Abstract
Introduction:
Primary care mental health integration (PCMHI) teams function to improve access and quality of integrative physical and mental health (MH) care through a stepped care treatment approach. The project's primary objective was to evaluate the impact a PCMHI clinical pharmacist made on treatment outcomes and interventions. The secondary objective was to assess medication adherence rates.
Methods:
An electronic medical record was used to identify PCMHI patient referrals for medication management during an 8-month period. Patients were included if they were at least 18 years old and referred for medication management of depression, anxiety, posttraumatic stress disorder, or alcohol use disorder. The scores for the Patient Health Questionnaire (PHQ-9), the Generalized Anxiety Disorder Questionnaire (GAD-7), and the Posttraumatic Stress Disorder Checklist (PCL-C) were recorded at baseline and weeks 4, 8, and 12 during treatment.
Results:
The analysis included 50 patients, which resulted in a total of 156 contacts between July 2014 and March 2015. The mean change in PHQ-9, GAD-7, and PCL-C scores at week 12 as compared to baseline were a decrease of 10 (95% confidence interval [CI], 6.2-13.8, P < .001), 8 (95% CI, 3.1-12.9, P = .006), and 14.5 (95% CI, –17.3-46.3, P = .109), respectively. A total of 336 treatment interventions were made, and the overall medication adherence rate was 82.9%.
Discussion:
Medication management, provided by a clinical pharmacist, was associated with a statistically and clinically significant improvement on several MH disorder rating scale scores.
Keywords: depression, anxiety, posttraumatic stress disorder, care management, pharmacist, primary care mental health integration
Introduction
In a given year, about 44 million Americans experience a mental health (MH) disorder episode.1 Depression was the leading cause of disability in the world, and suicide was the 10th leading cause of death in 2015. These numbers disproportionately affect the veteran population as twice as many veterans age 65 years and older have a diagnosis of major depressive disorder when compared to the general population of the same age. Additionally, the suicide rate of veterans is nearly twice that of the general population.2,3
Treatments are available for MH disorders; however, numerous barriers exist that prevent access to high-quality care. Many patients present with various symptoms, such as insomnia, fatigue, or chest pain, which can be easily misdiagnosed. The stigma associated with MH disorders often prevents patients from seeking care as well. Lastly, the lack of resources and trained providers make it difficult to obtain high-quality MH care in a timely manner.4
As a result, health care is moving toward an interprofessional approach to improve MH outcomes.4 Applying a collaborative care model to manage MH disorders may assist in meeting the growing care demands and allows nonphysician providers to improve the quality of care for patients.5-7
Extensive research has demonstrated the positive impact of integrated MH care, resulting in improved identification of MH disorders, improved rates of evidence-based treatment and patient engagement, and improved adherence to therapy. Additionally, reduced wait times and a more rapid clinical response have been shown.8-16 None of these studies included pharmacists providing medication management, which is one of the reasons for this analysis.
In 2007, the primary care mental health integration (PCMHI) service was established in Veterans Affairs medical centers (VAMCs) nationwide as a new stepped care structure targeting patients with mild-to-moderate depression, anxiety, posttraumatic stress disorder (PTSD), and alcohol use disorder (AUD). The PCMHI model includes colocated, collaborative care services and care management in which the primary care provider (PCP) and his or her team work together with the PCMHI team to deliver brief, effective MH therapies within the primary care (PC) setting.17
The capabilities of each PCMHI team vary based on the available health care professionals at the respective VAMC. The prior existing PCMHI team at the Clement J. Zablocki VAMC (ZVAMC), which was active from 2007 to 2013, consisted of a half-time MH nurse practitioner and a full-time nurse and social worker. In 2013, this team collectively saw 49 patients in 1 of the PC clinics. As a result, a PCMHI trainee team was piloted to serve this same PC clinic in hopes of reestablishing the desired vision of PCMHI and increasing visibility within the ZVAMC. This trainee team consisted of various MH trainees and trained preceptors. A MH clinical pharmacy specialist, a psychologist, and a social worker served as preceptors. The trainees included a postgraduate year 2 psychiatric pharmacy resident (clinical pharmacist), a psychology fellow, a psychology intern, and a social work student.
Patients are referred to the PCHMI team if they screen positively on the 2-question Patient Health Questionnaire or directly by the PCP, nurse, or social worker. Once referred, a warm hand-off to the PCMHI team is utilized when possible. A warm hand-off is when the PCP directly introduces the patient to the PCMHI provider at the time of the medical visit. The psychologist usually completes the initial assessment and continues to see the patient for brief therapy if warranted or refers the patient to the appropriate services, including PCMHI medication management.
