Abstract
Patients with underlying medical disease can present to the health care system with psychiatric symptoms predominating. Identification of an underlying medical condition masquerading as a psychiatric disorder can be challenging for clinicians, especially in patients with an existing psychiatric condition. The term medical mimic or secondary psychosis has been used to describe this clinical situation. Diagnostic categories from The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, that may encompass medical mimics include substance-induced disorders, which includes medications, and unspecified mental disorder due to another medical condition in situations where the clinician may lack needed information for a complete diagnosis. At this time, there is no single diagnostic test or procedure available to differentiate primary versus secondary psychosis on the basis of psychopathology presentation alone. When considering a diagnosis, clinicians should evaluate for the presence of atypical features uncharacteristic of the psychiatric symptoms observed; this may include changes in functionality and/or age of onset and symptom presentation severity. The purpose of this work is to provide a structured clinical framework for evaluation for medical mimics, identify groups considered to be at highest risk for medical mimics, and present common syndromic features suggestive of a medical mimic. Selected case scenarios are used to illustrate key concepts for evaluating and assessing a patient presenting with acute psychiatric symptomatology to improve judgment in ruling out potential medical causality.
Keywords: diagnostic evaluation, medical mimic, physical examination, psychotic disorder due to another medical condition, secondary psychosis, substance-induced disorder
Background
Patients with underlying medical disease can present to the health care system with psychiatric symptoms predominating. Identification of an underlying medical condition masquerading as a psychiatric disorder can be challenging for clinicians, especially in patients with an existing psychiatric condition.1 There is no single test, examination, or procedure to easily and effectively differentiate primary versus secondary psychosis on the basis of presenting psychopathology alone.1 The general terms medical mimic or secondary psychosis have been used to describe this clinical situation. Although certain presenting signs and symptoms may be suggestive of a medical mimic, there is no clear-cut constellation of pathognomonic signs and symptoms to guide the clinician to the correct diagnosis.1 In older literature, the term organic cause referenced a physical or physiologic change to some tissue or organ of the body; however, this term has fallen out of favor.2 The term secondary psychosis generally applies to a psychotic disorder arising from substance abuse or a preexisting physical health diagnosis.3 The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), addresses this phenomenon via two diagnostic categories: substance-induced disorders, which includes medications, and unspecified mental disorder due to another medical condition in situations where the clinician may lack needed information for a complete diagnosis.4 In both of the DSM-5 diagnostic categories, the individual may present with symptoms of delusions and/or hallucinations, while the broader interpretation of medical mimics may include other psychiatric symptoms, such as depression, confusion, or mood lability. Overall crucial assessment procedures are less likely to be performed if the patient is admitted to a psychiatric service than if he or she is admitted to a medical service.5 Symptoms in patients with a history of mental illness are more likely to be attributed to psychiatric illness than those of patients without such a history. Of note, there is a relative dearth of published literature on this topic, and most published reports predate the publication of the DSM-5 in 2013.
Hallmark signs and symptoms of a medical mimic include one or more features that are atypical for the psychiatric symptoms. These comprise, but are not limited to, normal functioning prior to onset, unusual age at onset, and/or paroxysmal onset. Other elements to consider in the evaluative process include the presence or absence of a prior personal or family history of mental illness, recent substance abuse, prescription medication use (new medication, recent dosage change, unreported overuse or abuse), waxing and waning mental status change, treatment resistance, or any unusual response to treatment.1 Groups considered to be at higher risk for medical illness presenting with psychiatric symptoms include the elderly, patients with a history of substance abuse disorder(s), patients without a prior history of psychiatric illness, patients with preexisting medical illness, and patients from lower socioeconomic strata.6
It is clear that initial misdiagnosis can lead to a variety of issues, including unnecessary or harmful treatment, unintended delay in treatment, increased length of hospitalization, and increased costs to the health care system and payers. Diagnoses traditionally are based on the clinical features observed at the time of presentation to the health care system. In general, these observed clinical features are consistent with the known body of literature for symptoms classification of disorders or disease states (ie, rule in or rule out based on the clinical presentation and initial evaluation results).7 In persons with a history of mental illness, there may be the potential to attribute observed symptoms to that mental illness before doing a thorough medical evaluation. Therefore, a careful and consistent evaluation framework may improve the larger body of information that informs the interpretation of the clinical presentation and minimizes initial misdiagnosis.
