Abstract
Purpose
In this study, we evaluated the anticancer activity of non-steroidal anti-inflammatory drugs (NSAIDs) in BxPC-3 and MIA PaCa-2 pancreatic cancer cell cultures.
Methods
To test the effect of compounds on the viability of cells, the MTT assay was used. The activity of NSAIDs in 3D cell cultures was evaluated by measuring the size change of spheroids. The type of cell death was identified by cell staining with Hoechst 33342 and propidium iodide. To evaluate the effect on the colony-forming ability of cancer cells, the clonogenic assay was used.
Results
Five out of seven tested NSAIDs reduced the viability of BxPC-3 and MIA PaCa-2 cancer cells. Fenamates were more active against cyclooxygenase-2 expressing BxPC-3 than cyclooxygenase-2 non-expressing MIA PaCa-2 cell line. Fenamates and coxibs exerted higher activity in monolayer cultured cells, whereas salicylates were more active in 3D cultures. Fenamates and coxibs induced dose-dependent apoptosis and necrosis. NSAIDs also inhibited the colony-forming ability of cancer cells. Meclofenamic acid, niflumic acid, and parecoxib possessed higher activity on BxPC-3, and celecoxib possessed higher activity on MIA PaCa-2 cell colony formation.
Conclusion
Our results show that fenamates, coxibs, and salicylates possess anticancer activity on human pancreatic cancer BxPC-3 and MIA PaCa-2 cell cultures.
Keywords: anticancer activity, viability, spheroid, apoptosis, clonogenic assay
Introduction
Despite the progress in chemotherapy, during the past decades, pancreatic cancer mortality rate has been increasing and it is still one of the deadliest types of cancer.1 Five-year relative survival for pancreatic cancer is around 8%.2 This is mainly because more than half of pancreatic cancer cases are diagnosed only in the late stages of the disease. However, the survivability of patients diagnosed with local cancer is only 15%.3–5 Another important reason why treatment of this type of cancer has limited success is resistance to chemotherapy.5,6
Epidemiological studies have shown that there is a link between inflammatory processes and cancer development.7–9
One way to reduce inflammation is the inhibition of cyclooxygenase (COX). Non-steroidal anti-inflammatory drugs (NSAIDs) by this mechanism not only reduce inflammation, but also inhibit processes associated with cancer initiation and development, such as DNA synthesis, cell proliferation, apoptosis, angiogenesis, and migration.10 However, there are evidences showing that NSAIDs can exert their anticancer activity through COX-independent mechanisms. According to some research, the derivative of selective COX-2 inhibitor celecoxib, 2,5-dimethyl-celecoxib, which lacks COX inhibitory properties, still retains antiproliferative activity, triggers apoptosis, and reduces cancer cells migration and invasion.11–13 Other mechanisms include activation of cyclic guanosine monophosphate-dependent protein kinase,14,15 activation of peroxisome proliferator-activated receptors,16 inhibition of 3-phosphoinositide-dependent kinase-1,17 or downregulation of matrix metalloproteinases.18
Many clinical trials have been conducted to test the anticancer activity of NSAIDs. However, there are only few clinical trials dedicated to test NSAID application for the treatment of pancreatic cancer and majority of them focus on NSAID activity in combination with anticancer drugs.19
The aim of the study was to evaluate an anticancer activity of seven selective and non-selective COX inhibitors and compare the effects between salicylate (non-selective),20 fenamate (mecofenamic acid non-selective and mefenamic and niflumic acid selective COX-2),20 and coxib (selective COX-2)20,21 groups (Table 1). In order to investigate whether the effect of NSAIDs on cancer cells is COX-dependent, we chose two different cancer cell lines – COX-2 expressing BxPC-3 and non-expressing MIA PaCa-2. The anticancer activity was evaluated in 2D (the ability to inhibit cell proliferation, colony formation) and 3D cancer cell cultures (the activity on spheroid growth).
Table 1.
Selectivity and inhibitory activity of NSAIDs for COX-1 and COX-2
| NSAIDs | Selectivity | EC50 (µM)
|
COX-1/COX-2 | |
|---|---|---|---|---|
| COX-1 | COX-2 | |||
| Acetylsalicylic acid | Non-selective | 1.7–4.5* | >100* | >100 |
| Salicylic acid (as sodium salt) | Non-selective | 4956* | 34440* | 0.1 |
| Mefenamic acid | Selective COX-2 | 25* | 2.9* | 8.6 |
| Meclofenamic acid | Non-selective | 0.2* | 0.7* | 0.2 |
| Niflumic acid | Selective COX-2 | 25* | 5.4* | 4.6 |
| Celecoxib | Selective COX-2 | 1.2* | 0.83* | 1.4 |
| Valdecoxib (active metabolite of parecoxib) | Selective COX-2 | 21.9** | 0.2** | 109.5 |
Materials and methods
Drugs
Acetylsalicylic acid, salicylic acid, niflumic acid, mefenamic acid, and meclofenamic acid were obtained from Sigma-Aldrich Co. (St. Louis, MO, USA), celecoxib was obtained from Cayman Chemical (Ann Arbor, MI, USA), parecoxib from Fluka Analytical (Munich, Germany). Stocks of compounds were prepared in dimethyl sulfoxide (100 mM concentrations of fenamates and salicylates, and 20 mM concentrations of coxibs) and stored at +4°C in a refrigerator until biological experiments. Dilutions in media were prepared fresh just before the assays.
