ABSTRACT
Background
Kidney transplant survival benefits are not observed for around 8 months after transplantation because of a higher complications rate in early post-transplant periods. This study compares survival of patients awaiting transplantation with survival of transplant recipients and non-listed dialysis patients in Ireland.
Methods
In this retrospective analysis, the relative-risk (RR) of death was assessed with time-dependent, non-proportional hazards analysis, with adjustment for age, cause of end-stage kidney disease (ESKD), time from first treatment for ESKD to placement on the waiting list and year of initial placement on the list.
Results
A total of 3597 patients were included. Annual death rates per 100 patient-years at risk for all patients on dialysis, waiting-list patients and transplant recipients were 16.5, 2.4 and 1.2, respectively. Death rate was highest among diabetics. The relative risk of death for all patients on dialysis was five times higher than the waiting-list patients [RR, 4.90; 95% confidence interval (CI), 3.70–6.52; P < 0.001]. Time to survival equilibration was 1 year. Thereafter, the 5-year mortality risk was estimated to be 47% lower than that of the patients on the waiting list (RR, 0.53; 95% CI, 0.37–0.77; P = 0.001).
Conclusions
Transplant recipients had a higher risk of death initially, but a better long-term survival. Time to death risk equilibration was longer compared with other studies. This could be explained by better survival rates in our waiting-list cohort.
Keywords: dialysis, kidney transplantation, mortality, survival analysis, waiting list
Introduction
Kidney transplantation remains the best available treatment for end-stage kidney disease (ESKD). When successful, transplantation reduces mortality and improves the quality of life for most patients when compared with dialysis [1–3]. However, the degree of pre-existing cardiovascular risk in kidney transplant recipients (KTR) is a major determinant of post-transplantation survival. Starting from Day 1, survival benefits are seen in patients with low and intermediate risk [4]. Unfortunately, patients with high cardiovascular risk might not see a survival benefit for a period of up to 6–12 months after having a successful kidney transplant [1, 4]. It has been shown before that patients who are on the waiting list for transplantation have a better survival compared with non-listed dialysis patients [1, 4]. The most likely explanation for this observation is that the KTR group comprises patients who were carefully selected from the dialysis population, and they likely represent the healthiest individuals compared with those who were not listed for transplantation. In fact, it has been shown, in previous studies, that dialysis patients who were on the deceased-donor kidney transplantation waiting list were usually healthier and younger than non-listed dialysis patients [5–7].
Waiting times for transplantation are on the rise and, subsequently, the burden of comorbid disease in patients awaiting transplantation is increasing. The main reason behind this is the shortage of heart-beating organs. The rate of growth of the chronic kidney disease/ESKD population has continued to increase while the transplant organs availability rate has not grown at the same pace. During the last decade, the number of adults waiting for a kidney transplant almost doubled in the USA [8]. Every year, waiting times are getting longer. Around 10 000 patients, approximately, wait for at least 11 years to receive a kidney transplant [8]. To keep up with the pace of the rapidly expanding pool of patients waiting for a kidney transplant, optimization of the use of available allografts is required. This increases pressure on many transplant centres to develop robust selection criteria to determine those patients who will benefit most from receiving a transplant. Previous studies by Wolfe et al. [1] and Gill et al. [4] have shown survival benefits of kidney transplantation in various groups of patients. In this study, we wanted to assess if it was possible to demonstrate this effect in a single transplant centre experience. Therefore, comparing the survival of KTR with the survival of patients awaiting transplantation and non-listed dialysis patients in Ireland was the main aim of this study.
Materials and methods
Study population and data source
We carried out an analysis of the National Renal Transplant Registry and the Beaumont Hospital Renal Database (Clinical Vision 3.4a Version 1.1.34.1, Clinical Computing, Cincinnati, OH, USA) from 1 January 2004 to 31 December 2013, to determine the mortality of KTR, dialysis patients on the transplant waiting list and non-listed dialysis patients. This registry is maintained prospectively by dedicated full-time staff. A total of 1538 adult renal transplants were performed during this study period. The National Kidney Transplant Centre at Beaumont Hospital has performed all adult renal transplants in Ireland since 1987 (previous transplant surgery in Ireland was performed at the Charitable Infirmary, Jervis Street, since 1964). Elderly patients with an age of ≥70 years comprised <0.5% of KTRs and hence they were excluded from this study. We also excluded patients who received a pre-emptive kidney transplant and recipients of a living-donor transplant.
