Abstract
Background
The cognitive processes involved in individuals’ perceptions and prioritization of information, and how these change with experience or exposure to interventions, are rarely examined in the evaluation of nutrition interventions. Exclusive breastfeeding counseling is a common infant and young-child feeding intervention and is used to promote HIV-free survival in the prevention of mother-to-child transmission programs. However, it is often designed without adequate attention to the changes in mothers’ perceptions over the course of their early breastfeeding experiences.
Objective
The aim of this study was to identify HIV-infected breastfeeding mothers’ cognitive structure (their organization of messages and ideas) of infant feeding messages and to characterize whether their cognitive organization of infant feeding messages changed from pregnancy through the first 5 mo postpartum.
Methods
With the use of semistructured interviews and the cognitive mapping technique of pile sorting, we interviewed 30 HIV-infected breastfeeding mothers in Port-au-Prince, Haiti. We asked them to sort and rate 18 infant feeding messages 3 times (during pregnancy, 0- to 1-mo postpartum, and 3- to 5-mo postpartum). We analyzed their responses by using multidimensional scaling, property fitting, and partition analyses.
Results
At all 3 visits, we found consistency in women's cognitive mapping of messages. For example, mothers consistently differentiated messages pertinent for exclusive breastfeeding compared with those that pertained to other practices. However, subtle variations in mothers’ cognition over time were also evident, particularly at 0- to 1-mo postpartum, when message proximity was tightly clustered compared with the earlier and later periods.
Conclusions
We conclude that mothers share a common cognitive organization of infant feeding messages and that this organization changes over time. Attention to variations in cognition can support context-sensitive, patient-centered counseling by practitioners and improve the effectiveness of nutrition interventions. Pile sorting is an efficient, systematic technique to examine cognitive processes related to health and nutrition.
Keywords: HIV, breastfeeding, infant and young child feeding, pregnant and lactating women, maternal perceptions, cognitive mapping, pile sorting, Haiti
Introduction
In nutrition, it is not only important to determine what kinds of interventions are effective but also to establish the process of how they are implemented and the issues and problems stakeholders face in that implementation (1, 2). This requires a set of methods to describe and interpret the processes by which individuals arrive at decisions about nutrition-related behaviors, as well as knowledge about the economic, political, social, and ethical factors that drive those decisions (1, 3). Individuals’ cognitive processes—how they perceive and organize the wide array of information they receive and the value judgments they make about it—have been consistently shown to be important determinants of nutrition-related behaviors (4, 5). These processes are dynamic and change with life experiences, including exposure to interventions. At present, the cognitive processes underlying nutrition-related behaviors are often not measured or captured in evaluations of nutrition outcomes.
Describing and interpreting the ways individuals think about information requires techniques from multiple disciplines. Because individuals’ perceptions are shaped by cultural norms and standards (5–7), investigators need tools to examine cultural patterns and shared cognitive models (3, 8). Pile sorting is one such technique. Pile sorting is a cognitive mapping methodology used in anthropology, psychology, and other disciplines to empirically describe how people cognitively shelve or organize information and items within a cultural domain (8, 9). The relations between different items can be visually represented as “cognitive maps” (9). Pile sorting has been applied in the fields of health and nutrition to study women's perceptions about reproductive health (10–12), caregivers’ perceptions about infant feeding behaviors (13), and foods for infant and young child feeding (14–17). Pile sorting permits researchers to examine cultural constructions or cultural knowledge and to analyze them graphically and statistically. Thus, pile sorting can be used to preserve an emic (or “insider's”) view of cognitive organization based on the categorizations and patterns that emerge from participants, while also providing a means of analysis from an etic perspective of the researcher (18–20). Pile sorting can also be used to supplement data from in-depth qualitative interviews with quantitative analyses that permit statistical inferences (21).
Breastfeeding counseling is a common nutrition intervention to support infant and young child feeding. However, in many countries, breastfeeding counseling is often prescriptive (22–24) and is generally provided to women uniformly, without flexibility or attention to mothers’ experiences and knowledge (25–27). By using cognitive mapping techniques to explore mothers’ cognitive processes as normative cultural patterns and comparing them over time, we can better understand mothers’ perspectives about infant feeding recommendations over the course of their breastfeeding experiences. This, in turn, can yield insights to promote better and timelier communication with mothers about their early infant feeding experiences (28, 29).
Effective breastfeeding management and counseling are particularly important and challenging in the context of HIV. Breastfeeding is one of the modes of vertical transmission of HIV, and HIV-infected mothers face unique and often isolating experiences in feeding their infants (22). Many physical, biological, social, and economic facilitators and barriers influence HIV-infected mothers’ perceptions about infant feeding (22, 24, 30–32). These mothers live in environments in which evidence-based recommendations from the health center often clash with culturally based recommendations from their households, social networks, and communities (33). Moreover, they face the moral dilemma of putting their child's life at risk of HIV or respecting cultural norms (33). How HIV-infected mothers think about and prioritize infant feeding recommendations can illuminate the tension between international infant feeding guidelines and these mothers’ social environments.
In this article, we explore HIV-infected Haitian mothers’ perspectives about infant feeding from pregnancy through the first 5 mo postpartum. We sought to determine whether the experience of breastfeeding, including the practice of breastfeeding and other factors such as exposure to recommendations about breastfeeding, changed mothers’ cognitive processes and how they perceived and prioritized infant feeding messages. We addressed the following questions: 1) What is the cognitive structure of HIV-infected breastfeeding mothers’ knowledge about infant feeding messages, and 2) is the way that HIV-infected, breastfeeding mothers organize infant feeding messages stable over time? To answer these questions, we conducted a repeated pile-sorting task and analyzed the responses with the use of nonparametric statistical and graphical methods to explore mothers’ cognitive processes over the course of their breastfeeding experience. This is a novel approach for analyzing pile-sorting results in nutrition. This approach combines the virtues of qualitative and quantitative methods to explore emic perspectives, which in nutrition research are typically analyzed with qualitative methods alone (Table 1).
TABLE 1.
Conceptual differences between etic and emic approaches in nutrition research
| Qualitative approach | Quantitative approach | |
|---|---|---|
| Etic approach | Constructs and hypotheses are predefined; subjects are asked to respond in relation to predefined categories, constructs and understandings [e.g., What barriers do you face when trying to exclusively breastfeed for 6 mo? (with prompts for social support, time, workplace, self-efficacy)] | Prespecified variables to measure dependent and independent variables; randomized controlled trials; prespecified regression models (e.g., What is the effect of social support on duration of exclusive breastfeeding?) |
| Emic approach | Constructs emerge from the data using locally-ascribed meaning and categories [e.g., Tell me about your experiences feeding your 3-mo-old baby? (with follow-up questions and identification of emergent themes)] | Varied methods to detect patterns that emerge from the data and quantitatively describe the similarities and differences (e.g., counts of emic themes, multidimensional scaling analysis of pile sorting, factor analysis of Q-sorts) |
Methods
Study context
The study was conducted in Port-au-Prince, Haiti, where exclusive breastfeeding is not the cultural norm. Although 98% of infants in Port-au-Prince are breastfed, only 68% are exclusively breastfed in the first month, 41% are exclusively breastfed at 2–3 mo, and 24% are exclusively breastfed at 4–5 mo (34).
