Abstract
Introduction
Cognitive biases are associated with psychosis liability and paranoid ideation. This study investigated the moderating relationship between pre-existing self-reported cognitive biases and the occurrence of paranoid ideation in response to different levels of social stress in a virtual reality environment.
Methods
This study included 170 participants with different levels of psychosis liability (55 recent onset psychosis, 20 ultrahigh risk for psychosis, 42 siblings of psychotic patients, and 53 controls). All participants were exposed to virtual environments with different levels of social stress. The level of experienced paranoia in the virtual environments was measured with the State Social Paranoia Scale. Cognitive biases were assessed with a self-report continuous measure. Also, cumulative number of cognitive biases was calculated using dichotomous measures of the separate biases, based on general population norm scores.
Results
Higher belief inflexibility bias (Z = 2.83, P < .001), attention to threat bias (Z = 3.40, P < .001), external attribution bias (Z = 2.60, P < .001), and data-gathering bias (Z = 2.07, P < .05) were all positively associated with reported paranoid ideation in the social virtual environments. Level of paranoid response increased with number of cognitive biases present (B = 1.73, P < .001). The effect of environmental stressors on paranoid ideation was moderated by attention to threat bias (Z = 2.78, P < .01) and external attribution bias (Z = 2.75, P < .01), whereas data-gathering bias and belief inflexibility did not moderate the relationship.
Conclusion
There is an additive effect of separate cognitive biases on paranoid response to social stress. The effect of social environmental stressors on paranoid ideation is further enhanced by attention to threat bias and external attribution bias.
Keywords: cognition, stress, psychosis, first episode, schizophrenia
Introduction
There is a relationship between exposure to stressful social environments and risk for developing psychosis.1,2 Associations with psychosis have been documented for childhood abuse,3 recent stressful life events,4 social defeat,5 belonging to an ethnic minority group,6,7 urban upbringing,8 and being a victim of bullying.9 As a result of long-term or repeated exposure to stressful social environments, cognitive biases, such as an increased attention for potential threat, may develop. Psychological models suggest that cognitive biases increase vulnerability to develop paranoid ideations or delusions when confronted with environmental social stress later in life.10,11
Psychotic disorders are characterized by both cognitive deficits12,13 and cognitive biases.11 Cognitive deficits are impairments in cognitive functioning, such as problems with verbal memory.12 Cognitive biases represent selective processing of information, such as the tendency to attend to a certain type of stimulus or consistently interpret emotionally ambiguous information in a negative direction.14 Cognitive biases are implicated in developing and maintaining paranoid ideation.15 Paranoid ideation characterizes 90% of patients with psychotic disorder.16 Psychotic patients with paranoid delusions anticipate intentional harm inflicted by other people. Cognitive models of paranoia propose that cognitive biases distort the processing of information from the social environment toward a more paranoid interpretation.17 Several types of cognitive biases are associated with paranoid ideation.11 Cognitive biases are measured with experimental tasks; only recently have self-report measures been developed and validated against experimental tasks.18–20 “Data-gathering bias” (also known as “jumping to conclusions”) is a cognitive bias characterized by hasty decision making. “Belief inflexibility” is a cognitive bias that results in rigidity of beliefs when exposed to contradictory evidence; it overlaps with confirmatory bias and the bias against disconfirmatory evidence.21 The tendency to attend selectively to threat-related information is known as “attention to threat bias.” “External attribution bias” is the tendency to blame other people for negative events. All of these four biases were found to be more prevalent in patients with a schizophrenia spectrum disorder11,22–25 and in people with subclinical psychotic symptoms at ultrahigh risk for psychosis (UHR)26–29 than in healthy controls. They seem specifically related to the development and maintenance of paranoid delusions.15 These findings suggest that the level of cognitive biases is associated with the level of paranoid ideation in response to social stressors in the environment, in particular in patients with a psychotic disorder and UHR.
Some evidence for this psychopathological mechanism is derived from experimental and time-sampling studies. In an experimental study, when patients with persecutory delusions were exposed to a crowded street in inner London, they reported an increase in paranoid ideation, auditory hallucinations, and in data-gathering bias.30 Time-sampling studies using observations in daily life found a temporal association between social contact and paranoid ideation.31 However, due to the complexity of interactions between personal and contextual factors, it is difficult to examine the context of paranoid ideation in daily life social environments. Ideally, the interaction between social environments, cognitive biases, and paranoid ideation should be explored using an experimental design, in which exposure to social stress is controlled.
