Abstract
Cannabis is being increasingly used as a medical treatment for a variety of illnesses. However, the cannabis plant has more than 70 different phytocannabinoids with potential pharmacologic activity. Two of the most researched phytocannabinoids are delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD). Evidence suggests CBD can decrease some of the psychomimetic effects of THC. This has led to the development of a new drug, Nabiximols, for the treatment of moderate to severe spasticity due to multiple sclerosis. A discussion of evidence supporting proposed pharmacodynamic interplay between CBD and THC is presented.
Keywords: cannabis, delta-9-tetrahydrocannabinol, cannabidiol, marijuana, Nabiximols
Introduction
Cannabis sativa, or cannabis, is increasingly being approved as a medical treatment for a variety of illnesses, although it is still a Schedule I drug per federal law. As of June 2015, a total of 23 states and the District of Columbia had approved cannabis for medical purposes and another 4 states approved it for recreational uses. However, the cannabis plant has more than 70 different phytocannabinoids with potential pharmacologic activity.1 Although there is interest in many of these molecules, two of the phytocannabinoids contained in cannabis, delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), have been researched extensively because of their biologic effects. In this discussion, we will review the effects of each of these molecules and describe their pharmacodynamic interactions.
Endocannabinoid System
The ability of cannabis to cause physiologic effects is due to the endogenous cannabinoid or endocannabinoid system. There are two primary receptors for the endocannabinoid within the brain: cannabinoid 1 receptors (CB1Rs), which are primarily located on neurons in the central nervous system (CNS) and the peripheral nervous system, and cannabinoid 2 receptors (CB2Rs), which are located on glial cells in the CNS and in the immune and enteric nervous systems.2-4 Other receptors (eg, GPR55 and peroxisome proliferator–activated receptor-alpha [PPAR-alpha]) in the CNS are also activated by endocannabinoids but are not considered part of the endocannabinoid system.5 The psychotomimetic effects produced by cannabinoids, such as THC, are attributed to activation of CB1Rs.6 Cannabinoid 1 receptors are found on GABAergic terminals and on glutamatergic terminals in several areas of the brain, including the basal ganglia, frontal cortex, hippocampus, and cerebellum.7,8 Cannabinoid 2 receptors are expressed in similar areas of the brain but to a much lesser extent. Although several molecules have been suggested to have effects on the endocannabinoid system, the primary endogenous agonists are anandamide (AEA) and 2-arachidonoyl-glycerol (2-AG).9 Endocannabinoids are released on demand from the postsynaptic sites and exert their effects through fast retrograde signaling of the CB1Rs on the presynaptic membrane.10,11 Once bound, these G protein–coupled receptors activate inwardly rectifying K+ channels and inhibit voltage-sensitive N-type and P/Q-type Ca2+ channels, thus inhibiting the release of neurotransmitters.12 The pharmacologic term for endocannabinoid inhibition of GABA or glutamate release is depolarized suppression of inhibition or depolarization of excitation, respectively.13 The primary catabolic pathways for AEA and 2-AG are fatty acid amide hydrolase and monoacylglycerol lipase, respectively, which have become medication targets for pharmaceutical companies for new treatments, such as those for pain, depression, and osteoarthritis.14,15
Delta-9-Tetrahydrocannabinol
Delta-9-tetrahydrocannabinol is a partial agonist at both the CB1R and the CB2R. The binding to the CB1R is primarily responsible for the psychotomimetic effects of cannabis. The binding to the CB2R may have other immunologic or other anti-inflammatory effects.1 Delta-9-tetrahydrocannabinol can be administered in several formulations, including oral ingestion, sublingually, topically, vapor inhalation, smoked, mixed in food, and drunk in tea, and research studies have also administered it intravenously. It causes several potentially negative effects, including an increase in psychoactive symptoms, cognitive deficits, and an increase in heart rate.16 The psychoactive effects are generally related to perceptual alterations (ie, changes in intensity of sounds). At higher doses, and in vulnerable individuals, THC has been associated with exacerbating psychotic symptoms, such as delusions and hallucinations. In people with schizophrenia, THC causes worsening psychotic symptoms that are not counteracted by antipsychotic medications.17,18 It has an anxiogenic effect that in severe cases causes paranoia.