We recruited participants from the Haitian Group for the Study of Kaposi's Sarcoma and Opportunistic Infections [Groupe Haitien d'Etude du Sarcome de Kaposi et des Infections Opportunistes (GHESKIO)] from June to December 2014. At GHESKIO, HIV-infected mothers receive free antenatal, postnatal, and pediatric outpatient care and are followed by GHESKIO's nutrition program, where they receive monthly growth monitoring and counseling for their infants (35). They also receive infant feeding counseling during antenatal care as well as during postnatal follow-up for themselves and their children. At the time of the study, GHESKIO's infant feeding programs for HIV-exposed infants were aligned with the 2013 Haitian national guidelines for the prevention of mother-to-child transmission of HIV, which corresponded to the 2012 WHO guidelines for infant feeding in the context of HIV (36). Thus, the women in our study were provided with lifelong antiretroviral therapy and received recommendations to exclusively breastfeed their HIV-exposed infants for the first 6 mo of life and to continue breastfeeding with appropriate introduction of complementary foods from 6 to 12 mo of life (or until an adequate and sustainable diet was achieved).
Study population and recruitment
To characterize a population, sample size requirements for cognitive mapping techniques, including pile sorting, depend on the variability of responses among participants. In this research, our goal was to test whether there were any longitudinal changes in women's cognitive organization of breastfeeding information as a function of time and experience from the prenatal period through the first few months postpartum. All of the women in our sample received antenatal care from GHESKIO, were HIV-infected, were breastfeeding (or had an intention to breastfeed), received the same information by the same health providers about breastfeeding, had children of the same age, and lived in or near urban areas of Port-au-Prince. Given these characteristics, we used procedures recommended by Weller (37) and Romney et al. (38) to calculate a sample size for a relatively homogenous group. We determined that we needed 17–29 participants to capture the normative pattern of HIV-infected, breastfeeding women who were followed at GHESKIO 95% of the time with a 0.99 confidence level.
We purposely sampled 30 HIV-infected pregnant women who intended to breastfeed for our initial sample, to account for loss to follow-up over time. We targeted mothers who expected to deliver before September 2014. We invited them to participate in a series of 3 semistructured interviews: during pregnancy, at 0- to 1-mo postpartum, and at 3- to 5-mo postpartum. All of the mothers were initially identified by health workers during their routine antenatal care visits. We explained to potential participants that we were interested in following them over time and that their participation (or lack thereof) would not affect the care or services they received at GHESKIO.
All of the participants provided oral and written informed consent before their enrollment in the study. The consent process was provided to the mothers in Haitian Creole. Ethical approval was granted by the GHESKIO Human Ethics Committee in Port-au-Prince, Haiti, and by the Institutional Review Board for Human Participants at Cornell University in Ithaca, New York. All of the mothers received compensation for transportation to and from the clinic, as well as a culturally appropriate gift (baby clothes and a framed photograph of their infant) to thank them for their participation in the study.
Data collection
The first author and the head of the nutrition clinic used a free-listing activity to compile a list of messages that mothers heard about infant feeding. Free listing is a technique used in cultural anthropology to characterize items in a cultural domain (18, 39). It typically precedes activities such as pile sorting (39, 40). Before conducting the interviews with the women who were followed longitudinally in the present study, we conducted the free-listing exercise with 43 key informants, in which we asked them to recall all of the messages they heard from various sources about infant feeding. We specifically probed for messages from the health center, family, friends, and others in the community. We report on the methods and findings from our free-listing activity in additional detail elsewhere (41). Both free listing and pile sorting, as well as other methods relevant to cultural domain analysis, are described in greater detail by Weller and Romney (40) and Borgatti and Halgin (39). For the interviews with the women in the present study, we selected 18 common infant messages from the free lists to inform the development of a semistructured interview guide (Table 2). We placed each of the 18 messages on an index card with a corresponding image and used the set of messages to guide the interview.
TABLE 2.
The common infant feeding messages used in the pile-sorting exercises with 30 HIV-infected Haitian women
| ID | Infant feeding message |
|---|---|
| 1 | Exclusively breastfeed for the first 6 mo, without giving any other food or liquids |
| 2 | Initiate breastfeeding early for your baby to habituate to the breast |
| 3 | Express your milk in a clean vessel if you are going out |
| 4 | Breastfeed regularly for your breast milk to be produced/to come |
| 5 | After 6 mo, breastfeed and give other foods until 1 y |
| 6 | You can breastfeed if you have HIV if you take your medication |
| 7 | If your breast is hurt, see the doctor and use your other breast in the interim |
| 8 | Exclusively breastfeed for the first 6 mo to protect the baby from getting HIV |
| 9 | Breastfeed the baby to protect it from illness/infection, such as diarrhea |
| 10 | Exclusively breastfeed because it is more economical |
| 11 | Breastfeed for the baby's brain to develop well |
| 12 | Breastfeed regularly so that your baby gains more weight |
| 13 | Give your baby other foods to prevent it from pulling gas from you |
| 14 | Do not breastfeed if you have not eaten well |
| 15 | Give the baby lok to clean the tar in the baby's gut1 |
| 16 | Do not breastfeed after 6 mo so that the baby does not get the virus |
| 17 | If you have bad blood or you have spent too much time out, do not breastfeed, your milk has spoiled |
| 18 | Wash your hands each time you are going to breastfeed |
Lok is a commonly used prelacteal feed in Haiti that is made from castor oil, grated nutmeg, sour orange juice, garlic, unrefined sugar, and water (42).
The first author and a research assistant conducted the semistructured interviews in Haitian Creole, interviewing mothers about their expectations of and experiences with breastfeeding. The set of cards with the messages was shuffled in random order at the beginning of each interview. During the interview, mothers were asked to sort the messages using an unconstrained pile-sorting technique (18, 39). That is, they were instructed to put together in piles all messages they felt “belonged together” using as many or as few piles as they wanted (40). Respondents were instructed to set aside any unfamiliar messages and not sort them. After mothers finished sorting the infant feeding messages, we asked them to explain why they sorted the messages the way they did, and probed for differences and similarities between the different piles (18, 40). After mothers completed the unconstrained sorting exercise, we asked them to rate each individual message on 2 features: importance and difficulty. For each feature, mothers could rate messages into 3 categories: very, somewhat, or not at all. After we finished this series of rating questions, we asked mothers to explain their ratings and probed for differences and similarities between the rated piles.
The interviews, which included the pile-sorting exercise itself and the discussions with mothers about their explanations of the similarities and differences between the piles, were audio-recorded, transcribed verbatim into Haitian Creole by a research assistant, and spot-checked for fidelity to the recordings by the first author. We repeated these procedures at the second and third visits.
Data analysis
Each respondent's Haitian Creole transcript was coded by using a standard grounded theory approach, which utilizes comparative analysis of the interview data to generate conceptual categories and identify emerging themes (43). The first author coded and analyzed the transcripts with NVivo version 10.2.2 (44), and discussed the coding scheme and a subset of the interview transcripts with 2 of the co-authors. The coding structure was composed of themes that can be regarded as mothers’ emic explanations of the similarities and differences between their piles, as well as etic themes that the authors had identified from previous research on breastfeeding. In an iterative process, as new themes emerged, the transcripts were reanalyzed. The quotes were translated from Haitian Creole to English. All of the findings were discussed with practitioners in Haiti.
The quantitative analysis of the pile-sorting exercise followed procedures recommended by Borgatti and Halgin (39). We first tabulated mothers’ responses into individual 18-by-18 message-similarity matrices, where “1” in the i-th row and the j-th column represented a pair of messages that were sorted together and “0” represented messages that were sorted in separate piles (39, 45). We combined the individual matrices into an aggregate 18 × 18 message-similarity matrix (i.e., a proximity matrix) by taking the mean of the individual matrices to account for the total number of times that 2 messages could have been sorted together (S Borgatti, University of Kentucky, personal communication, 2016). [The proximity matrix used the mean values, instead of the summed values, of the individual proximity matrices because mothers did not sort unfamiliar messages. Using the mean value accounts for analytical problems resulting from the unsorted messages (i.e., missing data)]. The proximity matrix represented the proportion of people who grouped each message-pair together. Values ranged from “0” to “1”, where “0” meant that no one grouped that message-pair together (i.e., everyone had a “0” in their individual similarity matrix) and where “1” meant that every person sorted that message pair together (i.e., everyone had a “1” in their similarity matrix) (45). Small values in the proximity matrix corresponded to pairs of messages that were conceptually different, and values closer to “1” corresponded to pairs of messages that were conceptually similar (46).