Analytical methods
Analysis of survival was from the time of initial inclusion in the transplant waiting list to the time of death. We censored data when the patient received the first transplant from a living donor or on 31 December 2013. Some patients switched between the dialysis and the transplantation groups during follow-up and hence time-dependent, non-proportional hazards analysis was used to account for this switching. We calculated the number of days between inclusion in the transplant waiting list and the time at which the death rates equalized in the two groups; we calculated cumulative survival probabilities as well. Both calculations were adjusted for the time spent on the waiting list. The analyses were adjusted for age, sex, year of placement on the waiting list, time from first dialysis for ESKD to inclusion in the waiting list and the cause of ESKD. The latter was classified into subgroups of diabetes mellitus, glomerulonephritis or others. The loss of an allograft and the removal from the transplant waiting list did not exclude affected patients from the analyses. Analyses were conducted according to the intention to treat analysis. All data were analysed using STATA Version 10.0 (College Station, TX, USA). P < 0.05 was considered to be statistically significant.
Results
During the study period, 10 years, a total of 3597 patients were commenced on dialysis. Subsequently, 1157 patients were placed on the transplant waiting list, 990 received a deceased-donor kidney and 1450 were not eligible for transplantation. Mean age (standard deviation) was 46 (±15) years. Mean follow-up was 2.5 years. Baseline characteristics of the study population are shown in Table 1.
Table 1.
Characteristics of the study population
| Characteristic | All patients on dialysis | Patients on the waiting list | Deceased-donor transplant recipients | P-value |
|---|---|---|---|---|
| n = 1450 | n = 1157 | n = 990 | ||
| Age number (%) | ||||
| ≤19 years | 58 (4) | 97 (8) | 62 (6) | <0.001 |
| 20–39 years | 317 (22) | 372 (32) | 334 (34) | |
| 40–59 years | 615 (42) | 517 (45) | 436 (44) | |
| 60–70 years | 460 (32) | 171 (15) | 158 (16) | |
| Sex | ||||
| Male | 923 (64) | 751 (65) | 624 (63) | 0.646 |
| Female | 527 (36) | 406 (35) | 366 (37) | |
| Cause of ESKD | ||||
| Diabetes mellitus | 141 (10) | 66 (6) | 57 (6) | <0.001 |
| Glomerulonephritis | 214 (15) | 230 (20) | 214 (22) | |
| Others | 1095 (75) | 861 (74) | 719 (72) |
The group of patients on dialysis but not on the transplant waiting list had an annual death rate that was seven times higher than the group of patients on the waiting list. The annual death rate for patients on the waiting list was twice as high as that for KTR (Table 2). The unadjusted annual death rate per 100 patient-years at risk was 1.2 for KTRs, 2.4 for patients on the waiting list and 16.5 for all patients on dialysis (Table 2).
Table 2.
Annual death rates per 100 patient-years
| Variable | Patients on dialysis not on pool (rate per 100 patient-years) | Patients on the transplant waiting list (rate per 100 patient-years) | Recipients of deceased-donor transplants (rate per 100 patient-years) |
|---|---|---|---|
| All patients | 16.5 | 2.4 | 1.2 |
| Age (years) | |||
| 0–19 | 12.9 | 0.8 | 0.0 |
| 20–39 | 3.1 | 2.1 | 0.3 |
| 40–59 | 14.2 | 2.3 | 0.9 |
| 60–70 | 23.2 | 3.9 | 4.7 |
| Sex | |||
| Male | 16.5 | 2.5 | 1.1 |
| Female | 16.6 | 2.1 | 1.5 |
| Cause of ESKD | |||
| Diabetes | 19.0 | 5.5 | 3.8 |
| Other | 16.1 | 2.1 | 1.1 |
Compared with dialysis patients on the transplant waiting list, the relative risk of death was five times higher for patients on dialysis not on the transplant waiting list [RR, 4.90; 95% confidence interval (CI), 3.70–6.52; P < 0.001].