Once referred to PCMHI medication management, the clinical pharmacist will work with the PCP to provide brief psychotropic medication management. The PCP will usually initiate the psychotropic medication; however, the clinical pharmacist may also prescribe psychotropic medications by utilizing his or her scope of practice. The medications managed include antidepressants, prazosin, non-controlled anxiolytics, and sleep aids as appropriate. Medication regimens will be adjusted appropriately based on MH rating scales and patient report. The brief rating scales used were the Patient Health Questionnaire (PHQ-9) for depression, the Generalized Anxiety Disorder Questionnaire (GAD-7), and the PTSD Checklist (PCL-C).18-21 After the initial visit, the clinical pharmacist conducted phone or in-person follow-up at 2, 4, 8, and 12 weeks. Once stable, as defined by scale scores, the patient's care was transferred back to the PCP or he or she was referred to specialty care if further treatment was warranted. Response was defined as a decrease in PHQ-9 or GAD-7 score by at least 5 points. Remission was defined as a PHQ-9 or GAD-7 score of 0 to 4.
The primary objective of this project was to evaluate the impact of a clinical pharmacist on treatment outcomes as measured by rating scale scores and interventions. The secondary objective was to evaluate medication adherence rates.
Methods
Project Structure
This project was exempt from institutional review board approval because it was conducted for quality improvement purposes. The retrospective chart review looked at 50 patients referred to PCMHI medication management from July 2014 to March 2015 at the ZVAMC. The electronic medical record was used to identify patients who were referred to the PCMHI team. Patients were included in the review if they were at least 18 years old and referred for medication management of mild-to-moderate depression, anxiety, PTSD, or AUD. Patients were excluded if they had a severe MH disorder or received treatment in an outpatient MH clinic at the time of the PCMHI consult. The MH disorder severity was determined by patient report, rating scale scores, and past medical history.
Data Collection
The following data was collected in Microsoft Excel (Redmond, WA): patient demographics, chief complaint, diagnosis, pertinent comorbidities, PCMHI referral date, concomitant psychotherapy, week of treatment for each PCMHI pharmacy visit, interventions made, and adherence rates. Types of interventions included medication initiation, discontinuation, or dose adjustment; adherence and administration education; medication counseling; adverse drug reaction or allergy identification; drug interaction identification and management; smoking cessation management; and referral to other services. Additionally, PHQ-9, GAD-7, and PCL-C scores were recorded.
Statistics
Statistical Package for the Social Sciences software (Chicago, IL) was used to complete statistical analysis of the data. Two-tailed Student t tests and multilevel model regressions were performed to analyze the primary outcome. The mean change was calculated from baseline rating scale scores as compared to week 4, 8, and 12 scores. Medication adherence was calculated by utilizing refill frequency and patient report. Descriptive statistics were used to analyze qualitative data.
Results
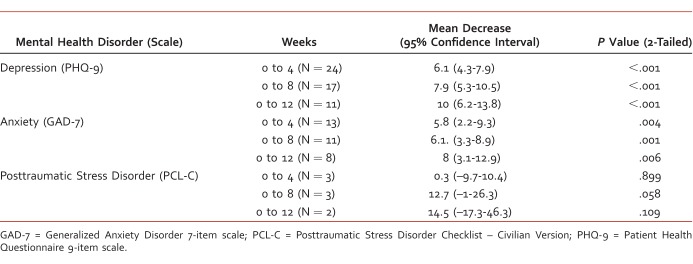
A total of 156 patients were referred to the PCMHI team. Fifty of them were medication management consults to the clinical pharmacist for depression, anxiety, or PTSD. The average age of the patients was 57 years old, and they were 100% male. A majority of the patients were referred for depression (Table 1). All 50 consults were analyzed at baseline. However, only 39 patients' medications were managed by the clinical pharmacist as 9 declined pharmacotherapy and 2 were referred to the outpatient MH clinic and psychotherapy. Of the 39 patients, 4 were lost to follow-up, 2 passed away due to non-MH-related causes, and 3 were new consults who did not have data to examine at the time of analysis. Of the 30 remaining patients, 16 were still being managed, and 14 patients were successfully transferred back to their PCP by March 2015. Twenty-four patients participated in brief therapy concomitantly, which included cognitive behavioral therapy, motivational interviewing, problem solving, goal setting, and mindfulness and relaxation. The mean total length of PCMHI medication management was 12 weeks among those transferred to their PCP.