Cell culture
Human pancreatic cancer cell lines BxPC-3 and MIA PaCa-2 were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). Cells were grown in DMEM Glutamax medium (Gibco, Carlsbad, CA, USA) containing 10% fetal bovine serum and 1% antibiotic mixture (10,000 U/mL penicillin and 10 mg/mL streptomycin; Gibco). Human foreskin fibroblasts CRL-4001 (ATCC) were kindly provided by Dr. Ramūnas Valiokas (Center for Physical Sciences and Technology, Department of Nanoengineering, Institute of Physics). Fibroblasts were grown in Medium 106 with Low Serum Growth Supplement (Gibco). All cells were incubated at 37°C in a humidified atmosphere containing 5% CO2.
Cell viability assay
The viability of cells treated with NSAIDs was determined by MTT (Sigma-Aldrich Co.) assay. BxPC-3 and MIA PaCa-2 cells were plated (5000 cells/well) in 96-well plate and incubated overnight at 37°C in a humidified atmosphere containing 5% CO2. Cells were affected by various concentrations of NSAIDs (from 500 to 3.13 μM). As positive control, only medium without cells was used and the medium with 0.5% DMSO (Sigma-Aldrich Co.) served as a negative control. After 24, 48, and 72 h of incubation with drugs, 20 μL of MTT (5 mg/mL) was added into each well and incubated for 4 h under the same conditions. The supernatant was removed and 100 μL DMSO was added. The absorbance was measured at 570 and 630 nm, and EC50 (half maximal effective concentration of a drug at which 50% of its maximum response is observed) values were calculated.
Spheroid assay
Spheroids were formed by the 3D bioprinting method from BxPC-3, MIA PaCa-2 cells mixed with human fibroblasts (1:1) to better imitate the tumor microenvironment. Cells were incubated with nanoparticles NanoShuttle (Nano3D Biosciences Inc., Houston, TX, USA) for 8–10 h at 37°C in a humidified atmosphere containing 5% CO2. Then cells were plated in ultra-low attachment 96-well plates (2000 cancer cells and 2000 fibroblasts/well), placed on a magnetic drive and incubated for 48 h, until spheroids were formed. Then the medium was replaced by the fresh one containing 5 and 20 μM of NSAIDs. The phase-contrast images of spheroids were taken using an inverted microscope Olympus IX73 (Olympus, Tokyo, Japan). The effect of NSAIDs on cancer spheroids was evaluated by their differences in size, measuring the change of diameter with ImageJ program (National Institutes of Health, Bethesda, MD, USA).
Apoptosis and necrosis assay
BxPC-3 and MIA PaCa-2 cells were seeded in 24-well plate (15,000 cells/well) and incubated at 37°C in a humidified atmosphere containing 5% CO2. After 24 h, 90%, 50%, and 10% of EC50 of NSAIDs were added to the wells and incubated for 72 h. Then 3 μL Hoechst 33342 (1 mg/mL; Invitrogen, Paisley, UK) and 1 μL propidium iodide (1 mg/mL, Invitrogen) were added to each well and cells were incubated for 10 min. Images were taken using inverted fluorescent microscope (Olympus IX73). Apoptotic and necrotic cells were counted and the percentage number of cells was calculated.
Clonogenic assay
BxPC-3 and MIA PaCa-2 cells were plated in 12-well plate (100 cells/well) and treated with 100% and 10% of EC50 of NSAIDs. Medium containing 0.2% of DMSO served as a negative control. BxPC-3 cells were incubated for 12 days and MIA PaCa-2 for 14 days at 37°C in an atmosphere containing 5% CO2. Then the colonies were fixed with 4% paraformaldehyde (Thermo Scientific, Waltham, MA, USA) and stained with 0.1% crystal violet (Sigma-Aldrich Co.). The photos of the colonies were taken with G:Box gel documentation system (Syngene International Ltd., Bengaluru, India) and analyzed using Genesys software (Syngene International Ltd.) by calculating the number and the area of colonies.
Statistical analysis
All values are shown as the mean ± SD. p-values were calculated using Student’s t-test. A value of p<0.05 was considered as the level of significance. Correlation between results in 2D and 3D cell cultures was measured using Pearson’s correlation coefficient r, evaluating the strength of relationship and verifying the reliability.
