Abstract
Objectives
Despite the decline in the use of electroconvulsive therapy (ECT) in patients with schizophrenia, ECT augmentation is still recommended for those with poor response to standard pharmacological intervention. However, the effectiveness of augmentation of antipsychotics with ECT on long-term clinical outcomes needs to be verified in an expanded sample.
Methods
Patients who were hospitalized for schizophrenia and received ECT for the first time during that hospitalization were identified from the total population health insurance database in Taiwan between 2002 and 2011. A comparison group was randomly selected and matched by age, gender, calendar year of hospitalization, and duration of hospitalization. Using a mirror-image design, the changes in rates of psychiatric and overall hospitalization, length of hospital stay, number of emergency department visits, and direct medical costs across the 1-year pre- and post-treatment periods were examined.
Results
A total of 2074 patients with the same number of comparison participants were included in the analysis. The rate of re-hospitalization decreased significantly in the ECT group during the 1-year post-treatment period, while there was no significant difference in the comparison group. Correspondingly, the total medical expenses increased significantly in the non-ECT group, but not in the ECT group. Notably, the reduction in the psychiatric re-hospitalization rate in the ECT group was more pronounced among those treated with clozapine or a medium-high average daily dose of antipsychotics.
Conclusion
This 1-year mirror-image analysis indicated that augmentation of antipsychotics with ECT in schizophrenic patients was associated with a reduced rate of psychiatric re-hospitalization.
Keywords: electroconvulsive therapy, schizophrenia, long-term outcome, re-hospitalization, medical costs
Introduction
Schizophrenia is a chronic mental disorder that bears heavy disease burden.1,2 Approximately 30% of patients with schizophrenia do not respond to standard antipsychotic treatment.3 The prognosis for such treatment-resistant schizophrenia is poor, characterized by long-term functional impairment and repeated exacerbations.3
Electroconvulsive therapy (ECT) has been used in psychotic patients since 1930s.4 A recent review indicated that ECT use in schizophrenia patients resulted in greater clinical improvement and higher discharge rates than placebo or sham ECT.5 However, the use of ECT has declined in recent decades since the introduction of antipsychotics.6 Currently, ECT is mainly used as an augmentative treatment for patients with schizophrenia who are resistant to pharmacotherapy.7–10 Its effectiveness has been supported by 2 recent meta-analyses that demonstrated a significant effect in reducing symptom severity among those who received ECT augmentation of clozapine or nonclozapine antipsychotics.11,12
Few studies have specifically investigated the effect of ECT augmentation with antipsychotics for schizophrenia on long-term relapse/re-hospitalization rates. One case series that enrolled 11 clozapine-resistant patients with schizophrenia showed that 63% relapsed within months after ECT was discontinued.13 Another uncontrolled, small-scale study including 28 adolescents with schizophrenia-spectrum disorder showed that over 30% of patients who received ECT augmentation were re-hospitalized during a 1-year follow-up period.14 These high relapse rates might have reflected the underling severity of disease rather than the therapeutic effect of ECT. Currently, there is no long-term, randomized controlled clinical trial to evaluate the efficacy of ECT augmentation with antipsychotics for treatment-refractory schizophrenia. Pending a comparison group, whether ECT augmentation had an effect on reducing relapses remains elusive. Additionally, potential factors affecting ECT response and outcome could not be properly explored with the small number of participants enrolled in these previous studies.
The current study aimed to examine whether ECT augmentation reduced re-hospitalization within 1 year after discharge. The study was conducted in a population-based study sample drawn from a nationwide database that included all patients with schizophrenia who received ECT augmentation and a properly matched comparison group of patients who received pharmacotherapy alone. The current study employed a mirror-image study design to examine the changes in various clinical outcome indices 1-year before and after the ECT. The outcome indices included psychiatric and overall hospitalization rates, length of hospital stay, number of emergency department (ED) visits, and direct medical costs during the pre- and post-treatment periods. In addition, factors affecting the effectiveness of ECT were also examined.
Methods
Data Source and Study Sample
The current study utilized data from the total Taiwanese population collected in the National Health Insurance Research Database (NHIRD) derived from the health insurance claims records in Taiwan’s National Health Insurance (NHI) program. By 2009, 99.8% of the Taiwanese population had been enrolled in the NHI program. The data from 2001 to 2012 was included in this study. The NHIRD includes beneficiaries’ demographics, medical contacts, ICD-9-CM diagnoses, and prescription/treatment claims. This study was approved by the Research Ethics Committee of the National Taiwan University Hospital.
In Taiwan, most ECT treatments are performed during hospitalization; hence, we included only those patients treated with ECT in an inpatient setting. In order to have a 1-year observation period before and after the index hospitalization, only psychiatric hospitalizations for schizophrenia between 2002 and 2011 were considered in this study. During the study period, there were 2821 patients with 4434 psychiatric admissions with ECT (27.2% of patients were hospitalized with ECT more than once) and 78742 patients with 279752 psychiatric admissions without ECT. Three patients with ECT (0.07% per hospitalization) and 441 patients without ECT (0.16% per hospitalization) died during hospitalization and hence were excluded from further analyses.