Virtual reality (VR) allows systematic manipulation of social environments.32 VR is a safe and valid method to investigate paranoia in healthy individuals, in UHR patients, and in patients with persecutory delusions.33,34 Recent research has demonstrated that virtual social stressors were able to elicit paranoid ideation in VR social environments33,35,36 and psychosis liability and pre-existing negative affect moderated the levels of paranoia and distress.36
The present study manipulated the number of social stressors presented in the virtual environment. The moderating effect of cognitive biases on the association between the number of social stressors and paranoid ideation was examined in groups with a different liability to psychosis. Our hypothesis was that the level and number of cognitive biases present will be positively associated with the level of paranoid ideation when participants are exposed to increased social stress
Methods
Participants
Four groups of participants (aged 18–35 years) with different liability to psychosis were recruited. Namely, a group with high liability for psychosis consisting of (1) patients with recent onset psychotic disorder (N = 55) and (2) patients with an UHR status (N = 20); as well as a group with low liability for psychosis with (3) siblings of patients with a psychotic disorder, who had never had a psychotic episode themselves (N = 42), and (4) healthy controls without a history of psychotic disorder or a first-degree relative with a psychotic disorder (N = 53). The exclusion criteria were poor command of the Dutch language, a history of epilepsy, and an IQ ≤ 75.
This study was approved by the Medical Ethics Committee of the Leiden University Medical Centre (NL37356.058.12/P12.182). Written informed consent was obtained from all participants.
The psychotic group included individuals with a recent (<5 years) diagnosis of a psychotic disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), with the exception of substance-induced psychotic disorder and psychotic disorder due to a medical condition. They were recruited from five participating mental health services. The UHR group included individuals with an UHR status, who were recruited among patients seeking help for nonpsychotic psychiatric symptoms at two mental health services. The siblings group included siblings of persons diagnosed with a psychotic disorder, who did not themselves have a personal history of psychotic disorder or meet UHR criteria. The healthy control group included persons recruited from the general population without a history of psychotic disorder or a first-degree relative with a psychotic disorder.
Measurement Instruments
Diagnostic Instruments.
The Comprehensive Assessment of At-Risk Mental States (CAARMS)37 was used to assess UHR status. The CAARMS identifies three inclusion groups: (1) people with a schizotypal personality disorder and/or a first-degree relative with psychosis; (2) people that experience attenuated positive psychotic symptoms, such as paranoid ideas and unusual perceptual experiences; and (3) people who have experienced a brief psychotic episode lasting ≤1 week and remitted without treatment with antipsychotic medication. Additional inclusion criteria were either a recent drop of 30% in social functioning as assessed with the Social and Occupational Functional Assessment Scale (SOFAS)38,39 or dropping below a score of 55 on the SOFAS.
Psychotic disorder was diagnosed with either the Comprehensive Assessment of Symptoms and History (CASH)40 or the Schedules for Clinical Assessment in Neuropsychiatry (SCAN).41 CASH and SCAN are similar semistructured interviews for diagnosing psychotic disorders, following DSM and ICD diagnostic criteria. Choice of instrument varied per participating mental health center.
Cognitive Biases.
At baseline, the Davos Assessment of Cognitive Biases Scale (DACOBS) was administered to assess cognitive biases.19 The DACOBS is a self-rating assessment scale, consisting of seven subscales (four cognitive biases, two assessing subjective deficits in cognition and social cognition, and one on safety behaviors). In this study, we used the four subscales that measure cognitive biases, ie, (1) data-gathering bias, (2) belief inflexibility bias, (3) selective attention to threat bias, and (4) external attribution bias. The subscales had an acceptable reliability (Cronbach’s alpha ranging from .64 to .72) and an acceptable convergent validity (Spearman’s Rho ranging from .36 to .63). Factor analysis confirmed that the four cognitive biases are separate constructs.19 All factors independently explained the variance (eigenvalues >2) and total explained variance was 45%. The DACOBS was cross-validated with correlations ranging from .360 to .627. The beads task, a probabilistic inference task,42 was used as a validation test for the “Jumping to conclusions” subscale (r = −.360, P < .01). The Dogmatism scale, a self-report measurement, was used to validate the Belief inflexibility bias (r = .403, p < .01). The Green Paranoid Thoughts Scale, a self-report measurement, has two subscales. Subscale A measures ideas of social reference and subscale B measures paranoid thoughts. Part A was used to validate the Attention to threat bias (r = .408, P < .01), whereas subscale B was used to validate the External attribution bias (r = .627, P < 0.01). The factor structure was replicated in an independent sample by confirmative factor analysis.20
A cognitive bias was considered to be present in a participant when the score was “above average,” “high,” or “very high” according to the norm scores for the normal control population.19 The number of elevated cognitive biases was summed to create a cumulative cognitive biases variable.
