associated with DEG signatures in CCA. The present study may be developed to further examine drug repurposing and to search for additional anticancer activities among known pharmaceuticals. The results may provide a novel hypothesis regarding the mechanisms of non-antineoplastic drugs in cancer treatment. The data may be a useful resource for preclinical and clinical research on existing FDA-approved drugs into their potential use in CCA treatment.
Acknowledgements
The authors are thankful to Dr Janice M. Wongsurawat of the Chulabhorn Research Institute (Bangkok, Thailand), for proof-reading the manuscript.
Funding
The present study was supported by the Chulabhorn Graduate Institute and Chulabhorn Research Institute (Bangkok, Thailand).
Availability of data and materials
All data used and analyzed during this study are included in this published article.
Authors' contributions
SC performed data acquisition and data analysis and contributed to the drafting of the manuscript. TS was responsible for initiation, conception, experimental design and execution of the project and for critical revision of the manuscript. TU supervised the collection of anti-cancer drug information and contributed to the revision of the manuscript. YP supervised data analysis and contributed to the revision of the manuscript. JS supervised experimental design and critical revision of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med. 1999;341:1368–1378. doi: 10.1056/NEJM199910283411807. [DOI] [PubMed] [Google Scholar]
- 2.Wu T, Han C, Lunz JG, III, Michalopoulos G, Shelhamer JH, Demetris AJ. Involvement of 85-kd cytosolic phospholipase A(2) and cyclooxygenase-2 in the proliferation of human cholangiocarcinoma cells. Hepatology. 2002;36:363–373. doi: 10.1053/jhep.2002.34743. [DOI] [PubMed] [Google Scholar]
- 3.Patel T. Worldwide trends in mortality from biliary tract malignancies. BMC Cancer. 2002;2:10. doi: 10.1186/1471-2407-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaib YH, Davila JA, McGlynn K, El-Serag HB. Rising incidence of intrahepatic cholangiocarcinoma in the United States: A true increase? J Hepatol. 2004;40:472–477. doi: 10.1016/j.jhep.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 5.Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224:463–473. doi: 10.1097/00000658-199610000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33:1353–1357. doi: 10.1053/jhep.2001.25087. [DOI] [PubMed] [Google Scholar]
- 7.Sahu S, Sun W. Targeted therapy in biliary tract cancers-current limitations and potentials in the future. J Gastrointest Oncol. 2017;8:324–336. doi: 10.21037/jgo.2016.09.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohashi K, Nakajima Y, Kanehiro H, Tsutsumi M, Taki J, Aomatsu Y, Yoshimura A, Ko S, Kin T, Yagura K, et al. Ki-ras mutations and p53 protein expressions in intrahepatic cholangiocarcinomas: Relation to gross tumor morphology. Gastroenterology. 1995;109:1612–1617. doi: 10.1016/0016-5085(95)90650-9. [DOI] [PubMed] [Google Scholar]
- 9.Furubo S, Harada K, Shimonishi T, Katayanagi K, Tsui W, Nakanuma Y. Protein expression and genetic alterations of p53 and ras in intrahepatic cholangiocarcinoma. Histopathology. 1999;35:230–240. doi: 10.1046/j.1365-2559.1999.00705.x. [DOI] [PubMed] [Google Scholar]
