Abstract
Root resorption has been the subject of many studies, and it can be caused by many factors such as the mechanics used during orthodontic treatment, factors related to the type and magnitude of the force, and other factors related to treatment such as the type of tooth movement and malocclusion. The clinical importance of root resorption is directly related to its detectability. Therefore, orthodontic and biological factors that may cause root resorption were evaluated using various imaging methods in present use. In this review, root resorption in orthodontics was considered from different viewpoints.
Keywords: Orthodontics, root resorption
INTRODUCTION
Root resorption is a pathological and physiological process that results in the loss of the cementum and dentine (1).
History of Root Resorption
Root resorption was first described by Bates in 1856. Chase in 1875 and Harding in 1878 also mentioned root resorption. In 1914, the term was used in orthodontic literature. Bates referred to root resorption as absorption (1, 2). Ketcham (3) was the first author who explained root resorption with radiology. Following Ketcham, when it was found that orthodontic treatment could shorten the roots, interest in this subject increased. Becks and Marshall brought the word “resorption” into orthodontic literature in 1932. Oppenheim stated in 1944 that following orthodontic treatment, there was inevitable damage in the cementum, periodontal tissues, alveolar bone, and pulp (2).
Histopathology of Root Resorption
Root resorption in orthodontics is referred to as induced inflammatory resorption, and it is a form of pathological root resorption, in which orthodontic forces are transferred to the teeth and hyalinized areas are thus removed in the periodontal area. During the removal of hyalinized tissues, the cementum is also removed. The resorption process is initiated by dentinoclasts. Osteoclast-like cells referred to as odontoclasts caused resorption. They have a pleomorphic shape and are usually multinuclear (2, 4).
Etiology of Root Resorption
The dental history, history of trauma and dental treatments, related systemic conditions, and medical details of patients could cause the pathogenesis of root resorption. While the multifactorial etiology of root resorption is very complex, it is thought that a combination of the biological variability of a person, genetic predisposition, and mechanical factors are the reason for resorption (5). In line with many studies on the etiology of root resorption, the possible reasons for root resorption can be classified as follows:
Factors related to orthodontic treatment
These include the magnitude of orthodontic force, type of force (continuous, interrupted, or intermitted), direction of tooth movement, amount of apical movement, sequence of the arch wire, type of orthodontic appliance, duration of orthodontic treatment, and treatment technique.
Factors related to the patient
These include genetic factors, chronological age, dental age, gender, ethnic factors, syndromes, psychological stress, increased occlusal force, tooth vitality, type of teeth, dental invaginations, features of dentoalveolar and facial structures, existing root resorption before treatment, proximity of the root to the cortical bone, nutrition, systemic factors (illnesses that cause inflammation, asthma, allergy, etc.), hormonal irregularities, systemic medicine use, metabolic skeletal disorders, parafunctional habits, morphology of teeth/root, developmental abnormalities of roots, properties of cementum mineralization, hypofunction of the periodontium, history of trauma, endodontic treatment, density of the alveolar bone, and type and severity of malocclusion and alcoholism.
Factors related to orthodontic treatment
While Jacobson (6) stated that a 1-mm loss in the apex is not important because the apical region has the smallest diameter in a tooth, Kalkwarf et al. (7) mentioned that there can be an important relationship between the length of the root and periodontal connection; thus, even the smallest loss in the root can be significant.
Magnitude of orthodontic force
Harris et al. (8), Barbagallo et al. (9), Cheng et al. (10), and Paetyangkul et al. (11) stated that with an increasing force, root resorption also increases. Paetyangkul et al. (11) concluded that even if a light force was applied, whenever there is an increase in the application time, root resorption also increases.
Type of orthodontic force
Although it is clinically difficult to apply intermittent forces in fixed orthodontic treatment, it has been suggested that intermittent forces should be preferred instead of continuous forces to prevent serious root resorptions (12). Aras et al. (13) concluded that intermittent forces result in lesser root resorption than continuous forces.
Direction of tooth movement
According to the type of movement, high points of pressure, where the force is intensified, are more prone to root resorption. In intrusive movements, almost all pressure is gathered in the root apex; the risk of resorption markedly increases because of root anatomy (14). When compared with intrusive movements, extrusive movements occur easily, but they also cause root resorption in interdental areas in the cervical third of the root. It has been stated that root resorption occurs four times more during intrusion than during extrusion (15).
The most detrimental orthodontic movement that may induce root resorption is the combination of lingual root movement with intrusion (16). Li et al. (17) evaluated the amount of root resorption after mini-screw-supported molar intrusion and stated that the most volumetric material loss occurs in the mesiobuccal root. During rotation, resorption lacunae are mostly prevalent in the middle third of the root (18).
Amount of apical movement
While it has been stated that an increase in apical movement can lead to an increase in resorption (19), according to Philips (20), there was no direct relationship between root resorption and the sagittal or angular movements of the root apex.