State Paranoia.
Immediately after exposure to each virtual social environment, momentary paranoia was assessed using the Social State Paranoia Scale (SSPS). The SSPS is a valid (Spearman’s rho is .41) and reliable (Cronbach’s alpha is .91) measure of state persecutory ideation in virtual social environments.43
VR Setting
The virtual environment used was a café with both indoor and outdoor areas. Participants could navigate in the virtual environment, using a Logitech F310 Gamepad. For VR display, participants used the Sony HMZ-T1 Head-Mounted Display with a HD resolution of 1280 × 720 (per eye), with 51.6 diagonal field of view, a 3DOF tracker for head rotation, and built-in headphones. The researcher controlled the VR system using a graphical user interface, whereby several actions could be activated within the virtual environment. Avatars could be placed in the café and chatted among themselves while sitting or standing at a table. Sounds and café noises were audio-played in the background. The avatars looked at participants for 5 s when they were approached.
Experiments
The number of social stressors in the virtual social environments was manipulated by (1) the number of avatars in the virtual environment (6 or 40 avatars); (2) own ethnic or other ethnic identity of the avatars; and (3) neutral or hostile facial expressions by the avatars. Pre-existing cognitive biases were measured with a self-reported questionnaire before participants were exposed to the virtual environments with a varying number (0–3) of social stressors. Paranoid ideation was assessed after each exposure session of 4 min.
To engage participants in the virtual social environment, the computer randomly assigned a number (0–99) to five of the avatars. Participants were encouraged to explore the VR environment and to remember the number and sex of the avatar assigned the highest number. In a small pilot, patients reported that the task was easy and not stressful or distracting. All participants participated in four conditions with exposure to no, one, two, or three social stressors in the VR environment. The order of exposure to the different conditions was randomized.
Detailed information on the conditions have been published previously.36
Statistical Analyses
Analysis was performed using Stata version 13. Differences in age between the psychosis liability groups were tested with one-way ANOVA. Group differences in the dichotomous variables sex, ethnic minority status, and education were tested using χ2 tests. Multilevel random intercept regression analysis was conducted to test associations between cognitive biases and paranoid ideations in VR using the XTREG procedure in Stata. The study data have a hierarchical structure, with repeated measurements (level 1) nested within individuals (level 2). Multilevel analyses take into account that observations within an individual are more similar than those between individuals. The interaction effects between the number of virtual stressors and cognitive biases were added to the multilevel regression models to investigate a moderating relationship with sex, age, level of education, and psychosis liability as covariates. We examined whether the interaction between level of cognitive bias and level of social stress significantly predicted paranoid ideation. If moderation analysis found a significant interaction for different levels of cognitive biases, post hoc probing analysis was conducted to see how the different levels of cognitive biases (high vs low) affected the association between social stress and paranoid ideation.44
Results
Sociodemographic characteristics of the participants and level of cognitive biases are presented in table 1. Patients with psychosis had (on average) a lower level of education than siblings or the healthy controls. The proportion of males was high in the psychosis group (76%) and low in the UHR group (35%). Overall, males reported a higher level of data-gathering bias than females (M 25.5 vs F 22.9, P = .006). The covariate effect of sex was nonsignificant.
Table 1.
Sociodemographic Characteristics of the Study Sample
| Controls N = 53 |
Siblings N = 42 |
UHR N = 20 |
Psychosis N = 55 |
P | ||
|---|---|---|---|---|---|---|
| Sex male, n (%) | 25 (47.2) | 23 (54.8) | 7 (35) | 42 (76.4) | χ2 (3) = 14.5 | .002 |
| Age in years | 25 (4) | 26 (5) | 24 (4) | 26 (5) | F (df) = 2.1 (3) | .097 |
| Non-Dutch origin, n (%) | 16 (30.2) | 11 (26.2) | 5 (25) | 26 (47.3) | χ2 (3) = 6.3 | .099 |
| Level of education, n (%) | χ2 (9) = 19.7 | .020 | ||||
| No/primary | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (5.5) | ||
| Vocational ((V)MBO) | 13 (24.5) | 11 (26.2) | 8 (40) | 25 (45.5) | ||
| Higher secondary (HAVO/VWO) | 10 (18.9) | 4 (9.5) | 5 (25) | 10 (18.2) | ||
| Higher tertiary (HBO/University) | 30 (56.6) | 26 (61.9) | 7 (35) | 17 (30.9) | ||
| Medication usea, n (%) | ||||||
| None | 49 (94.2) | 39 (92.9) | 6 (30.0) | 18 (32.7) | ||
| Antipsychotic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 35 (63.6) | ||
| Antidepressant | 1 (1.9) | 1 (2.4) | 12 (60.0) | 5 (9.1) | ||
| Benzodiazepine | 0 (0.0) | 0 (0.0) | 4 (20.0) | 6 (10.9) | ||
| Other | 2 (3.8) | 2 (4.8) | 5 (25.0) | 2 (3.6) |
Note. Values are presented as mean (standard deviation; sd) or N (%). P-values are given from ANOVA (for continuous variables) and tested with Bonferroni correction, or χ2 tests (for categorical variables). UHR, patients with ultra-high risk for psychosis. Bold values are significant at <.05.
a Self-report.