Results
Coxibs and fenamates reduce the viability of pancreatic cancer BxPC-3 and MIA PaCa-2 cell lines
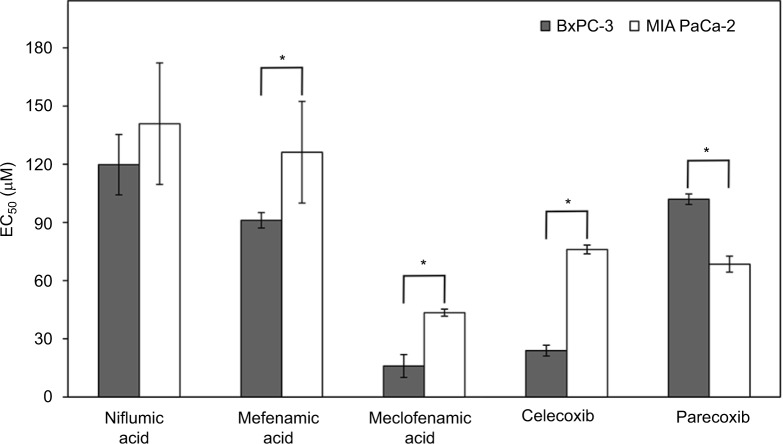
The most potent drug against both cancer cell lines was meclofenamic acid (EC50 16.0±5.9 μM against BxPC-3 and 43.5±1.8 μM against MIA PaCa-2 cells; Figure 1). Meanwhile, salicylates (aspirin and salicylic acid) had no effect on the viability of BxPC-3 and MIA PaCa-2 cells. Coxibs and fenamates possessed higher antiproliferative activity against BxPC-3 than MIA PaCa-2 cell line. The EC50 for celecoxib in BxPC-3 cell line was 23.9±2.8 μM. Parecoxib moderately decreased the viability of BxPC-3 cells, its EC50 value was 4 times higher than that one of celecoxib (102.0±2.7 μM). On the other hand, parecoxib was more active in MIA PaCa-2 cell line than celecoxib (EC50 68.5±4.2 μM and 76.1±2.3 μM, respectively).
Figure 1.
The effect of NSAIDs on the viability of BxPC-3 and MIA PaCa-2 cells.
Notes: The most potent COX inhibitor meclofenamic acid showed the highest antiproliferative activity on both BxPC-3 and MIA PaCa-2 cell line (EC50 values after 72 h of drug exposure were 16,0 μM for BxPC-3 and, 43,5 μM for MIA PaCa-2 cells). The rank order of the activity of tested NSAIDs on BxPC-3 cell viability was as follows: meclofenamic acid>celecoxib>mefenamic acid>parecoxib>niflumic acid; on MIA PaCa-2 cell viability: meclofenamic acid>parecoxib>celecoxib>mefenamic acid=niflumic acid. Acetylsalicylic acid and salicylic acid had no effect on the viability of cancer cells (data not shown). The asterisks (*) indicate p<0.05.
Abbreviations: EC50, half maximal effective concentration; NSAIDs, non-steroidal anti-inflammatory drugs.
It was also found, that the cell survival rate was time dependent – it decreased over time.
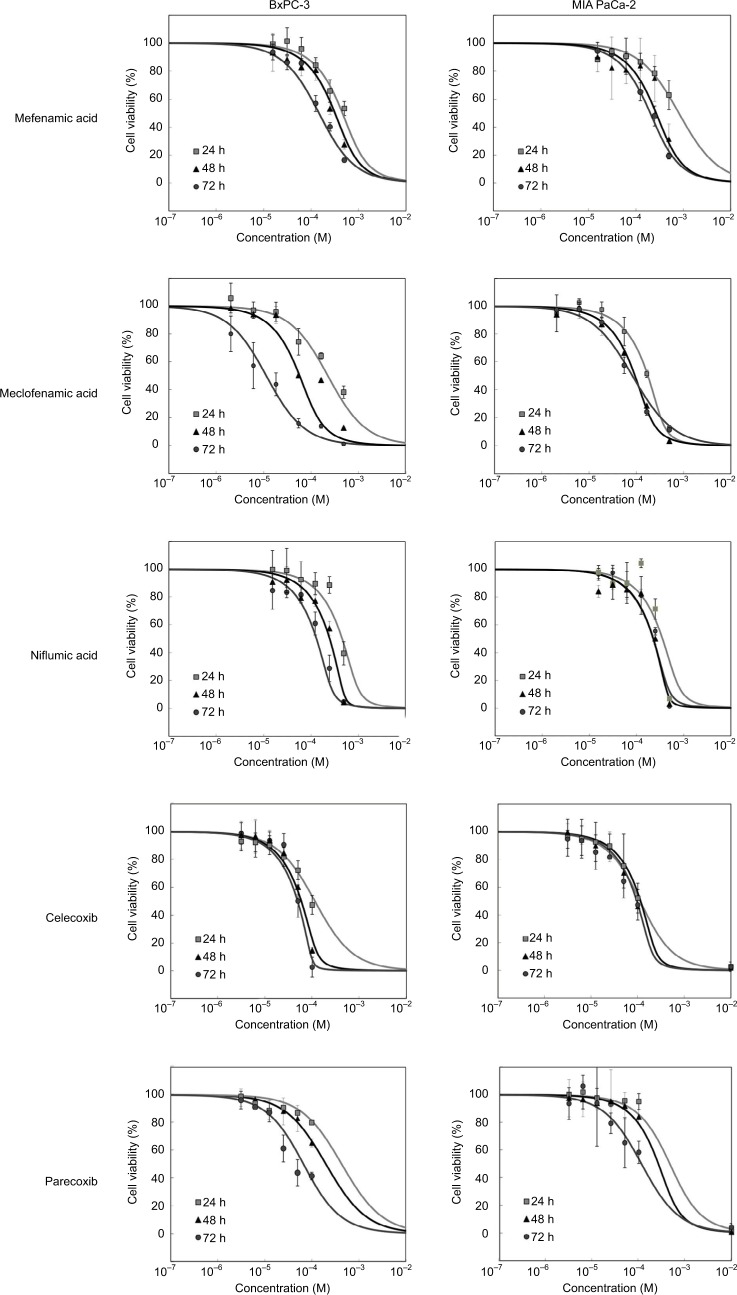
Fenamates and coxibs exerted time-dependent anti-proliferative effect, though the differences between EC50 value after 48 and 72 h of incubation changed only 1.5–1.9 times for all compounds except parecoxib in MIA Paca-2 cell line, while in BxPC-3, those changes varied from 1.5 to 3.2 times (p<0.05; Figure 2).
