Abstract
Introduction:
This chart review utilizes readmission rates and mean time to readmission as markers of drug efficacy to compare different categories of long-acting injectable antipsychotics (LAIAs), antipsychotic polypharmacy, and clozapine to oral antipsychotic monotherapy (OM) at a state psychiatric hospital in Oregon (Oregon State Hospital).
Methods:
Charts were reviewed for patients discharged between October 20, 2011, and September 23, 2015, with a diagnosis of schizophrenia spectrum or mood disorder. Admission dates, discharge dates, and discharge antipsychotics were reviewed for each patient dating back to 1991. Discharge antipsychotics were categorized into groupings of LAIAs, antipsychotic polypharmacy, and clozapine and compared with OM to assess readmission data within 1, 3, and 5 years of discharge. The primary end point was readmission rate, measured as a percentage, and the secondary end point was mean time to readmission (MTR), measured in days.
Results:
Of 1088 patients reviewed, there were 2031 patient discharges associated with antipsychotic agents and 1258 readmissions. Patients discharged on LAIA monotherapy or clozapine generally had a lower readmission rate, and patients discharged on antipsychotic polypharmacy generally had a higher readmission rate. Statistical significance for these findings varied over time frames and subgroup analyses. The most notable finding for the secondary end point was a significantly shorter MTR for patients discharged on clozapine for all diagnoses and the subgroup analysis of schizoaffective disorder.
Discussion:
These results are only a reflection of the patient population at this hospital, and additional reviews at other facilities with different patient characteristics could clarify applicability to other patient populations.
Keywords: psychiatric recidivism, psychiatric readmission, antipsychotic drug, antipsychotic polypharmacy, long-acting injectable antipsychotic, clozapine
Introduction
Psychiatric readmission and time between discharge and relapse are commonly used clinical markers of how well antipsychotic drugs are managing a patient's psychiatric symptoms. Antipsychotic drugs are most commonly used in schizophrenia spectrum disorders and mood disorders. Review of the literature revealed several studies that compared individual antipsychotic types but none that compared all the categories that this review addresses. In one meta-analysis, fluphenazine long-acting injectable antipsychotic (LAIA) showed significant superiority over oral antipsychotics (OAPs) for end points of relapse rate (P = .02), discontinuation due to inefficacy (P = .002), and prevention of hospitalization (P = .04), but pooled LAIAs did not significantly separate from OAPs.1 Lafeuille et al2 found that atypical LAIAs resulted in significantly lower rates of all cause hospitalizations (P < .0001), emergency department visits (P = .0158), and days in the hospital (P = .0081) as compared to OAPs. Conley et al3 found the mean time to readmission was longer for oral risperidone than clozapine, but a higher percentage of patients discharged on clozapine remained in the community at 2 years. Werneck et al4 found clozapine favorable over other second-generation antipsychotics (SGAs) for time to rehospitalization (P = .0125). The PROACTIVE study5 found no significant differences between risperidone LAIA and oral SGAs for relapse or hospitalization. The purpose of this chart review was to compare readmission rates and mean time to readmission for different categories of antipsychotic drugs in order to assess drug therapy used for the patient population served at a state psychiatric hospital in Oregon (Oregon State Hospital).