TABLE 1.
Sample demographics
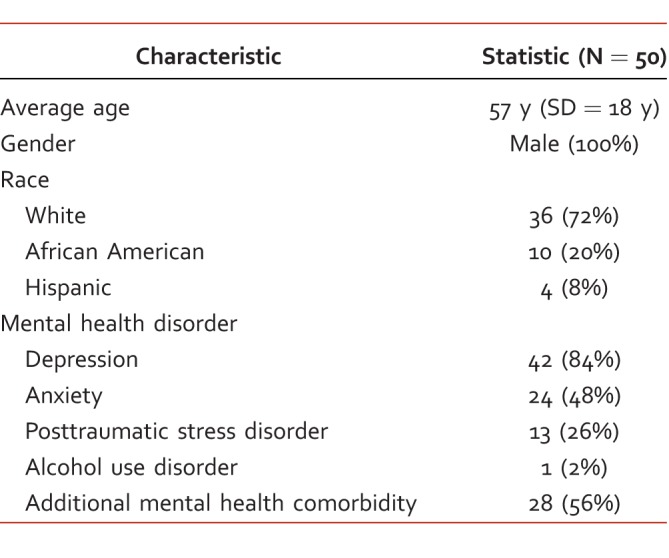
Thirty patients received at least 2 PHQ-9 assessments during follow-up, 20 received GAD-7, and 3 received PCL-C. The mean baseline PHQ-9, GAD-7, and PCL-C scores were 14 (N = 30), 11 (N = 20), and 60 (N = 3), respectively. The mean final PHQ-9, GAD-7, and PCL-C scores were 4 (N = 11), 4 (N = 8), and 45 (N = 2), respectively. The mean changes in PHQ-9 scores from baseline were a decrease of 6.1, 7.9, and 10 at weeks 4, 8, and 12, respectively (P < .001, P < .001, P < .001; Table 2). A multilevel model regression demonstrated an estimated 0.87 decrease per week in PHQ-9 score (P < .001). The mean changes in GAD-7 scores from baseline were a decrease of 5.8, 6.1, and 8 at weeks 4, 8, and 12, respectively (P = .004, P = .001, P = .006; Table 2). A multilevel model regression demonstrated an estimated 0.66 decrease per week in GAD-7 score (P < .001). The mean changes in PCL-C scores were a decrease of 0.3, 12.7, and 14.5 at weeks 4, 8, and 12, respectively (P = .899, P = .058, P = .109; Table 2).
TABLE 2.
Mean change of mental health exam scores over 12 weeks
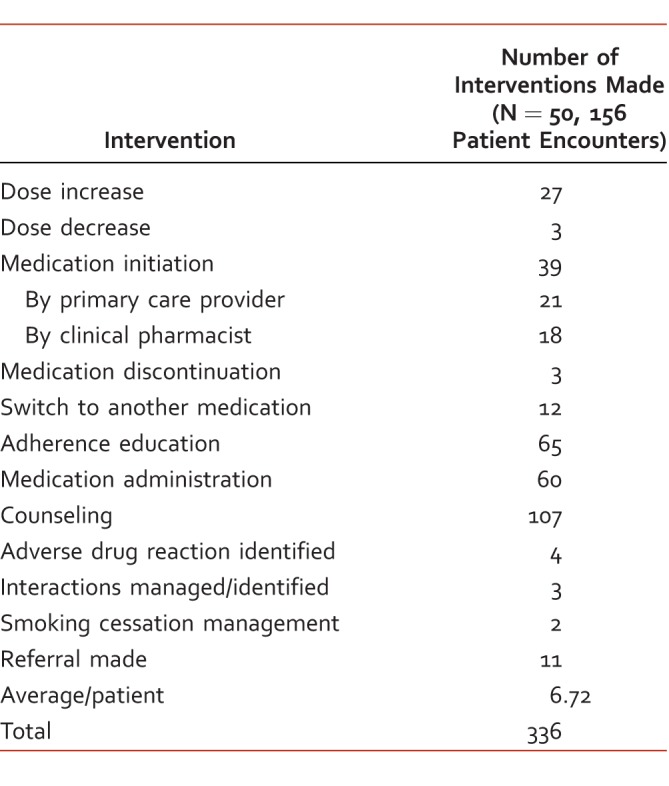
A total of 336 interventions were made over 156 patient encounters by the clinical pharmacist, which was an average of 6.72 interventions per patient. The most common interventions included medication adjustment and medication counseling (Table 3). A total of 11 referrals were made by the clinical pharmacist, which included 1 to the outpatient MH clinic, 6 to psychotherapy, 2 to couples therapy, 1 to pain psychology, and 1 to the smoking cessation clinic. Lastly, the overall medication adherence rate was 82.9% (N = 47).