In general it is thought that THC causes acute cognitive problems, but the most stable cognitive deficits seen with THC administration are verbal learning deficits, specifically an inability to encode new information.19 Previously there has been debate regarding whether chronic cannabis use could result in a decrease in cognitive function. Recent evidence has suggested longer-term use of cannabis, especially if started in adolescents, results in memory deficits. Meier et al20 followed 1037 individuals during more than 20 years and found almost a 10-point decrease in IQ with chronic cannabis use starting in adolescents.20 The most common physiologic effect of THC is an increase in heart rate, but this generally is time limited and does not usually cause significant sequela.21
Other effects of THC have been used for clinical benefit. These include antiemetic, appetite stimulation, analgesic properties, and possibly some immunologic-modulating actions.22 Dronabinol, an oral THC product, is approved in the United States specifically for treatment of chemotherapy-induced nausea and vomiting and as an appetite stimulant. The purported effects of THC have led to states approving cannabis, which is a combination of dozens of phytocannabinoids, for a variety of diseases, including chronic pain, seizures, glaucoma, HIV/AIDS, and many other chronic medical illnesses. Several states have also approved cannabis for the treatment of posttraumatic stress disorder. Whiting et al22 conducted a meta-analysis of cannabis and cannabinoid drugs for medical usage and discovered 79 trials thought to be of adequate quality to review. In the final analysis they found moderate levels of evidence for efficacy in chronic pain and spasticity. There was limited evidence of efficacy in several other conditions, such as chemotherapy-induced vomiting and weight gain in HIV, although in general the short-term side effect burden was very high. Common adverse events reported included dizziness (66%), dry mouth (65%), nausea (55%), fatigue (42%), somnolence (49%), euphoria (37%), vomiting (34%), disorientation (27%), drowsiness (20%), confusion (18%), loss of balance (14%), and hallucinations (14%).22 Available data23 suggest there are a great deal of questions related to the wisdom of marketing cannabis as a medical treatment.
Cannabidiol
Experiments with CBD started in the early 1970s, with many of the studies analyzing how CBD interacted with THC in animals and humans. In general CBD has been found to be well tolerated and have few to no psychoactive effects. The most common side effect of CDB is sedation.24 The pharmacology of CBD is complex, because more than 20 different mechanisms of action have been described.5 It binds to both the CB1R and CB2R but acts as an antagonist at these receptors. Another mechanism of action that has received a lot of attention is the ability of CBD to inhibit the activity of fatty acid amide hydrolase, thus increasing AEA concentrations in the body. Clinical effects of CBD are being explored in a variety of illnesses, including epilepsy, anxiety disorders, cancer, anti-inflammatory effects, and schizophrenia.25