Methods
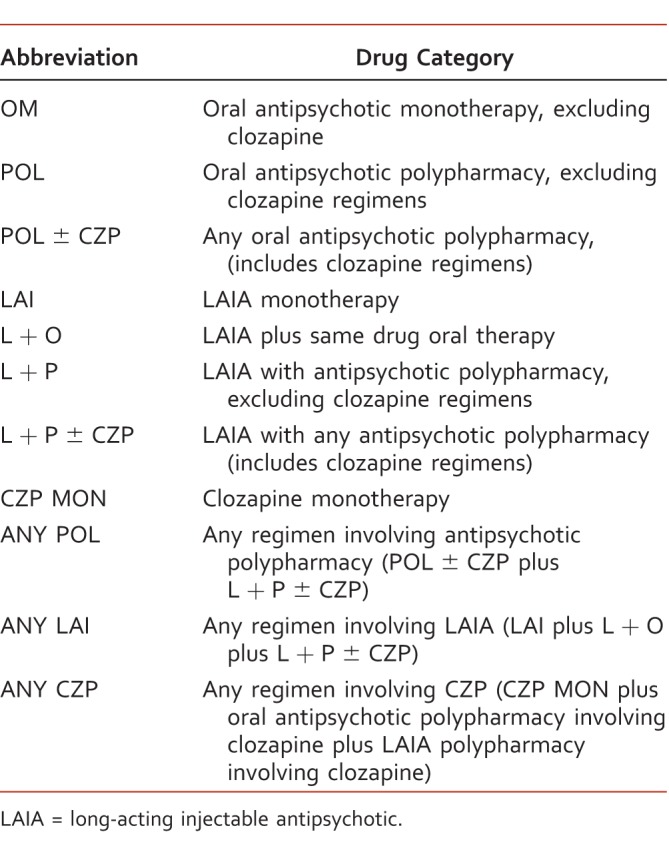
A chart review was performed for patients discharged between October 20, 2011, and September 23, 2015, with a diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, psychotic disorder not otherwise specified (NOS), delusional disorder, bipolar disorder, or mood disorder NOS. Any patient with a qualifying discharge diagnosis who was discharged on any antipsychotic was included in the review. The database had access to admission records for more than 30 surrounding hospitals. Each patient's record was reviewed for admission dates to accessible facilities, discharge dates from Oregon State Hospital, and discharge antipsychotics from Oregon State Hospital dating back to 1991. Regimens at discharge were categorized to reflect how readmission data for LAIAs, antipsychotic polypharmacy, and clozapine regimens compared with oral antipsychotic monotherapy (OM). These 3 categories were analyzed alone and in combination to assess how they affected one another when used in combination, which is commonly seen in clinical practice. The readmission data for OM was compared to the following antipsychotic drug categories, which are described in Table 1: oral antipsychotic polypharmacy, excluding clozapine regimens (POL); any oral antipsychotic polypharmacy (POL ± CZP); LAIA monotherapy (LAI); LAIA with same drug oral therapy (L + O); LAIA with antipsychotic polypharmacy, excluding clozapine regimens (L + P); LAIA with any antipsychotic polypharmacy (L + P ± CZP); and clozapine monotherapy (CZP MON). Using the same data set, a simplified scheme compared any regimen involving antipsychotic polypharmacy (ANY POL), any regimen involving a LAIA (ANY LAI), and any regimen involving clozapine (ANY CZP) to OM for each time point. Antipsychotic polypharmacy was defined as 2 or more antipsychotics, which could include any combination of oral and LAIA formulations. ANY POL included POL ± CZP and L + P ± CZP. ANY LAI included LAI, L + O, and L + P ± CZP. ANY CZP included CZP MON, oral antipsychotic polypharmacy involving clozapine, and LAIA with antipsychotic polypharmacy involving clozapine. The primary end point was readmission rate, measured as a percentage, within 1, 3, and 5 years of discharge. The readmission rate was determined by comparing the number of patients readmitted within 1, 3, or 5 years to the sum of patients readmitted and not readmitted within each time frame. The relative risk of readmission and number needed to treat or harm was calculated for each antipsychotic drug category versus OM. Many patients were readmitted more than 1 time, so each readmission was counted as an event that was not specific to each individual patient. For patients who were readmitted, the secondary end point was mean time to readmission (MTR), measured in days, for each antipsychotic drug category versus OM for 0 to 1 year, >1 to 3 years, and >3 to 5 years of discharge. A 2-sample t test assuming unequal variances with a 2-tailed P value was used to test for statistical significance. If there were less than 20 data points to analyze in a category, the results were considered statistically unacceptable. Data analysis revealed schizophrenia and schizoaffective disorder to be the most common diagnoses, so a subgroup analysis of those diagnoses was performed.
TABLE 1.
Antipsychotic drug categories and abbreviations
Results
Patient Characteristics
A total of 1088 patient charts were reviewed, resulting in 2031 patient discharges associated with antipsychotic drugs. Of these, 1258 patient discharges resulted in readmission, and 773 were not readmitted within 1, 3, or 5 years of discharge, providing an overall readmission rate of 62%. Discharge diagnoses included 797 patients with schizophrenia, 685 with schizoaffective disorder, 329 with bipolar disorder, 180 with psychotic disorder NOS, 29 with mood disorder NOS, 10 with delusional disorder, and 1 with schizophreniform disorder.
