Abstract
The progresses made in minimally invasive surgery, make it not only possible to perform isolated cholecystectomy, but also to provide a totally laparoscopic treatment of common bile duct lithiasis. In this approach, the use of choledochoscopy is indispensable for diagnostic and therapeutic success. This study describes the use of a disposable endoscope for choledochoscopy in the laparoscopic treatment of choledocholithiasis. We have analyzed the use of the Ambu® aScope 3™ disposable endoscope, normally used for bronchoscopy, in nine consecutive patients needing choledochoscopy in our Hospital. The patient average age was 78 years. Total clearance of the bile duct was obtained in seven patients. Bile duct vacuity was not obtained in two patients, but this is not attributed to equipment failure. There was one case of hemoperitoneum not related to equipment usage. This device is easy to use and looks promising for choledochoscopy in laparoscopic treatment of coledocholithiasis.
INTRODUCTION
The presence of gallstones in the main bile duct occurs in 10–15% of patients submitted to symptomatic vesicular lithiasis surgery [1]. When detected, by means of intraoperative cholangiography, or preoperative imaging exams, their removal should be done whenever possible in order to avoid complications such as obstructive jaundice, acute pancreatitis, suppurative cholangitis or hepatic abscesses. With the technological advances in laparoscopic surgery, less invasive methods for the treatment of main bile duct lithiasis have been developed, in addition to cholecystectomy as an isolated act.
The possible options for gallstone removal are the exploration of the choledochal duct by simultaneous laparoscopy and cholecystectomy, or two-stage technique treatment with ERCP before or after surgery. When compared, there are no differences between them, as far as the success rate in bile duct clearance, morbidity or mortality is concerned [2, 3]. However, the cumulative hospital stay is shorter with one-stage laparoscopic treatment [3].
Total laparoscopic treatment has two advantages, as far as the ERCP is concerned; it maintains the Oddi sphincter intact and avoids other invasive procedures.
In our department, cholecystectomy and laparoscopic exploration of the bile duct is the treatment of choice for choledocholithiasis with associated lithiasis of the main bile duct. For patients who already have undergone cholecystectomy, or those who are not apt for surgery, the reference approach is ERCP.
When gallstones in the bile duct are found during intraoperative cholangiography, the transcystic approach is preferential, because it is less invasive and presents fewer biliary complications. We reserve choledochotomy for cases where the cystic duct is not permeable, long, with insertion on the left side of the choledochal duct, with gallstones larger than 10 mm, in greater number than 5, or located above the joint of the cystic choledochal ducts. Using choledochoscopy is paramount and crucial for the diagnostic and therapeutic success of this approach.
MATERIAL AND METHODS
We present a brief note about the disposable endoscope used on the choledochoscopy for laparoscopic treatment of bile duct lithiasis.
Between May and November 2017, we used Ambu’s aScope 3™ on nine consecutive patients, who needed to undergo choledochoscopy. This equipment is a flexible and disposable endoscope, designed for bronchofibroscopy and tracheal intubation. We used the large version of the device, which is 60 cm long, 5.8 mm in diameter, which fits into a dilated choledochus, and a work channel 2.8 mm in diameter, that allows the passage of Dormia baskets for bile duct instrumentation. The LED light source is located at the tip of the device, which has a flexing capacity of 140° upwards and 110° downwards. The image is reproduced on an 8.5′, TFT/LCD monitor, with a 800 × 480 pixel resolution.
All patients underwent laparoscopy, and intraoperative cholangiography which showed signs of gallstones in the bile duct. Four conventional ports were used for the cholecystectomy, and another port, the subcostal right, for the introduction of the choledochoscope. In all cases, the choledochoscopy was performed by longitudinal choledochotomy, due to the cystic duct diameter, or due to the above-mentioned criteria.