Figure 2.
The changes in cell viability after 24, 48, and 72 h of incubation with fenamates and coxibs.
Notes: Salicylates had no effect on viability of both pancreatic cell lines at tested concentrations (up to 500 μM). Fenamates and coxibs exerted time-dependent anti-proliferative effect, though EC50 values against MIA Paca-2 cell line were more consistent after 24 and 72 h compared to BxPC-3 cell line, especially for niflumic acid, meclofenamic acid and celecoxib (p>0.05).
Abbreviation: EC50, half maximal effective concentration.
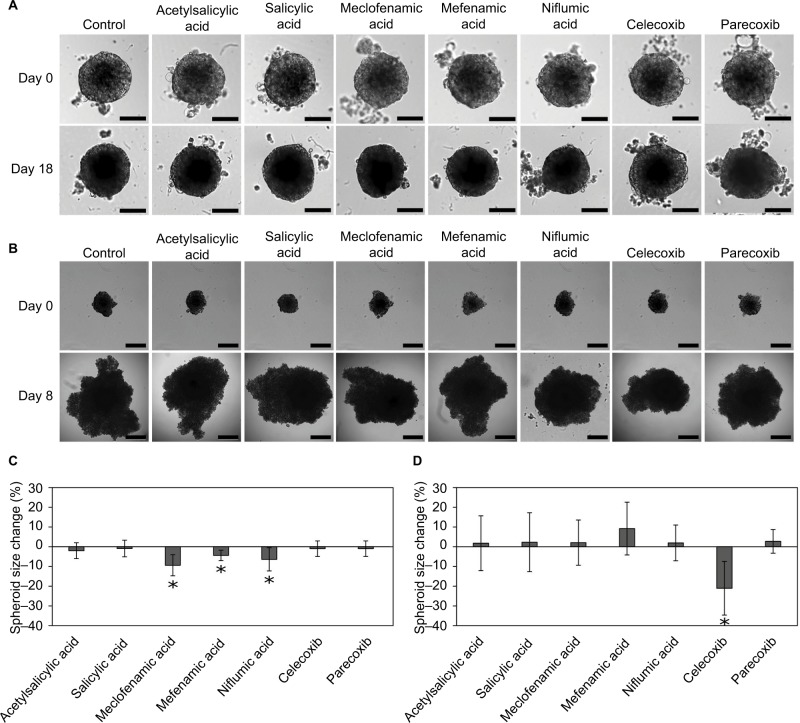
NSAIDs reduce the growth of pancreatic cancer cell spheroids
3D cell cultures were less sensitive to NSAID treatment compared with the cells growing in monolayer (Figure 3A–D). Fenamates had the strongest effect on the BxPC-3 spheroid growth. However, after incubation with 20 μM of these drugs for 10 days, the spheroid diameter was only 4.6%–9.9% smaller when compared with the control (Figure 3A and C). Also, all fenamates did not reduce the growth of MIA PaCa-2 spheroids.
Figure 3.
Spheroid size after incubation with NSAIDs.
Notes: BxPC-3 spheroids after incubation with 20 μM NSAIDs, magnification 100× (A). MIA PaCa-2 spheroids after incubation with 20 μM NSAIDs, magnification 40× (B). BxPC-3 spheroid diameter after incubation with NSAIDs for 18 days (C). BxPC-3 and MIA PaCa-2 spheroid size change after incubation with NSAIDs for 10 days (D). The asterisks (*) indicate p<0.05.
Abbreviations: EC50, half maximal effective concentration; NSAIDs, non-steroidal anti-inflammatory drugs.
Even though meclofenamic acid exerted the strongest antiproliferative activity in 2D cell cultures, this drug showed no effect on the spheroid growth. Mefenamic acid and parecoxib did not reduce the spheroid growth, too.
It is also worth noticing, that celecoxib had the opposite effect on BxPC-3 3D cultures. The diameter of spheroids incubated with celecoxib after 18 days of incubation was bigger compared with the control (data not shown). However, only 20 μM of celecoxib showed inhibitory effect on MIA PaCa-2 spheroid growth after 11 days treatment. It reduced the size of spheroids by 21% compared with the control (p<0.05; Figure 3B and D) and was the only active compound in MIA Paca-2 3D cell cultures.