We applied a new user design15 and included only patients who received their first ECT during the study period since including previous ECT recipients could over-estimate treatment effectiveness as ECT might have been chosen due to a previous good response. Thus, 163 patients who received ECT before 2002 were excluded. Another concern was that including newly diagnosed schizophrenia patients in a mirror-image design study might induce asymmetric bias because they would not receive any treatment before the diagnosis was confirmed. Therefore, we excluded patients with an illness duration of schizophrenia that was less than 1 year from the admission date (n = 390). Furthermore, we excluded those with long-term hospitalizations, specifically durations >180 days (n = 114), who might have had a complicated treatment course or were treated in a different treatment setting (such as long-term care facilities or psychiatric day-care hospitals). Based on above-mentioned exclusion criteria, there remained 5 hospitalized patients who received only ECT without antipsychotics, thus we further excluded these cases. Moreover, 72 patients received maintenance ECT after discharge were also excluded. Finally, 2074 patients with augmentation ECT were included in the analysis.
Because the practice patterns might have varied across hospital settings, we selected comparison participants only from those hospitals that provided ECT. If a comparison patient had repeat hospitalizations during the study period, one among them was randomly selected as the comparison index hospitalization. In total, there were 41750 patients who had psychiatric hospitalizations and were treated with antipsychotics but not ECT during the study period. For each patient treated with ECT, we randomly selected one comparison participant matched by age group (<25, 25–44, 45–64, or ≥65), gender, calendar year of hospitalization, and duration of hospitalization (≤30, 31–90, or 91–180 days). As a result, a total of 2074 matched comparison participants were included in this study.
Patient Characteristics and Potential Confounders
Demographic variables included age at index hospitalization, gender, and calendar year of index hospitalization; and comorbid psychiatric conditions included mood disorders (ICD-9-CM: 296.x, 300.4, and 311), alcohol or substance use disorders (ICD-9-CM: 291.x, 292.x, 303.x, 304.x, 305.0, 305.2–305.9, 357.5, 425.5, 535.3, 571.0, 571.1, 571.2, and 571.3), and epilepsy (ICD-9-CM: 345.x).
The number and average daily dose of antipsychotics used during the index hospitalization were also assessed. The average daily dose was calculated by using the defined daily dose (DDD), “the assumed average maintenance dose per day for a drug used for its main indication in adults.”16 We calculated the cumulative dose by multiplying the tablet size of the DDD by the total number of tablets prescribed during the index hospitalization. If two or more antipsychotics were used, individual cumulative doses were added together. The average daily dose was then calculated by dividing the cumulative dose by the length of the index hospitalization. We further categorized the average daily dose into low (<1 DDD) and medium-high dose (≥1 DDD). Clozapine use was specifically quantified to evaluate ECT’s effectiveness in augmenting its use in treatment refractory schizophrenia. We also examined the long-acting antipsychotic injections commonly administrated to those with a history of poor compliance.
Outcome Measures
The primary outcome indices were psychiatric hospitalization and overall hospitalization (psychiatric and nonpsychiatric). The secondary outcome indices included the length of psychiatric and overall hospitalizations, the number of ED visits, and direct medical costs.
Direct medical costs were calculated from the actual claims records in outpatient, emergency department, and inpatient settings, encompassing those of hospitalization, health care professional consultations, medications, laboratory tests, imaging, surgery, and medical procedures performed in both psychiatric and nonpsychiatric departments. All costs were reported in New Taiwan dollars (NT$); the approximate exchange rate of the NT$ in US dollars was 31.5 in 2008.
Statistical Analysis
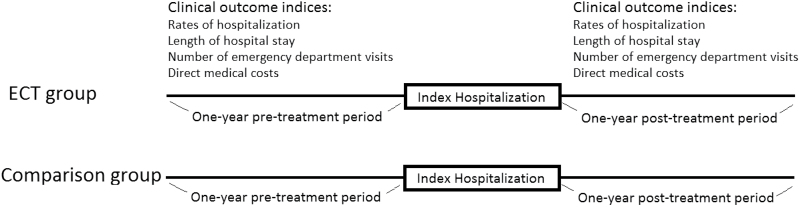
We applied a mirror-image study design in the present study. Specifically, this mirror-image study design, in which the participants served as their own controls, was used to explore changes in the outcome indices across the 1-year pre- and post-treatment periods. The pretreatment period was the 1-year period preceding the admission date of the index hospitalization; the post-treatment period was the 1-year period after the discharge date of the index hospitalization (figure 1).
Fig. 1.
Mirror-image design.
We applied conditional logistic regression with a stratum by each patient to evaluate the change in probability of psychiatric hospitalization or overall hospitalization from the pre- to the post-treatment period. Wilcoxon matched-pair signed-rank tests were conducted to examine the changes in length of psychiatric or overall hospital stay, number of ED visits, and direct medical costs across the pre- and post-treatment mirror-periods.
