Dear Sir:
Recently, the diffusion-weighted imaging (DWI) or computed tomography perfusion (CTP) Assessment With Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) trial showed that the time window for endovascular thrombectomy (EVT) could be extended to within 24 hours of the time last known well [1]. As expansion of the eligible population for EVT is expected, we aimed to estimate the number of ischemic stroke patients who met the eligibility criteria of the DAWN trial South Korea and the United States and the number of candidates who should be screened for EVT.
Using a multicenter prospective stroke registry (Clinical Research Collaboration for Stroke in Korea [CRCS-K]), adult patients (aged ≥18 years) with acute ischemic stroke or transient ischemic attack, who were hospitalized in one of the 11 participating centers between May 2011 and December 2012 and who had available lesion volume on DWI were identified as eligible for this study. Information on MRI acquisition time was available in 46.7% of the study subjects, and the median duration from symptom onset to image acquisition was 1 day (interquartile range, 0 to 2). The infarct lesions on DWI were transferred to a standard brain template using an imaging software package (Image_QNA, a custom-built software package) [2,3]. The infarct volume was then calculated by multiplying the known mean brain volume of the Korean elderly population (1,170 cm3) to the proportion of the lesions (lesional voxel count in the template divided by total brain parenchymal voxel count in the template) [4]. The local ethics committees of all the participating centers approved the study protocol.
The number, age, and sex of ischemic stroke patients in Korea was obtained using reported ischemic stroke incidence rates [5] and data from the 2016 Statistics of Registered Population (http://www.mois.go.kr/frt/sub/a05/ageStat/screen.do). The age- and sex-specific proportions of the eligible patients from the CRCS-K registry were multiplied to reach the number in each age and sex stratum. For the United States population, data from the National Impatient Sample were used to identify the patients hospitalized for acute ischemic stroke in 2014 [6].
Data from a total of 6,742 patients were subjected to analysis. We applied the DAWN trial’s eligibility criteria step-wise (Table 1). Thirty-two percent of the starting population arrived at the hospital within the time window dictated by the DAWN trial’s eligibility criteria. Only 1.1% of individuals were eligible for EVT. From the initial population, the proportions of patients arriving within 6 hours of symptom onset and within the extended time window were 43.9% and 67.6%, respectively.
Table 1.
Numbers and proportions of the Korean acute ischemic stroke patients when applying the eligibility criteria of DAWN trial to the study subjects
| Criteria | No. (%) |
|---|---|
| Acute ischemic stroke or TIA patients with measurable infarct on DWI (age ≥18 years) | 6,742 (100) |
| Within 6 to 24 hours of last known well | 2,145 (31.8) |
| Pre-stroke mRS 0 or 1 | 1,826 (27.1) |
| NIHSS ≥10 | 343 (5.1) |
| Intracranial ICA or MCA occlusion | 152 (2.3) |
| Clinical deficit: infarct volume mismatch | |
| Group A (age ≥80 years, NIHSS ≥10, infarct volume <21 mL) | 13 (0.2) |
| Group B (age <80 years, NIHSS ≥10, infarct volume <31 mL) | 60 (0.9) |
| Group C (age <80 years, NIHSS ≥20, infarct volume ≥31 mL & <51 mL) | 4 (0.06) |
| Final eligible patients | 77 (1.1) |
DAWN, DWI or computed tomography perfusion (CTP) Assessment With Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo; TIA, transient ischemia attack; DWI, diffusion-weighted imaging; mRS, modified Rankin’s scale; NIHSS, National Institute of Health Stroke Scale score; ICA, internal carotid artery; MCA, middle cerebral artery.