The purpose of the present work is to provide a clear, comprehensive, and structured process for consideration in evaluating and assessing a patient with an acute psychiatric presentation. Differentiating primary from secondary psychosis is critical in order to minimize the risk of overlooking and addressing an underlying medical issue that may be causal.
Evaluation Schema
The presentation of confusion or disorientation, agitation, mood lability, and hallucinations and/or delusions may be multifactorial. Medications, substance use/abuse and withdrawal, infections, stroke, metabolic or endocrine conditions, and cardiopulmonary disease are common underlying causes for psychiatric symptomatology presenting acutely.1,6,8-10 To aid in establishing a cause and effect relationship between psychiatric symptoms and physical findings, Keshaven and Kaneko11 created the following set of questions as a guide.
Is the presentation of the psychiatric symptom(s) atypical?
Is the medical condition or substance use temporally related to the psychiatric symptom?
Are the psychiatric symptoms better explained by a primary psychiatric disorder?
Is the psychiatric presentation a direct consequence of a medical illness or substance use?
Integration and consideration of these elements as one aspect of the clinical assessment process will further inform clinicians as they seek to determine causality of the presenting symptoms.
Components of Evaluation
Multiple sources suggest a variety of elements as part of a comprehensive patient workup. The published literature consensus is that these elements should include1,6,8-11:
A complete medical and psychiatric history
History of present illness with review of systems to identify symptoms suggestive of medical causality
Physical exam
Review of current prescription, over-the-counter and alternative medications, and recent changes
Mental status examination
Laboratory and diagnostic testing (see specific tests below)
Interpretation of aggregated findings
It is paramount that clinicians avoid diagnostic overshadowing (defined as the tendency to attribute symptoms of mental or physical illness to the primary mental illness), and consider the impact of culture (such as behaviors toward authority figures) during the patient evaluation process.12 Furthermore, it is important to note that patients with a well-controlled psychiatric illness may develop an as yet undetected physical illness (such as new-onset diabetes or diabetic ketoacidosis, or an acute infection) that leads to an exacerbation of the psychiatric disorder.13,14 Clinicians are cautioned to avoid the often erroneous assumption that all psychiatric symptoms are related to that disorder. New-onset psychiatric symptoms may be qualitatively different in a patient with a known or well-controlled preexisting psychiatric illness.6,8
Laboratory and Diagnostic Testing
A comprehensive battery of laboratory and metabolic assessments should include:
-
•
Pulse oximetry
-
•
Chemistry panel (including electrolytes, blood glucose, liver function tests, blood urea nitrogen, creatinine)
-
•
Assessment of therapeutic drug levels as appropriate
-
•
Urine drug screen for substance use
-
•
Blood alcohol level
-
•
Complete blood count
-
•
Urinalysis
-
•
Thyroid function testing
-
•
Erythrocyte sedimentation rate and/or C-reactive protein
-
•
Rapid plasma reagin screening for syphilis
-
•
Acquired immune deficiency syndrome/human immunodeficiency virus (AIDS/HIV) screening, with additional follow-up testing if positive
Examples of additional tests include1,6,8-10:
-
•
Head computed tomography: patients with new-onset psychiatric symptoms that are atypical or incongruent with other findings, those with delirium, headache, history of recent trauma, or focal neurologic findings (weakness of an extremity)
-
•
Lumbar puncture: patients with meningeal signs or normal head computed tomography findings with symptoms of fever, headache, or delirium
-
•
Chest x-ray: patients with low oxygen saturation, fever, productive cough, or hemoptysis
-
•
Blood cultures and/or urine cultures: seriously ill patients with unexplained fever
-
•
Testing for systemic lupus erythematosus, syphilis, demyelinating disorders, or Lyme disease in patients with vision or gait changes, numbness, burning, or tingling
-
•
Vitamin B12 or thiamine deficiency testing, especially in patients presenting with signs of dementia that are otherwise unexplained
Additional diagnostic testing not part of a typical battery of assessments should be performed only if clinical findings indicate the need for more information in order to form an accurate diagnosis.1,8,11 More tests are not necessarily useful in time utility and/or cost effectiveness. The potential for false-positive test results should also be evaluated.