Participants with higher psychosis liability scored higher on attention to threat, belief inflexibility, and external attribution, while participants with lower psychosis liability scored average or below average. There was no psychosis liability effect on data-gathering bias, ie, all groups scored average and showed no statistical differences; the results are shown in table 2.
Table 2.
Group Differences in Pre-existing Self-reported Cognitive Biases Measured with the DACOBS
| Controls n = 53 |
Siblings n = 42 |
UHR n = 20 |
Psychosis n = 55 |
F(df) | P | |
|---|---|---|---|---|---|---|
| Data-gathering bias (sd) | 24.2 (6.1) | 23.9 (6.7) | 24.6 (5.4) | 24.8 (6.3) | 0.2 (3) | .911 |
| Belief inflexibility bias (sd) | 14.2 (4.9) | 13.3 (4.4) | 18.1 (5.1) | 19.7 (6.9) | 14.2 (3) | <.001 |
| Attention to threat bias (sd) | 17.8 (7.5) | 16.1 (5.7) | 28.8 (6.9) | 22.8 (7.4) | 13.5 (3) | <.001 |
| External attribution bias (sd) | 14.1 (4.9) | 12.3 (3.9) | 23.2 (5.1) | 19.8 (7.7) | 25.3 (3) | <.001 |
Note. DACOBS, Davos assessment of cognitive biases scale. DACOBS values are presented as mean (standard deviation; sd). P-values are given from ANOVA. Biases were tested with Bonferroni correction. Bold values are significant at <.05.
The association between cognitive biases and paranoid ideation is shown in table 3. All four types of cognitive biases were significantly associated with higher levels of paranoid ideation experienced in the VR environments (table 3a).
Table 3.
Effect of Pre-existing Self-reported Cognitive Biases, on Paranoid Ideations Reported in Virtual Social Stress Environments
| Paranoia SSPS | Coefficienta | Standard error | Z | P | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Type of bias | ||||||
| Data-gathering bias | .183 | .089 | 2.07 | .039 | .00948 | .35649 |
| Belief inflexibility bias | .288 | .101 | 2.83 | .005 | .08888 | .48726 |
| Attention to threat bias | .262 | .077 | 3.40 | .001 | .11113 | .41379 |
| External attribution bias | .253 | .097 | 2.60 | .009 | .06247 | .44400 |
| Cumulative number of biasesb | ||||||
| One | .074 | 1.57 | .05 | .962 | −3.0090 | 3.1579 |
| Two | 3.056 | 1.56 | 1.96 | .050 | −.00493 | 6.1162 |
| Three | 5.995 | 1.77 | 3.39 | .001 | 2.5256 | 9.4636 |
| Four | 5.828 | 1.81 | 3.22 | .001 | 2.2843 | 9.3714 |
Note. SSPS, Social State Paranoia Scale. Bold values are significant at <.05.
a B coefficient in multilevel random regression analysis (cognitive bias). Analyses were adjusted for sex, education, age, and psychosis liability.
bCalculated using dichotomous measures of the separate biases, based on general population norm scores, no cognitive biases as reference category.
Fourty-four percent of the low-liability group had no cognitive biases, compared to only 9% in the high-liability group. A significant effect was found for cumulative number of cognitive biases on reported paranoid ideation (B = 1.73, 95% CI: 0.93–2.53, P < .001). Effect of cumulative number of biases is shown in table 3b.
We found a significant interaction effect between the number of cognitive biases and the number of social stressors on paranoid ideation B = 0.52, 95% CI: 0.22–0.82, P = .001).