To answer our first research question about the cognitive structure of HIV-infected mothers’ knowledge about infant feeding messages, we used multidimensional scaling (MDS) of the proximity matrices to model the cognitive arrangements of messages (39), separately for each of the 3 visits. We completed the MDS analysis using Analytic Technologies' UCINET, version 6.614 (47). UCINET is a software program for social network and cultural domain analyses (47). Other software programs, such as ANTHROPAC (48), a DOS-based program specific for cultural domain analyses also developed by Analytic Technologies, and R-CMap (49), an open-source software implemented in R, can also be used to complete cultural domain analysis and display MDS plots. MDS is used to display proximities between message-pairs using Euclidean distance; greater distances or space between messages on the MDS plot indicate that those messages are not often grouped together and are not conceptually similar (45, 46). We ran the congruence procedure on our MDS plots to rotate and scale the pictures to make them maximally similar to one another for subsequent analyses (47).
For the purposes of our study, we used 2-dimensional, nonmetric MDS. Inasmuch as the 2-dimensional MDS plot is a distorted representation of an 18-dimension MDS plot (which would be a perfect representation of the 18 × 18 message-pair proximity matrix), we used the Kruskal stress test to determine the degree of distortion and the goodness-of-fit of the 2-dimensional MDS plot to the message-pair proximity matrix. A low stress value indicates a good fit of the MDS plot to the proximity matrix data, whereas a large stress value indicates a poor fit and a highly distorted representation of the proximity matrix data (50). For 2 dimensions and 18 sorted items, the stress cutoff at which the data exceeds an acceptable level of distortion is 0.263 (50).
To determine how messages were clustered together in the MDS plot, we used hierarchical cluster analysis to identify cutoffs for clusters at each study visit. We completed the hierarchical cluster analysis with the use of UCINET version 6.614 (47). To interpret the cluster results, we drew on the mothers’ narratives from the qualitative interview transcripts in which they explained why they grouped certain infant feeding messages together, as well as their experiences with and interpretations of the different messages (40). To assign the cluster names, we identified commonalities between the mothers’ descriptive explanations of similarities and differences of the clusters, as well as our own understanding of message differences. [Rather than inferring the cluster names on the basis of descriptive qualitative data, an alternative (and more cost-effective) approach to interpret the clusters names is to ask a group of the same participants or a group of similar participants to explain the names of the clusters.]
We also completed a property fitting (PROFIT) analysis with our message ratings to further understand the axes of the MDS plot. This was done with the use of UCINET version 6.614 (47). PROFIT analyses compute multiple linear regressions using the MDS plot coordinates as the independent variables and aggregated rating data as the dependent variable (47). Before aggregating the rating data, we carried out a consensus analysis to assess agreement across participants and to confirm that the ratings were representative of a shared culture (40). The output of the PROFIT analyses included the following: vector coordinates (representing the direction of rating data on the MDS plot), R2 values to assess the fit of the vector to the MDS plot, and P values to assess the statistical significance of the fit (47, 51). R2 values >0.9 with corresponding P < 0.01 indicate strong fit to the MDS plot (51).
To answer our second question about whether there were differences in the ways mothers cognitively organized messages over time, we used partition analysis to test if the aggregated matrices differed between time points (52). For example, we compared the 18 × 18 aggregated proximity matrix at 1 visit (e.g., pregnancy, visit 1) with the 18 × 18 aggregated proximity matrix of another visit (e.g., 0- to 1-mo postpartum, visit 2). To test for statistical differences, we used partition analysis to permute the observed proximity matrices by individual group (or “visit”) membership (52). That is, we wanted to determine whether random allocation to a group (or “visit”) would show as much difference or similarity as the differences or similarities between our observed groups (52). The output of partition analysis includes correlation coefficients (Pearson's r) between each pair of matrices (e.g., visit 1 matrix compared with visit 2 matrix) and corresponding P values. The P values were calculated by determining the proportion of random correlations that were as small or as large as the observed correlation measure in order to indicate the likelihood of such matrix arrangements occurring by chance (52). We completed the partition analysis with the use of UCINET version 6.614 (47).
Results
Participant characteristics
Thirty mothers were recruited for this study. In our analyses, we did not include the sorting results of 3 mothers who had trouble with the sorting task. These 3 women put each card in a separate pile (i.e., saw no similarities between messages) or put them into piles randomly without explanation as to why the messages were similar. We also did not include the sorting data from mothers who were mixed feeding (i.e., providing food and other liquids with breast milk to their infants aged <6 mo) or who completely stopped breastfeeding. At visit 2 (0- to 1-mo postpartum), we excluded 2 women who were no longer breastfeeding and 1 woman who was practicing mixed feeding. In addition, 2 mothers were lost to follow-up between visit 1 (pregnancy) and visit 2 and 3 mothers were lost to follow-up between visit 2 and visit 3 (3- to 5-mo postpartum). All of the mothers who were lost to follow-up or who were dropped from the analyses because of their breastfeeding practice were exclusively breastfeeding or had an intention to exclusively breastfeed at the preceding study visit. The total sample size for visit 1 was 27 women, for visit 2 was 22 women, and for visit 3 was 19 women. Because the unit of analysis was the shared cultural pattern (and not individual participants’ unique responses), we did not remove participants’ data if they did not complete all 3 interviews.
The majority of the women in our study were exclusively breastfeeding (Table 3). Those who were not exclusively breastfeeding were predominantly breastfeeding (e.g., had provided water but not foods or other liquids to their infants). As determined by nonparametric statistical tests (Fisher's exact test, chi-square test for independence, and Kruskal-Wallis H test), the time-variant characteristics of the mothers included in our analysis (e.g., perceived difficulty of exclusive breastfeeding, perceived breastfeeding support, perceived social support, etc.) were similar across all time periods (Table 3).
TABLE 3.
Characteristics of HIV-infected mothers who completed the pile-sorting interviews at pregnancy, 0- to 1-mo postpartum, and 3- to 5-mo postpartum1
| Pregnancy | 0–1 mo | 3–5 mo | |
|---|---|---|---|
| (n = 27) | (n = 22) | (n = 19) | |
| Age,2 y | 31.1 ± 5.33 | 31.3 ± 5.3 | 31.4 ± 5.4 |
| Children, n | 3.0 ± 1.4 | 3.2 ± 1.4 | 3.1 ± 1.4 |
| Primiparous (yes), n (%) | 4 (14.8) | 2 (9.1) | 2 (10.5) |
| Past EBF experience (yes), n (%) | 5 (18.5) | 5 (22.7) | 5 (26.3) |
| Current practice (EBF),4n (%) | 22 (81.5) | 19 (86.4) | 17 (89.5) |
| Perceived difficulty of EBF, n (%) | |||
| None | 17 (63.0) | 14 (63.6) | 15 (78.9) |
| Somewhat | 6 (22.2) | 7 (31.8) | 3 (15.8) |
| Very | 4 (14.8) | 1 (4.5) | 1 (5.3) |
| Perceived BF support,5n (%) | 18 (72.0) | 16 (72.7) | 14 (73.7) |
| Perceived social support, n (%) | |||
| Low | 9 (33.3) | 4 (18.2) | 2 (10.5) |
| Medium | 17 (63.0) | 16 (72.7) | 17 (89.5) |
| High | 1 (3.7) | 2 (9.1) | 0 (0.0) |
| Maternal depression, n (%) | |||
| None | 11 (40.7) | 12 (54.5) | 11 (57.9) |
| Sometimes | 14 (51.9) | 8 (36.4) | 6 (31.6) |
| Always | 2 (7.4) | 2 (9.1) | 2 (10.5) |
| Duration of HIV infection, n (%) | |||
| <1 y | 3 (11.1) | 3 (13.6) | 3 (15.8) |
| 1-4.9 y | 14 (51.9) | 12 (54.5) | 11 (57.9) |
| 5-9.9 y | 9 (33.3) | 7 (31.8) | 5 (26.3) |
| ≥10 y | 1 (3.7) | 0 (0.0) | 0 (0.0) |
| Fear of HIV disclosure, n (%) | |||
| Low | 2 (7.4) | 2 (9.1) | 2 (10.5) |
| Medium | 16 (59.3) | 12 (54.5) | 9 (47.4) |
| High | 9 (33.3) | 8 (36.4) | 8 (42.1) |
| Number of piles | 6.0 ± 2.8 | 5.0 ± 2.8 | 4.6 ± 2.8 |
BF, breastfeeding; EBF, exclusive breastfeeding.