Interpretation of Findings
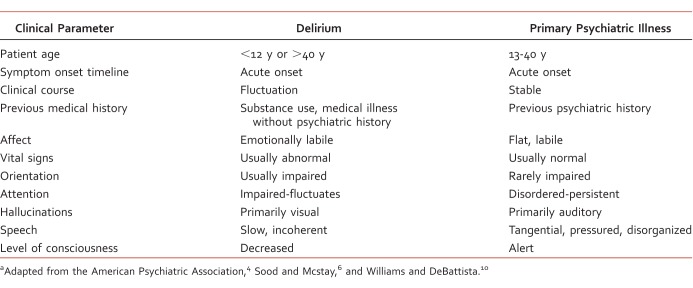
Findings from the comprehensive workup serve to guide any additional testing, diagnostic formulation, and subsequent treatment. The extent of the medical workup beyond that outlined above should be determined by probabilities (ie, rule out the more likely disorders), identifying treatable conditions prior to focusing on less frequently encountered disorders.1 Examples of signs/symptoms/findings that may suggest or flag a potential medical mimic for further consideration are listed in Table 1.
TABLE 1: .
Signs and symptomsa
Some clinical findings may point to a specific cause, especially when signs and symptoms are of recent onset or vary from a well-established baseline. Comprehensive tables listing psychiatric emergency findings with potential medical causality are available elsewhere.3,9-11 However, some common examples of physical findings that may be indicative of medical mimics related to medications or substances are noted below—for example, dilated pupils, particularly if accompanied by flushed, hot, dry skin which might suggest anticholinergic effects. Constricted pupils may be suggestive of opioid intoxication. Mydriasis may be related to opioid withdrawal, whereas nystagmus is suggestive of phenytoin toxicity in a patient receiving this agent. Cognitive changes, paired with autonomic instability, skeletal muscle rigidity, and antipsychotic use, may suggest neuroleptic malignant syndrome.
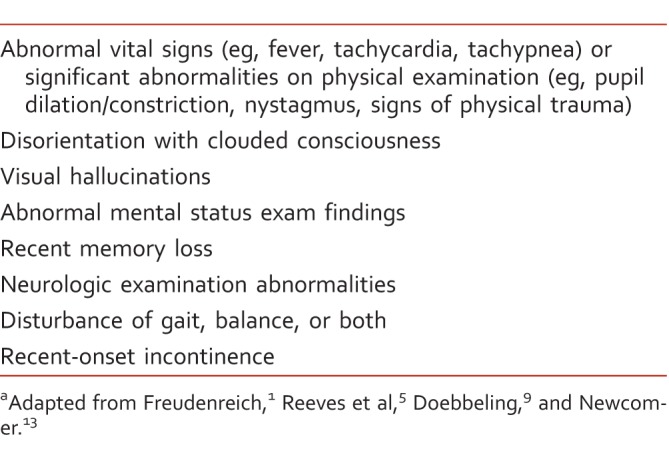
Another challenge is delirium identification and differentiation from a primary psychiatric illness. With incomplete and/or erroneous information regarding the symptom timeline, clinical course, and medical history prior to presentation, the immediate signs and symptoms of delirium and primary psychiatric disturbance are similar and difficult to discriminate. It is critical to differentiate delirium from primary psychiatric illness, given the symptoms may fully or partially remit once the underlying cause is identified and addressed.6 Table 2 outlines key clinical features to aid in distinguishing delirium from a primary psychiatric illness. Without a complete history and clinical course timeline, it is difficult to accurately differentiate delirium from a primary psychosis. Another commonly encountered situation includes the sudden onset of aphasia, which may suggest a stroke. Similarly, symptoms that began shortly after significant trauma or after beginning a new drug may be related to those events.1,9,10
TABLE 2: .
Differential factors distinguishing delirium from primary psychiatric illnessa
Drug or alcohol abuse (determined either via patient history and/or lab testing) should be ruled out as potentially causal for hallucinations and delusions in particular, because a significant percentage of the population of patients with a psychiatric disorder have a comorbid substance use disorder (lifetime comorbidity prevalence of 47% or more for persons diagnosed with schizophrenia).15 The 2014 national survey16 conducted by the Substance Abuse and Mental Health Services Administration on drug use and health reported illicit use for persons 12 years and older to be 10.2%.