Pharmacodynamic Effects of THC and CBD
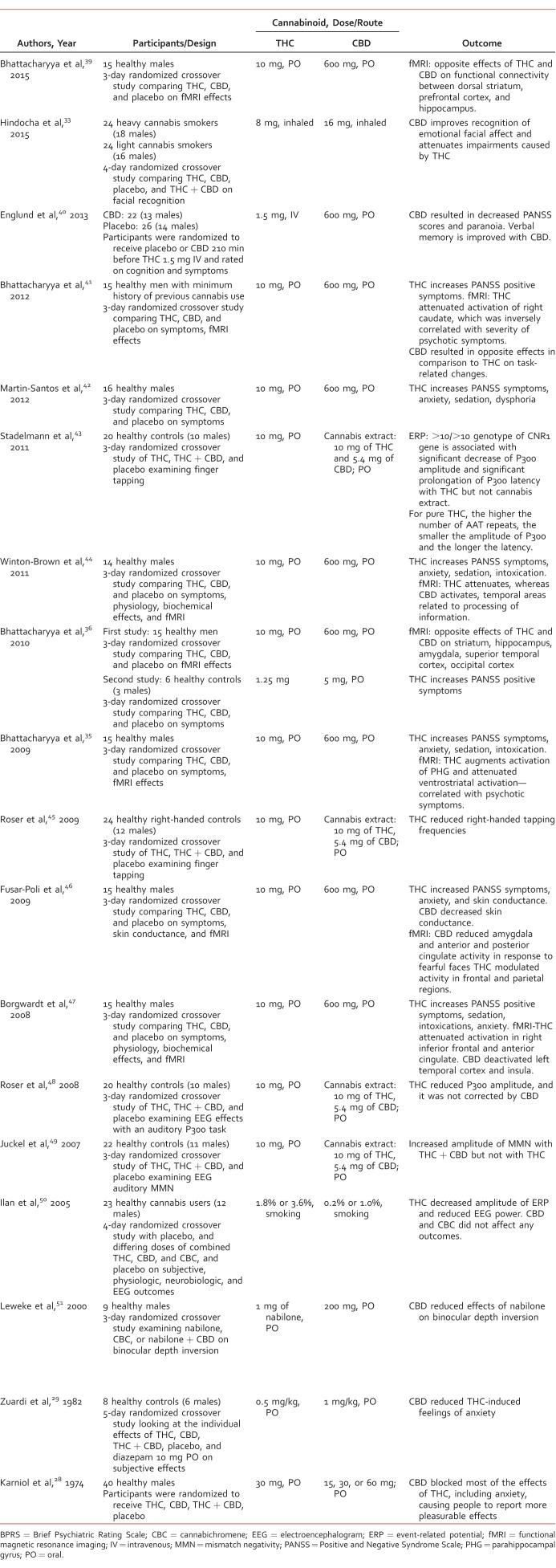
Cannabidiol and THC seem to have an important interaction in both negation of detrimental effects and potentiation of positive effects. For a list of human studies investigating the interactive and opposing actions of CBD and THC, see the Table. In one of the earliest animal studies by Karniol and Carlini,26 CBD was found to decrease many negative effects related to anxiety but potentiated the analgesic effects of THC. Another rodent study by Fernandes et al27 found that CBD actually prolonged the effects of THC in mice, and therefore potentiates the effects of THC. A series of subsequent studies in humans found CBD had few effects in healthy adults, but when combined with THC participants reported less anxiety and psychotic symptoms.28,29 Interestingly, one of the early studies, similar to the rodent study by Fernandes et al,30 showed that smoked cannabis with higher concentrations of CBD prolonged the effects of THC. Although there have been some contradictive studies, most evidence suggests CBD diminishes many of the psychoactive effects of THC. An epidemiologic study investigated this by taking hair samples from 120 current cannabis smokers. In the study31 they found individuals with CBD in hair samples reported fewer psychiatric affects then those with higher THC concentrations. This gives further credence that the laboratory findings are valid that CBD decreases psychotomimetic effects of cannabis by decreasing THC effects.
TABLE:
Human studies evaluating the effects of delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD)
Whether CBD could affect other clinical effects of THC has still been questioned. A study in 46 adults found oral CBD 600 mg given 3.5 hours before intravenous THC (1.5 mg) reduced verbal memory deficits to a greater extent than placebo when administered with THC. Furthermore, CBD reduced psychotic symptoms from THC as measured by the Positive and Negative Symptom Scale (PANSS).32 Emotional perception is altered in many people with cannabis use disorder. Hindocha et al33 conducted a randomized, crossover, double-blinded study during 4 days to examine the effects of oral THC (8 mg) and oral CBD (16 mg) and placebo in 48 participants, regarding the ability of participants to recognize emotional facial affect from pictures. Although the test participants reported no difference of feeling “stoned” with THC or THC + CBD, the THC test day resulted in more errors in emotion facial recognition that were corrected when CBD was given concurrently.33 The authors concluded that CBD reverses the deficits in emotional processing caused by THC.