Missing data from 1 woman during pregnancy; the mean accounts for this.
Mean ± SD (all such values).
Current EBF practice in pregnancy represents what a woman intended to do and not her current practice.
Missing data from 2 women during pregnancy; the percentage value accounts for this.
Cognitive structure of infant feeding messages during pregnancy
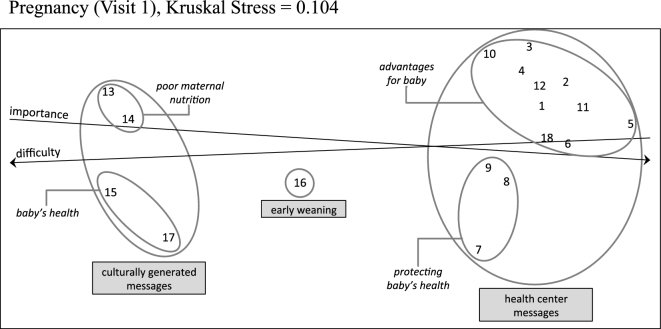
We determined that, before delivery, mothers shared a common cognitive structure to organize infant feeding messages. The MDS analysis of mothers’ cognitive organization of infant feeding messages during pregnancy showed a good fit to the proximity data, with a stress value of 0.104 (cutoff = Kruskal stress < 0.263) (Figure 1). With the use of hierarchical cluster analysis, we identified 3 main clusters. We labeled the clusters, using both etic and emic analyses of the coded interviews, as follows: culturally generated messages (messages 13, 14, 15, and 17), health center messages (messages 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, and 18), and an early weaning message (message 16).
FIGURE 1.
HIV-infected mothers’ cognitive structures about infant feeding messages at pregnancy (as mapped by using MDS, hierarchical cluster, and PROFIT analyses). This figure represents the MDS plot of 27 HIV-infected mothers. The Kruskal stress test indicated a good fit, less than the cutoff of 0.273. Numbers represent individual messages (as described in Table 2) and the circles around the numbers indicate clusters based on hierarchical cluster analysis. From this figure, we can discern that mothers’ perceptions are patterned into 3 main clusters. The distance between numbers (i.e., messages) indicates how closely related they are to one another—the greater the distance, the less similar the message pair, and the smaller the distance, the more similar the message pair. For example, messages 1 and 12 were grouped close together and are more similar to one another than, for example, messages 5 and 15, which are much further apart. The lines in the figure represent the dimensions of the MDS plots based on the PROFIT analysis. The direction of the arrows indicates the increasing value of the dimension. MDS, multidimensional scaling; PROFIT, property fitting.
The dimensions of importance and difficulty showed good fit to the MDS plot, based on the PROFIT analysis (lines in Figure 1). R2 values were 0.91 (P < 0.001) and 0.86 (P < 0.001), respectively. Although the R2 for difficulty was <0.9, we retained it because it approached the 0.9 threshold. We found that the directions of importance and difficulty were inversely related. For instance, the cluster of culturally generated messages (messages 13, 14, 15, and 17; bottom left of Figure 1) were rated as highly difficult and not very important. Conversely, items deemed to be very important were considered to be not difficult to practice.
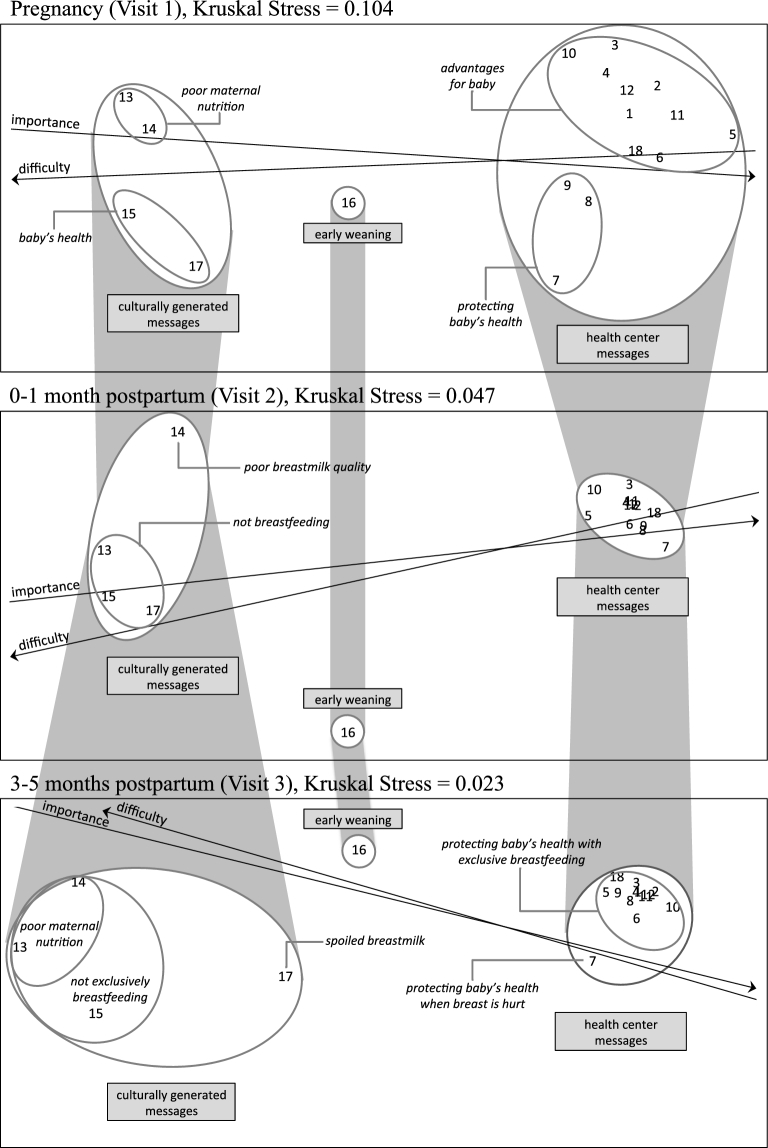
The MDS maps of mothers’ sorted messages at visit 2 and visit 3 also showed a good fit to the proximity data, with stress values <0.10 (Figure 2). The lines representing importance and difficulty also showed a good fit; the R2 values from the PROFIT analyses for importance and difficulty were 0.97 (P < 0.001) and 0.96 (P < 0.001) at 0- to 1-mo postpartum (visit 2) and 0.96 (P < 0.001) and 0.91 (P < 0.001) at 3- to 5-mo postpartum (visit 3), respectively. Over the course of the 3 visits, mothers consistently identified the same 3 main clusters and consistently identified which messages were important and which were difficult.