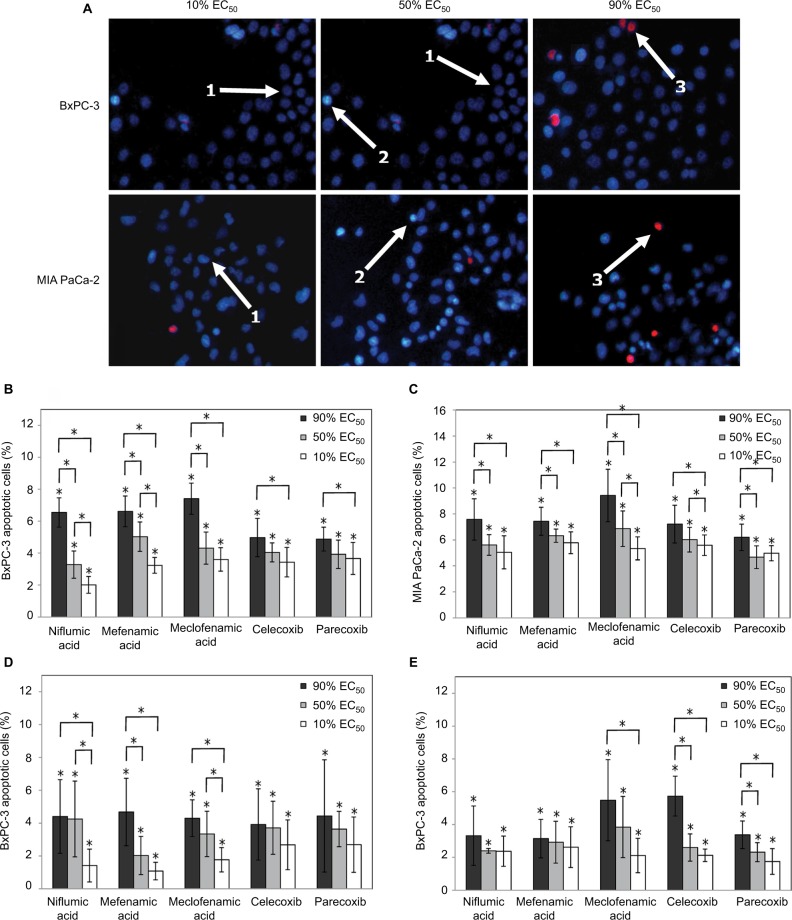
Coxibs and fenamates induce apoptosis rather than necrosis in pancreatic cancer BxPC-3 and MIA PaCa-2 cell lines
Since salicylates showed no effect on the cell viability in 2D cultures, apoptosis and necrosis assay were performed only with coxibs and fenamates. These drugs induced dose-dependent BxPC-3 and MIA PaCa-2 cells apoptosis and necrosis. 15 μM meclofenamic acid (90% EC50) had the strongest apoptosis-inducing effect on BxPC-3 cells – the percentage of apoptotic cells was 7.4% (Figure 4A). The effect of other fenamates, niflumic acid and mefenamic acid, in BxPC-3 cell line was similar (6.5% of apoptotic cells; Figure 4B). Coxibs effect on apoptosis of BxPC-3 cells was lower than fenamates.
Figure 4.
Apoptosis and necrosis by NSAIDs in BxPC-3 and MIA PaCa-2 cell lines.
Notes: BxPC-3 and MIA PaCa-2 cells after incubation with meclofenamic acid (1, viable cells; 2, apoptotic cells; and 3, necrotic cells); cells were stained with Hoechst 33342 and propidium iodide; magnification 100× (A). Effect of NSAIDs on apoptosis of BxPC-3 cells (B). Effect of NSAIDs on apoptosis of MIA PaCa-2 cells (C). The percentage of necrotic cells in BxPC-3 cell line (D). The percentage of necrotic cells in MIA PaCa-2 cell line (E). The asterisks (*) indicate p<0.05.
Abbreviations: EC50, half maximal effective concentration; NSAIDs, non-steroidal anti-inflammatory drugs.
Fenamates were the most potent compounds against MIA PaCa-2 cells as well (Figure 4C). After treatment with the highest concentration of meclofenamic acid (40 μM) apop-tosis was induced in 9.4% cells. Coxibs activity against MIA PaCa-2 cells was a bit lower.
Necrosis-inducing effect of both coxibs and fenamates on BxPC-3 and MIA PaCa-2 cells was similar (Figure 4D and E). The amount of necrotic cells in both cell lines varied between 3.1% and 5.7%.