It is unclear if the attenuation of effects is due to only pharmacodynamic effects or if pharmacokinetic effects are also involved. THC concentrations in the blood do not seem to be altered by CBD, but CBD may prevent THC from being converted into a more psychoactive metabolite, 11-hydroxy-THC.34 Bhattacharyya et al35 performed a functional magnetic resonance imaging (fMRI) study in which 15 individuals performed a series of cognitive tasks after given oral THC, CBD, or placebo during 3 different study days. They found THC and CBD had opposing neurobiologic effects on blood oxygen level–dependent responses, with CBD generally showing an increase in activation relative to placebo, and THC showing a decrease. In a second phase of the study they gave 6 individuals oral CBD or placebo before intravenous THC on 2 different test days and found that, similarly to previous studies, CBD diminished the psychotomimetic effects of THC. Several subsequent imaging studies from this group have consistently shown that CBD has opposing biologic effects in the brain,36 suggesting many of the effects are pharmacodynamic.
Nabiximols (Sativex®)
Nabiximols, a THC and CBD combination medication, has been approved in Europe for the treatment of symptomatic improvement in adult patients who experience moderate to severe spasticity due to multiple sclerosis.37 Pharmaceutical companies have been pursuing development of a selective CB2 agonist for their therapeutic action in areas of analgesia, inflammatory, and cancer. Given that the THC component acts as an agonist at CB1 and CB2, risking the CNS side effects, CBD was added since it is an antagonist at CB1. This mechanism would potentially neutralize the adverse CNS effects from the THC component, rendering this product to act as if it were selective for the CB2 receptor.38
Nabiximols is available as an oromucosal spray that contains 2.7 mg THC and 2.5 mg CBD per 100 mL spray. Patients are initially required to titrate nabiximols over an approximated 14-day period in order to achieve the desired dose. In clinical trials, the average therapeutic dose was 8 sprays per day in two-divided doses.37 Of note, the maximum dose is 12 sprays per day in two divided doses, though clinical trials have studied up to 48 sprays per day.37 Once desired total daily dose is achieved, patients are allowed to spread individual sprays across a 24-hour period based on individual tolerability and response. Given this, nabiximols is available as either three 10-mL spray bottles, or four 5.5-mL spray bottles for a total quantity of 30 mL and 22 mL respectively. These quantities would provide a 25 and 18-day supply, respectively, for patients taking the maximum recommended dosage of 12 sprays per day. Currently, nabiximols is undergoing phase 3 clinical trials in the United States for the treatment of cancer pain, although there has not been any regulatory application submitted for multiple sclerosis spasticity.
Conclusion
During the past 25 years we have gained a much better understanding of the endocannabinoid system and the effects of phytocannabinoids, such as THC and CBD. Evidence is accumulating that when CBD is administered with THC, CBD has the ability to diminish the psychoactive symptoms induced by THC through pharmacodynamics and possible pharmacokinetic interplay. Despite diminishing the psychoactive effects of THC, it is thought that CBD reserves the potential for THC to exert possible therapeutic action among many different disease states. It is with these findings that novel medications containing a combination of THC and CBD are being explored for potential clinical benefit.
Footnotes
Disclosures: Dr Ranganathan has received research support from Insys Therapeutics. The other authors have no disclosures to make.