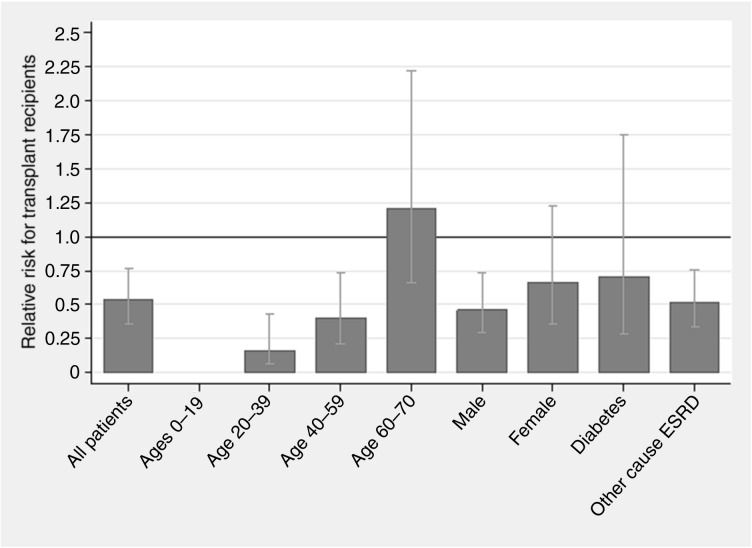
Figure 1 shows the adjusted relative risk of death among KTR, as compared with patients on the waiting list. Relative risk was adjusted for age, sex and diabetes as the cause of ESKD and other causes of ESKD. The relative risk of death was significantly lower in transplant recipients among each subgroup except for the age 60–70 years subgroup. However, the relative risk in the latter subgroup was not statistically significant.
Fig. 1.
Relative risk of death for transplant recipients compared with on-pool dialysis patients. Subgroups were classified according to age, sex and diabetes as the cause of ESKD and other causes of ESKD. The relative risk was adjusted for age, sex and diabetes as the cause of ESKD and other causes of ESKD.
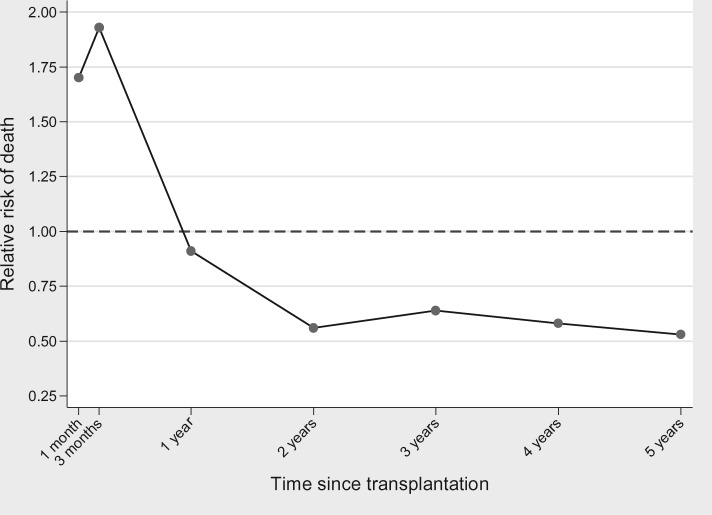
A comparison was made between KTRs and patients on the waiting list who had not yet received a deceased-donor kidney transplant, but who had equal lengths of follow-up since placement on the waiting list; patients with unsuccessful transplantation were included in this comparison. During the first 4 weeks after transplantation, the adjusted relative risk of death among the KTRs was 1.7 times higher than the risk among patients on the transplant waiting list. This risk continued to increase during the first 12 weeks and peaked at 1.9 times as high by the end of Week 12. Although this risk of death started to fall thereafter, it remained elevated until 1 year post-transplantation. After this time, the risk was lower among the KTRs (Figure 2). The 5-year mortality risk was estimated to be 47% lower than that of patients on the waiting list (RR, 0.53; 95% CI, 0.37–0.77; P = 0.001).
Fig. 2.
Adjusted relative risk of death for transplant recipients compared with on-pool dialysis patients during the first 5 years post-transplant. The reference group was the 1157 patients on dialysis who were on the transplant waiting list (RR, 1.0). Values were adjusted for age, sex cause of ESKD, year of placement on the waiting list and time from first treatment for ESKD to placement on the waiting list.
Discussion
Our analysis showed that transplantation improved survival in KTRs. In the subgroups analysis, according to age, sex and cause of ESKD, the mortality rate for all patients on dialysis was five times higher than that of patients who were on the transplant waiting list. These findings prove the fact that there is substantial selection of healthier patients for placement on the waiting list for transplantation.
The annual relative risk of death in our cohort was 1.2 per 100 patient-years for deceased-donor transplant recipients. This risk is lower compared with findings reported in previous studies [1, 3]. Wolfe et al. reported a relative risk of 3.8 in their cohort [1]. Gill et al. stratified this relative risk of death according to waiting times for transplantation [3]. They showed a risk of 4.0 per 100 patient-years for deceased-donor transplant recipients who waited for up to 36 months before transplantation. Waiting times beyond 36 months increased the risk to 5.4 [3].