To compare the differences in the change of the rate of psychiatric hospitalization between the ECT and comparison groups, we combined the data from these 2 groups and used a conditional logistic regression model to test the interactions between treatment and group (ECT vs comparison participants). If the interactions between treatment and group are significant, this would indicate that ECT had a significant impact on the differences in the change of the rate of psychiatric hospitalization between pre- and post-treatment. In addition, we used the Wilcoxon rank-sum test to test the difference in changes in length of hospitalization, number of ED visits, and direct medical costs between the ECT and comparison groups. Subgroup analyses were employed to investigate the association between various factors related to demographic and clinical characteristics, and the rate of psychiatric hospitalization in the ECT and comparison groups, separately. Statistical significance was assessed using 95% CIs or a P-value <.05. All analyses were conducted with SAS 9.4 software (SAS Institute).
Results
During the study period from 2002 to 2011, the inpatient use of ECT augmentation for schizophrenia declined significantly while the total number of psychiatric hospitalizations increased (table 1). Compared to patients not receiving ECT, those receiving ECT were more likely to be younger and female and have comorbid epilepsy. After matching by age group, gender, duration of hospitalization, and calendar year of hospitalization, patients receiving ECT were more likely to receive more types and higher average daily doses of antipsychotics. In addition, clozapine and long-acting injectable antipsychotics were more frequently used in patients receiving ECT than in those in the comparison group (table 1). The number of ECT session was 7.3 ± 5.9. The information for the type of ECT was not available in the NHIRD.
Table 1.
Baseline Characteristics of Inpatients With and Without Electroconvulsive Therapy
| Overall Study Sample | Matched Sample | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ECT Group (n = 4434)a | Comparison Group (n = 279752)a | P-Value | ECT Group (n = 2074)b | Comparison Group (n = 2074)b | P-Value | |||||
| N | (%) | N | (%) | N | (%) | N | (%) | |||
| Age groups | ||||||||||
| <25 | 588 | (13.3) | 33080 | (11.8) | 212 | (10.2) | 212 | (10.2) | ||
| 25–44 | 2544 | (57.4) | 154039 | (55.1) | <.001 | 1238 | (59.7) | 1238 | (59.7) | N/A |
| 45–64 | 1202 | (27.1) | 82970 | (29.7) | 584 | (28.2) | 584 | (28.2) | ||
| ≥65 | 100 | (2.3) | 9663 | (3.5) | 40 | (1.9) | 40 | (1.9) | ||
| Gender | ||||||||||
| Female | 2149 | (48.5) | 118362 | (42.3) | <.001 | 938 | (45.2) | 938 | (45.2) | N/A |
| Male | 2285 | (51.5) | 161390 | (57.7) | 1136 | (54.8) | 1136 | (54.8) | ||
| Duration of index hospitalization, days | ||||||||||
| ≤30 | 932 | (21.0) | 96464 | (34.5) | 383 | (18.5) | 383 | (18.5) | N/A | |
| 31–90 | 2772 | (62.5) | 104744 | (37.4) | 1418 | (68.4) | 1418 | (68.4) | ||
| 91–180 | 516 | (11.6) | 25726 | (9.2) | <.001 | 273 | (13.2) | 273 | (13.2) | |
| >180 | 214 | (4.8) | 52818 | (18.9) | ||||||
| Calendar year of hospitalization | ||||||||||
| 2002–2003 | 1003 | (22.6) | 51567 | (18.4) | 537 | (25.9) | 537 | (25.9) | ||
| 2004–2005 | 940 | (21.2) | 56422 | (20.2) | 459 | (22.1) | 459 | (22.1) | ||
| 2006–2007 | 927 | (20.9) | 55239 | (19.7) | <.001 | 435 | (21.0) | 435 | (21.0) | N/A |
| 2008–2009 | 853 | (19.2) | 55961 | (20.0) | 381 | (18.4) | 381 | (18.4) | ||
| 2010–2011 | 711 | (16.0) | 60563 | (21.6) | 262 | (12.6) | 262 | (12.6) | ||
| Comorbid conditions | ||||||||||
| Mood disorder | 344 | (7.8) | 21002 | (7.5) | 0.53 | 147 | (7.1) | 131 | (6.3) | 0.32 |
| Alcohol or substance use disorder | 376 | (8.5) | 38542 | (13.8) | <.001 | 160 | (7.7) | 200 | (9.6) | 0.03 |
| Epilepsy | 320 | (7.2) | 16574 | (5.9) | <.001 | 128 | (6.2) | 75 | (3.6) | <.001 |
| Antipsychotic treatment during hospitalization | ||||||||||
| Number of oral antipsychotics | ||||||||||
| None | 17 | (0.4) | 3364 | (1.2) | ||||||
| Monotherapy | 899 | (20.3) | 142796 | (51.0) | <.001 | 361 | (17.4) | 933 | (45.0) | <.001 |
| Polytherapy | 3511 | (79.2) | 131431 | (47.0) | 1713 | (82.6) | 1141 | (55.0) | ||
| Average daily dose of antipsychotics, DDD | ||||||||||
| 0 | 17 | (0.4) | 3364 | (1.2) | ||||||
| Low (<1 DDD) | 1039 | (23.4) | 123133 | (44.0) | <.001 | 460 | (22.2) | 876 | (42.2) | <.001 |
| Medium-high (≥1 DDD) | 3378 | (76.2) | 153255 | (54.8) | 1614 | (77.8) | 1198 | (57.8) | ||
| Use of clozapine | 1964 | (44.3) | 45897 | (16.4) | <.001 | 906 | (43.7) | 360 | (17.4) | <.001 |
| Long-acting antipsychotic injections | 1631 | (36.8) | 52208 | (18.7) | <.001 | 811 | (39.1) | 449 | (21.6) | <.001 |
Note: N/A, not applicable; ECT, electroconvulsive therapy; DDD, defined daily dose.