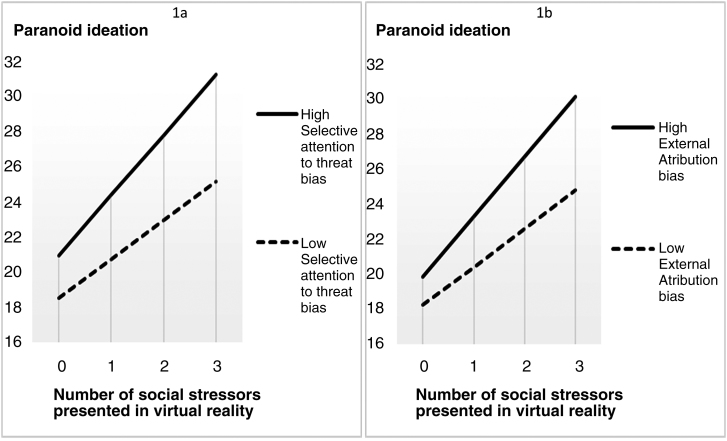
We found a significant interaction effect between attention to threat bias and the number of social stressors on paranoid ideation (p < .01) and also a significant interaction effect between external attribution bias and the number of social stressors on paranoid ideation in the VR environment (P < .01). The interaction results are shown in table 4.
Table 4.
Interaction Effect Between Cognitive Biases and Level of Social Stress, on Paranoid Ideations Reported in Virtual Social Stress Environments
| Paranoia SSPS | Coefficienta | Standard error | Z | P | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Data-gathering bias | .052 | .036 | 1.45 | .148 | −.01842 | .12231 |
| Belief inflexibility bias | .038 | .036 | 1.05 | .292 | −.03271 | .10861 |
| Attention to threat bias | .079 | .028 | 2.78 | .005 | .02337 | .13452 |
| External attribution bias | .090 | .033 | 2.75 | .006 | .02583 | .15366 |
Note. Bold values are significant at <.05.
a B coefficient in multilevel random regression analysis (cognitive bias × number of social stressors). Analyses were adjusted for sex, education, age, and psychosis liability.
Post hoc probing showed that both low and high levels of attention to threat bias significantly affected the association between social stress and paranoid ideation (low: B = 2.21, 95% CI: 1.62–2.80, P < .001; high: B = 3.43, 95% CI: 2.81–4.05, P < .001). Post hoc probing shows that both low and high levels of external attribution bias significantly affect the association between social stress and paranoid ideation (low: B = 2.19, 95% CI: 1.59–2.79, P < .001; high: B = 3.43, 95% CI: 2.81–4.06, P < .001). The effect of the difference in slopes is presented in figure 1. A high level of attention to threat bias showed a stronger paranoid response to an increase in social stressors. A high level of external attribution bias also showed a steeper paranoid response to an increase in social stressors.
Fig. 1.
The moderating effect of high versus low self-reported cognitive biases on the association between number of social stressors presented in virtual reality (0–3) and elicited paranoid ideation (Social State Paranoia Scale). Note. Analyses were adjusted for sex, education, age. and psychosis liability.
Discussion
In this experimental VR study, higher psychosis liability was associated with higher levels of the cognitive biases attention to threat, belief inflexibility, and external attribution but not with data-gathering bias. Also, belief inflexibility, attention to threat, external attribution bias, and data-gathering bias all predicted paranoid ideation in controlled virtual social environments. When more cognitive biases were present that person showed a stronger paranoid response. Both attention to threat and external attribution bias moderated the paranoid response during exposure to social environmental stress (figure 1).
By using VR to fully control the level of exposure to social stressors, this study found experimental evidence to support current cognitive psychological models17,45 of the development and persistence of paranoid delusions. When people are exposed to social stress in the environment, higher levels of attention to threat bias and external attribution bias contribute to a more paranoid interpretation of the social environment. When multiple cognitive biases are present, this increases the paranoid interpretation.
In accordance with previous research, the present study found a positive relationship between the presence of cognitive biases and the experience of paranoid ideation. However, there was no significant difference in scores for data-gathering bias between the four groups with different psychosis liability. This may indicate poor sensitivity of the DACOBS subscale to measure data-gathering bias. Although the DACOBS data-gathering bias subscale is validated against the beads task, their shared variance is limited.19 Other explanations may be the fact that data-gathering bias may be difficult to measure using a self-report questionnaire, as those with the bias, compared with those without the bias, do not differ in the self-rated level of decisiveness.46 Not finding different levels of data gathering in different liability groups is at odds with the literature, but finding a marginally significant effect of data gathering on paranoid ideation and no moderating effect is in accordance with the meta-analytical findings.47 Our findings suggest that data-gathering biases may not be as relevant in the model of paranoid symptoms as was formerly expected.
Although we found a significant difference for belief inflexibility bias between the groups with different psychosis liability, there was no interaction effect between environmental social stress and belief inflexibility bias on paranoid ideation. Apparently, the relationships between specific cognitive biases and paranoid ideation differ. Cognitive biases describe selective processing of information in general; subdivision into more specific categories may improve our understanding of the cognitive processes involved in paranoid ideation.