References
- 1. Pertwee RG. . The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. 2008; 153 2: 199- 215. DOI: 10.1038/sj.bjp.0707442. PubMed PMID: 17828291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Devane WA, Dysarz FA, Johnson MR, Melvin LS, Howlett AC. . Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol. 1988; 34 5: 605- 13. PubMed PMID: 2848184. [PubMed] [Google Scholar]
- 3. Schatz AR, Lee M, Condie RB, Pulaski JT, Kaminski NE. . Cannabinoid receptors CB1 and CB2: a characterization of expression and adenylate cyclase modulation within the immune system. Toxicol Appl Pharmacol. 1997; 142 2: 278- 87. DOI: 10.1006/taap.1996.8034. PubMed PMID: 9070350. [DOI] [PubMed] [Google Scholar]
- 4. Cabral GA, Raborn ES, Griffin L, Dennis J, Marciano-Cabral F. . CB2 receptors in the brain: role in central immune function. Br J Pharmacol. 2008; 153 2: 240- 51. DOI: 10.1038/sj.bjp.0707584. PubMed PMID: 18037916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Izzo AA, Borrelli F, Capasso R, Di Marzo V, Mechoulam R. . Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci. 2009; 30 10: 515- 27. DOI: 10.1016/j.tips.2009.07.006. PubMed PMID: 19729208. [DOI] [PubMed] [Google Scholar]
- 6. Huestis MA, Gorelick DA, Heishman SJ, Preston KL, Nelson RA, Moolchan ET, et al. Blockade of effects of smoked marijuana by the CB1-selective cannabinoid receptor antagonist SR141716. Arch Gen Psychiatry. 2001; 58 4: 322- 8. PubMed PMID: 11296091. [DOI] [PubMed] [Google Scholar]
- 7. Domenici MR, Azad SC, Marsicano G, Schierloh A, Wotjak CT, Dodt HU, et al. Cannabinoid receptor type 1 located on presynaptic terminals of principal neurons in the forebrain controls glutamatergic synaptic transmission. J Neurosci. 2006; 26 21: 5794- 9. DOI: 10.1523/JNEUROSCI.0372-06.2006. PubMed PMID: 16723537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eggan SM, Lewis DA. . Immunocytochemical distribution of the cannabinoid CB1 receptor in the primate neocortex: a regional and laminar analysis. Cereb Cortex. 2007; 17 1: 175- 91. DOI: 10.1093/cercor/bhj136. PubMed PMID: 16467563. [DOI] [PubMed] [Google Scholar]
- 9. Mechoulam R, Parker LA. . The endocannabinoid system and the brain. Annu Rev Psychol. 2013; 64: 21- 47. DOI: 10.1146/annurev-psych-113011-143739. PubMed PMID: 22804774. [DOI] [PubMed] [Google Scholar]
- 10. Wilson RI, Nicoll RA. . Endogenous cannabinoids mediate retrograde signalling at hippocampal synapses. Nature. 2001; 410 6828: 588- 92. DOI: 10.1038/35069076. PubMed PMID: 11279497. [DOI] [PubMed] [Google Scholar]
- 11. Alger BE. . Retrograde signaling in the regulation of synaptic transmission: focus on endocannabinoids. Prog Neurobiol. 2002; 68 4: 247- 86. PubMed PMID: 12498988. [DOI] [PubMed] [Google Scholar]
- 12. Di Marzo V, Stella N, Zimmer A. . Endocannabinoid signalling and the deteriorating brain. Nat Rev Neurosci. 2014; 16 1: 30- 42. DOI: 10.1038/nrn3876. PubMed PMID: 25524120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parsons LH, Hurd YL. . Endocannabinoid signalling in reward and addiction. Nat Rev Neurosci. 2015; 16 10: 579- 94. DOI: 10.1038/nrn4004. PubMed PMID: 26373473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Justinova Z, Panlilio LV, Moreno-Sanz G, Redhi GH, Auber A, Secci ME, et al. Effects of fatty acid amide hydrolase (FAAH) inhibitors in non-human primate models of nicotine reward and relapse. Neuropsychopharmacology. 