aThe number in the overall original sample indicated the number of hospitalizations. One patient might contribute several hospitalizations.
bThe number in the matched sample could be the number of patients because only hospitalization with first ECT were included.
Overall, patients receiving ECT have higher psychiatric hospitalization rate than comparison groups, no matter in pre- or post-treatment periods. However, the patterns of change were distinct between the 2 groups (table 2). In the group of patients treated with ECT, the rate of psychiatric hospitalization during the post-treatment period was significantly less than that during the pretreatment period (53.4% vs 59.4%; odds ratio [OR] = 0.74, 95% CI = [0.65–0.85], P < .001). In contrast, there were no overt changes between the rates of psychiatric hospitalizations in the post- and pretreatment periods among comparison participants (42.2% vs 40.8%; OR = 1.09, 95% CI = [0.94–1.26], P = .28). Similar patterns were found for overall hospitalizations.
Table 2.
Changes in Clinical Indices Across Pre- and Post-Treatment Mirror-Image Comparison Periods Among Inpatients With and Without ECT
| Participants With ECT (n = 2074) | Comparison Participants Without ECT (n = 2074) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Prehospitalization | Posthospitalization | P-Value for Pre-Post Comparison | Prehospitalization | Posthospitalization | P-Value for Pre-Post Comparison | P-Value for Between Group Comparisons | |||
| Primary outcomes | N (%) | N (%) | ORs (95% CI) | N (%) | N (%) | ORs (95% CI) | |||
| Psychiatric hospitalization | 1231 (59.4) | 1107 (53.4) | 0.74 (0.65–0.85) | <.001 | 847 (40.8) | 876 (42.2) | 1.09 (0.94–1.26) | 0.28 | <.001 |
| Overall hospitalization | 1297 (62.5) | 1173 (56.6) | 0.74 (0.65–0.85) | <.001 | 947 (45.7) | 1000 (48.2) | 1.15 (1.00–1.33) | 0.06 | <.001 |
| Secondary outcomes | Mean ± SD | Mean ± SD | Difference | P-value | Mean ± SD | Mean ± SD | Difference | P-value | |
| Psychiatric hospitalizations, days | 76.1 ± 102.5 | 72.4 ± 103.7 | -3.7 | 0.43 | 49.6 ± 45.6 | 62.9 ± 58.3 | 13.3 | <.001 | <.001 |
| Overall hospitalizations, days | 77.5 ± 103.3 | 73.9 ± 104.0 | -3.6 | 0.50 | 50.9 ± 92.3 | 64.7 ± 105.6 | 13.8 | <.001 | <.001 |
| ED visits, number | 1.3 ± 2.9 | 0.9 ± 2.9 | -0.4 | <.001 | 1.0 ± 2.5 | 0.7 ± 1.9 | -0.3 | <.001 | <.001 |
| Medical costs, 1000 NTD | 132.8 ± 124.8 | 134.6 ± 171.7 | 1.8 | 0.57 | 88.0 ± 96.4 | 106.2 ± 112.8 | 18.3 | <.001 | <.001 |
Note: N/A, not applicable; ED, emergency department; NTD, New Taiwan Dollar; OR, odds ratio. P-value for pre-post comparison was determined by conditional logistic regression with a stratum by each patient or by Wilcoxon matched-pair signed-rank tests among ECT or comparison groups, respectively. P-value for between group comparisons was determined using a conditional logistic regression model to test the interactions between treatment and comparison group on the change in probability of hospitalization or by Wilcoxon rank-sum test for the pre-post difference between ECT and comparison groups.
In terms of the secondary outcomes, the number of ED visits declined in both groups; however, the magnitude of the decrease was greater in the ECT group than in the comparison group. The length of psychiatric hospital stay did not change in the ECT group (−3.7 days, P = .43) but increased significantly in the comparison group (+13.3 days, P < .001). The direct medical costs did not change in the ECT group (+1800 NT$, P = .57) but increased significantly in the comparison group (+18300 NT$, P < .001) (table 2).