Strengths and Limitations
The main strength of this study is the use of VR to control the social environments and the social stressors the participants are exposed to. All participants were exposed to exactly the same environmental conditions, which would be impossible in a real-life social situation. The use of VR also prevents unintended effects of interactions between the participant and the social environment, allowing us to study the effect of cognitive biases on paranoid ideation. An additional strength is the variety of participants with different liability to psychosis, allowing to investigate the relationship between cognitive biases, social stress, and paranoid ideation over different levels of psychosis liability.
The study has several limitations. First, cognitive biases were assessed using self-report questionnaires only. Also, only 20 participants were included in the UHR group and this group consisted mainly of females. Our psychosis sample consisted of patients with recent onset psychosis only and was mainly males. The differences in sex distribution in these groups are consistent with previous research39,48 and may have influenced the results in the high psychosis liability group. This study used the facial expressions of the avatars to convey hostility; however, since facial affect recognition impairments are found in patients with a first episode of psychosis,49 this may have affected the results in our high-liability group. Difficulty with interpreting the avatars’ hostile faces may have caused additional anxiety or may have influenced the effect between social hostility and paranoid interpretation. Also, although the categories of cognitive biases were based on exploratory factor analysis19 and replicated in confirmatory factor analysis in another sample,20 it is important to note that these biases likely interact and possibly partially overlap. Moreover, this study is limited to four cognitive biases. For example, we did not include interpretation bias, which is the tendency to draw negative conclusions when presented with ambiguous information.50 Interpretation bias occurs in a nonpsychiatric population with higher psychosis vulnerability and may be associated with paranoid ideations.51 Prevalence and severity of cognitive biases were too small in the low-liability group to analyze high- and low-liability groups separately. The effects remained statistically significant when psychosis liability was included as a covariate in the regression models, suggesting that cognitive biases predict paranoid response to social stressors independent of psychosis liability. Further research is needed to investigate this issue. Last, we only included patient groups with UHR or a diagnosis of psychotic disorder, whereas paranoid ideations are also common in other psychiatric disorders. Inclusion of a broader range of psychiatric disorders may help to increase the understanding of paranoia.
Clinical Implications
Both attention to threat bias and external attribution bias are viable targets for interventions in cognitive behavioral therapy, aiming to mitigate the effect of these biases on paranoid appraisal of the social environment. Patients could be trained to normalize their attention to threat bias. However, as findings on the effect of specific techniques are not consistent further development is needed.52–54 External attribution can be explored and competing explanations may be generated and tested with behavioral experiments. Interestingly, these procedures implicitly address belief inflexibility by contrasting several different beliefs with an event. In patients suffering from paranoid ideation, belief inflexibility has indeed been found to improve with cognitive behavioral therapy.55 Psychological therapy in a VR social environment would allow us to integrate exposure to social situations with an active correction of dysfunctional cognitions. Such cognitive behavioral therapy enhanced by VR (VR-CBT) is currently under investigation.56,57
Funding
This work was supported by ZonMw: The Netherlands Organization for Health Research and Development (Veni grant 916.12.013 to W.V.).
Acknowledgments
The authors thank all individuals who participated in the study, and the five participating mental health centers: Parnassia, Dijk en Duin, BAVO, GGZ-Delfland, and GGZ-Noord Holland Noord. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflict of Interest
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. 2010;468:203–212. [DOI] [PubMed] [Google Scholar]
- 2. Fusar-Poli P, Tantardini M, De Simone S, et al. Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. Eur Psychiatry. 2017;40:65–75. [DOI] [PubMed] [Google Scholar]
- 3. Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012;42:1025–1036. [DOI] [PubMed] [Google Scholar]