FIGURE 2.
HIV-infected mothers’ cognitive structures about infant feeding messages over time (as mapped by using MDS, hierarchical cluster, and PROFIT analyses). This figure represents the MDS plot of 27 HIV-infected breastfeeding mothers at pregnancy, 22 HIV-infected breastfeeding mothers at 0- to 1-mo postpartum, and 19 HIV-infected breastfeeding mothers at 3- to 5-mo postpartum. The Kruskal stress indicated a good fit, at <0.273. Numbers represent individual messages (as described in Table 2) and the circles around the numbers indicate clusters based on hierarchical cluster analysis. The lines in the figure represent the dimensions of the MDS plots based on the PROFIT analysis. The direction of the arrows indicates the increasing value of the dimension. The 3 main clusters of messages were maintained over time. The shading in the figure depicts how the proximity or similarity between messages changed over time (i.e., the spread of the clusters). MDS, multidimensional scaling; PROFIT, property fitting.
Changes in cognitive organization of infant feeding messages over time
There were subtle differences in how closely or tightly clustered messages were to one another over time, as shown by the shaded spread of clusters across the 3 visits (Figure 2). During pregnancy, the health center messages were less tightly clustered than at either of the 2 postpartum visits. This was particularly true for the comparison of the pregnancy visit with the 0- to 1-mo postpartum visit. At 0- to 1-mo postpartum, mothers were highly consistent in their grouping of messages, and as a result, messages were more tightly clustered. We hypothesize that this resulted from an increased dichotomization of health center compared with culturally generated infant feeding messages, which may be associated with a heightened sense of duty to and concern for the new infant and successful breastfeeding practice. This idea was expressed by one mother, as follows:
I am [exclusively breastfeeding] because I am a mother. God gave me this baby for me to manage her life. If the baby undergoes a shock tomorrow, I do not want to be the one responsible. When the child comes and says, “Mother, where did I get this thing (HIV)” I do not want to tell my child where I got the virus. I would not want to have any other children again if that happened. —Primiparous mother, 0- to 1-mo postpartum
At 3- to 5-mo postpartum, mothers were more nuanced in their views about how some of the messages related to one another, the perceived importance and difficulty of those messages, and the implications of those messages for the child's health. For instance, although not clustered as tightly as messages 0- to 1-mo postpartum, there were some health center messages that were more tightly clustered at 3- to 5-mo postpartum than they were during pregnancy. Two messages, message 7, which was concerned with injured breasts and cracked nipples, and message 17, which was concerned with spoiled milk, mapped further apart from the other messages in their respective clusters. That is, they were not as conceptually similar to other messages at the 3- to 5-mo postpartum interview as they were in the pregnancy and 0- to 1-mo postpartum interviews. By 3–5 mo postpartum, the PROFIT analyses indicated that message 17 had become more important and less difficult for mothers than their perceptions at the other visits.
Both message 7 and message 17 are concerned with adverse cultural and biomedical outcomes if mothers are not careful with breastfeeding management. These adverse outcomes are shown in the narratives of these mothers:
If your breast is hurt, you need to use just one. You go to the doctor for the doctor to give you some medicine. . . . If your breast is hurt, and the baby pulls at that breast, the baby will get sick [with HIV]. The baby will pull blood, and that is not good.—Multiparous mother, 3- to 5-mo postpartum regarding message 7
[When you have been out for a while], after a bit of time, you can breastfeed. Sometimes I drink water, or if not, I do not breastfeed for a while and then after [I have waited], I do breastfeed. It is important because… if you just come in and you breastfeed your baby, your milk is hot, and it can give the baby diarrhea, it can make the baby sick. —Multiparous mother, 3- to 5-mo postpartum regarding message 17
Despite these time-related differences, the partition analysis, which compared the aggregated proximity matrices over time, showed that the MDS maps of mothers at all 3 visits (during pregnancy, 0- to 1-mo postpartum, and 3- to 5-mo postpartum) were correlated (Table 4). That is, mothers’ sorting patterns, reflecting how they organized infant feeding messages, were similar across the 3 periods, and the time of the visit did not significantly influence how they sorted. These results were observed in the stability of the 3 fundamental clusters of messages in the MDS plots and the mothers’ evaluation of the content of those clusters with respect to difficulty and importance. For example, in our interviews, mothers consistently articulated the importance of exclusive breastfeeding and of health-center messages. One mother stated,
Exclusive breastfeeding is good for him [the baby] because it makes him not sick; it helps him to grow well. They [the health providers at the health center] do not recommend anything else, because other things can give diarrhea. Exclusive breastfeeding is best.—Multiparous mother, pregnancy
TABLE 4.
Correlations of HIV-infected mothers’ aggregate proximity matrices across pregnancy (visit 1), 0- to 1-mo postpartum (visit 2), and 3- to 5-mo postpartum (visit 3)
| Pearson's r | P | |||
|---|---|---|---|---|
| Observed correlation | Average permutation correlation | Correlation ≥ observed | Correlation ≤ observed | |
| Visit 1 vs. Visit 2 | 0.880 | 0.889 | 0.677 | 0.324 |
| Visit 1 vs. Visit 3 | 0.867 | 0.905 | 0.936 | 0.065 |
| Visit 2 vs. Visit 3 | 0.951 | 0.937 | 0.231 | 0.769 |
One message, message 16, stood on its own at each time period. This message was related to weaning the infant completely off the breast at 6 mo. This message was recommended in earlier WHO guidelines for HIV-infected women but is no longer recommended. Nonetheless, it is still part of the feeding-related messages that women hear, although where they hear it (health centers, their past experience, or the community) is not clear. In the respondents’ sorting, this message was consistently placed in a separate pile and not seen as related to the other messages. In addition, many mothers expressed discomfort about continuing to breastfeed after the introduction of complementary foods, even though, as described in the quote below, that is what they felt they would have to do:
They say the baby does not have [HIV]. If it were possible, I would completely wean the baby from the breast. But I do not have any other possibilities. When the baby is ready to eat, he is familiar with the breast and you have to make sure you have something to give him to drink. I might not be able, so I will continue to breastfeed. But I am not comfortable giving food and breast together.—Multiparous mother, 3- to 5-mo postpartum
Discussion
This study shows the insights that emerge with the use of the cognitive mapping technique of pile sorting. It provides a systematic framework to examine shared perceptions and cognitive classifications and can be used as a tool for researchers to measure and evaluate cognitive processes in nutrition interventions, including changes over time. Our research also shows the use of quantitative methods to interpret emic data and shows that ethnography is a mixed-method approach that is not synonymous with narrative analysis alone (9). Pile sorting is one method of several that can be used to identify emerging patterns and to quantify the degree of shared culture and consensus among a group of study participants. For researchers concerned with quantification, the approach provides a means to quantify qualitative data with a small sample of respondents. Software programs, such as UCINET, ANTHROPAC, and R-CMap, provide easy-to-use platforms to analyze pile-sorting data and can be used to produce proximity matrices for MDS and cluster analyses of items (and individuals).
In this study, our analyses identified the existence of a shared “culture” among HIV-infected, breastfeeding mothers. Our results indicate that mothers systematically organized infant feeding messages, and this organization can be characterized as a shared cognitive structure. This level of sharing was not a foregone conclusion before the study showed it. Intracultural diversity is often revealed in cognitive mapping studies (53). Proximity matrices produced by the pile-sorting method can identify individuals or groups of individuals who do not share the same cognitive structure. For breastfeeding, in which the complex organization of ideas involves both traditional and new, “foreign” cultural elements, one might have predicted a much lower level of shared cognitive organization than that which was found in our study.