TABLE 3.
Clinical pharmacist interventions
Discussion
As mentioned, 49 patients were seen by the previous PCMHI team in 2013 compared to a total of 239 patients seen by the new PCMHI trainee team in 2014 in the same clinic. Medication management, provided by a clinical pharmacist, resulted in statistically and clinically significant decreases in MH scale scores at week 12 as compared to baseline. The mean PHQ-9 and GAD-7 scores at week 12 were indicative of remission. These results were likely an outcome of the increased monitoring and frequency of patient contact. This supports previous studies that showed integrative care may assist in increasing access to brief and effective MH care.8-16 Primary care mental health integration pharmacy services offer a practical and valid method of providing medication management for mild-to-moderate MH disorders. Moreover, the use of clinical pharmacists and telephone assessments, rather than face-to-face specialty visits, led to no cost or travel for the patients. This review demonstrates that clinical pharmacists play an integral role in improvement of patient outcomes, and they should be required members of all PCMHI teams.
This project has several limitations that may affect its interpretation. It was retrospective in nature and had a short review period and a small sample size. Data collection was still in progress at the time of analysis, which may have excluded valuable data. In addition, there was no control group because the MH rating scales were not commonly utilized by PCPs or specialty clinics. All of the MH rating scales were subjective, thus introducing interpatient variability. The adherence rate calculation may have been complicated by conflicting dates of when prescriptions were filled versus mailed.
Several factors may have limited the project's generalizability. The data collected was from a single specialty program with a patient population limited to male veterans. Additionally, results may not be generalizable to women or patients with MH disorders other than depression or anxiety. It may be specifically difficult to generalize the results to patients with PTSD or AUD as the clinical pharmacist only managed a few patients with PTSD and no patients with AUD.
One of the project's strengths is its applicability to other PCMHI teams as this model may be replicated at other facilities. Also, the data and scales were collected by 1 person, which provides consistency. The project used ordinal rating scales with standardized definitions and guidelines, which minimized interviewer bias. Confounding factors were decreased by excluding individuals with severe MH disorders or those managed in an outpatient MH clinic and using multilevel model regressions to decrease the impact of confounding variables on effect estimates. Furthermore, this was an intention-to-treat analysis, which provides a conservative estimate on the clinical pharmacist's effects.
A new clinical pharmacist position was created as a result of this project's positive outcomes to assist in expanding the PCMHI services. In the future, the PCMHI pharmacy services may expand to meet additional specific MH care needs, such as AUD treatment and assistance with prazosin titration. Data will continue to be collected with the goal of expanding pharmacy involvement within PCMHI further.
Conclusion
This project supports the use of clinical pharmacists in PCMHI teams. The clinical pharmacist can make an impact by improving mild-to-moderate MH conditions, promoting interdisciplinary collaboration, and increasing documentation and follow-up that align with published treatment guidelines.
Footnotes
Disclosures: There are no actual or potential conflicts of interest by any authors of this paper.