- 4. Beards S, Gayer-Anderson C, Borges S, Dewey ME, Fisher HL, Morgan C. Life events and psychosis: a review and meta-analysis. Schizophr Bull. 2013;39:740–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Valmaggia LR, Day F, Garety P, et al. Social defeat predicts paranoid appraisals in people at high risk for psychosis. Schizophr Res. 2015;168:16–22. [DOI] [PubMed] [Google Scholar]
- 6. Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41:897–910. [DOI] [PubMed] [Google Scholar]
- 7. Veling W. Ethnic minority position and risk for psychotic disorders. Curr Opin Psychiatry. 2013;26:166–171. [DOI] [PubMed] [Google Scholar]
- 8. Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38:1118–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Valmaggia LR, Day FL, Kroll J, et al. Bullying victimisation and paranoid ideation in people at ultra high risk for psychosis. Schizophr Res. 2015;168:68–73. [DOI] [PubMed] [Google Scholar]
- 10. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. The Lancet 2013. Published online December 6. doi: 10.1016/S0140-6736(13)62036-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bentall RP, de Sousa P, Varese F, et al. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1011–1022. [DOI] [PubMed] [Google Scholar]
- 12. Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23:315–336. [DOI] [PubMed] [Google Scholar]
- 13. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–445. [DOI] [PubMed] [Google Scholar]
- 14. Savulich G, Shergill S, Yiend J. Biased cognition in psychosis. J Exp Psychopathol. 2012. ;3(4):514–536. [Google Scholar]
- 15. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moutoussis M, Williams J, Dayan P, Bentall RP. Persecutory delusions and the conditioned avoidance paradigm: towards an integration of the psychology and biology of paranoia. Cogn Neuropsychiatry. 2007;12:495–510. [DOI] [PubMed] [Google Scholar]
- 17. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peters ER, Moritz S, Schwannauer M, et al. Cognitive Biases Questionnaire for Psychosis. Schizophr Bull. 2014;40:300–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van der Gaag M, Schütz C, Ten Napel A, et al. Development of the Davos assessment of cognitive biases scale (DACOBS). Schizophr Res. 2013;144:63–71. [DOI] [PubMed] [Google Scholar]
- 20. Bastiaens T, Claes L, Smits D, De Wachter D, van der Gaag M, De Hert M. The Cognitive Biases Questionnaire for Psychosis (CBQ-P) and the Davos Assessment of Cognitive Biases (DACOBS): validation in a Flemish sample of psychotic patients and healthy controls. Schizophr Res. 2013;147:310–314. [DOI] [PubMed] [Google Scholar]
- 21. Moritz S, Woodward TS. A generalized bias against disconfirmatory evidence in schizophrenia. Psychiatry Res. 2006;142:157–165. [DOI] [PubMed] [Google Scholar]
- 22. Garety PA, Freeman D, Jolley S, et al. Reasoning, emotions, and delusional conviction in psychosis. J Abnorm Psychol. 2005;114:373–384. [DOI] [PubMed] [Google Scholar]
- 23. So SH, Freeman D, Dunn G, et al. Jumping to conclusions, a lack of belief flexibility and delusional conviction in psychosis: a longitudinal investigation of the structure, frequency, and relatedness of reasoning biases. J Abnorm Psychol. 2012;121:129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Veckenstedt R, Randjbar S, Vitzthum F, Hottenrott B, Woodward TS, Moritz S. Incorrigibility, jumping to conclusions, and decision threshold in schizophrenia. Cogn Neuropsychiatry. 2011;16:174–192. [DOI] [PubMed] [Google Scholar]
- 25. Woodward TS, Moritz S, Menon M, Klinge R. Belief inflexibility in schizophrenia. Cogn Neuropsychiatry. 2008;13:267–277. [DOI] [PubMed] [Google Scholar]
- 26. Broome MR, Johns LC, Valli I, et al. Delusion formation and reasoning biases in those at clinical high risk for psychosis. Br J Psychiatry Suppl. 2007;51:s38–s42. [DOI] [PubMed] [Google Scholar]
- 27. Woodward TS, Buchy L, Moritz S, Liotti M. A bias against disconfirmatory evidence is associated with delusion proneness in a nonclinical sample. Schizophr Bull. 2007;33:1023–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lim M, Gleeson JF, Jackson HJ. Selective attention to threat bias in delusion-prone individuals. J Nerv Ment Dis. 2011;199:765–772. [DOI] [PubMed] [Google Scholar]
- 29. Lee TY, Hong SB, Shin NY, Kwon JS. Social cognitive functioning in prodromal psychosis: a meta-analysis. Schizophr Res. 2015;164:28–34. [DOI] [PubMed] [Google Scholar]
- 30. Freeman D, Emsley R, Dunn G, et al. The stress of the street for patients with persecutory delusions: a test of the symptomatic and psychological effects of going outside into a busy urban area. Schizophr Bull. 2015;41:971–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Collip D, Oorschot M, Thewissen V, Van Os J, Bentall R, Myin-Germeys I. Social world interactions: how company connects to paranoia. Psychol Med. 2011;41:911–921. [DOI] [PubMed] [Google Scholar]