The study also shows the value of using nonparametric statistics to compare the cultural patterns of different groups—in this case, comparisons of the effects of time. Although we used the UCINET software program to complete the partition analysis, R-CMap is also developing functionality to evaluate and statistically compare pile-sorting results with one another. Care providers and program planners can use these methods to explore how different concepts are classified and cognitively organized by different groups of people they are working with, and how those change with participation in interventions or experience with practice of nutrition-related behaviors.
Our analysis documented both continuities and changes over time in how mothers related individual messages to one another. We found that mothers’ progressive experiences with breastfeeding did not change the basic clustering of infant feeding messages from pregnancy to 5-mo postpartum. The visual representation showed 2 distinct clusters: 1) messages whose origins are in traditional culture, as experienced by women as members of their larger community, and 2) messages whose origins lie in the international biomedical culture, as conveyed by the health system. Community-generated cultural messages appeared to be less important for mothers (as determined by the PROFIT analysis). The finding of the 2 distinct clusters raises the question about whether HIV-infected mothers experience a conflict between the cultural norms of their community and the biomedical recommendations they receive from the health center, which they had indicated as being more important and less difficult.
The narrative data from this study elucidated the distinction between different sources of information and suggest that women placed a heavy reliance on their health care providers with respect to recommendations about infant feeding. This reliance might have been magnified by mothers’ fears of adverse outcomes for their infants if they do not follow health center guidelines, specifically about vertical transmission of HIV. This result aligns with other studies in which HIV-infected women discuss the importance of “informed” messages from the biomedical community about exclusive breastfeeding and in which they express difficulty with navigating constant pressures to not breastfeed exclusively (31, 54–59). Mothers are often responsible for translating the advice they receive from the clinic to their families and communities. For instance, in Malawi, mothers were responsible for attending clinic visits and receiving child feeding advice from health care providers (57). They were then responsible for sharing that infant feeding advice with other caregivers in the family and navigating conflicts between that advice and advice from other sources (57). Our findings are also consonant with findings from other studies about breastfeeding in the context of HIV concerning mothers’ general fear of transmitting the virus to their infants through breast milk (54, 60) and after 6 mo with complementary feeding (56). In sum, this study provides further evidence about the disconnect between culturally generated messages and health center messages.
Our results also showed that at 0- to 1-mo postpartum, mothers’ cognitive organization of infant feeding messages is much more closely clustered than it is before giving birth or after more months of experience. We suggest that one explanation for this lies in the intensity of the breastfeeding experience in the immediate, postdelivery period. From the literature, we know that women often experience problems with breastfeeding in the first month postpartum (61–63) and find that breastfeeding is more exhausting and time-intensive than they had anticipated (27, 64, 65). The reality of breastfeeding often does not align with the idealistic recommendations mothers receive (27). In the first month, mothers are relearning and sifting through information that they received during pregnancy and are trying to connect it to their experiences with their own bodies and infants in a practical way (64). The tighter clustering of messages in the first month postpartum might reflect this cognitive stress. It is often not until a few months postpartum that mothers develop a “routine” (66). In our study, by 3- to 5-mo postpartum, mothers’ MDS plot became somewhat more differentiated with respect to their perceptions of similarity, as well as their perceptions of importance and difficulty. Attention to this feature has implications for breastfeeding education. It suggests the need to develop patient-centered counseling strategies that respond to changes in mothers’ cognitive patterns by better tailoring the content and better targeting the timing of recommendations about infant feeding.
Our findings have several limitations. First, one of the criteria for participating in the study was breastfeeding practice, and we therefore only documented the cognitive structure of mothers who were exclusively breastfeeding or predominantly breastfeeding. As such, our results are specific to HIV-infected, breastfeeding, health-seeking mothers at GHESKIO, and their generalizability should be viewed with caution. These mothers are likely to be more influenced by and responsive to infant feeding messages from the health center. Mothers in Haiti who are not breastfeeding (or who are mixed feeding) or who do not seek antenatal care may have different cultural views. Second, we did not examine the connection between mothers’ cognitions and their breastfeeding practices because the purpose of the study was to explore changes in breastfeeding mothers’ cognitive structure over time. A larger, more heterogeneous sample would allow us to explore differences in cognitive structure for different infant feeding practices, as well as for other aspects that might result in heterogeneity of the sample (e.g., history of care, etc.). Third, pile sorting is limited in its ability to answer questions about directionality. The sorting results alone can indicate that the cognitive structure changed, but they do not provide reasons why (e.g., as a result of breastfeeding practice, recommendations from the health center, or other experiential factors). Although narratives from respondents can provide useful insights to interpret findings (40), additional follow-up and inquiry are required to strengthen interpretations. Finally, we note that our findings are limited to the messages we asked women to sort. However, we believe that these were representative of common and salient infant feeding messages in the community.
Despite the limitations, the study highlights the value of empirically investigating changes in mothers’ cognitive processes about infant feeding messages over time and shows that changes can occur even over a relatively short period of time. This research fills gaps in the knowledge about how women perceive and prioritize different recommendations about infant feeding. The proximity of different messages to one another also has implications for how practitioners might tailor messages. It can inform practitioners about when they might best target their interventions or reorient their counseling support. In the future, investigators may want to apply cognitive mapping techniques to explore the cognitive processes of other groups of women in Haiti, including women who are not HIV-infected or not practicing exclusive breastfeeding. Going beyond the Haitian context, we hope the approach taken in this research will lead to insights about breastfeeding in other countries and cultures.
In conclusion, this study shows the use of pile sorting to investigate cognitive processes with the use of emic, quantitative methods that identify emerging patterns in a group of people. The identification of mothers’ cognitive structures and the recognition of how they change over the course of their breastfeeding experience contribute to continuing efforts to develop patient-centered infant feeding counseling to support recommended infant feeding behaviors. It highlights how the content and timing of recommendations matter, because their relevance changes with lived experience. Beyond the realm of infant feeding, our study suggests the utility of using transdisciplinary methods to capture the dynamism of cognitive processes resulting from experience, practice, or exposure to public health interventions.
Acknowledgments
We thank the GHESKIO team (Edwidge Byron, Ghislaine Saint Louis, Ruthza Mondesir, Evelyne Pierre Solon, Adeline Bernard, Suzette Fleury, Sandra Dorceus, and Vanessa Rivera) for their collaboration in making this study possible. We also thank Barbara Strupp for her feedback on the design of the study, Roseanne Schuster and Jean-Pierre Habicht for their comments on this manuscript, and Erika Mudrak from the Cornell Statistical Consulting Unit and Steve Borgatti from University of Kentucky for their guidance on the statistical analyses.
The authors’ responsibilities were as follows—ELF, GHP, KMR, and DLP: were involved in the conception and design of the research; ELF, MGD, VAR, and JWP: were involved in the acquisition of the data; ELF, GHP, HB, KMR, SLY, and DLP: were responsible for the analysis and interpretation of the data; ELF: wrote the manuscript and had primary responsibility for the final content; GHP, HB, KMR, SLY, MGD, VAR, JWP, and DLP: were involved in providing detailed comments and revising the manuscript for important intellectual content; and all authors: read and approved the final manuscript.
Notes
Supported by the Cornell Human Ecology Alumni Association, the Mario Einaudi Center for International Studies, the Cornell Graduate School, the First Presbyterian Church of Ithaca, and the American Association of University Women. SLY was supported by K01 MH098902 from the National Institute of Mental Health.