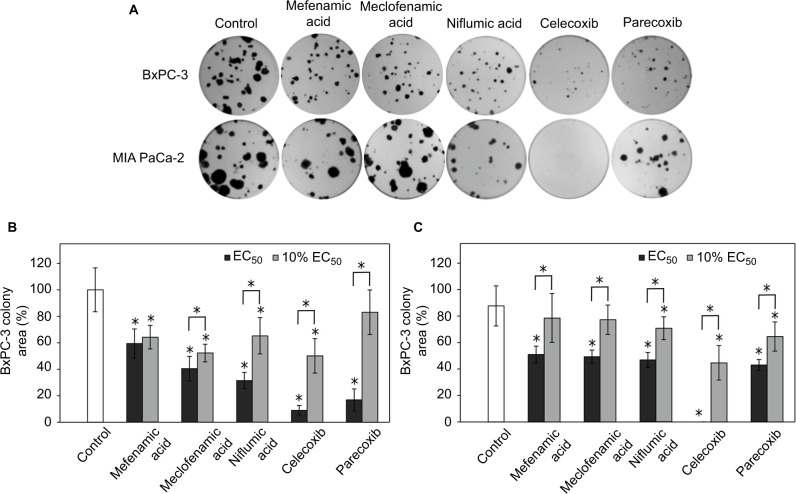
Coxibs and fenamates inhibit colony formation of BxPC-3 and MIA PaCa-2 cells
Coxibs and fenamates exerted different effect on pancreatic cancer cell colony formation. Coxibs, compared with fenamates, had the strongest activity against both BxPC-3 and MIA PaCa-2 cells (Figure 5A). After treatment with celecoxib, BxPC-3 cell colonies were 11 times smaller when compared with control. Parecoxib reduced the size of colonies 6 times in comparison with control (Figure 5B). Meanwhile, niflumic acid and meclofenamic acid reduced the area of colonies 3 and 2.5 times, respectively. Also, celecoxib reduced the number of BxPC-3 colonies by half, while fenamates showed no effect on this parameter.
Figure 5.
Inhibition of clonogenicity of BxPC-3 and MIA PaCa-2 cell lines by NSAIDs.
Notes: BxPC-3 and MIA PaCa-2 colonies after incubation with the highest concentrations (100% EC50) of the most active NSAIDs (A). Effect of NSAIDs on colony formation of BxPC-3 cells (B). Effect of NSAIDs on colony formation of MIA PaCa-2 cells (C). The asterisks (*) indicate p<0.05.
Abbreviations: EC50, half maximal effective concentration; NSAIDs, nonsteroidal anti-inflammatory drugs.
The effect of NSAIDs on the colony formation of both pancreatic cancer cell lines MIA PaCa-2 and BxPC-3 was similar (Figure 5C). MIA PaCa-2 cells were less sensitive to drug treatment, except for celecoxib and mefenamic acid. Celecoxib completely inhibited MIA PaCa-2 colony growth. Fenamates inhibitory effect was similar to parecoxib, these drugs reduced the area of MIA PaCa-2 cells about 1.5 times.
Discussion
Our study showed that two out of seven NSAIDs, namely acetylsalicylic and salicylic acid, exerted no antiprolifera-tive activity against BxPC-3 and MIA PaCa-2 pancreatic cancer cell lines. Ou et al reported that acetylsalicylic acid inhibits the viability of PANC-1 cell line only at high drug concentrations (2–4 mM).22 In the present study, we used much lower acetylsalicylic acid and salicylic acid concentrations (15.6–500 μM) and this could explain why salicylates did not exhibit antiproliferative properties. Fenamates and celecoxib had stronger effect on the viability of BxPC-3 cell line compared with MIA PaCa-2 cells. It might be related to the fact, that neither COX-1 nor COX-2 are expressed in MIA PaCa-2 cell line whereas BxPC-3 expresses both of them.21 However, differences between EC50 values show that individual NSAIDs might have distinct mechanism of action. EC50 concentrations of NSAIDs, that inhibit 50% of COX-1, are mainly in the range of 0.04–140 μM and EC50 concentrations for COX-2 – 0.04–66 μM.23–25 Even though we did not measure the activity of COX, in our study, we used 3.1–500 μM concentrations of drugs; therefore, it is likely that COX was inhibited almost in all cases.
Most of the anticancer activity experiments are conducted in monolayer cultured cells. However, 2D cell models do not reflect tumor microenvironment, whereas spheroids represent biological and physicochemical properties of tumor more accurately. They better mimic in vivo interactions between cancer cells, gradients of oxygen, and nutrients. Also, similarly as in the real tumor, drugs cannot easily penetrate the spheroids.26 These factors have a big influence on efficacy of drugs and might be one of the main reasons of cancer resistance to the treatment.27 Pancreatic cancer cells in normal conditions do not easily form spheroid structures. MIA PaCa-2 cells have weak aggregation properties and special conditions are needed to form 3D cultures.28 BxPC-3 cells form compact spheroids with a well-defined contour, but cells start to separate from spheroid soon and 3D structure might collapse.27,29 Therefore, to improve cell aggregation and stability of 3D cultures, in this study, we formed spheroids together with fibroblasts. Furthermore, non-cancer cells, like fibroblasts, endothelial, and immune cells also play an important role on cell signaling, tumor growth, and development.30
In 2D model, niflumic and mefenamic acids had low effect on the viability of BxPC-3 cells, but these drugs exerted the strongest inhibitory activity on BxPC-3 spheroid growth together with meclofenamic acid. Salicylates did not show any effect both in 2D and 3D cell cultures at used concentrations (up to 500 μM). On the other hand, meclofenamic acid, which exhibited the highest antiproliferative properties in BxPC-3 cell line, had a similar effect on spheroid growth as niflumic acid, though its EC50 value in BxPC-3 cell monolayer was about 7.5 times higher. Similarly, Cui et al reported that the effect of celecoxib on liver cancer Hep G2 spheroids was much lower than in monolayer cultured cells. EC50 value of celecoxib in 3D cell culture was 60.6±15.9 μM whereas in 2D cell culture it was 31.0±12.4 μM.31 The reason behind these differences of drug activity between 2D and 3D cell cultures might be distinct mechanism of actions.