2015; 40 9: 2185- 97. DOI: 10.1038/npp.2015.62. PubMed PMID: 25754762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ramesh D, Gamage TF, Vanuytsel T, Owens RA, Abdullah RA, Niphakis MJ, et al. Dual inhibition of endocannabinoid catabolic enzymes produces enhanced antiwithdrawal effects in morphine-dependent mice. Neuropsychopharmacology. 2013; 38 6: 1039- 49. DOI: 10.1038/npp.2012.269. PubMed PMID: 23303065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. D'Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004; 29 8: 1558- 72. DOI: 10.1038/sj.npp.1300496. PubMed PMID: 15173844. [DOI] [PubMed] [Google Scholar]
- 17. D'Souza DC, Braley G, Blaise R, Vendetti M, Oliver S, Pittman B, et al. Effects of haloperidol on the behavioral, subjective, cognitive, motor, and neuroendocrine effects of Δ-9-tetrahydrocannabinol in humans. Psychopharmacology (Berl). 2008; 198 4: 587- 603. DOI: 10.1007/s00213-007-1042-2. PubMed PMID: 18228005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. D'Souza DC, Abi-Saab WM, Madonick S, Forselius-Bielen K, Doersch A, Braley G, et al. Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry. 2005; 57 6: 594- 608. DOI: 10.1016/j.biopsych.2004.12.006. PubMed PMID: 15780846. [DOI] [PubMed] [Google Scholar]
- 19. Ranganathan M, D'Souza DC. . The acute effects of cannabinoids on memory in humans: a review. Psychopharmacology (Berl). 2006; 188 4: 425- 44. DOI: 10.1007/s00213-006-0508-y. PubMed PMID: 17019571. [DOI] [PubMed] [Google Scholar]
- 20. Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RSE, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012; 109 40: E2657- 64. DOI: 10.1073/pnas.1206820109. PubMed PMID: 22927402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Carbuto M, Sewell RA, Williams A, Forselius-Bielen K, Braley G, Elander J, et al. The safety of studies with intravenous Δ9-tetrahydrocannabinol in humans, with case histories. Psychopharmacology (Berl). 2012; 219 3: 885- 96. DOI: 10.1007/s00213-011-2417-y. PubMed PMID: 21845389. [DOI] [PubMed] [Google Scholar]
- 22. Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015; 313 24: 2456- 73. DOI: 10.1001/jama.2015.6358. PubMed PMID: 26103030. [DOI] [PubMed] [Google Scholar]
- 23. D'Souza DC, Ranganathan M. . Medical marijuana: is the cart before the horse? JAMA. 2015; 313 24: 2431- 2. DOI: 10.1001/jama.2015.6407. PubMed PMID: 26103026. [DOI] [PubMed] [Google Scholar]
- 24. Zuardi AW, Hallak JEC, Dursun SM, Morais SL, Sanches RF, Musty RE, et al. Cannabidiol monotherapy for treatment-resistant schizophrenia. J Psychopharmacol. 2006; 20 5: 683- 6. DOI: 10.1177/0269881106060967. PubMed PMID: 16401651. [DOI] [PubMed] [Google Scholar]
- 25. Zuardi AW. . Cannabidiol: from an inactive cannabinoid to a drug with wide spectrum of action. Rev Bras Psiquiatr. 2008; 30 3: 271- 80. PubMed PMID: 18833429. [DOI] [PubMed] [Google Scholar]
- 26. Karniol IG, Carlini EA. . Pharmacological interaction between cannabidiol and delta 9-tetrahydrocannabinol. Psychopharmacologia. 1973; 33 1: 53- 70. PubMed PMID: 4358666. [DOI] [PubMed] [Google Scholar]
- 27. Fernandes M, Schabarek A, Coper H, Hill R. . Modification of delta9-THC-actions by cannabinol and cannabidiol in the rat. Psychopharmacologia. 1974; 38 4: 329- 38. PubMed PMID: 4473791. [DOI] [PubMed] [Google Scholar]
- 28. Karniol IG, Shirakawa I, Kasinski N, Pfeferman A, Carlini EA. . Cannabidiol interferes with the effects of delta 9-tetrahydrocannabinol in man. Eur J Pharmacol. 1974; 28 1: 172- 7. PubMed PMID: 4609777. [DOI] [PubMed] [Google Scholar]