- 10.Tannapfel A, Sommerer F, Benicke M, Katalinic A, Uhlmann D, Witzigmann H, Hauss J, Wittekind C. Mutations of the BRAF gene in cholangiocarcinoma but not in hepatocellular carcinoma. Gut. 2003;52:706–712. doi: 10.1136/gut.52.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu X, Kobayashi S, Qiao W, Li C, Xiao C, Radaeva S, Stiles B, Wang RH, Ohara N, Yoshino T, et al. Induction of intrahepatic cholangiocellular carcinoma by liver-specific disruption of Smad4 and Pten in mice. J Clin Invest. 2006;116:1843–1852. doi: 10.1172/JCI27282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Endo K, Yoon BI, Pairojkul C, Demetris AJ, Sirica AE. ERBB-2 overexpression and cyclooxygenase-2 up-regulation in human cholangiocarcinoma and risk conditions. Hepatology. 2002;36:439–450. doi: 10.1053/jhep.2002.34435. [DOI] [PubMed] [Google Scholar]
- 13.Sugawara H, Yasoshima M, Katayanagi K, Kono N, Watanabe Y, Harada K, Nakanuma Y. Relationship between interleukin-6 and proliferation and differentiation in cholangiocarcinoma. Histopathology. 1998;33:145–153. doi: 10.1046/j.1365-2559.1998.00445.x. [DOI] [PubMed] [Google Scholar]
- 14.Chabner BA. Early accelerated approval for highly targeted cancer drugs. N Engl J Med. 2011;364:1087–1089. doi: 10.1056/NEJMp1100548. [DOI] [PubMed] [Google Scholar]
- 15.Wu T, Leng J, Han C, Demetris AJ. The cyclooxygenase-2 inhibitor celecoxib blocks phosphorylation of Akt and induces apoptosis in human cholangiocarcinoma cells. Mol Cancer Ther. 2004;3:299–307. [PubMed] [Google Scholar]
- 16.Peng YC, Lin CL, Hsu WY, Chang CS, Yeh HZ, Tung CF, Wu YL, Sung FC, Kao CH. Statins are associated with a reduced risk of cholangiocarcinoma: A population-based case-control study. Br J Clin Pharmacol. 2015;80:755–761. doi: 10.1111/bcp.12641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andersen JB, Spee B, Blechacz BR, Avital I, Komuta M, Barbour A, Conner EA, Gillen MC, Roskams T, Roberts LR, et al. Genomic and genetic characterization of cholangiocarcinoma identifies therapeutic targets for tyrosine kinase inhibitors. Gastroenterology. 2012;142:1021–1031e15. doi: 10.1053/j.gastro.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, et al. The Gene Ontology Consortium: Gene ontology: Tool for the unification of biology. Nat Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang W, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37:1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanehisa M, Goto S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Szklarczyk D, Franceschini A, Kuhn M, Simonovic M, Roth A, Minguez P, Doerks T, Stark M, Muller J, Bork P, et al. The STRING database in 2011: Functional interaction networks of proteins, globally integrated and scored. Nucleic Acids Res. 2011;39:D561–D568. doi: 10.1093/nar/gkq973. (Database) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.von Mering C, Jensen LJ, Snel B, Hooper SD, Krupp M, Foglierini sM, Jouffre N, Huynen MA, Bork P. STRING: Known and predicted protein-protein associations, integrated and transferred across organisms. Nucleic Acids Res. 2005;33:D433–D437. doi: 10.1093/nar/gki005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, et al. Cancer Genome Atlas Research Network: Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73. doi: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:11. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoo M, Shin J, Kim J, Ryall KA, Lee K, Lee S, Jeon M, Kang J, Tan AC. DSigDB: Drug signatures database for gene set analysis. Bioinformatics. 2015;31:3069–3071. doi: 10.1093/bioinformatics/btv313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lamb J, Crawford ED, Peck D, Modell JW, Blat IC, Wrobel MJ, Lerner J, Brunet JP, Subramanian A, Ross KN, et al. The Connectivity Map: Using gene-expression signatures to connect small molecules, genes, and disease. Science. 2006;313:1929–1935. doi: 10.1126/science.1132939. [DOI] [PubMed] [Google Scholar]