Readmission Rate
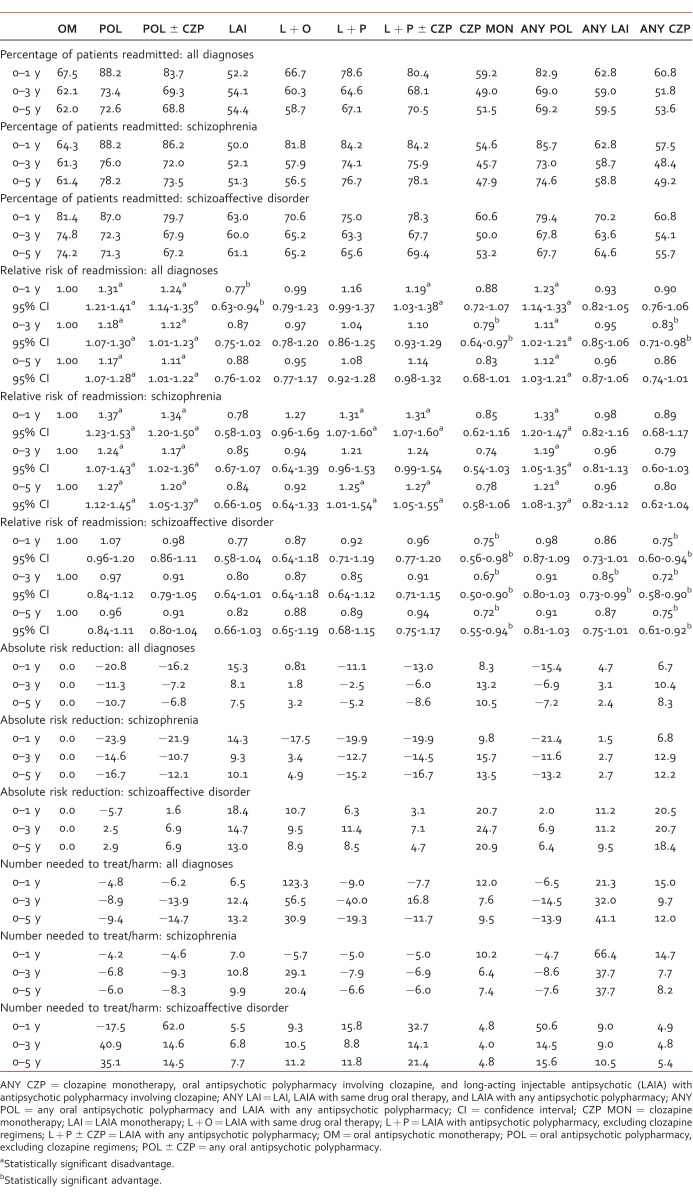
All Diagnoses
Percentage readmitted, relative risk of readmission, absolute risk reduction, and number needed to treat for each time point are outlined in Table 2. Within 1 year of discharge, patients discharged on LAI demonstrated significantly lower readmission rates than patients discharged on OM. Patients discharged on POL, POL ± CZP, L + P ± CZP, or ANY POL exhibited significantly higher readmission rates than patients discharged on OM. Although not statistically significant, CZP MON and ANY CZP demonstrated lower readmissions, and L + P exhibited higher readmissions versus OM.
TABLE 2.
Readmission rate, all diagnoses
Within 3 years of discharge, patients discharged on CZP MON or ANY CZP demonstrated significantly lower readmission rates than patients discharged on OM. Patients discharged on POL, POL ± CZP, or ANY POL exhibited significantly higher readmission rates than patients discharged on OM. LAI demonstrated a nonsignificant advantage versus OM.
Within 5 years of discharge, patients discharged on POL, POL ± CZP, or ANY POL demonstrated significantly higher readmission rates than patients discharged on OM. Although not statistically significant, LAI, CZP, and ANY CZP demonstrated an advantage and L + P ± CZP exhibited a disadvantage versus OM.
In terms of readmission rate, LAI and clozapine generally appeared to have an advantage over OM, and polypharmacy regimens appeared to be at a disadvantage to OM.
Schizophrenia
The subgroup analysis of schizophrenia revealed patients discharged on POL, POL ± CZP, or ANY POL exhibited significantly higher readmission rates versus patients discharged on OM for all time points. Patients discharged on L + P or L + P ± CZP exhibited significantly higher readmission rates within 1 year and 5 years of discharge and a nonsignificant disadvantage within 3 years of discharge. LAI, CZP MON, and ANY CZP demonstrated nonsignificant advantages versus OM (Table 2).