Sequence of the arch wire
There is no information on the relationship between root resorption and the arch wire sequence. The arch wire sequence is mostly a clinician-dependent factor. A significant relationship between resorption and the arch wire sequence has not been proven (21). This is important because the aim of the clinician is to reach the square stainless steel working arch wires efficiently. However, a balance should exist between the potential benefits of a more rapid progression to working wires and risks of root resorption.
Type of orthodontic appliance
It has been found that the mean decrease in root length was 8.2% in the straight wire group and 7.5% in the conventional edgewise group. There was no a significant difference between the mean prevalence of apical root resorptions between the two groups (22). Scott et al. (23) stated that the amount of root resorption in Damon-3 self-ligating braces and brackets and conventional brackets are similar. In their prospective randomized controlled clinical trial, Barbagallo et al. (9) found that the amount of resorption in thermoplastic removable appliances is similar with light forces transmitted by fixed orthodontic appliances. It has also been found that the use of Class II elastics might be a risk factor for root resorption.
Heavy forces during rapid maxillary expansion might also induce root resorption in attached premolars and molars. Further, there are studies that have found that rapid expansion might induce root resorption in the unattached second premolar tooth (24).
Factors related to the patient
Genetic factors
The resorption process, which may vary among patients and cannot be explained either by orthodontic or environmental factors, has led researches to evaluate the presence of genetic factors that may increase the tendency for resorption (25). Significant differences in root resorption between patients, even in situations where factors related to the treatment and clinician are standardized, reveal the importance of personal tendency. Error! Reference source not found. There are studies inferring that personal tendency on root resorption may be more effective than the amount and duration of orthodontic force (26).
Abnormal root morphology
The geometrical forms of roots can affect the distribution of the force through the alveolar bone and root. The force is more concentrated on localized areas in trigonal sharp apexes than in roots with a normal shape. Generally, teeth with root dilacerations are prone to root resorption, particularly in maxillary lateral incisors (27).
Endodontic treatment
There are several studies that have reached different conclusions on the effect of endodontic treatment on root resorption. However, the lack of studies evaluating the relationship between root resorption and endodontic treatment in vivo is clear (28). It has been suggested that pulpal neuropeptides play a role in root resorption. The main idea is that less root resorption occurs due to the removal of red blood cells with endodontic treatment Some authors have stated that filling the root canal with calcium hydroxide might be effective in inhibiting root resorption (28). Esteves et al. found a 0.2-mm difference in root resorption between teeth with endodontic treatment and symmetric vital teeth. Mirabella and Artun (29) found a 0.45-mm difference, and Spurrier et al. (30) found a 0.77-mm difference. However, authors have also mentioned that these little differences cannot be clinically detected.
Hypofunction of the periodontium
The hypofunction of teeth during static or dynamic occlusal relationships may result in atrophic changes in Sharpey’s fibers, a decrease in the fibroblastic proliferation activity, and vascular constriction. Further, the periodontal space narrows, and the force becomes concentrated in pressure areas (31). These histological changes accelerate the resorption/destruction process. Motokawa et al. (32) found that the prevalence of root resorption in hypofunctional teeth (66.9%) is higher than that in normal teeth (33.5%).
Chronological age
The risk of root resorption increases with age because of a decrease in periodontal membrane vascularity and an increase bone density (2). On the other hand, Cheng et al. (10) and Baumrind et al. (33) stated that there is no significant relationship between the chronological age and root resorption.
Visualization and Diagnosis of Root Resorption
Even if the direction and amount of the orthodontic force are carefully determined, it is not possible to predict where and how root resorption occurs (34). For this reason, while surface resorptions are located in buccal, palatal/lingual, mesial or distal areas in the apical region, a decrease in root length may not be observed. In such situations, two-dimensional methods can be insufficient to diagnose and locate resorption. With an increase in the duration and amount of the orthodontic force, the depth of resorption lacunae may proceed to the dentine, while there is no change in the root length (35).
Root resorption after orthodontic treatment was examined for many years with conventional radiographs (periapical graphs, digital radiography, orthopantomography, and lateral cephalometric radiography), light microscopes, and scanning electron microscopes. Recently, computed tomography (CT) and micro-CT were prevalent, and later on, cone-beam CT (CBCT) has come to the forefront.
Conventional Radiological Evaluations
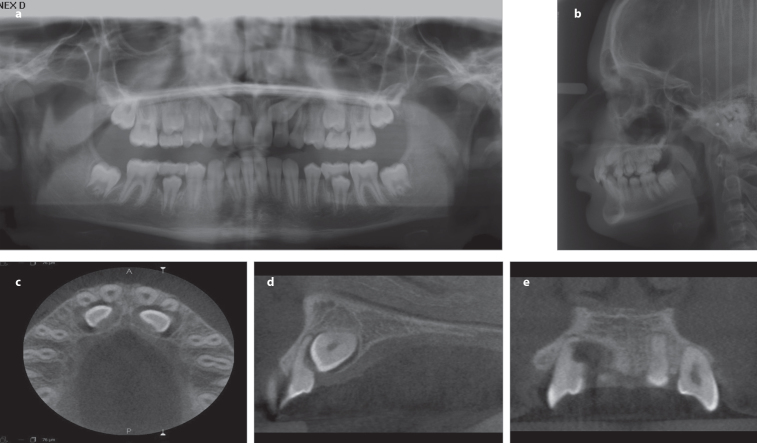
Although shortening of the root length might be detected with conventional methods, the location, depth, and width of resorption in different parts of the root cannot be detected or measured (Figure 1 a, b).