- 32. Freeman D. Studying and treating schizophrenia using virtual reality: a new paradigm. Schizophr Bull. 2008;34:605–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Veling W, Brinkman WP, Dorrestijn E, van der Gaag M. Virtual reality experiments linking social environment and psychosis: a pilot study. Cyberpsychol Behav Soc Netw. 2014;17:191–195. [DOI] [PubMed] [Google Scholar]
- 34. Valmaggia LR, Freeman D, Green C, et al. Virtual reality and paranoid ideations in people with an ‘at-risk mental state’ for psychosis. Br J Psychiatry Suppl. 2007;51:s63–s68. [DOI] [PubMed] [Google Scholar]
- 35. Freeman D, Pugh K, Antley A, et al. Virtual reality study of paranoid thinking in the general population. Br J Psychiatry. 2008;192:258–263. [DOI] [PubMed] [Google Scholar]
- 36. Veling W, Pot-Kolder R, Counotte J, van Os J, van der Gaag M. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophr Bull. 2016;42(6):1363–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–971. [DOI] [PubMed] [Google Scholar]
- 38. Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149:1148–1156. [DOI] [PubMed] [Google Scholar]
- 39. Rietdijk J, Klaassen R, Ising H, et al. Detection of people at risk of developing a first psychosis: comparison of two recruitment strategies. Acta Psychiatr Scand. 2012;126:21–30. [DOI] [PubMed] [Google Scholar]
- 40. Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry. 1992;49:615–623. [DOI] [PubMed] [Google Scholar]
- 41. Wing JK, Babor T, Brugha T, et al. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–593. [DOI] [PubMed] [Google Scholar]
- 42. Phillips LD, Edwards W. Conservatism in a simple probability inference task. J Exp Psychol. 1966;72:346–354. [DOI] [PubMed] [Google Scholar]
- 43. Freeman D, Pugh K, Green C, Valmaggia L, Dunn G, Garety P. A measure of state persecutory ideation for experimental studies. J Nerv Ment Dis. 2007;195:781–784. [DOI] [PubMed] [Google Scholar]
- 44. Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. [DOI] [PubMed] [Google Scholar]
- 45. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Freeman D, Garety P, Kuipers E, et al. Delusions and decision-making style: use of the Need for Closure Scale. Behav Res Ther. 2006;44:1147–1158. [DOI] [PubMed] [Google Scholar]
- 47. Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the “jumping to conclusions” reasoning bias: a systematic review and meta-analysis. Schizophr Bull. 2016;42:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stouten LH, Veling W, Laan W, van der Helm M, van der Gaag M. Psychosocial functioning in first-episode psychosis and associations with neurocognition, social cognition, psychotic and affective symptoms. Early Interv Psychiatry. 2017;11:23–36. [DOI] [PubMed] [Google Scholar]
- 49. Addington J, Penn D, Woods SW, Addington D, Perkins DO. Facial affect recognition in individuals at clinical high risk for psychosis. Br J Psychiatry. 2008;192:67–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lee JS, Mathews A, Shergill S, Yiend J. Magnitude of negative interpretation bias depends on severity of depression. Behav Res Ther. 2016;83:26–34. [DOI] [PubMed] [Google Scholar]
- 51. Savulich G, Freeman D, Shergill S, Yiend J. Interpretation biases in paranoia. Behav Ther. 2015;46:110–124. [DOI] [PubMed] [Google Scholar]
- 52. van Oosterhout B, Smit F, Krabbendam L, Castelein S, Staring AB, van der Gaag M. Metacognitive training for schizophrenia spectrum patients: a meta-analysis on outcome studies. Psychol Med. 2016;46:47–57. [DOI] [PubMed] [Google Scholar]
- 53. Gawęda Ł, Krężołek M, Olbryś J, Turska A, Kokoszka A. Decreasing self-reported cognitive biases and increasing clinical insight through meta-cognitive training in patients with chronic schizophrenia. J Behav Ther Exp Psychiatry. 2015;48:98–104. [DOI] [PubMed] [Google Scholar]
- 54. Mogg K, Bradley BP. Anxiety and attention to threat: cognitive mechanisms and treatment with attention bias modification. Behav Res Ther. 2016;87:76–108. [DOI] [PubMed] [Google Scholar]
- 55. Waller H, Emsley R, Freeman D, et al. Thinking well: a randomised controlled feasibility study of a new CBT therapy targeting reasoning biases in people with distressing persecutory delusional beliefs. J Behav Ther Exp Psychiatry. 2015;48:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pot-Kolder R, Veling W, Geraets C, van der Gaag M. Effect of virtual reality exposure therapy on social participation in people with a psychotic disorder (VRETp): study protocol for a randomized controlled trial. Trials. 2016;17:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Freeman D, Bradley J, Antley A, et al. Virtual reality in the treatment of persecutory delusions: randomised controlled experimental study testing how to reduce delusional conviction. Br J Psychiatry. 2016;209:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]