Another important finding demonstrated by our study was that the relative risk of death among KTR, who received their first transplant, relative to that among patients on the transplant waiting list varies significantly with time. Mortality was higher in the transplantation group immediately after transplantation. This finding was demonstrated in previous studies [1, 4]. The leading cause of death during the early post-transplantation period is cardiovascular disease [9]. Previous studies have shown the importance of optimizing the management of cardiovascular risk factors in wait-listed patients by coordination between nephrologists and transplant teams [10]. Unfortunately, so far no studies have shown a strategy or an intervention to reduce cardiovascular mortality during the early post-transplant period [11]. Other important causes of high mortality in the early post-transplantation period are complications of surgery and effects of immunosuppression medications at high doses. Subsequently, the risk of death decreased and the survival benefit began to be observed (time to equal survival) 365 days after transplantation. In comparison with our findings, Wolfe et al. demonstrated a shorter time to equal survival, i.e. 244 days [1]. We think the most likely explanation for this difference is that our waiting list, i.e. patients in Ireland, are healthier compared with their counterparts in USA, because of the stringent criteria used for inclusion into the kidney transplant pool in Ireland. This long-term improvement in survival was significant for all patients’ subgroups, when compared with the survival rate among corresponding dialysis patients on the transplant waiting list. The excess early mortality after transplantation remains an important consideration that should be addressed adequately when counselling potential transplant recipients.
Both Wolfe et al. and Gill et al. showed that elderly transplant recipients' survival benefits from transplantation when compared with dialysis patients on the transplant waiting list [1, 4]. We found that transplant recipients with ages 60–70 years had a higher risk of death by 1.2 times than those on the transplant waiting list. However, this finding was not statistically significant. Gill et al. showed that the time to equal survival was 521 days and 470 days for elderly recipients of a deceased-donor kidney transplant, with high cardiovascular risk and low cardiovascular risk, respectively [4]. Schaeffner et al. demonstrated that only 7% of patients who are ≥65 years of age are transplanted after 3 years of initiating dialysis [12]. Schold et al. showed that the 5-year probability of deceased-donor transplantation in patients aged ≥65 years is nearly equal to the probability of death on the waiting list [13]. This reflects the importance of longer follow-up periods, where the survival benefit in the elderly becomes more apparent in subsequent years following transplantation. In contrast to this, the survival of elderly dialysis patients on the waiting list reduces significantly year after year. Therefore, a short follow-up period might be misleading when comparing the elderly patients’ survival, and might show a better survival in the waiting-list cohort than in transplant recipients. Additionally, Gill et al. demonstrated that, in low cardiovascular risk patients, living-donor kidney transplantation was associated with an immediate survival advantage compared with dialysis [4].
Our study has a number of strengths. Generally, in this study, we employed similar methods to those used by Wolfe et al. [1]. An important strength is that we used an intention to treat analysis and hence mortality post-transplantation assessment was independent of allograft function. This type of analysis also allows comparison of KTRs with patients on the transplant waiting list who had equal lengths of time on the waiting list. This approach and methodology have previously been used in other studies [1, 14–16]. The estimation of time to equal risk and equal survival in this study was determined in KTRs compared with similar risk patients who remained on the waiting list, and differs from that in the study done by Merion et al. [17]. In their study, the outcomes after Extended Criteria Donor transplantation were compared with continued waiting on the transplant waiting list and transplantation from a standard criteria deceased donor. As a result, the times to equal risk and equal survival among Extended Criteria Donor recipients are longer than those among KTRs in this study. We adjusted for the year of placement on the transplant waiting list and the interval between placement on the transplant waiting list and transplantation; this helped to minimize the potential effects of outcomes improvement over time.
This study has some limitations. Firstly, we did not study the use of transplants from living donors, although it has a better outcome than deceased-donor transplantation [18, 19]. Secondly, although our multivariate analyses were adjusted for differences in a variety of factors that impact transplant outcome, there are undoubtedly unaccounted differences between standard and Extended Criteria Donor recipients in this study that may confound our findings. Thirdly, despite including a reasonable number of transplant recipients in Ireland, the results may be difficult to apply to individual patients. Fourthly, in the last two decades, both short- and long-term survival have been improving for patients on dialysis and transplant recipients [20], and this could affect our results. Finally, limitations of observational studies and secondary analyses of registry data cannot be overlooked when appraising this study.