- 29. Zuardi AW, Shirakawa I, Finkelfarb E, Karniol IG. . Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology (Berl). 1982; 76 3: 245- 50. PubMed PMID: 6285406. [DOI] [PubMed] [Google Scholar]
- 30. Hollister LE, Gillespie H. . Interactions in man of delta-9-tetrahydrocannabinol. II. Cannabinol and cannabidiol. Clin Pharmacol Ther. 1975; 18 1: 80- 3. PubMed PMID: 1097148. [DOI] [PubMed] [Google Scholar]
- 31. Morgan C, Gardener C, Schafer G, Swan S, Demarchi C, Freeman TP, et al. Sub-chronic impact of cannabinoids in street cannabis on cognition, psychotic-like symptoms and psychological well-being. Psychol Med. 2012; 42 2: 391- 400. DOI: 10.1017/S0033291711001322. PubMed PMID: 21798112. [DOI] [PubMed] [Google Scholar]
- 32. Wright MJ Jr, Vandewater SA, Taffe MA. . Cannabidiol attenuates deficits of visuospatial associative memory induced by Δ(9) tetrahydrocannabinol. Br J Pharmacol. 2013; 170 7: 1365- 73. DOI: 10.1111/bph.12199. PubMed PMID: 23550724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hindocha C, Freeman TP, Schafer G, Gardener C, Das RK, Morgan CJA, et al. Acute effects of delta-9-tetrahydrocannabinol, cannabidiol and their combination on facial emotion recognition: a randomised, double-blind, placebo-controlled study in cannabis users. Eur Neuropsychopharmacol. 2015; 25 3: 325- 34. DOI: 10.1016/j.euroneuro.2014.11.014. PubMed PMID: 25534187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bornheim LM, Grillo MP. . Characterization of cytochrome P450 3A inactivation by cannabidiol: possible involvement of cannabidiol-hydroxyquinone as a P450 inactivator. Chem Res Toxicol. 1998; 11 10: 1209- 16. DOI: 10.1021/tx9800598. PubMed PMID: 9778318. [DOI] [PubMed] [Google Scholar]
- 35. Bhattacharyya S, Fusar-Poli P, Borgwardt S, Martin-Santos R, Nosarti C, O'Carroll C, et al. Modulation of mediotemporal and ventrostriatal function in humans by Delta9-tetrahydrocannabinol: a neural basis for the effects of Cannabis sativa on learning and psychosis. Arch Gen Psychiatry. 2009; 66 4: 442- 51. DOI: 10.1001/archgenpsychiatry.2009.17. PubMed PMID: 19349314. [DOI] [PubMed] [Google Scholar]
- 36. Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, et al. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010; 35 3: 764- 74. DOI: 10.1038/npp.2009.184. PubMed PMID: 19924114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Electronic Medicines Compendium. Sativex: Summary of product characteristics [Internet]. Leatherhead, UK: Datapharm [cited 2016. Apr 23]. Available from: http://www.medicines.org.uk/emc/search/Sativex?term=Sativex&searchtype=QuickSearch
- 38. Russo E, Guy GW. . A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Med Hypotheses. 2006; 66 2: 234- 46. DOI: 10.1016/j.mehy.2005.08.026. PubMed PMID: 16209908. [DOI] [PubMed] [Google Scholar]
- 39. Bhattacharyya S, Falkenberg I, Martin-Santos R, Atakan Z, Crippa JA, Giampietro V, et al. Cannabinoid modulation of functional connectivity within regions processing attentional salience. Neuropsychopharmacology. 2015; 40 6: 1343- 52. DOI: 10.1038/npp.2014.258. PubMed PMID: 25249057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Englund A, Morrison PD, Nottage J, Hague D, Kane F, Bonaccorso S, et al. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J Psychopharmacol. 2013; 27 1: 19- 27. DOI: 10.1177/0269881112460109. PubMed PMID: 23042808. [DOI] [PubMed] [Google Scholar]