Schizoaffective Disorder
The subgroup analysis of schizoaffective disorder revealed patients discharged on CZP MON or ANY CZP demonstrated significantly lower readmission rates versus patients discharged on OM for all time points. Patients discharged on ANY LAI demonstrated significantly lower readmission rates within 3 years of discharge and a nonsignificant advantage within 1- and 5-year time frames. Although not statistically significant, LAI and L + O demonstrated an advantage (Table 2).
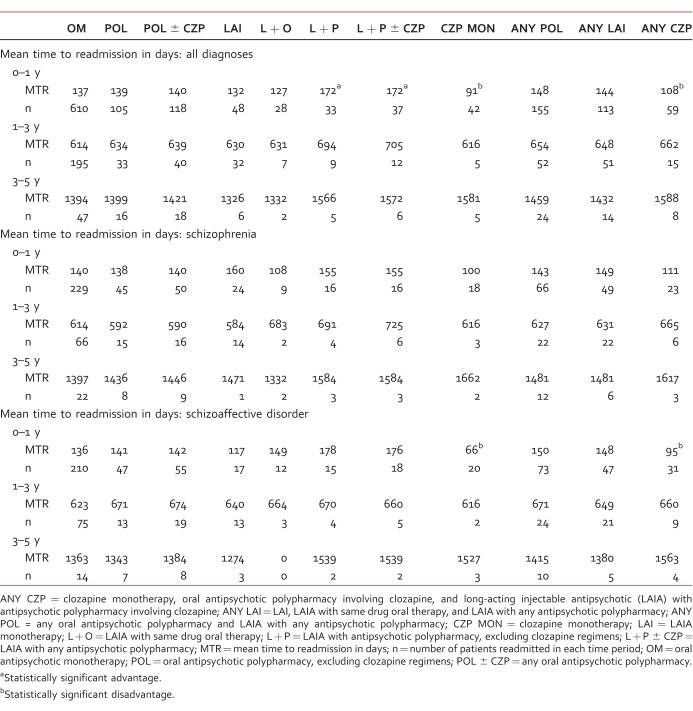
For Patients Who Were Readmitted: MTR
All Diagnoses
The data for MTR is outlined in Table 3. For patients readmitted within 1 year of discharge, patients discharged on L + P or L + P ± CZP had a significantly longer MTR than patients discharged on OM (P = .047, P = .036). Patients discharged on CZP MON or ANY CZP had a significantly shorter MTR than patients discharged on OM (P = .0025, P = .032). There were no statistically significant differences in MTR for time frames of >1 to 3 or >3 to 5 years, which is likely attributed to smaller sample sizes.
TABLE 3.
Mean time to readmission in days
Schizophrenia
There were no statistically significant differences in MTR for the subgroup analysis of schizophrenia (Table 3).
Schizoaffective Disorder
Patients discharged on CZP MON or ANY CZP had a significantly shorter MTR than patients discharged on OM within 1 year of discharge (P < .01, P = .02). There were no statistically significant differences in MTR for time frames of >1 to 3 or >3 to 5 years, which is likely attributed to smaller sample sizes (Table 3).
Discussion
Long-acting injectable monotherapy generally demonstrated lower readmission rates than OM, but statistical significance was only achieved for all diagnoses within 1 year of discharge. The MTR for patients discharged on LAI was similar to the MTR for patients discharged on OM. Overall, it appears that patients discharged on LAI are less likely to be readmitted, and if they are readmitted, the MTR is generally similar to patients discharged on OM. One potential explanation for the benefit seen could be the simplicity of the medication regimen leading to increased adherence.
CZP MON and ANY CZP generally demonstrated an advantage over OM, and statistical significance was achieved for all diagnoses within the 3-year time point and for every time point in the subgroup analysis of schizoaffective disorder. However, MTR for patients discharged on CZP MON or ANY CZP was similar to or shorter than the MTR for patients discharged on OM. It appears that patients discharged on clozapine are less likely to be readmitted, but if they are readmitted, it is generally sooner than if they were discharged on OM. The lower readmission rate could reflect clozapine's efficacy in treatment-resistant schizophrenia.6 The shorter MTR could be related to a number of factors, such as disease severity, insufficient discharge planning with respect to clozapine services in the community, difficulty in keeping lab appointments, or a drop in clozapine levels secondary to resumption of smoking upon discharge.