In our study, NSAIDs triggered both pancreatic cancer cell apoptosis and necrosis in a dose-dependent manner, but the rate of apoptosis was greater than that of necrosis. However, there were a small amount of necrotic and apoptotic cells, and higher drug concentrations are needed to achieve stronger effect on cell apoptosis and necrosis.32 Ding et al reported that after treating PANC-1 cells with 1 μM celecoxib, apoptosis was induced in 4% of cells, and after treatment with 10 μM celecoxib it was induced in 12%. This effect was also dose-dependent.33
Fenamates and coxibs inhibited the clonogenicity of pancreatic cancer cells. Parecoxib, meclofenamic acid, and niflumic acid were more active against BxPC-3 and celecoxib against MIA PaCa-2 cells. Even though celecoxib is a selective COX-2 inhibitor, the anticancer mechanism of action in MIA PaCa-2 cell line could be COX-2 independent. Xu et al reported that celecoxib inhibited colon cancer HCT116 cell colony formation and the mechanism of action was COX-2 independent.34 Therefore, we presume that NSAIDs reduce colony formation not only through the inhibition of COX-2, but also that some other COX-independent mechanisms may be involved.
Conclusion
Our results show that NSAIDs inhibit pancreatic cancer spheroids growth. Fenamates and coxibs also inhibit pancreatic cancer cell viability, formation of colonies, and induce apoptosis and necrosis in dose-dependent manner. Since NSAIDs were active against both COX-2 expressing and non-expressing cell lines, it implies that these drugs may act also through COX-independent mechanisms.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KM, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.Stan SD, Singh SV, Brand RE. Chemoprevention strategies for pancreatic cancer. Nat Rev Gastroenterol Hepatol. 2010;7:347–356. doi: 10.1038/nrgastro.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 5.Iovanna J, Mallmann MC, Goncalves A, Turrini O, Dagorn JC. Current knowledge on pancreatic cancer. Front Oncol. 2012;2:6. doi: 10.3389/fonc.2012.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–1617. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 7.Flossmann E, Rothwell PM. Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet. 2007;369:1603–1613. doi: 10.1016/S0140-6736(07)60747-8. [DOI] [PubMed] [Google Scholar]
- 8.Brasky TM, Liu J, White E, et al. Non-steroidal anti-inflammatory drugs and cancer risk in women: results from the Women’s Health Initiative. Int J Cancer. 2014;135:1869–1883. doi: 10.1002/ijc.28823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradley MC, Hughes CM, Cantwell MM, Napolitano G, Murray LJ. Non-steroidal anti-inflammatory drugs and pancreatic cancer risk: a nested case-control study. Br J Cancer. 2010;102:1415–1421. doi: 10.1038/sj.bjc.6605636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rayburn ER, Ezell SJ, Zhang R. Anti-inflammatory agents for cancer therapy. Mol Cell Pharmacol. 2009;1:29–43. doi: 10.4255/mcpharmacol.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Backhus LM, Petasis NA, Uddin J, et al. Dimethyl celecoxib as a novel non-cyclooxygenase 2 therapy in the treatment of non-small cell lung cancer. J Thorac Cardiovasc Surg. 2005;130:1406–1412. doi: 10.1016/j.jtcvs.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 12.Sobolewski C, Rhim J, Legrand N, et al. 2,5-Dimethyl-celecoxib inhibits cell cycle progression and induces apoptosis in human leukemia cells. J Pharmacol Exp Ther. 2015;355:308–328. doi: 10.1124/jpet.115.225011. [DOI] [PubMed] [Google Scholar]
- 13.Kardosh A, Soriano N, Liu YT, et al. Multitarget inhibition of drug-resistant multiple myeloma cell lines by dimethyl-celecoxib (DMC), a non-COX-2 inhibitory analog of celecoxib. Blood. 2005;106:4330–4338. doi: 10.1182/blood-2005-07-2819. [DOI] [PubMed] [Google Scholar]
- 14.Lee K, Piazza AG. The interaction between the Wnt/beta-catenin signaling cascade and PKG activation in cancer. J Biomed Res. 2017;31:189–196. doi: 10.7555/JBR.31.20160133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soh JW, Kazi JU, Li H, Thompson WJ, Weinstein IB. Celecoxib-induced growth inhibition in SW480 colon cancer cells is associated with activation of protein kinase G. Mol Carcinog. 2008;47:519–525. doi: 10.1002/mc.20409. [DOI] [PubMed] [Google Scholar]
- 16.Wick M, Hurteau G, Dessev C, et al. Peroxisome proliferator-activated receptor-gamma is a target of nonsteroidal anti-inflammatory drugs mediating cyclooxygenase-independent inhibition of lung cancer cell growth. Mol Pharmacol. 2002;62:1207–1214. doi: 10.1124/mol.62.5.1207. [DOI] [PubMed] [Google Scholar]