- 41. Bhattacharyya S, Crippa JA, Allen P, Martin-Santos R, Borgwardt S, Fusar-Poli P, et al. Induction of psychosis by Δ9-tetrahydrocannabinol reflects modulation of prefrontal and striatal function during attentional salience processing. Arch Gen Psychiatry. 2012; 69 1: 27- 36. DOI: 10.1001/archgenpsychiatry.2011.161. PubMed PMID: 22213786. [DOI] [PubMed] [Google Scholar]
- 42. Martin-Santos R, Crippa JA, Batalla A, Bhattacharyya S, Atakan Z, Borgwardt S, et al. Acute effects of a single, oral dose of d9-tetrahydrocannabinol (THC) and cannabidiol (CBD) administration in healthy volunteers. Curr Pharm Des. 2012; 18 32: 4966- 79. PubMed PMID: 22716148. [DOI] [PubMed] [Google Scholar]
- 43. Stadelmann AM, Juckel G, Arning L, Gallinat J, Epplen JT, Roser P. . Association between a cannabinoid receptor gene (CNR1) polymorphism and cannabinoid-induced alterations of the auditory event-related P300 potential. Neurosci Lett. 2011; 496 1: 60- 4. DOI: 10.1016/j.neulet.2011.04.003. PubMed PMID: 21513772. [DOI] [PubMed] [Google Scholar]
- 44. Winton-Brown TT, Allen P, Bhattacharyya S, Borgwardt SJ, Fusar-Poli P, Crippa JA, et al. Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an FMRI study. Neuropsychopharmacology. 2011; 36 7: 1340- 8. DOI: 10.1038/npp.2011.17. PubMed PMID: 21412224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Roser P, Gallinat J, Weinberg G, Juckel G, Gorynia I, Stadelmann AM. . Psychomotor performance in relation to acute oral administration of Delta9-tetrahydrocannabinol and standardized cannabis extract in healthy human subjects. Eur Arch Psychiatry Clin Neurosci. 2009; 259 5: 284- 92. DOI: 10.1007/s00406-009-0868-5. PubMed PMID: 19224107. [DOI] [PubMed] [Google Scholar]
- 46. Fusar-Poli P, Allen P, Bhattacharyya S, Crippa JA, Mechelli A, Borgwardt S, et al. Modulation of effective connectivity during emotional processing by Delta 9-tetrahydrocannabinol and cannabidiol. Int J Neuropsychopharmacol. 2009; 13 4: 421- 32. DOI: 10.1017/S1461145709990617. PubMed PMID: 19775500. [DOI] [PubMed] [Google Scholar]
- 47. Borgwardt SJ, Allen P, Bhattacharyya S, Fusar-Poli P, Crippa JA, Seal ML, et al. Neural basis of Delta-9-tetrahydrocannabinol and cannabidiol: effects during response inhibition. Biol Psychiatry. 2008; 64 11: 966- 73. DOI: 10.1016/j.biopsych.2008.05.011. PubMed PMID:18589404. [DOI] [PubMed] [Google Scholar]
- 48. Roser P, Juckel G, Rentzsch J, Nadulski T, Gallinat J, Stadelmann AM. . Effects of acute oral Delta9-tetrahydrocannabinol and standardized cannabis extract on the auditory P300 event-related potential in healthy volunteers. Eur Neuropsychopharmacol. 2008; 18 8: 569- 77. DOI: 10.1016/j.euroneuro.2008.04.008. PubMed PMID: 18544469. [DOI] [PubMed] [Google Scholar]
- 49. Juckel G, Roser P, Nadulski T, Stadelmann AM, Gallinat J. . Acute effects of Delta9-tetrahydrocannabinol and standardized cannabis extract on the auditory evoked mismatch negativity. Schizophr Res. 2007; 97 1-3: 109- 17. PubMed PMID: 17884351. [DOI] [PubMed] [Google Scholar]
- 50. Ilan AB, Gevins A, Coleman M, ElSohly MA, de Wit H. . Neurophysiological and subjective profile of marijuana with varying concentrations of cannabinoids. Behav Pharmacol. 2005; 16 5-6: 487- 96. PubMed PMID: 16148455. [DOI] [PubMed] [Google Scholar]
- 51. Leweke FM, Schneider U, Radwan M, Schmidt E, Emrich HM. . Different effects of nabilone and cannabidiol on binocular depth inversion in Man. Pharmacol Biochem Behav. 2000; 66 1: 175- 81. PubMed PMID:10837858. [DOI] [PubMed] [Google Scholar]