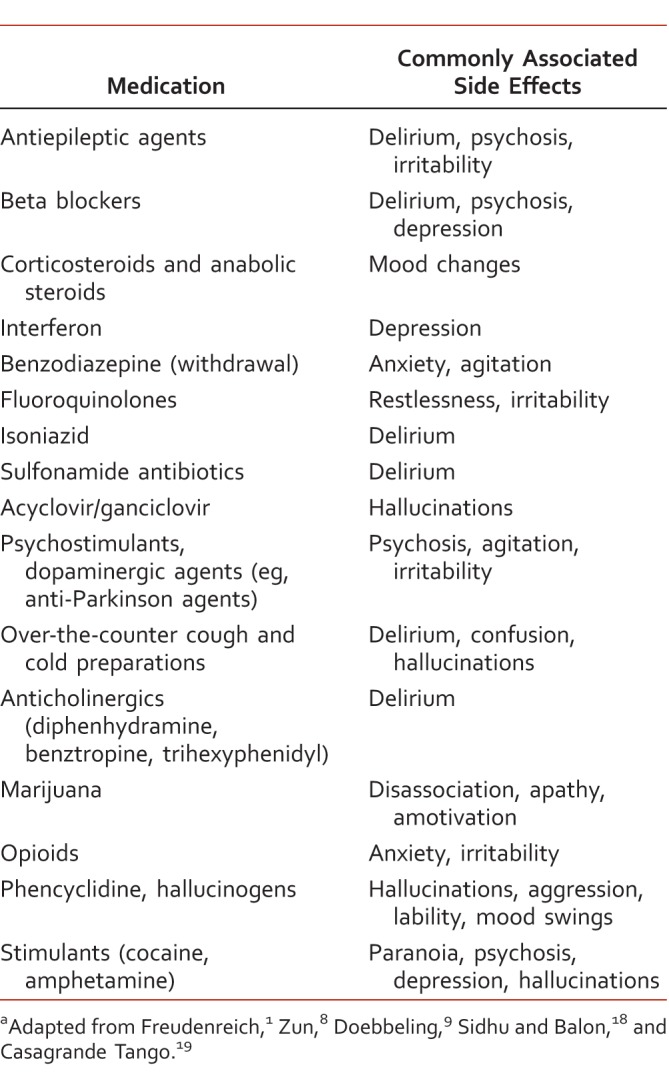
A comprehensive medication history may reveal additional useful information for the clinician. The medication history should include prescription, over-the-counter, and herbal/alternative medications, as well as substance use and alcohol intake. In addition, questions related to prescription sharing, defined as taking medications prescribed to another individual, should be asked.17 Any recent changes in a regimen (additions, dose changes, and/or discontinuation) should also be determined.18,19 A clinical pharmacist's evaluation in this domain is a key step to determine if any drug-drug or drug–disease state interactions, adverse medication effects, or other potential medication or substance use or withdrawal issues are contributory. Risk factors for medication-related psychiatric side effects include increased patient age, hepatic and/or renal insufficiency, past or present history of psychiatric illness, polypharmacy, doses at the upper end of the recommended range (both psychiatric and nonpsychiatric medications), sublingual/intravenous/intrathecal route of administration, as well as use of central nervous system (CNS)-active agents and narrow therapeutic index agents.1,9,18,20
Many medications may be associated with psychiatric side effects, and comprehensive lists of medications frequently implicated are widely available. A brief list along with the corresponding commonly associated psychiatric side effects may be found in Table 3.1,9,18,20 The most frequent offenders are CNS-active drugs (anticonvulsants, antidepressants, antipsychotics, sedative/hypnotics, psychostimulants), dopaminergic anti-Parkinson therapies, anticholinergics, and corticosteroids.8,9,11 Drugs of abuse, notably alcohol, amphetamines, cocaine, hallucinogens, and phencyclidine, are also frequently implicated in triggering or exacerbating psychiatric side effects. Withdrawal from substances, especially alcohol or benzodiazepines, may cause anxiety and/or extreme agitation in addition to symptoms of physical withdrawal.8,9 In general, most psychiatric adverse effects related to medication use can be managed by stopping the offending medication(s) and replacing it with a different therapy, as clinically indicated, with the assistance of a pharmacist's evaluation and consultative recommendations.
TABLE 3: .
Commonly associated psychiatric side effectsa
Although it is beyond the scope of this review to fully explore and elucidate the differential diagnosis and treatment of medical mimics a clinician may encounter in all situations, the following cases from the authors' practices, or those drawn from the published literature, are intended to illustrate the utility of routine application of the above clinical construct in patient evaluation and assessment. In particular, employing this structured process may be of value to the clinician in evaluating causality of the presenting psychiatric symptoms when an underlying medical condition may, in fact, be undetected.
