Abstract
BEZOARS are retained concretions of indigestible foreign material that accumulate and conglomerate in the gastrointestinal tract, most commonly in the stomach. Prevalence of bezoar is 0.4%. Bezoars are classified in four categories: phytobezoars; trichobezoars; pharmacobezoars; lactobezoars. A 58-year-old man admitted with complains of pain abdomen and recurrent vomiting since last 3 months. Upper GI endoscopic biopsy reported—chronic gastritis with very occasional non-caseating epitheloid granuloma in lamina propria, no evidence of neoplasia? Crohn’s disease. Keeping Crohn’s as diagnosis patient was given mesalamine 400 mg tid by gastrophyscian. But patient did not respond so the patient was advised surgical management. Repeat UGI endoscopy revealed multiple pills (mesalamine) in the stomach with gastric outlet obstruction (GOO). Around 40 pills were extracted with the help of flower basket, and then patient develope GOO and underwent Laparoscopic gastrojejunostomy and truncal vagotomy.
INTRODUCTION
BEZOARS are retained concretions of indigestible foreign material that accumulate and conglomerate in the gastrointestinal tract, most commonly in the stomach. The term bezoar is derived from the Arabic ‘badzehr’ or from the Persian ‘padzahr’ both means ‘to expel potion’ or antidote. Prevalence of bezoar is 0.4%. Bezoars are classified in four categories: phytobezoars (vegetable matter); trichobezoars (hair balls); pharmacobezoars (tablets or semi-liquid masses drugs); lactobezoars (which are composed of milk protein) miscellaneous material (clay, stone, etc.) [1].
It may lead to intraluminal obstruction. If endoscopic management (dissolution therapy) fails, surgical intervention is needed and now it can be managed by the laparoscopy approach.
CASE REPORT
A 58-year-old man admitted with complains of pain abdomen and recurrent vomiting since last 3 months. USG abdomen was normal. CECT abdomen reported a short segment (4.9 cm) of marked circumferential wall thickening (20 mm) involving pylorus of stomach. It was causing marked luminal narrowing with mild dilatation of stomach? Mitotic? Inflammatory, multiple enlarged lymph nodes are noted in mesentery and pre–para aortic region.
Upper GI endoscopic biopsy reported—chronic gastritis with very occasional non-caseating epitheloid granuloma in lamina propria, no evidence of neoplasia? Crohn’s disease.
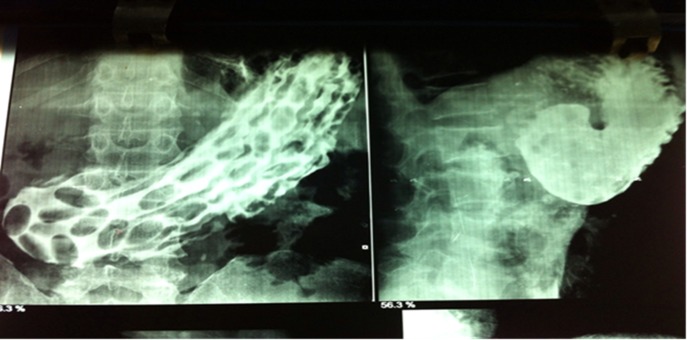
Keeping Crohn’s as diagnosis patient was given mesalamine 400 mg tid by gastrophyscian. But patient didn’t respond so the Patient was advised surgical management. Barium meal follow through (BMFT) (Fig. 1), reported multiple hyperplastic polyps with gastric outlet obstruction (GOO). Repeat UGI endoscopy revealed multiple pills (mesalamine) in the stomach with GOO (Fig. 2). Around 40 pills were extracted with the help of flower basket, and then patient underwent laparoscopic management of GOO. Surgical procedure done was laparoscopic gastrojejunostomy (Fig. 3). Patient also underwent left and right truncal vagotomy (Fig. 4).
Figure 1:
BMFT Film, reported multiple hyperplastic polyps with GOO.
Figure 2:
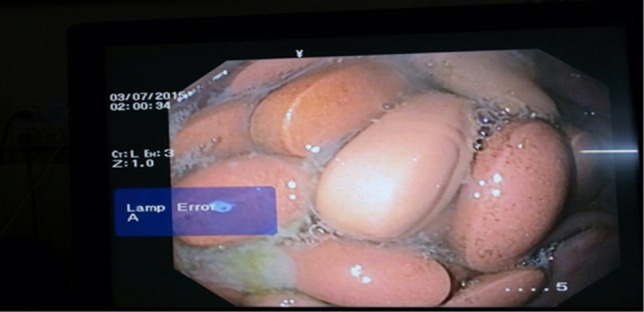
UGI endoscopy showing multiple pills.
Figure 3:

Gastrojejunostomy by endostaplers.