Antipsychotic polypharmacy regimens generally exhibited a disadvantage to OM. Statistical significance was achieved for several of the polypharmacy categories in all diagnoses and the subgroup analysis of schizophrenia but not in the subgroup analysis of schizoaffective disorder. The MTR for patients discharged on antipsychotic polypharmacy was similar to the MTR for patients discharged on OM, except for L + P or L + P ± CZP within 1 year of discharge. It appears that patients discharged on polypharmacy are more likely to be readmitted, and if they are readmitted, the MTR tends to be similar to patients discharged on OM. Possible explanations for these results could be difficulty adhering to complicated medication regimens, increased incidence of adverse effects, or greater severity of illness.
Strengths
One of the strengths of this retrospective chart review was the large data pool, which provided the ability to compare a variety of antipsychotic drug categories across several time frames, permitted assessment of long-term outcomes, and allowed for subgroup analysis of the most common disease states. Additionally, admission records were available for Oregon State Hospital and several surrounding hospitals, which allowed for greater ability to capture rehospitalizations.
Limitations
This chart review also has several limitations. An in-depth analysis of baseline patient characteristics was not performed, and there was not an equal representation of each discharge diagnosis in the data set. There was no way to ensure the antipsychotic was not changed after the patient was discharged. A number of variables that are not addressed by this review could have an impact on readmission data, including comorbid psychiatric disorders, the use of mood stabilizers, quality of discharge planning, and availability of mental health providers and services in the community. This review was performed at a single hospital in Oregon with civil and forensic patient populations, so there is limited confidence in extrapolation to other populations.
Conclusion
At Oregon State Hospital, patients discharged on LAI or clozapine were less likely to be readmitted, but statistical significance for this finding varied across time frames and subgroup analyses. Patients discharged on antipsychotic polypharmacy regimens were more likely to be readmitted, and statistical significance of this finding was fairly consistent for all diagnoses and the subgroup analysis of schizophrenia but not for the subgroup analysis of schizoaffective disorder. For mean time to readmission, the most notable finding was a significantly shorter MTR for clozapine versus oral monotherapy. These results are only a reflection of the patient population at this hospital, and additional reviews at other facilities with different patient characteristics could clarify the applicability to other populations.
Footnotes
Disclosures: The authors have no conflicts of interest to declare.
References
- 1. Kishimoto T, Robenzadeh A, Leucht C, Leucht S, Watanabe K, Mimura M, et al. . Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr Bull. 2014; 40 1: 192- 213. DOI: 10.1093/schbul/sbs150. PubMed PMID: 23256986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lafeuille MH, Laliberté-Auger F, Lefebvre P, Frois C, Fastenau J, Duh MS. . Impact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: a retrospective database analysis. BMC Psychiatry. 2013; 13: 221 DOI: 10.1186/1471-244X-13-221. PubMed PMID: 24016390; PubMed Central PMCID: PMC3847215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Conley RR, Love RC, Kelly DL, Bartko JJ. . Rehospitalization rates of patients recently discharged on a regimen of risperidone or clozapine. Am J Psychiatry. 1999; 156 6: 863- 8. DOI: 10.1176/ajp.156.6.863. PubMed PMID: 10360124. [DOI] [PubMed] [Google Scholar]
- 4. Werneck AP, Hallak JC, Nakano E, Elkis H. . Time to rehospitalization in patients with schizophrenia discharged on first generation antipsychotics, non-clozapine second generation antipsychotics, or clozapine. Psychiatry Res. 2011; 188 3: 315- 9. DOI: 10.1016/j.psychres.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 5. Buckley PF, Schooler NR, Goff DC, Hsiao J, Kopelowics A, Lauriello J, et al. . Comparison of SGA oral medications and long-acting injectable SGA: the PROACTIVE study. Schizophr Bull. 2015; 41 2: 449- 59. DOI: 10.1093/schbul/sbu067. PubMed PMID: 24870446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Novartis Pharmaceutical Corporation. CLOZARIL (clozapine) tablet [Internet]. 1989 [rev. 2015 Sept; cited 2016 Jun 20]. In: DailyMed. [33 p.]. Bethesda (MD): National Library of Medicine (US). Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5f0c6f5f-b906-4c8f-8580-3939a476a1c1