Cases
Myxedema Madness
Hypothyroidism is a clinical condition resulting from insufficient circulating thyroid hormone manifesting as a metabolic slowing. Commonly reported symptoms include fatigue, weakness, weight gain, cold intolerance, and dry, coarse hair, with corresponding dry, rough, pale skin. Psychiatric symptoms may include depression, irritability, memory loss or impairment, and myxedema coma. Much less frequently reported is a clinical condition referred to as myxedema madness, a severe psychosis related to significant hypothyroidism.1,20,21 Recent case reports highlighted the presentation of this change in cognition and onset of psychiatric symptoms.
In the first case, the patient had no prior psychiatric history but had a past medical history significant for hypothyroidism and was levothyroxine nonadherent for 4 months. On admission, delusions and visual hallucinations were reported. Admission lab work revealed a thyroid-stimulating hormone concentration of 60.29 mIU/L (normal range = 0.47-4.68 mIU/L), a total triiodothyronine concentration of 34 ng/dL (normal range = 97-169 ng/dL), and a thyroxine concentration of 1.3 μg/dL (normal range = 5.1-13.8 μg/dL). The patient's age and substance use history were not reported. Levothyroxine was resumed, and haloperidol was added. Clinicians were unable to evaluate whether the presenting psychotic features were due to the general medical condition or an unrelated change in mental status, leading to the plan to initiate low-dose haloperidol, discharge, and evaluate as an outpatient.20
In a separate case, the patient developed signs and symptoms of psychosis secondary to a thyroidectomy for thyroid cancer done prior to admission. Changes in mental status for this patient were characterized by psychomotor agitation, directives from an “inner voice,” and aggression (screaming and hitting family). Admission lab work was consistent with severe hypothyroidism: thyroid-stimulating hormone concentration of 62.9 mIU/L, a free thyroxine concentration less than 0.35 ng/dL (normal = 0.7-1.9 ng/dL), a triiodothyronine concentration of 70 ng/dL, and a total thyroxine concentration less than 1 μg/dL. Thyroid supplementation was initiated with levothyroxine, as were psychiatric agents (haloperidol, lorazepam, and levomepromazine—currently not available in the United States).
Following levothyroxine initiation, the severe hypothyroidism had almost completely resolved, and within 4 months of treatment, the psychopharmacologic medications were tapered to discontinuation with complete resolution of psychiatric symptoms.21 These case reports illustrate the presentation of an infrequently diagnosed medical condition masquerading as a psychosis in individuals with no prior history of mental illness. The sudden onset of psychosis with no prior history flagged the cases for additional follow-up. Following the comprehensive intake procedure, which consisted of a complete medical history, diagnostic lab work, and review of medication adherence, appropriate pharmacotherapy and follow-up were successfully initiated.
Delirium
To illustrate how delirium can be difficult to identify, the case of a 56-year-old white man diagnosed with bipolar I disorder (most recent episode manic), nicotine dependence, chronic kidney disease stage 3, and benign prostatic hypertrophy is described. The patient's history was significant for previous lithium toxicity and mood instability. At times the patient demonstrated neurocognitive deficits characterized by gait instability and balance problems. Social history was positive for tobacco (approximately 1 pack per day) and marijuana use (believed to be 2-3 times per week).
When the patient was evaluated in the psychiatric clinic, speech was fluent, rapid, and pressured. Thought processes were vague, tangential, and disorganized, with illogical content. He denied delusions or hallucinations. His medication regimen included aripiprazole 25 mg, olanzapine oral disintegrating tablet 15 mg daily, clonazepam 0.5 mg at bedtime, and hydroxyzine 50 mg at bedtime and 25 mg up to twice daily for anxiety. To monitor for divalproex adherence, a valproic acid level was ordered and found to be within normal limits. The attending physician did not order a serum ammonia level, although with the use of divalproex in this case (1500 mg), it may have been useful to rule out divalproex-associated encephalopathy. The patient was monitored for medication adherence, then returned home. Two weeks later, hospitalization was needed because of increasingly bizarre statements and behaviors. A urine drug screen and urinalysis were obtained. The urine drug screen was negative; however, the urinalysis revealed a urinary tract infection (UTI), which, when treated with appropriate antibiotics, led to a resolution of psychiatric symptoms. The admitting psychiatrist determined delirium was the primary cause for psychiatric decompensation based on patient presentation, time course of onset, and laboratory results. Following initiation of antibiotic therapy, the psychosis remitted, and he returned to his preadmission level of psychosocial functioning.