Figure 4:
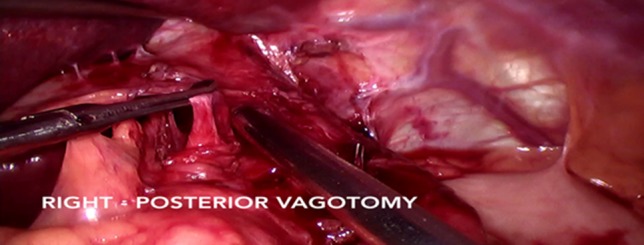
Left and right truncal vagotomy.
DISCUSSION
The majority of bezoars are located in the stomach. Four different types of bezoars:
Phytobezoar—composed of non-digestible food particles found in fruit and vegetables
Trichobezoar—hair bezoar
Lactobezoar—compact mass of undigested milk concretions
Pharmacobezoar—conglomeration of medications
Others
Trichophytobezoar—mixture of hair, fruit, and vegetable fibres
Diospyrobezoar—persimmons
Dead ascaris—worm bezoars [1]
Risk factors for bezoar are cystic fibrosis, intrahepatic cholestasis, diabetes, hypothyroidism and renal failure. Edentulous patients with poor mastication of food and patients with psychiatric illness. Cases of gastroparesis with decreased or absent gastric peristalsis, surgical resection/bypass of the gastric antrum and body, or undergoing a bariatric surgery are particularly susceptible to the development of bezoars [2, 3].
Medications reported to cause bezoars include aluminium hydroxide gel, enteric-coated aspirin, sucralfate, guar gum, cholestyramine, enteral feeding formulas, psyllium preparations, nifedipine XL, mesalamine and meprobamate. Bowel hypoactivity, dehydration, and concomitant use of anticholinergic and narcotic appear to contribute to the propensity for bezoar formation by aluminium hydroxide gel and Isocal. Insolubility of the carrying vehicle of enteric-coated aspirin and nifedipine is the setting in which these medications form bezoars. In contrast to non-medication bezoars, pharmacobezoars may produce additional symptoms, those related to the release of their active ingredients [4]. Mesalamine is an anti-inflammatory amino salicylate drug used in the treatment of ulcerative colitis, as well as Crohn’s disease. It works by reducing or stopping the production of natural chemicals which cause inflammation, swelling, tissue damage and diarrhoea. It does not get dissolved in acidic media and there is no dissolution therapy available for it [5].
Pharmacobezoars can present with symptoms of gastric outlet obstruction, but these bezoars can also produce symptoms due to their pharmacologic properties such as epigastric pain or discomfort, dyspepsia, postprandial fullness. As a result, there is an increased potential for drug intoxication in these patients. Complications such as gastrointestinal bleeding (6%) or intestinal obstruction or perforation (10%).
Our patient actually had benign GOO but due to misleading biopsy of Crohn’s disease and mesalamine therapy lead to formation of pharmacobezoar secondary to GOO.
One should always rule out GOO before prescribing any medication especially one which does not get dissolve in acidic media otherwise patients may develop pharmacobezoar and that may lead to diagnostic dilemma. Patient has to undergo many investigations and hospitalization, which increases the cost of treatment along with the psychological trauma and many days of work loss. So this type of secondary pharmacobezoar though rare but it’s a new evolving entity and should be kept in mind as one of the cause of recurrent upper gastrointestinal problem.
Rules for suspecting, diagnosing, and properly managing a pharmacobezoar are highly dependent on the pharmaceutical agent or agents involved. Becoming familiar with the sparse data available on pharmacobezoars and maintaining a high index of suspicion in future clinical encounters may be the best way to improve diagnostic sensitivity and accuracy.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Andru CH, Ponskky JL. Bezoars: classification, pathophysiology, and treatment. Am J Gastroenterol 1988;83:476–8. [PubMed] [Google Scholar]
- 2. Escamilla C, Robles-Campos R, Parrilla-Paricio P, Lujan-Mompean J, Liron-Ruiz R, Torralba-Martinez JA. Intestinal obstruction and bezoars. J Am Coll Surg 1994;179:285–8. [PubMed] [Google Scholar]
- 3. Robles R, Parrilla P, Escamilla C, Lujan JA, Torralba JA, Liron R, et al. . Gastrointestinal bezoars. Br J Surg 1994;81:1000–1. [DOI] [PubMed] [Google Scholar]
- 4. Taylor JR, Streetman DS, Castle SS. Medication bezoars: a literature review and a report of a case. Ann Pharmacother 1998;32:940–6. [DOI] [PubMed] [Google Scholar]
- 5. de Albuquerque IC, Carvalho MA, Betista RR, Formiga GJS. Bezoar by mesalamine tablet: cause of intestinal obstruction in Crohn’s disease. J Coloproctol (Rio J) 2012;32 (4:422-5). [Google Scholar]