- 28.Qin C, Zhang C, Zhu F, Xu F, Chen SY, Zhang P, Li YH, Yang SY, Wei YQ, Tao L, et al. Therapeutic target database update 2014: A resource for targeted therapeutics. Nucleic Acids Res. 2014;42(D1):D1118–D1123. doi: 10.1093/nar/gkt1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis AP, Wiegers TC, Roberts PM, King BL, Lay JM, Lennon-Hopkins K, Sciaky D, Johnson R, Keating H, Greene N, et al. A CTD-Pfizer collaboration: Manual curation of 88,000 scientific articles text mined for drug-disease and drug-phenotype interactions. Database (Oxford) 2013;2013:bat080. doi: 10.1093/database/bat080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silsirivanit A, Sawanyawisuth K, Riggins GJ, Wongkham C. Cancer biomarker discovery for cholangiocarcinoma: The high-throughput approaches. J Hepatobiliary Pancreat Sci. 2014;21:388–396. doi: 10.1002/jhbp.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Massey AJ. Tumour growth environment modulates Chk1 signalling pathways and Chk1 inhibitor sensitivity. Sci Rep. 2016;6:35874. doi: 10.1038/srep35874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang L, Feng S, Yang Y. Identification of transcription factors (TFs) and targets involved in the cholangiocarcinoma (CCA) by integrated analysis. Cancer Gene Ther. 2016;23:439–445. doi: 10.1038/cgt.2016.64. [DOI] [PubMed] [Google Scholar]
- 33.Seubwai W, Kraiklang R, Wongkham C, Wongkham S. Hypoxia enhances aggressiveness of cholangiocarcinoma cells. Asian Pac J Cancer Prev. 2012;13:53–58. (Suppl): [PubMed] [Google Scholar]
- 34.Borad MJ, Champion MD, Egan JB, Liang WS, Fonseca R, Bryce AH, McCullough AE, Barrett MT, Hunt K, Patel MD, et al. Integrated genomic characterization reveals novel, therapeutically relevant drug targets in FGFR and EGFR pathways in sporadic intrahepatic cholangiocarcinoma. PLoS Genet. 2014;10:e1004135. doi: 10.1371/journal.pgen.1004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tongtawee T, Kaewpitoon SJ, Loyd R, Chanvitan S, Leelawat K, Praditpol N, Jujinda S, Kaewpitoon N. High expression of matrix metalloproteinase-11 indicates poor prognosis in human cholangiocarcinoma. Asian Pac J Cancer Prev. 2015;16:3697–3701. doi: 10.7314/APJCP.2015.16.9.3697. [DOI] [PubMed] [Google Scholar]
- 36.Severino FE, Hasimoto CN, Rodrigues MAM, Llanos JC, Reis PP. Integrative analysis of transcriptome and microRNome profiles in cholangiocarcinoma. J Cancer Sci Ther. 2017;09:580–588. doi: 10.4172/1948-5956.1000477. [DOI] [Google Scholar]
- 37.Navaneethan U, Lourdusamy V, Gk Venkatesh P, Willard B, Sanaka MR, Parsi MA. Bile proteomics for differentiation of malignant from benign biliary strictures: A pilot study. Gastroenterol Rep (Oxf) 2015;3:136–143. doi: 10.1093/gastro/gou066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang QX, Cui JY, Ma H, Jia XM, Huang FL, Jiang LX. Screening of potential biomarkers for cholangiocarcinoma by integrated analysis of microarray data sets. Cancer Gene Ther. 2016;23:48–53. doi: 10.1038/cgt.2015.66. [DOI] [PubMed] [Google Scholar]
- 39.Smith J, Tho ML, Xu N, Gillespie DA. The ATM-Chk2 and ATR-Chk1 pathways in DNA damage signaling and cancer. Adv Cancer Res. 2010. pp. 73–112. [DOI] [PubMed]
- 40.Bartek J, Lukas J. Chk1 and Chk2 kinases in checkpoint control and cancer. Cancer Cell. 2003;3:421–429. doi: 10.1016/S1535-6108(03)00110-7. [DOI] [PubMed] [Google Scholar]
- 41.Kuroki T, Tomioka T, Tajima Y, Inoue K, Ikematsu Y, Ichinose K, Furui J, Kanematsu T. Detection of the pancreas-specific gene in the peripheral blood of patients with pancreatic carcinoma. Br J Cancer. 1999;81:350–353. doi: 10.1038/sj.bjc.6690699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nath A, Chan C. Genetic alterations in fatty acid transport and metabolism genes are associated with metastatic progression and poor prognosis of human cancers. Sci Rep. 2016;6:18669. doi: 10.1038/srep18669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen Y, Li P. Fatty acid metabolism and cancer development. Sci Bull (Beijing) 2016;61:1473–1479. doi: 10.1007/s11434-016-1129-4. [DOI] [Google Scholar]