Delirium has been characterized as one of the most underrecognized and undertreated neuropsychiatric syndromes, with disturbances in cognition, psychomotor behaviors, and alertness.22 The origins are typically multifactorial. Risk factors include illicit drug use, medications (examples in Table 3), hydration status, and metabolic disorders.21 Appropriate and timely treatment are dependent on recognition. Common presentations include lethargy, disorientation, agitation, delusions, and hallucinations. Diagnostic criteria for delirium encompass disorganized thinking, disturbances in perception, and fluctuating clinical symptoms.4 Consistent with the components for a comprehensive evaluation, clinicians are encouraged to consider delirium (until proven otherwise) in cases of a sharp and sudden decline in cognitive function.
A systemic review of the published literature relative to UTIs and delirium reported UTIs as one of the most common bacterial infections in elderly patients, whose ages may include persons as young as 55 years. They are highly correlated with the onset or exacerbation of neuropsychiatric disorders. The mean weighted prevalence of UTI in individuals with delirium was 19.4% versus 12.8% in individuals without delirium. The 8 studies reviewed suggested that UTIs were an independent risk factor for developing delirium.23
Typical management of delirium includes completion of a validated, evidence-based delirium rating scale, pre-episode functioning (preexisting deficits in cognitive function), thorough medication history focusing on the use of psychoactive medications, and elimination of the possibility of metabolic imbalances and/or infection. In addition to routine laboratory studies, additional diagnostic tests may be performed to provide additional clinical information when indicated. Any abnormal findings, such as electrolyte imbalance, dehydration, hypercalcemia, and hypoxia, should be corrected, and potentially offending drugs discontinued or decreased.24 The sudden exacerbation of psychotic symptoms in the above delirium case was secondary to a UTI. As an example of the potential consequences of not performing a thorough medical workup in the evaluation schema outlined, a delay identifying the underlying correctable medical condition (UTI) occurred, along with lag time to appropriate treatment and associated increased morbidity.
Degenerative Neurologic Disorder
As the clinician gathers information, interprets diagnostic test results, and formulates a diagnosis, psychotic symptoms as features of degenerative neurologic disorders, such as Parkinson disease (PD), must also be considered.
Secondary psychosis or psychotic disorder due to another medical condition, arising from a degenerative neurologic disorder, such as PD, is relatively common. Features include visual hallucinations, progression over time, and emergence later in the disease course.25 The prevalence of hallucinations in this population has been reported to be up to 40%.26,27 Adverse medication effects have also been reported in persons with a diagnosis of PD, as illustrated by the following case.
A psychiatrically stable 56-year-old man with PD receiving a total daily dose of pramipexole 0.75 mg was titrated to 1.125 mg per day. Following this change, verbal and physical aggression increased. Psychotic symptoms presented. During the course of the next month, episodes of hallucinations and delusions tripled. Pramipexole was tapered to the previous total daily dose of 0.75 mg, and the behaviors returned to baseline levels by the second month. Anti-Parkinson pharmacotherapy and the corresponding increase in CNS dopamine are often implicated in causing or exacerbating psychosis.28
In this case, a thorough medication history, review of recent changes in a regimen (particularly the small dose change), and understanding of the patient's degenerative disease process contributed to a timely intervention and stabilization. Clinicians who may be new to neuropsychiatric patients are reminded that unintended behavioral and intended clinical response to medication may be impacted by a multidimensional set of variables, specifically age-related changes in drug metabolism and excretion (hepatic and/or renal insufficiency), multiple medications, and the use of CNS-active agents.
Conclusions
This work was developed to outline key elements in a clinical assessment construct that, when followed, should minimize the frequency of overlooking an underlying and potentially treatable medical illness that may be masquerading as a primary psychiatric illness, and thus avoiding delays in correct diagnosis and appropriate treatment. Formulation of a diagnosis conceptualizes the various possibilities in determining whether the clinical presentation is due to a primary psychiatric illness or a medical mimic and requires clinical vigilance as well as a structured process of evaluation. In addition to evaluating onset, duration, changes in medication use patterns, or metabolic abnormalities as part of a comprehensive assessment, clinicians are encouraged to consider (and obtain) information regarding change from the patient's baseline psychosocial functionality whenever possible. The diagnostic schema for ruling out medical mimics requires critical thinking, a multifactorial approach, clinical diligence, exclusion of infectious disease(s), metabolic disturbances, respiratory disorders, endocrine abnormalities, medications, trauma, and substance use when considering the potential for nonpsychiatric causes of the presenting symptoms, especially in the case of patients with a preexisting psychiatric illness.