- 17.Arico S, Pattingre S, Bauvy C, et al. Celecoxib induces apoptosis by inhibiting 3;:-phosphoinositide-dependent protein kinase-1 activity in the human colon cancer HT-29 cell line. J Biol Chem. 2002;277:27613–27621. doi: 10.1074/jbc.M201119200. [DOI] [PubMed] [Google Scholar]
- 18.Pan MR, Hung WC. Nonsteroidal anti-inflammatory drugs inhibit matrix metalloproteinase-2 via suppression of the ERK/Sp1-mediated transcription. J Biol Chem. 2002;277:32775–32780. doi: 10.1074/jbc.M202334200. [DOI] [PubMed] [Google Scholar]
- 19.Ferrari V, Valcamonico F, Amoroso V, et al. Gemcitabine plus celecoxib (GECO) in advanced pancreatic cancer: a phase II trial. Cancer Chemother Pharmacol. 2006;57:185–190. doi: 10.1007/s00280-005-0028-1. [DOI] [PubMed] [Google Scholar]
- 20.Warner TD, Giuliano F, Vojnovic, Bukasa A, Mitchell JA, Vane JR. Nonsteroid drug selectivities for cyclo-oxygenase-1 rather than cyclooxygenase-2 are associated with human gastrointestinal toxicity: a full in vitro analysis. Proc Natl Acad Sci USA. 1999;96:7563–7568. doi: 10.1073/pnas.96.13.7563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gierse JK. Valdecoxib: assessment of cyclooxygenase-2 potency and selectivity. J Pharmacol Exp Ther. 2004;312:1206–1212. doi: 10.1124/jpet.104.076877. [DOI] [PubMed] [Google Scholar]
- 22.Ou YQ, Zhu W, Li Y, et al. Aspirin inhibits proliferation of gemcitabine-resistant human pancreatic cancer cells and augments gemcitabine-induced cytotoxicity. Acta Pharmacol Sin. 2010;31:73–80. doi: 10.1038/aps.2009.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marnett LJ, Kalgutkar AS. Structural diversity of selective COX-2 inhibitors. In: Pairet M, van Ryn J, editors. COX-2 inhibitors. Boston: Birkhauser-Verlag; 2004. pp. 15–40. [Google Scholar]
- 24.Atukorala I, Hunter DJ. Valdecoxib: the rise and fall of a COX-2 inhibitor. Expert Opin Pharmacother. 2013;14:1077–1086. doi: 10.1517/14656566.2013.783568. [DOI] [PubMed] [Google Scholar]
- 25.Barnett J, Chow J, Ives D, et al. Purification, characterization and selective inhibition of human prostaglandin G/H synthase 1 and 2 expressed in the baculovirus system. Biochim Biophys Acta. 1994;1209:130–139. doi: 10.1016/0167-4838(94)90148-1. [DOI] [PubMed] [Google Scholar]
- 26.Antoni D, Burckel H, Josset E, Noel G. Three-dimensional cell culture: a breakthrough in vivo. Int J Mol Sci. 2015;16:5517–5527. doi: 10.3390/ijms16035517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ware MJ, Colbert K, Keshishian V, et al. Generation of homogenous three-dimensional pancreatic cancer cell spheroids using an improved hanging drop technique. Tissue Eng Part C Methods. 2016;22:312–321. doi: 10.1089/ten.tec.2015.0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeon SE, No da Y, Lee SH, et al. Application of concave microwells to pancreatic tumor spheroids enabling anticancer drug evaluation in a clinically relevant drug resistance model. PLoS One. 2013;8:e73345. doi: 10.1371/journal.pone.0073345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Longati P, Jia X, Eimer J, et al. 3D pancreatic carcinoma spheroids induce a matrix-rich, chemoresistant phenotype offering a better model for drug testing. BMC Cancer. 2013;13:95. doi: 10.1186/1471-2407-13-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li H, Fan X, Houghton J. Tumor microenvironment: the role of the tumor stroma in cancer. J Cell Biochem. 2007;101:805–815. doi: 10.1002/jcb.21159. [DOI] [PubMed] [Google Scholar]
- 31.Cui J, Guo YH, Zhang HY, et al. Cyclooxygenase-2 inhibitor is a robust enhancer of anticancer agents against hepatocellular carcinoma multicellular spheroids. Onco Targets Ther. 2014;7:353–363. doi: 10.2147/OTT.S56115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarkar FH, Adsule S, Li Y, Padhye S. Back to the future: COX-2 inhibitors for chemoprevention and cancer therapy. Mini Rev Med Chem. 2007;7:599–608. doi: 10.2174/138955707780859431. [DOI] [PubMed] [Google Scholar]
- 33.Ding N, Cui XX, Gao Z, et al. A triple combination of atorvastatin, celecoxib and tipifarnib strongly inhibits pancreatic cancer cells and xenograft pancreatic tumors. Int J Oncol. 2014;44:2139–2145. doi: 10.3892/ijo.2014.2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu XT, Hu WT, Zhou JY, Tu Y. Celecoxib enhances the radiosensitivity of HCT116 cells in a COX-2 independent manner by up-regulating BCCIP. Am J Transl Res. 2017;9:1088–1100. [PMC free article] [PubMed] [Google Scholar]