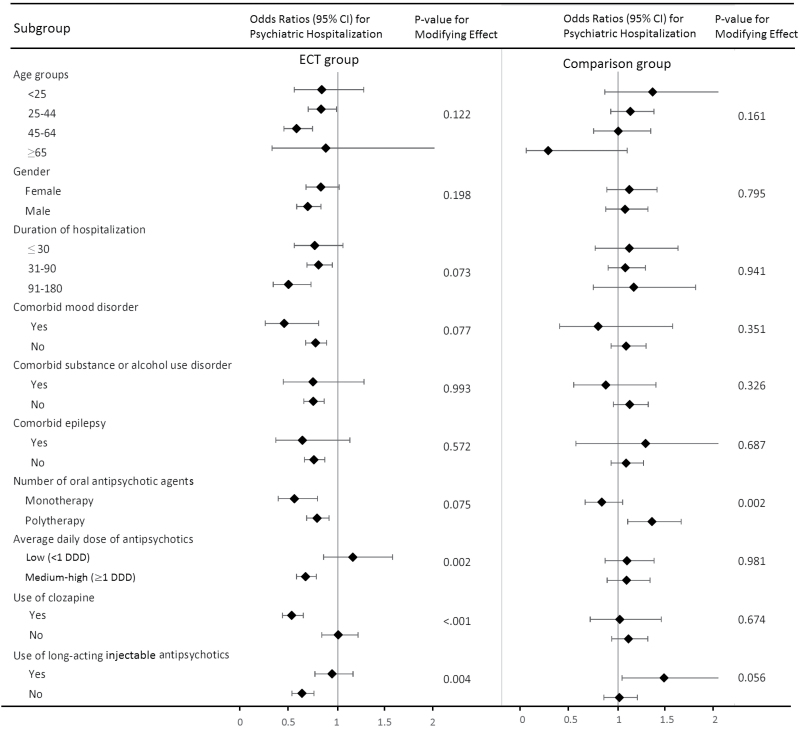
Figure 2 shows the results of the subgroup analyses. We found that age group, gender, duration of index hospitalization, comorbidity with epilepsy, substance or alcohol use disorders, and the number of antipsychotic medications used during the index hospitalization did not have modifying effects on the changes in the rates of psychiatric hospitalization between the pre-ECT and post-ECT periods. However, the effects of ECT on reducing psychiatric re-hospitalizations were more marked among those treated with medium-high average daily doses of antipsychotics, or clozapine, and those not treated with long-acting injectable antipsychotics. In addition, the changes in the rate of psychiatric hospitalization were marginally more prominent among those with mood disorders than among those without comorbid mood disorders (P = .08).
Fig. 2.
The odds ratios of psychiatric hospitalization in post-treatment period compared to those in pretreatment periods, subgroup analysis by patients’ characteristics. Note: P-value for the modifying effect was determined by the interactions between treatment and patient’s characteristics (age groups, gender, etc.) in conditional logistic regression. If P-value <.05, this would indicate that the patient’s characteristics had a significant impact on the differences in the change of the rate of psychiatric hospitalization between pre- and post-treatment.
Discussion
The current study used a mirror-image design to evaluate the changes in important clinical outcome indices across the pre- and post-treatment periods in patients receiving ECT augmentation as compared to those not receiving ECT. The results indicated that the rate of psychiatric hospitalization decreased among patients treated with ECT, but not in the comparison patients. Furthermore, the comparison group had increased hospitalization days and medical expenses during the 1-year period following the index hospitalization while the ECT group did not. Notably, the effectiveness of ECT was more pronounced among those treated with clozapine or a medium-high average daily dose of antipsychotics.
The effectiveness of combined treatment with ECT and antipsychotics in reducing symptoms has been demonstrated by several clinical trials and reviews9–12; however, few studies have examined the long-term effectiveness of ECT augmentation of antipsychotics in patients with schizophrenia. One small-scale double-blind study (n = 25) showed that those with ECT augmentation of antipsychotics had a 20% re-hospitalization rate within 6 months while those treated with sham ECT and antipsychotics had a 70% re-hospitalization rate.10 A Cochrane review also found that ECT resulted in fewer relapses in the short term than did sham ECT (n = 47, relative risk = 0.26; 95% CI = [0.03–2.2]), although the finding did not reach statistical significance.5 Three studies showed that ECT augmentation had an early advantage but there were no differences in long-term outcomes.7,17,18 Given the small sample sizes in these studies, such inconsistent findings might have been the result of clinical heterogeneity; thus, studies that include expanded, representative samples are crucial.