References
- 1. Results from the 2015 National Survey on Drug Use and Health: detailed tables [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2016 [cited 2016 Jul 4]. Available from: http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm#tab8-1a
- 2. FastStats: leading causes of death [Internet]. Georgia: Centers for Disease and Control and Prevention [updated 2016 Jun 7; cited 2016 Jul 4]. Available from: http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- 3. WHO: depression [Internet]. Switzerland: World Health Organization [updated 2016 Apr; cited 2016 Jul 4]. Available from: http://www.who.int/mediacentre/factsheets/fs369/en/
- 4. Giberson S, Yoder S, Lee MP. . Improving patient and health system outcomes through advanced pharmacy practice. A report to the US Surgeon General. Rockville (MD): Office of the Chief Pharmacist, US Public Health Service; 2011. [Google Scholar]
- 5. Capoccia KL, Boudreau DM, Blough DK, Ellsworth AJ, Clark DR, Stevens NG, et al. Randomized trial of pharmacist interventions to improve depression care and outcomes in primary care. Am J Health Syst Pharm. 2004; 61 4: 364- 72. PubMed PMID: 15011764. [DOI] [PubMed] [Google Scholar]
- 6. Thomas JE, Caballero J. . Impact of pharmacists in mental health over the past decade. Ment Health Clin [Internet]. 2012; 1 10: 252- 60. DOI: 10.9740/mhc.n102274. [Google Scholar]
- 7. Fisher R, Brands A, Herrier R. . History of the Indian Health Service model of pharmacy practice: innovations in pharmaceutical care. Pharmacy in History. 1995; 37 2: 107- 22. [Google Scholar]
- 8. Oslin DW, Ross J, Sayers S, Murphy J, Kane V, Katz IR. . Screening, assessment, and management of depression in VA primary care clinics. J Gen Intern Med. 2006; 21 1: 46- 50. DOI: 10.1111/j.1525-1497.2005.0267.x. PubMed PMID: 16423122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Watts BV, Shiner B, Pomerantz A, Stender P, Weeks WB. . Outcomes of a quality improvement project integrating mental health into primary care. Qual Saf Health Care. 2007; 16 5: 378- 81. DOI: 10.1136/qshc.2007.022418. PubMed PMID: 17913780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bartels SJ, Coakley EH, Zubritsky C, Ware JH, Miles KM, Areán PA, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004; 161 8: 1455- 62. DOI: 10.1176/appi.ajp.161.8.1455. PubMed PMID: 15285973. [DOI] [PubMed] [Google Scholar]
- 11. Hedrick SC, Chaney EF, Felker B, Liu C-F, Hasenberg N, Heagerty P, et al. Effectiveness of collaborative care depression treatment in veterans' affairs primary care. J Gen Intern Med. 2003; 18 1: 9- 16. DOI: 10.1046/j.1525-1497.2003.11109.x. PubMed PMID: 12534758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Unützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002; 288 22: 2836- 45. DOI: 10.1001/jama.288.22.2836. PubMed PMID: 12472325. [DOI] [PubMed] [Google Scholar]
- 13. Zanjani F, Miller B, Turiano N, Ross J, Oslin D. . Effectiveness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatr Serv. 2008; 59 7: 776- 81. DOI: 10.1176/appi.ps.59.7.776. PubMed PMID: 18586995. [DOI] [PubMed] [Google Scholar]
- 14. Pomerantz A, Cole BH, Watts BV, Weeks WB. . Improving efficiency and access to mental health care: combining integrated care and advanced access. Gen Hosp Psychiatry. 2008; 30 6: 546- 51. DOI: 10.1016/j.genhosppsych.2008.09.004. PubMed PMID: 19061681. [DOI] [PubMed] [Google Scholar]
- 15. Guck TP, Guck AJ, Brack AB, Frey DR. . No-show rates in partially integrated models of behavioral health care in a primary care setting. Fam Syst Health. 2007; 25 2: 137- 46. DOI: 10.1037/1091-7527.25.2.137. [Google Scholar]
- 16. Alexopoulos GS, Reynolds CF 3rd, Bruce ML, Katz IR, Raue PJ, Mulsant BH, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry. 2009; 166 8: 882- 90. DOI: 10.1176/appi.ajp.2009.08121779. PubMed PMID: 19528195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Primary Care Mental Health Integration Team: Medication management referral process and follow-up procedures. Wisconsin: Clement J. Zablocki VA Medical Center; 2013.
- 18. Spitzer RL, Williams JBW, Kroenke K. . Patient Health Questionnaire (PHQ) Screeners [Internet]. New York: Pfizer Inc; 1999 [cited 2015 Feb 28]. Available from: http://www.phqscreeners.com/sites/g/files/g10016261/f/201412/PHQ-9_English.pdf
- 19. Kroenke K, Spitzer RL. . The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Ann. 2002; 32 9: 509- 15. DOI: 10.3928/0048-5713-20020901-06. [Google Scholar]
- 20. Spitzer RL, Kroenke K, Williams JBW, Löwe B. . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166 10: 1092- 7. DOI: 10.1001/archinte.166.10.1092. PubMed PMID: 16717171. [DOI] [PubMed] [Google Scholar]
- 21. Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. . The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. In: Proceedings of the 9th annual meeting of the International Society for Traumatic Stress Studies ; San Antonio, Texas; 1993.