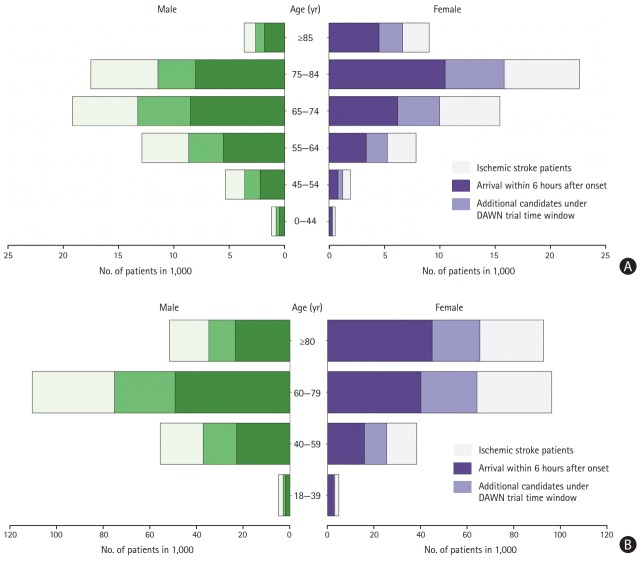
When we projected the final proportion of study patients who met the DAWN eligibility criteria to the annual nationwide expected number of ischemic stroke patients, 1,331 patients in Korea and 5,371 in the United States met the criteria. For the extended time window, the number of patients who required additional screening was expected to be 27,477 annually (range, 52,195 to 79,672) in Korea, and 106,795 (range, 200,867 to 307,662) in the United States (Figure 1).
Figure 1.
Plot of ischemic stroke patients who are candidates for endovascular thrombectomy according to various time windows. (A) Plot of the South Korean ischemic stroke population, stratified by age and gender. (B) Plot of the United States ischemic stroke population, stratified by age and gender. DAWN, diffusion-weighted imaging (DWI) or computed tomography perfusion (CTP) Assessment With Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo [1].
Recently, the Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke (DEFUSE 3) trial reported the efficacy of EVT that occurred within 6 to 16 hours of the time last known well with selection by perfusion imaging. The authors of the trial noted that approximately 40% of the patients in the DEFUSE 3 trial did not meet the DAWN selection criteria. We expect that a much larger population would have been able to undergo EVT had we applied the DEFUSE 3 criteria in addition to the DAWN criteria [7]. Our study showed that the number of patients who should be screened upon arrival should increase significantly. However, resources such as vascular neurologists and MRI equipment would be required in order for this to occur. Moreover, as the application of the DAWN criteria requires specific resources, such as acute image analysis tools and interventionists, setting up these resources and establishing rapid patient referral systems between primary and comprehensive stroke centers would be necessary.
Several limitations should be noted. First, there have been no recent efforts to shorten the interval from arrival to DWI acquisition in patients arriving within the DAWN time window; therefore, the delay in DWI acquisition might have resulted in an increase in infarct volume and, ultimately, the underestimation of the eligible study population. Second, as the CRCS-K registry is mostly composed of tertiary hospitals, it should be noted that there is a limitation in generalizing our results to the entire Korean stroke population. Additionally, because the United States acute ischemic stroke population was presumed using disease codes at discharge, the patient numbers and age and sex structure based on this population may differ from the true population.
Acknowledgments
The Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI10C2020) supported this study.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21. doi: 10.1056/NEJMoa1706442. [DOI] [PubMed] [Google Scholar]
- 2.Lim JS, Kim N, Jang MU, Han MK, Kim S, Baek MJ, et al. Cortical hubs and subcortical cholinergic pathways as neural substrates of poststroke dementia. Stroke. 2014;45:1069–1076. doi: 10.1161/STROKEAHA.113.004156. [DOI] [PubMed] [Google Scholar]
- 3.Kim DE, Park KJ, Schellingerhout D, Jeong SW, Ji MG, Choi WJ, et al. A new image-based stroke registry containing quantitative magnetic resonance imaging data. Cerebrovasc Dis. 2011;32:567–576. doi: 10.1159/000331934. [DOI] [PubMed] [Google Scholar]
- 4.Ryu WS, Woo SH, Schellingerhout D, Chung MK, Kim CK, Jang MU, et al. Grading and interpretation of white matter hyperintensities using statistical maps. Stroke. 2014;45:3567–3575. doi: 10.1161/STROKEAHA.114.006662. [DOI] [PubMed] [Google Scholar]
- 5.Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean Stroke Society and Clinical Research Center for stroke. J Stroke. 2013;15:2–20. doi: 10.5853/jos.2013.15.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otite FO, Liaw N, Khandelwal P, Malik AM, Romano JG, Rundek T, et al. Increasing prevalence of vascular risk factors in patients with stroke: a call to action. Neurology. 2017;89:1985–1994. doi: 10.1212/WNL.0000000000004617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718. doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]