To the best of our knowledge, this study was the largest study to date to explore the effectiveness of ECT augmentation on long-term clinical outcomes. During the 1-year observation period, we found that ECT was associated with a reduced rate of re-hospitalization. This finding could not be explained by the time trend since the rate of psychiatric hospitalization in the comparison group did not show a statistically significant change during the same time frame. In addition, the overall number of psychiatric hospitalizations for schizophrenia increased during the study period. This increasing trend might have been due to the increase in mental health facilities in Taiwan during the same time period. In addition, the increases in medical expenditures might have been caused by the introduction of second generation antipsychotics. However, we noted that the hospital stays and direct medical costs did not increase in the ECT group. These findings demonstrate that ECT augmentation of antipsychotics could help to reduce the trend of increasing mental health service utilization and medical expenses. No change in direct medical costs might also be attributed to a reduction in direct hospitalization costs as a result of fewer hospitalizations that could have been offset by increased outpatient costs.19,20
Intriguingly, we found that ECT augmentation of clozapine might be more effective than ECT augmentation of other antipsychotics. These findings could not be explained by the therapeutic effect of clozapine alone. In the comparison group, we did not find the effect of clozapine use to be superior to nonclozapine antipsychotic treatment (P = .67). Therefore, it is likely that the combination of ECT and clozapine might have had a synergistic effect. These findings were consistent with the findings from one randomized controlled trial of adolescents with schizophrenia spectrum disorder, which showed that the rate of re-hospitalization during a 1-year follow-up was lower in the group treated with ECT and clozapine (7.1%) than in the ECT and nonclozapine group (58.3%).14 This is also in line with the recent recommendations that ECT should be considered in those refractory to clozapine treatment.21,22
The decreased rate of re-hospitalization and improvement in other clinical indices could not be solely attributed to ECT. We found that the effectiveness of ECT augmentation was not statistically significant for those treated with low average daily doses of antipsychotics. Previous studies have shown that treatment with antipsychotics had a better effect than treatment with ECT alone.5 We believe that the synergistic effect of ECT and antipsychotics contributed to the improvement in clinical outcomes. ECT might have a rekindling effect on pharmacotherapy; therefore, the improvement could be continued after ECT treatment.23 Furthermore, the combination of ECT and antipsychotics could reduce residual symptoms, thereby decreasing the risk of relapse.24 In addition, the effectiveness of ECT in schizophrenic patients may be via the modulation of dopamine and serotonin neurotransmitter activity,25 neurotrophic effects such as increased serum BDNF levels,25,26 and anti-inflammatory effects,27which could further improve the clinical outcome of patients with schizophrenia.
We found that patients treated with long-acting injectable antipsychotics did not show reduced re-hospitalization rates during the post-treatment period. This might have been because long-acting injectable antipsychotics were administrated to patients with a history of medication noncompliance. Despite the use of long-acting injectable antipsychotics, these patients were still more likely to have poor medication compliance28 and this attenuated the effect of ECT on relapse prevention. Therefore, the importance of adequate antipsychotic treatment could not be overemphasized.
Although neither demographic variables nor underlying comorbid conditions of the patients significantly modified the effectiveness of ECT, our findings indicated that schizophrenic patients with comorbid mood disorders showed a trend of better response to ECT augmentation, which is consistent with previous reports that schizophrenic patients with suicidal behaviors had better responses to ECT.29,30 A growing body of literature has documented that depressive symptoms and depression are the most common correlates of suicidality in schizophrenia.31–33 The effectiveness of ECT augmentation for schizophrenic patients with mood symptoms warrants further investigation.
Limitations
There were several limitations to this study. First, as symptom severity was not available in the NHIRD, the changes in symptoms could not be ascertained, thus limiting the explanatory power regarding whether reduced hospitalizations were due to better symptom control. However, we used multiple clinical outcome indices, such as psychiatric re-hospitalizations and ED visits, to evaluate long-term outcomes, since both were often triggered by aggravated positive and/or aggressive symptoms. Second, information about potential clinical course confounders such as actual duration of illness, premorbid function, social support, and access to medical care was lacking. Nevertheless, it should be noted that the study participants served as their own control in comparing pre- and post-treatment indices; therefore, these factors were controlled to a certain extent and were unlikely to be the sole contributors to these changes. Third, the wash out period for excluding previous ECT users was only 1 year; hence, the sample population might have included some patients who had previously received and responded well to ECT, which could have resulted in an overestimation of the effectiveness of ECT. Fourth, because details about the ECT treatment, such as bilateral or unilateral and frequency of administration were not clear, we could not assess the impact of different types of ECT on treatment effectiveness. Fifth, we included a comparison group to evaluate the effect of time trend of health system utilization. It should be noted that the disease severity between these 2 groups could be different even though the duration of index hospitalization was equal. It is possible that patients with different clinical severity could have different time trends. Finally, even though we found no change in direct medical costs in the ECT group, indirect medical costs were not available in the NHIRD. Further studies are needed to clarify changes in both direct and indirect costs of ECT.
Despite such limitations, this study addressed previous methodological shortcomings by including a comparison group to control for the effects of time bias and overall changes in treatment pattern over the study period. The results clearly demonstrated that ECT augmentation of antipsychotics provided robust long-term effectiveness in reducing psychiatric re-hospitalizations and the number of ED visits by patients with schizophrenia. In addition, we identified several important factors related to patient responses to ECT in the course of this study.