- 44.Sung J, Wang Y, Chandrasekaran S, Witten DM, Price ND. Molecular signatures from omics data: From chaos to consensus. Biotechnol J. 2012;7:946–957. doi: 10.1002/biot.201100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu P, Aliabadi HM, Uludağ H, Han J. Identification of potential drug targets in cancer signaling pathways using stochastic logical models. Sci Rep. 2016;6:23078. doi: 10.1038/srep23078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mann BS, Johnson JR, He K, Sridhara R, Abraham S, Booth BP, Verbois L, Morse DE, Jee JM, Pope S, et al. Vorinostat for treatment of cutaneous manifestations of advanced primary cutaneous T-cell lymphoma. Clin Cancer Res. 2007;13:2318–2322. doi: 10.1158/1078-0432.CCR-06-2672. [DOI] [PubMed] [Google Scholar]
- 47.Audeh MW, Carmichael J, Penson RT, Friedlander M, Powell B, Bell-McGuinn KM, Scott C, Weitzel JN, Oaknin A, Loman N, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: A proof-of-concept trial. Lancet. 2010;376:245–251. doi: 10.1016/S0140-6736(10)60893-8. [DOI] [PubMed] [Google Scholar]
- 48.Wood L. Sunitinib malate for the treatment of renal cell carcinoma. Expert Opin Pharmacother. 2012;13:1323–1336. doi: 10.1517/14656566.2012.689130. [DOI] [PubMed] [Google Scholar]
- 49.Roskoski R., Jr RAF protein-serine/threonine kinases: Structure and regulation. Biochem Biophys Res Commun. 2010;399:313–317. doi: 10.1016/j.bbrc.2010.07.092. [DOI] [PubMed] [Google Scholar]
- 50.Ma J, Shi J, Zhao D, Cheng L, Wang W, Li F, Jiang X, Jiang H. Raf kinase inhibitor protein inhibits cholangiocarcinoma cell metastasis by downregulating matrix metalloproteinase 9 and upregulating tissue inhibitor of metalloproteinase 4 expression. Oncol Lett. 2015;9:15–24. doi: 10.3892/ol.2014.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dreyer C, Sablin MP, Bouattour M, Neuzillet C, Ronot M, Dokmak S, Belghiti J, Guedj N, Paradis V, Raymond E, et al. Disease control with sunitinib in advanced intrahepatic cholangiocarcinoma resistant to gemcitabine-oxaliplatin chemotherapy. World J Hepatol. 2015;7:910–915. doi: 10.4254/wjh.v7.i6.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eckmann KR, Patel DK, Landgraf A, Slade JH, Lin E, Kaur H, Loyer E, Weatherly JM, Javle M. Chemotherapy outcomes for the treatment of unresectable intrahepatic and hilar cholangiocarcinoma: A retrospective analysis. Gastrointest Cancer Res. 2011;4:155–160. [PMC free article] [PubMed] [Google Scholar]
- 53.Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, et al. ABC-02 Trial Investigators: Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 54.Merla A, Liu KG, Rajdev L. Targeted therapy in biliary tract cancers. Curr Treat Options Oncol. 2015;16:48. doi: 10.1007/s11864-015-0366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruzzenente A, Fassan M, Conci S, Simbolo M, Lawlor RT, Pedrazzani C, Capelli P, D'Onofrio M, Iacono C, Scarpa A, et al. Cholangiocarcinoma heterogeneity revealed by multigene mutational profiling: Clinical and prognostic relevance in surgically resected patients. Ann Surg Oncol. 2016;23:1699–1707. doi: 10.1245/s10434-015-5046-6. [DOI] [PubMed] [Google Scholar]