RESULTS
We used Ambu’s aScope 3™ to perform choledochoscopies on nine patients, where gallstones were removed using Dormia baskets through the device’s work channel. Four patients were females and five males. The average age was 78 years (35–87). Four patients were classified as ASA III, and five as ASA II. A total clearance of the bile duct was obtained on seven patients. On the remaining two, the existence of multiple gallstones, fragments of gallstones and debris, prevented obtaining vacuity of the bile duct. This cannot be attributed to equipment malfunction. For the same reason, these two patients underwent a choledochoduodenostomy, which is indicated in these situations. Five patients had primary closing of the choledochotomy and, in two, closing was made through placement of a Kehr tube.
There was one occurrence of hemoperitoneum, which lead to surgical reintervention. This complication was not related to the equipment used.
DISCUSSION
Choledochoscopy, either by transcystic way or direct way through choledochotomy, is a fundamental and indispensable resource for the resolution of most bile duct lithiasis cases.
Using reusable videoendoscopes for that purpose always raises the question of the ergonomy of use, and easy image capture. In that respect, the Ambu® aScope 3™ clearly exceeded the challenge. The image quality is also comparable to that of conventional choledochoscopes (Figs 1 and 2).
Figure 1:
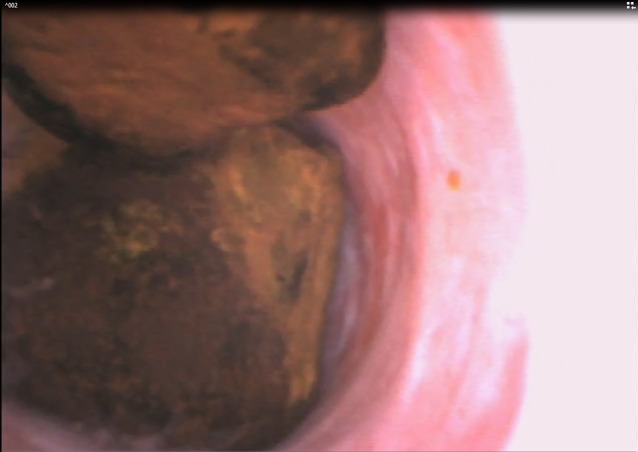
Choledochoscopic view of bile duct stones.
Figure 2:

Insertion of Dormia basket for stone retrieval.
The effectiveness in obtaining bile duct clearance was shown in these nine cases and in the results of other papers already published [4].
On the other hand, using these endoscopes has other advantages: no high costs of repair, no decontamination costs and no cross infection [5]. Using these devices could mean a financial benefit and a valid alternative to flexible, reusable choledochoscopes, which are more expensive and require exacting maintenance.
The results, as far as complications and therapeutic effectiveness are concerned, are comparable to those of interventions where conventional choledochoscopes were used, although a larger number of procedures need to be analysed.
CONCLUSIONS
Although additional research is required, thus far, the disposable Ambu® aScope 3™ endoscope proved to be easy to use and shows promise while performing choledochoscopy for treatment of coledocholithiasis via laparoscopic approach. Our group will continue to study the use of this device in order to further confirm its potential.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
There is no financial or non-financial support to declare.
REFERENCES
- 1. Verbesey J, Birkett D. Common bile duct exploration for choledocholithiasis. Surg Clin North Am 2008;88:1315–28. [DOI] [PubMed] [Google Scholar]
- 2. Lu J. Two-stage vs. single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol 2012;18:3156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kenny R, Richardson J, McGlone E, Reddy M, Khan O. Laparoscopic common bile duct exploration versus pre or post-operative ERCP for common bile duct stones in patients undergoing cholecystectomy: is there any difference? Int J Surg 2014;12:989–93. [DOI] [PubMed] [Google Scholar]
- 4. Aawsaj Y, Light D, Brown J, Horgan L. Use of the Ambu® aScope 2TM in laparoscopic common bile duct exploration. Surg Endosc 2016;30:5153–5. [DOI] [PubMed] [Google Scholar]
- 5. Perbet S, Blanquet M, Mourgues C, Delmas J, Bertran S, Longère B, et al. Cost analysis of single-use (Ambu® aScope™) and reusable bronchoscopes in the ICU. Ann Intensive Care 2017;7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]