Author disclosures: ELF, GHP, HB, KMR, SLY, MGD, VAR, JWP, and DLP, no conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the NIH.
Abbreviations used:
- GHESKIO
Groupe Haitien d'Etude du Sarcome de Kaposi et des Infections Opportunistes
- MDS
multidimensional scaling
- PROFIT
property fitting
References
- 1. Pelletier DL, Porter CM, Aarons GA, Wuehler SE, Neufeld LM. Expanding the frontiers of population nutrition research: new questions, new methods, and new approaches. Adv Nutr 2013;4(1):92–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tumilowicz A, Neufeld LM, Pelto GH. Using ethnography in implementation research to improve nutrition interventions in populations. Matern Child Nutr 2015;11(Suppl 3):55–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leeming D, Marshall J, Locke A. Understanding process and context in breastfeeding support interventions: the potential of qualitative research. Matern Child Nutr 2017;13(4):e12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Larsen JS, Hall EO, Aagaard H. Shattered expectations: When mothers' confidence in breastfeeding is undermined—a metasynthesis. Scand J Caring Sci 2008;22(4):653–61. [DOI] [PubMed] [Google Scholar]
- 5. Monterrosa EC, Pelto GH, Frongillo EA, Rasmussen KM. Constructing maternal knowledge frameworks: how mothers conceptualize complementary feeding. Appetite 2012;59(2):377–84. [DOI] [PubMed] [Google Scholar]
- 6. Rohner RP. Toward a conception of culture for cross-cultural psychology. J Cross Cult Psychol 1984;15(2):111–38. [Google Scholar]
- 7. D'Andrade RG. The cultural part of cognition. Cogn Sci 1981;5(3):179–95. [Google Scholar]
- 8. Gravlee CC, Maxwell CR, Jacobsohn A, Bernard HR. Mode effects in cultural domain analysis: comparing pile sort data collected via internet versus face-to-face interviews. Int J Soc Res Methodol 2017:1–12. [Google Scholar]
- 9. Young SL, Pelto GH. Evaluative ethnography for maternal and child nutrition interventions. In: Dykes F, Flacking R, editors. Ethnography research in maternal and child health, 1st ed London: Routledge; 2015. p. 157–78. [Google Scholar]
- 10. Maitra S, Schensul SL. Reflecting diversity and complexity in marital sexual relationships in a low-income community in Mumbai. Cult Health Sex 2002;4(2):133–51. [Google Scholar]
- 11. Ross JL, Laston SL, Pelto PJ, Muna L. Exploring explanatory models of women's reproductive health in rural Bangladesh. Cult Health Sex 2002;4(2):173–90. [Google Scholar]
- 12. Weeks MR, Abbott M, Liao S, Yu W, He B, Zhou Y et al. Opportunities for woman-initiated HIV prevention methods among female sex workers in southern China. J Sex Res 2007;44(2):190–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santos-Acuin CC, Pelto PJ. Exploration of mother's activities: a multidimensional scale. Field Methods 1992;4(2):4–5. [Google Scholar]
- 14. Corral-Terrazas M, Martinez H, Flores-Huerta S, Duque LM, Turnbull B, Levario-Carrillo M. [Beliefs and knowledge of a group of doctors about the nutritional management of the child with acute diarrhea.] Salud Publica Mex 2002;44(4):303–14.(in Spanish). [PubMed] [Google Scholar]
- 15. Rodriguez-Oliveros MG, Bisogni CA, Frongillo EA. Knowledge about food classification systems and value attributes provides insight for understanding complementary food choices in Mexican working mothers. Appetite 2014;83:144–52. [DOI] [PubMed] [Google Scholar]
- 16. Kodish S, Aburto N, Hambayi MN, Kennedy C, Gittelsohn J. Identifying the sociocultural barriers and facilitating factors to nutrition-related behavior change: formative research for a stunting prevention program in Ntchisi, Malawi. Food Nutr Bull 2015;36(2):138–53. [DOI] [PubMed] [Google Scholar]
- 17. Thairu LN. Ethnography of infant feeding in sub-Saharan Africa: case studies in the context of HIV/AIDS and newborn care. Ithaca (NH): Cornell University; 2006. [Google Scholar]
- 18. Pelto PJ. Applied ethnography: guidelines for field research. Walnut Creek (CA): Left Coast Press; 2013. [Google Scholar]
- 19. Pelto GH, Pelto PJ, Messer E, editors. Research methods in nutritional anthropology. Tokyo: United Nations University; 1989. [Google Scholar]
- 20. Luborsky MR, Rubinstein RL. Sampling in qualitative research: rationale, issues, and methods. Res Aging 1995;17(1):89–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pelto PJ, Pelto GH. Anthropological research: the structure of inquiry. 2nd ed Cambridge (United Kingdom): Cambridge University Press; 1987. [Google Scholar]
- 22. Desclaux A, Alfieri C. Counseling and choosing between infant-feeding options: overall limits and local interpretations by health care providers and women living with HIV in resource-poor countries (Burkina Faso, Cambodia, Cameroon). Soc Sci Med 2009;69(6):821–9. [DOI] [PubMed] [Google Scholar]
- 23. McInnes RJ, Chambers JA. Supporting breastfeeding mothers: qualitative synthesis. J Adv Nurs 2008;62(4):407–27. [DOI] [PubMed] [Google Scholar]
- 24. Tuthill E, McGrath J, Young S. Commonalities and differences in infant feeding attitudes and practices in the context of HIV in sub-Saharan Africa: a metasynthesis. AIDS Care 2014;26(2):214–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. de Paoli M Manongi R, Klepp K. Counsellors' perspectives on antenatal HIV testing and infant feeding dilemmas facing women with HIV in northern Tanzania. Reprod Health Matters 2002;10:144–56. [DOI] [PubMed] [Google Scholar]
- 26. Lazarus R, Struthers H, Violari A. Promoting safe infant feeding practices—the importance of structural, social and contextual factors in southern Africa. J Int AIDS Soc 2013; 16:18037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoddinott P, Craig LC, Britten J, McInnes RM. A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open 2012;2(2):e000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pelto PJ, Pelto GH. Intra-cultural diversiy: some theoretical issues. Am Ethnol 1975;2(1):1–18. [Google Scholar]
- 29. Handwerker WP. The construct validity of cultures: cultural diversity, cultural theory, and a method for ethnography. Am Anthropol 2002;104(1):106–22. [Google Scholar]
- 30. Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. Effect of the HIV epidemic on infant feeding in South Africa: “When they see me coming with the tins they laugh at me”. Bull World Health Organ 2006;84:90–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Levy JM, Webb AL, Sellen DW. “On our own, we can't manage”: experiences with infant feeding recommendations among Malawian mothers living with HIV. Int Breastfeed J 2010;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Maman S, Cathcart R, Burkhardt G, Omba S, Thompson D, Behets F. The infant feeding choices and experiences of women living with HIV in Kinshasa, Democratic Republic of Congo. AIDS Care 2011;24(2):259–65. [DOI] [PubMed] [Google Scholar]
- 33. Young SL, Mbuya MNN, Chantry CJ, Geubbels EP, Israel-Ballard K, Cohan D Vosti SA Latham MC. Current knowledge and future research on infant feeding in the conte xt of HIV: basic, clinical, behavioral, and programmatic perspectives. Adv Nutr 2011;2(3):225–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cayemittes M, Busangu MF, Bizimana JD, Barrère B, Sévère B, Cayemittes V Charles E. Survey of Mortality, Morbidity and Service Utilization [Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-V)]. Port-au-Prince (Haiti): Ministère de la Santé Publique et de la Population; Institut Haïtien de l'Enfance (IHE), Inner City Fund (ICF) International, and Monitoring and Evaluation to Assess and Use Results Demographic and Health Surveys (MEASURE DHS); 2013. (in French). [Google Scholar]
- 35. Heidkamp RA, Stoltzfus RJ, Fitzgerald DW, Pape JW. Growth in late infancy among HIV-exposed children in urban Haiti is associated with participation in a clinic-based infant feeding support intervention. J Nutr 2012;142(4):774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ministère de la Santé Publique et de la Population (MSPP), Unité de Côntrole et de Coordination du Programme National de Lutte Contre le VIH/SIDA. National guidelines for the care and treatment of HIV-exposed and HIV-infected infants, children and adolescents (Directives nationales pour les soins et le traitement des nourrissons, des enfants et des adolescents exposés au VIH et infectés par le virus). Edition révisée, 2013. Port-au-Prince (Haiti): Ministère de la Santé Publique et de la Population, République d'Haïti; 2013 (in French).