- 56.Brandi G, Farioli A, Astolfi A, Biasco G, Tavolari S. Genetic heterogeneity in cholangiocarcinoma: A major challenge for targeted therapies. Oncotarget. 2015;6:14744–14753. doi: 10.18632/oncotarget.4539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dana P, Vaeteewoottacharn K, Kariya R, Matsuda K, Wongkham S, Okada S. Repurposing cimetidine for cholangiocarcinoma: Antitumor effects in vitro and in vivo. Oncol Lett. 2017;13:1432–1436. doi: 10.3892/ol.2017.5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang B, Yang R, Wu Y, Li H, Hu Z, Chen Y, Zou S. Sodium valproate inhibits the growth of human cholangiocarcinoma in vitro and in vivo. Gastroenterol Res Pract. 2013;2013:374593. doi: 10.1155/2013/374593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kwee SA, Okimoto GS, Chan OTM, Tiirikainen M, Wong LL. Metabolic characteristics distinguishing intrahepatic cholangiocarcinoma: A negative pilot study of (18)F-fluorocholine PET/CT clarified by transcriptomic analysis. Am J Nucl Med Mol Imaging. 2016;6:73–83. [PMC free article] [PubMed] [Google Scholar]
- 60.Yang SH, Lin HY, Chang VHS, Chen CC, Liu YR, Wang J, Zhang K, Jiang X, Yen Y. Lovastatin overcomes gefitinib resistance through TNF-α signaling in human cholangiocarcinomas with different LKB1 statuses in vitro and in vivo. Oncotarget. 2015;6:23857–23873. doi: 10.18632/oncotarget.4408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang SH, Lin HY, Changou CA, Chen CH, Liu YR, Wang J, Jiang X, Luh F, Yen Y. Integrin β3 and LKB1 are independently involved in the inhibition of proliferation by lovastatin in human intrahepatic cholangiocarcinoma. Oncotarget. 2016;7:362–373. doi: 10.18632/oncotarget.6238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim BB, Kim M, Park JB. The effects of lovastatin on the morphology, cell viability and differentiation of stem cells derived from gingiva. Biomed Res (Aligarh) 2017;28:4922–4927. [Google Scholar]
- 63.Ruff P, Chasen MR, Long JEH, van Rensburg CE. A phase II study of oral clofazimine in unresectable and metastatic hepatocellular carcinoma. Ann Oncol. 1998;9:217–219. doi: 10.1023/A:1008204911774. [DOI] [PubMed] [Google Scholar]
- 64.Das AK. Anticancer effect of antimalarial artemisinin compounds. Ann Med Health Sci Res. 2015;5:93–102. doi: 10.4103/2141-9248.153609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chariyalertsak S, Sirikulchayanonta V, Mayer D, Kopp-Schneider A, Fürstenberger G, Marks F, Müller-Decker K. Aberrant cyclooxygenase isozyme expression in human intrahepatic cholangiocarcinoma. Gut. 2001;48:80–86. doi: 10.1136/gut.48.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Verdina A, Cardillo I, Nebbioso A, Galati R, Menegozzo S, Altucci L, Sacchi A, Baldi A. Molecular analysis of the effects of piroxicam and cisplatin on mesothelioma cells growth and viability. J Transl Med. 2008;6:27. doi: 10.1186/1479-5876-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 67.Chung KD, Jeong YI, Chung CW, Kim DH, Kang DH. Anti-tumor activity of all-trans retinoic acid-incorporated glycol chitosan nanoparticles against HuCC-T1 human cholangiocarcinoma cells. Int J Pharm. 2012;422:454–461. doi: 10.1016/j.ijpharm.2011.10.057. [DOI] [PubMed] [Google Scholar]
- 68.Petrick JL, Freedman ND, Graubard BI, Sahasrabuddhe VV, Lai GY, Alavanja MC, Beane-Freeman LE, Boggs DA, Buring JE, Chan AT, et al. Coffee consumption and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma by sex: The liver cancer pooling project. Cancer Epidemiol Biomarkers Prev. 2015;24:1398–1406. doi: 10.1158/1055-9965.EPI-15-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kennedy OJ, Roderick P, Buchanan R, Fallowfield JA, Hayes PC, Parkes J. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: A systematic review and dose-response meta-analysis. BMJ Open. 2017;7:e013739. doi: 10.1136/bmjopen-2016-013739. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used and analyzed during this study are included in this published article.