The cases presented are designed to demonstrate the utility of application of a structured framework to aid patient evaluation. The case examples of myxedema demonstrate how a careful and comprehensive evaluation can aid in determining the medical etiology where psychiatric symptoms are the predominant initial presenting symptoms. In the case of delirium, the underlying cause was determined to be a UTI, and premorbid function resumed following antibiotic treatment. This case also illustrates how a potentially important lab test was not ordered, possibly leading to a delay in appropriate treatment. In the last case, a small medication change in a patient with a degenerative neurologic disorder resulted in the manifestation of psychiatric symptoms, whereby a dose reduction returned the patient to baseline psychosocial function. Improvements in diagnostic accuracy should aid in minimizing misdiagnosis and allow the patient's illness to be appropriately managed in a more timely manner.
References
- 1. Freudenreich O. . Differential diagnosis of psychotic symptoms: medical mimics. Psychiatr Times. 2010; 27: 56- 61. [Google Scholar]
- 2. Spitzer RL, First MB, Williams JB, Kendler K, Pincus HA, Tucker G. . Now is the time to retire the term “organic mental disorders”. Am J Psychiatry. 1992; 149 2: 240- 4. DOI: 10.1176/ajp.149.2.240. PubMed PMID: 1734746. [DOI] [PubMed] [Google Scholar]
- 3. Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. . Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv. 2005; 56 6: 671- 7. DOI: 10.1176/appi.ps.56.6.671. PubMed PMID: 15939942. [DOI] [PubMed] [Google Scholar]
- 4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): American Psychiatric Association; 2013. p. 487-9, 596, 708. [Google Scholar]
- 5. Reeves RR, Parker JD, Loveless P, Burke RS, Hart RH. . Unrecognized physical illness prompting psychiatric admission. Ann Clin Psychiatry. 2010; 22 3: 180- 5. PubMed PMID: 20680191. [PubMed] [Google Scholar]
- 6. Sood TR, Mcstay CM. . Evaluation of the psychiatric patient. Emerg Med Clin North Am. 2009; 27 4: 669- 83, ix. DOI: 10.1016/j.emc.2009.07.005. PubMed PMID: 19932400. [DOI] [PubMed] [Google Scholar]
- 7. Pearl PL, Weiss RE, Stein MA. . Medical mimics: medical and neurological conditions simulating ADHD. Ann N Y Acad Sci. 2001; 931: 97- 112. PubMed PMID: 11462759. [PubMed] [Google Scholar]
- 8. Zun L. . Mental health disorders: ED evaluation and disposition. In: Tintinalli J, . ed Tintinalli's emergency medicine: a comprehensive study guide. 8th ed. Chapter 286. New York: McGraw-Hill; 2015. p 1- 17.
- 9. Doebbeling CC. . Psychiatric disorders-approach to the patient with mental symptoms. In: Merck manual, professional version. Kenilworth(NJ): Merck and Co; December 2012 [cited 2016 Aug 17]. Available from: http://www.merckmanuals.com/professional/psychiatric-disorders/approach-to-the-patient-with-mental-symptoms/introduction-to-approach-to-the-patient-with-mental-symptoms
- 10. Williams N, DeBattista C. . Psychiatric disorders. In: Papadakis M, McPhee SJ, Rabow MW, . eds Current medical diagnosis and treatment 2016. Chapter 25. New York: McGraw-Hill; 2015 [cited 2016 Aug 17]. Available from: http://accessmedicine.mhmedical.com/content.aspx?bookid=1585§ionid=97194405
- 11. Keshavan MS, Kaneko Y. . Secondary psychoses: an update. World Psychiatry. 2013; 12 1: 4- 15. DOI: 10.1002/wps.20001. PubMed PMID: 23471787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bishop KM, Robinson LM, VanLare S. . Healthy aging for older adults with intellectual and development disabilities. J Psychosoc Nurs Ment Health Serv. 2013; 51 1: 15- 8. PubMed PMID: 23413456. [DOI] [PubMed] [Google Scholar]