In conclusion, this study, based on Irish data, shows that dialysis patients who were on the transplantation waiting list had a better survival when compared with dialysis patients who were not listed. First-time KTRs, who received a deceased-donor kidney transplant, had a higher risk of death initially when compared with dialysis patients who remained on the transplant waiting list, but their long-term survival was better. Time to equal survival was longer compared with other studies; this could be explained by better survival rates in our waiting list cohort. However, this excess early mortality after transplantation remains an important consideration that should be addressed adequately when counselling potential transplant recipients about transplantation.
Acknowledgements
The authors thank Cathal Collier for the great effort he put into the National Renal Transplant Registry and the Beaumont Hospital Renal Database, which made this study possible. No support or funding was used for this submission.
Conflict of interest statement
None declared.
References
- 1. Wolfe R, Ashby V, Milford E. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first deceased-donor transplant. N Engl J Med 1999; 341: 1725–1730 [DOI] [PubMed] [Google Scholar]
- 2. Laupacis A, Keown P, Pus N. et al. A study of the quality of life and cost-utility of renal transplantation. Kidney Int 1996; 50: 235–242 [DOI] [PubMed] [Google Scholar]
- 3. Gill JS, Tonelli M, Johnson N. et al. The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int 2005; 68: 2345–2351 [DOI] [PubMed] [Google Scholar]
- 4. Gill JS, Schaeffner E, Chadban S. et al. Quantification of the early risk of death in elderly kidney transplant recipients. Am J Transplant 2013; 13: 427–432 [DOI] [PubMed] [Google Scholar]
- 5. Gaylin DS, Held PJ, Port FK. et al. The impact of comorbid and sociodemographic factors on access to renal transplantation. J Am Med Assoc 1993; 269: 603–608 [PubMed] [Google Scholar]
- 6. Held PJ, Pauly MV, Bovbjerg RR. et al. Access to kidney transplantation: has the United States eliminated income and racial differences? Arch Intern Med 1988; 148: 2594–2600 [DOI] [PubMed] [Google Scholar]
- 7. Kasiske BL, London W, Ellison MD.. Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. J Am Soc Nephrol 1998; 9: 2142–2147 [DOI] [PubMed] [Google Scholar]
- 8. Matas AJ, Smith JM, Skeans MA. et al. OPTN/SRTR 2013 annual data report: kidney. Am J Transplant 2015; 15: 1–34 [DOI] [PubMed] [Google Scholar]
- 9. Gill JS, Pereira BJ.. Death in the first year after kidney transplantation: Implications for patients on the transplant waiting list. Transplantation 2003; 75: 113–117 [DOI] [PubMed] [Google Scholar]
- 10. Gill JS, Rose C, Pereira BJ. et al. The importance of transitions between dialysis and transplantation in the care of end-stage kidney disease patients. Kidney Int 2007; 71: 442–447 [DOI] [PubMed] [Google Scholar]
- 11. Lentine KL, Hurst FP, Jindal RM. et al. Cardiovascular risk assessment among potential kidney transplant candidates: approaches and controversies. Am J Kidney Dis 2010; 55: 152–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schaeffner ES, Rose C, Gill JS.. Access to kidney transplantation among the elderly in the United States: a glass half full, not half empty. Clin J Am Soc Nephrol 2010; 5: 2109–2114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schold J, Srinivas TR, Sehgal AR. et al. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol 2009; 4: 1239–1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mauger EA, Wolfe RA, Port FK.. Transient effects in the Cox proportional hazards regression model. Stat Med 1995; 14: 1553–1565 [DOI] [PubMed] [Google Scholar]
- 15. Port FK, Wolfe RA, Mauger EA. et al. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. J Am Med Assoc 1993; 270: 1339–1343 [PubMed] [Google Scholar]
- 16. Ojo AO, Port FK, Wolfe RA. et al. Comparative mortality risks of chronic dialysis and cadaveric transplantation in black end-stage kidney disease patients. Am J Kidney Dis 1994; 24: 59–64 [DOI] [PubMed] [Google Scholar]
- 17. Merion RM, Ashby VB, Wolfe RA. et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. J Am Med Assoc 2005; 294: 2726–2733 [DOI] [PubMed] [Google Scholar]
- 18. Ojo AO, Port FK, Mauger EA. et al. Relative impact of donor type on renal allograft survival in black and white recipients. Am J Kidney Dis 1995; 25: 623–628 [DOI] [PubMed] [Google Scholar]
- 19. Terasaki PI, Cecka JM, Gjertson DW. et al. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med 1995; 333: 333–336 [DOI] [PubMed] [Google Scholar]
- 20. United States Renal Data System. 2014 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2014, https://www.usrds.org/2014/view/Default.aspx (22 November 2016, date last accessed)