- 37. Weller SC. Cultural consensus theory: applications and frequently asked questions. Field Methods 2007;19(4):339–68. [Google Scholar]
- 38. Romney AK, Weller SC, Batchelder WH. Culture as consensus: a theory of culture and informant accuracy. Am Anthropol 1986;88(2):313–38. [Google Scholar]
- 39. Borgatti SP, Halgin DS. Elicitation techniques for cultural domain analysis. In: Schensul JJ, LeCompte MD, editors. Specialized ethnographic methods: a mixed methods approach. Ethnographer's Toolkit 4. Lanham (MD): AltaMira Press; 2013. p. 80–116. [Google Scholar]
- 40. Weller SC, Romney AK. Systematic data collection: qualitative research methods. Vol. 10 Newbury Park (CA): Sage Publications; 1988. [Google Scholar]
- 41. Fox EL, Pelto GH, Rasmussen KM, Debrosse MG, Rouzier VA, Pape JW, Pelletier DL. Who knows what: an exploration of the infant feeding message environment and intracultural differences in Port-au-Prince, Haiti. Matern Child Nutr 2017;14(2):e12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alvarez MD, Murray GF. Socialization for scarcity: child feeding beliefs and practices in a Haitian village. Port-au-Prince (Haiti): USAID/Haiti; 1981. [Google Scholar]
- 43. Glaser B, Strauss A. The discovery of grounded theory strategies for qualitative research. New Brunswick (NJ): Aldine Transaction; 1967. [Google Scholar]
- 44. QSR. NVivo qualitative data analysis software. Version 10. Melbourne (Australia): QSR International Pty. Ltd.; 2012. [Google Scholar]
- 45. Trochim WM, Kane M. Concept mapping analysis. In: Kane M, Trochim WM, editors. Concept mapping for planning and evaluation. Thousand Oaks (CA): Sage Publications; 2007. p. 87–111. [Google Scholar]
- 46. Kruskal JB, Wish M. Basic concepts of multidimensional scaling. In: Uslaner E, editor. Multidimensional scaling (Quantitative applications in the social sciences, series 11). Beverly Hills (CA): Sage Pu; blications; 1978. p. 7–28. [Google Scholar]
- 47. Borgatti SP, Everett MG, Freeman LC. UCINET for Windows: Software for Social Network Analysis. 6.6 ed. Harvard (MA): Analytic Technologies; 2002. [Google Scholar]
- 48. Borgatti S. ANTHROPAC 4.0. Natick (MA): Analytic Technologies; 1996. [Google Scholar]
- 49. Bar H, Mentch L. R-CMap—an open-source software for concept mapping. Eval Program Plan 2017;60(Suppl C):284–92. [DOI] [PubMed] [Google Scholar]
- 50. Sturrock K, Rocha J. A multidimensional scaling stress evaluation table. Field Methods 2000;12(1):49–60. [Google Scholar]
- 51. Weller S. Cross-cultural concepts of illness: variations and validation. Am Anthropol 1984;86(2):341–51. [Google Scholar]
- 52. Borgatti S. A statistical method for comparing aggregate data across a priori groups. Field Methods 2002;14(1):88–107. [Google Scholar]
- 53. Garro L. Intracultural variation in folk medical knowledge: a comparison between curers and noncurers. Am Anthropol 1986;88(2):351–70. [Google Scholar]
- 54. Cames C, Saher A, Ayassou KA, Cournil A, Meda N, Simondon KB. Acceptability and feasibility of infant-feeding options: experiences of HIV-infected mothers in the World Health Organization Kesho Bora Mother-to-Child Transmission Prevention (PMTCT) trial in Burkina Faso. Matern Child Nutr 2010;6(3):253–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mataya R, Mathanga D, Chinkhumba J, Chibwana A, Chikaphupha K, Cardiello J. A qualitative study exploring attitudes and perceptions of HIV positive women who stopped breastfeeding at six months to prevent transmission of HIV to their children. Malawi Med J 2013;25(1):15–9. [PMC free article] [PubMed] [Google Scholar]
- 56. Matovu J, Onyango-Makumbi C, Namuli P, Tanga E, Kagawa M, Nalwadda G, Motevalli M, Semitala FC, O´ Gara ET, Fowler MG. WHO 2010 infant feeding guidelines in resource-limited settings: attitudes of human immunodeficiency virus-infected women and other role players in Kampala, Uganda. South Afr J Clin Nutr 2014;27(2):63–8. [Google Scholar]
- 57. Chintalapudi N, Hamela G, Mofolo I, Maman S, Hosseinipour MC, Hoffman IF, Flax VL. Infant and young child feeding decision making and practices: Malawian mothers’ and fathers’ roles in the context of HIV. J Hum Lact 2018;34(1):68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Flax VL, Yourkavitch J, Okello ES, Kadzandira J, Katahoire AR, Munthali AC. “If my husband leaves me, I will go home and suffer, so better cling to him and hide this thing”: the influence of gender on Option B+ prevention of mother-to-child transmission participation in Malawi and Uganda. PLoS One 2017;12(6):e0178298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kim MH, Zhou A, Mazenga A, Ahmed S, Markham C, Zomba G, Simon K, Kazembe PN, Abrams EJ. Why did I stop? Barriers and facilitators to uptake and adherence to ART in Option B+ HIV care in Lilongwe, Malawi. PLoS One 2016;11(2):e0149527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tuthill EL, Chan J, Butler LM. Challenges faced by healthcare providers offering infant feeding counseling to HIV-positive women in sub-Saharan Africa: a review of current research. AIDS Care 2015;27(1):17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mogan J. A study of mothers' breastfeeding concerns. Birth 1986;13(2):104–8. [DOI] [PubMed] [Google Scholar]
- 62. McQueen A, Mander R. Tiredness and fatigue in the postnatal period. J Adv Nurs 2003;42(5):463–9. [DOI] [PubMed] [Google Scholar]
- 63. Osman H, Chaaya M, El Zein L, Naassan G, Wick L. What do first-time mothers worry about? A study of usage patterns and content of calls made to a postpartum support telephone hotline. BMC Public Health 2010;10:611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Forster DA, McLachlan HL, Rayner J, Yelland J, Gold L, Rayner S. The early postnatal period: exploring women's views, expectations and experiences of care using focus groups in Victoria, Australia. BMC Pregnancy Childbirth 2008;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kafulafula UK, Hutchinson MK, Gennaro S, Guttmacher S, Chirwa E. Practice environment related barriers to exclusive breastfeeding among HIV-positive mothers in Blantyre, Malawi. Health 2013;5(9):1412–21. [Google Scholar]
- 66. Froehlich J, Donovan A, Ravlin E, Fortier A, North J, Bloch MK. Daily routines of breastfeeding mothers. Work 2015;50(3):433–42. [DOI] [PubMed] [Google Scholar]