- 13. Newcomer JW. . Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005; 19 Suppl 1: 1- 93. PubMed PMID: 15998156. [DOI] [PubMed] [Google Scholar]
- 14. Leslie DL, Rosenheck RA. . Incidence of newly diagnosed diabetes attributable to atypical antipsychotic medications. Am J Psychiatry. 2004; 161 9: 1709- 11. DOI: 10.1176/appi.ajp.161.9.1709. PubMed PMID: 15337666. [DOI] [PubMed] [Google Scholar]
- 15. Buckley PF, Miller BJ, Lehrer DS, Castle DJ. . Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009; 35 2: 383- 402. DOI: 10.1093/schbul/sbn135. PubMed PMID: 19011234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health. Rockville (MD): Substance Abuse and Mental Health Services Administration [cited 2016 Aug 17]. HHS Publication No. SMA 15-4927, NSDUH Series H-50. Available from: http://www.samhsa.gov/data/2015
- 17. Goebel JR, Compton P, Zubkoff L, Lanto A, Asch SM, Sherbourne CD, et al. Prescription sharing, alcohol use, and street drug use to manage pain among veterans. J Pain Symptom Manage. 2011; 41 5: 848- 58. DOI: 10.1016/j.jpainsymman.2010.07.009. PubMed PMID: 21256706. [DOI] [PubMed] [Google Scholar]
- 18. Sidhu KS, Balon R. . Watch for nonpsychotropics causing psychiatric side effects. Curr Psychiatr. 2008; 7 4: 61- 74. [Google Scholar]
- 19. Casagrande Tango R. Psychiatric side effects of medications prescribed in internal medicine. Dialogues Clin Neurosci. 2003; 5 2: 155- 65. PubMed PMID: 22034468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hynicka LM. . Myxedema madness: a case for short-term antipsychotics? Ann Pharmacother. 2015; 49 5: 607- 8. DOI: 10.1177/1060028015570089. PubMed PMID: 25870443. [DOI] [PubMed] [Google Scholar]
- 21. Morosán Allo YJ, Rosmarin M, Urrutia A, Faingold MC, Musso C, Brenta G. Myxedema madness complicating postoperative follow-up of thyroid cancer. Arch Endocrinol Metab. 2015; 59 4: 359- 63. DOI: 10.1590/2359-3997000000090. PubMed PMID: 26331326. [DOI] [PubMed] [Google Scholar]
- 22. Chae JHJ, Miller BJ. . Beyond urinary tract infections (UTIs) and delirium: a systematic review of UTIs and neuropsychiatric disorders. J Psychiatr Pract. 2015; 21 6: 402- 11. DOI: 10.1097/PRA.0000000000000105. PubMed PMID: 26554322. [DOI] [PubMed] [Google Scholar]
- 23. Pae CU, Marks DM, Han C, Patkar AA, Masand P. . Delirium: underrecognized and undertreated. Curr Treat Options Neurol. 2008; 10 5: 386- 95. DOI: 10.1007/s11940-008-0041-x. PubMed PMID: 18782511. [DOI] [PubMed] [Google Scholar]
- 24. Meagher DJ. . Delirium: optimising management. BMJ. 2001; 322 7279: 144- 9. PubMed PMID: 11159573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zahodne LB, Fernandez HH. . Pathophysiology and treatment of psychosis in Parkinson's disease: a review. Drugs Aging. 2008; 25 8: 665- 82. PubMed PMID: 18665659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gordon PC, Kauark RB, Costa CD, de Oliveira MO, Godinho FL, Rocha MS. . Clinical implications of the National Institute of Neurological Disorders and Stroke criteria for diagnosing psychosis in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 2016; 28 1: 26- 31. DOI: 10.1176/appi.neuropsych.15050119. PubMed PMID: 26449268. [DOI] [PubMed] [Google Scholar]
- 27. Martinez-Martin P, Leentjens AF, de Pedro-Cuesta J, Chaudhuri KR, Schrag AE, Weintraub D. . Accuracy of screening instruments for detection of neuropsychiatric syndromes in Parkinson's disease. Mov Disord. 2015; 31 3: 270- 9. DOI: 10.1002/mds.26522. PubMed PMID: 26695691. [DOI] [PubMed] [Google Scholar]
- 28. Thanvi BR, Lo TCN, Harsh DP. . Psychosis in Parkinson's disease. Postgrad Med J. 2005; 81 960: 644- 6. DOI: 10.1136/pgmj.2004.032029. PubMed PMID: 16210460. [DOI] [PMC free article] [PubMed] [Google Scholar]