Clinical Implications
ECT augmentation of antipsychotic treatment was effective in reducing re-hospitalization rates and other clinical outcome indices in participants diagnosed with schizophrenia. Adequate antipsychotic treatment, including the use of medium-high, average daily doses of antipsychotics or clozapine might have a synergistic effect in improving clinical outcomes in this patient population. Despite the known and demonstrated effectiveness of ECT in patients with schizophrenia, the utilization of ECT declined from 2002 to 2011. A similar trend of declining ECT use has been noted in the United States and other countries.34,35 Although several new brain-stimulation treatments such as repetitive transcranial magnetic stimulation and transcranial direct current stimulation have been developed, the evidence for their effectiveness in treatment-refractory schizophrenia is still sparse.36,37 ECT is still the treatment of choice for those who do not respond to antipsychotics.
Conclusions
This study demonstrated the associations between ECT augmentation of antipsychotics and the reduction in rate of hospitalization and ED visits during a 1-year follow-up period after treatment with ECT. In addition, the effectiveness of ECT was noteworthy among those treated with medium-high, average daily doses of antipsychotics or with clozapine. A prospective controlled clinical trial is indicated to confirm the causal associations.
Funding
This work was supported by the National Taiwan University Hospital (NTUH-105-N3221 and 106-N3621) and National Health Research Institutes, Taiwan (PI: Tsai, PH–104–PP–14, PH–104–SP–05 and PH–104–SP–16).
Acknowledgments
We thank Tami R. Bartell at Ann & Robert H. Lurie Children’s Hospital of Chicago, Stanley Manne Children’s Research Institute for English editing. This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance of the Department of Health, Taiwan, and managed by the National Health Research Institutes, Taiwan. The interpretation and conclusions contained in this article do not represent those of the Bureau of National Health Insurance, the Department of Health, or the National Health Research Institutes. The National Taiwan University Hospital and National Health Research Institutes had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
References
- 1. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet 2013;382:1575–1586. [DOI] [PubMed] [Google Scholar]
- 2. Brenner HD, Dencker SJ, Goldstein MJ, et al. Defining treatment refractoriness in schizophrenia. Schizophr Bull. 1990;16:551–561. [DOI] [PubMed] [Google Scholar]
- 3. Kennedy JL, Altar CA, Taylor DL, Degtiar I, Hornberger JC. The social and economic burden of treatment-resistant schizophrenia: a systematic literature review. Int Clin Psychopharmacol. 2014;29:63–76. [DOI] [PubMed] [Google Scholar]
- 4. Endler NS. The origins of electroconvulsive therapy (ECT). Convuls Ther. 1988;4:5–23. [PubMed] [Google Scholar]
- 5. Tharyan P, Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev. 2005:CD000076. [DOI] [PubMed] [Google Scholar]
- 6. Fink M. Convulsive therapy: a review of the first 55 years. J Affect Disord. 2001;63:1–15. [DOI] [PubMed] [Google Scholar]
- 7. Abraham KR, Kulhara P. The efficacy of electroconvulsive therapy in the treatment of schizophrenia. A comparative study. Br J Psychiatry. 1987;151:152–155. [DOI] [PubMed] [Google Scholar]
- 8. Tang WK, Ungvari GS. Efficacy of electroconvulsive therapy combined with antipsychotic medication in treatment-resistant schizophrenia: a prospective, open trial. J ECT. 2002;18:90–94. [DOI] [PubMed] [Google Scholar]
- 9. Petrides G, Malur C, Braga RJ, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am J Psychiatry. 2015;172:52–58. [DOI] [PubMed] [Google Scholar]
- 10. Goswami U, Kumar U, Singh B. Efficacy of electroconvulsive therapy in treatment resistant schizophreinia: a double-blind study. Indian J Psychiatry. 2003;45:26–29. [PMC free article] [PubMed] [Google Scholar]
- 11. Lally J, Tully J, Robertson D, Stubbs B, Gaughran F, MacCabe JH. Augmentation of clozapine with electroconvulsive therapy in treatment resistant schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2016;171:215–224. [DOI] [PubMed] [Google Scholar]
- 12. Zheng W, Cao XL, Ungvari GS, et al. Electroconvulsive therapy added to non-clozapine antipsychotic medication for treatment resistant schizophrenia: meta-analysis of randomized controlled trials. PLoS One. 2016;11:e0156510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kho KH, Blansjaar BA, de Vries S, Babuskova D, Zwinderman AH, Linszen DH. Electroconvulsive therapy for the treatment of clozapine nonresponders suffering from schizophrenia—an open label study. Eur Arch Psychiatry Clin Neurosci. 2004;254:372–379. [DOI] [PubMed] [Google Scholar]
- 14. Flamarique I, Castro-Fornieles J, Garrido JM, et al. Electroconvulsive therapy and clozapine in adolescents with schizophrenia spectrum disorders: is it a safe and effective combination?J Clin Psychopharmacol. 2012;32:756–766. [DOI] [PubMed] [Google Scholar]
- 15. Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158:915–920. [DOI] [PubMed] [Google Scholar]
- 16. WHO. WHO Collaborating Centre for Drug Statistic Methodology: Guidelines for ATC Classification and DDD Assignment. Oslo: WHO; 2009. [Google Scholar]
- 17. Taylor P, Fleminger JJ. ECT for schizophrenia. Lancet. 1980;1:1380–1383. [DOI] [PubMed] [Google Scholar]
- 18. de la Serna E, Flamarique I, Castro-Fornieles J, et al. Two-year follow-up of cognitive functions in schizophrenia spectrum disorders of adolescent patients treated with electroconvulsive therapy. Journal of Child and Adolescent Psychopharmacology 2011;21:611–619. [DOI] [PubMed] [Google Scholar]
- 19. Latimer E, Wynant W, Clark R, et al. Underprescribing of clozapine and unexplained variation in use across hospitals and regions in the Canadian province of Québec. Clin Schizophr Relat Psychoses. 2013;7:33–41. [PubMed] [Google Scholar]
- 20. Fitton A, Benfield P. Clozapine: an appraisal of its pharmacoeconomic benefits in the treatment of schizophrenia. Pharmacoeconomics. 1993;4:131–156. [DOI] [PubMed] [Google Scholar]
- 21. Grover S, Chakrabarti S, Hazari N, Avasthi A. Effectiveness of electroconvulsive therapy in patients with treatment resistant schizophrenia: a retrospective study. Psychiatry Res. 2017;249:349–353. [DOI] [PubMed] [Google Scholar]
- 22. Grover S, Hazari N, Kate N. Combined use of clozapine and ECT: a review. Acta Neuropsychiatr. 2015;27:131–142. [DOI] [PubMed] [Google Scholar]
- 23. Hustig H, Onilov R. ECT rekindles pharmacological response in schizophrenia. Eur Psychiatry. 2009;24:521–525. [DOI] [PubMed] [Google Scholar]
- 24. Gaebel W, Riesbeck M. Are there clinically useful predictors and early warning signs for pending relapse?Schizophr Res. 2014;152:469–477. [DOI] [PubMed] [Google Scholar]
- 25. Rosenquist PB, Miller B, Pillai A. The antipsychotic effects of ECT: a review of possible mechanisms. J ECT. 2014;30:125–131. [DOI] [PubMed] [Google Scholar]
- 26. Li J, Ye F, Xiao W, et al. Increased serum brain-derived neurotrophic factor levels following electroconvulsive therapy or antipsychotic treatment in patients with schizophrenia. Eur Psychiatry. 2016;36:23–28. [DOI] [PubMed] [Google Scholar]
- 27. Kartalci S, Karabulut AB, Erbay LG, Acar C. Effects of electroconvulsive therapy on some inflammatory factors in patients with treatment-resistant schizophrenia. J ECT. 2016;32:174–179. [DOI] [PubMed] [Google Scholar]
- 28. Wu CS, Cheng IC, Feng J, Chen CL. Comparison of treatment effectiveness and medical costs for different long-acting injectable antipsychotics in patients with schizophrenia in Taiwan: a nationwide population-based cohort study. Schizophr Res. 2016;173:37–44. [DOI] [PubMed] [Google Scholar]
- 29. Phutane VH, Thirthalli J, Kesavan M, Kumar NC, Gangadhar BN. Why do we prescribe ECT to schizophrenia patients?Indian J Psychiatry. 2011;53:149–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pompili M, Lester D, Dominici G, et al. Indications for electroconvulsive treatment in schizophrenia: a systematic review. Schizophr Res. 2013;146:1–9. [DOI] [PubMed] [Google Scholar]
- 31. Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull. 1990;16:571–589. [DOI] [PubMed] [Google Scholar]
- 32. Fuller-Thomson E, Hollister B. Schizophrenia and suicide attempts: findings from a representative community-based Canadian sample. Schizophr Res Treatment. 2016;2016:3165243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15:127–135. [DOI] [PubMed] [Google Scholar]
- 34. Case BG, Bertollo DN, Laska EM, et al. Declining use of electroconvulsive therapy in United States general hospitals. Biol Psychiatry. 2013;73:119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Verdura E, Vera I, Sanz-Fuentenebro J. Temporal trends in the use of ECT in Europe. Eur Psychiatry 2015;30:839. [Google Scholar]
- 36. Freitas C, Fregni F, Pascual-Leone A. Meta-analysis of the effects of repetitive transcranial magnetic stimulation (rTMS) on negative and positive symptoms in schizophrenia. Schizophr Res. 2009;108:11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kekic M, Boysen E, Campbell IC, Schmidt U. A systematic review of the clinical efficacy of transcranial direct current stimulation (tDCS) in psychiatric disorders. J Psychiatr Res. 2016;74:70–86. [DOI] [PubMed] [Google Scholar]