Figure 1.
Two dimensional and three dimensional images of a patient. The evaluation of lateral incisor roots using ortopantomograph or lateral cephalograph in detail is difficult because of the superimposition of the canines on the lateral incisor roots. The length and the shape of the roots cannot be assessed clearly as well. Root length of the laterals can be considered as they are within the normal levels (a, b); the 3D images of the same patient demonstrate the root surface material loss without decrease in root length in three planes of the space which affect the diagnosis and treatment planning (c–e)
The reliability of the results of several studies might doubtful due to the magnification problems of two-dimensional radiographs (36). Surface root resorptions can only be detected with two-dimensional methods in situations where the depth of resorption lacunae increases at a certain level (37). Normal anatomic formations can be seen as radiopaque or radiolucent shadows, and as a result of superimpositions, there can be a decrease in the diagnostic quality of images. To clearly evaluate the root of teeth that are lingually or buccally inclined, the clear and absolute positioning of teeth along the focal spot is very difficult (36). According to evaluations made using OPG by Sameshima and Asgarifar (37), there was a 20% or more material loss in the root compared to evaluations using periapical graphics because the position of the focal spot in accordance with the root was different between these two imaging methods.
The most important factor to be considered when evaluating root resorption with periapical graphs is the repeatability of the position between an X-ray and the tooth. If the position of the X-ray cannot be reproduced, it is not possible to perform a reliable and accurate quantitative analysis (36). The magnification factor is generally less than 5% in periapical graphs. Therefore, periapical films are superior to panoramic graphs as periapical graphs can provide detailed information with less distortion.
A magnification factor that may vary between 5% and 12% should be considered while performing evaluations with lateral cephalometric X-rays. Because the roots of central incisors are superimposed, the reliability decreases, and it is difficult to accurately visualize root resorption (36).
It is possible to perform evaluations with the same sensitivity with periapical graphs and with a less radiation dose with digital radiographs (38). Some studies have stated that digital radiographs are more sensitive than conventional radiographs when determining root resorptions (39).
Chan and Darendeliler (40) stated that two-dimensional views during the diagnosis of root resorption is a good technique; however, a quantitative evaluation for resorption should be avoided using these techniques.
Serial Sectioning and Light Microscopy
Resorption craters can vary in size and depth. Therefore, irregular C-form craters and/or small craters can be partially or completely overlooked or miscalculated. Differences in teeth morphologies in the first premolar tooth that are constantly used at root resorption studies and changes in root numbers can be challenging during cross-sectioning, and it is difficult to make an ideal longitudinal cross-sectioning without any data loss along the long axis of the teeth. Apical resorptions or resorptions in the middle third of the root cannot be noticed (40).
Scanning Electron Microscopy
It has been reported that Scanning Electron Microscopy (SEM) results in an enhanced visual and perspective assessment of root surfaces and that when recorded in stereo pairs, they provide resolution and details that cannot be attained with histological models reconstructed from serial sections (40). A study that examined root resorption with SEM calculated resorption craters with surface signs obtained from micrographs (41). However, it is very difficult to obtain a plain image without data loss as premolar teeth in particular have curved root surfaces. Therefore, mistakes can occur during the calculations.
Micro-CT
Root resorption is essentially characterized by volumetric material loss, and the localization of lacunae on the root is changeable. The volumetric three-dimensional methods used during diagnosis and the quantitative measures of root resorption can provide more accurate results than those obtained using either quantitative or semi-quantitative two-dimensional methods (42). Micro-CT, when compared with other methods, has a resolution as high as 3 μm. For this reason, micro-CT in three-dimensional dental assessments is regarded as a reference method (8). With this method, root resorption can be measured or detected only in in vitro conditions, and to obtain high-resolution images in vivo, high radiation levels are required (8). This restricts the use of micro-CT images in vivo.
Cone Beam Computed Tomography
Cone beam computed tomography was developed for viewing the maxillofacial region, and it also caused a paradigm shift from two-dimensional methods to three-dimensional methods (43) (Figure 1 c–e).
When compared with conventional CT, the advantages in using CBCT are that it can take images with lower doses, has a shorter scan time, and has an improved image sharpness (44). Further, when compared with micro-CT, one of the most significant advantages is that it can be used in in vivo assessments. This situation is not a routine procedure in each patient; however, in accordance with “to obtain the best image with the minimal dose,” CBCT comes to the forefront in terms of related indications.
Dudic et al. (45) used CBCT to determine and measure root resorption; however, they could not pave the way to perform a real three-dimensional assessment with linear measurements instead of volumetric assessments. CBCT is used to determine resorption cavities, but there are few studies revealing material loss in the root by volumetric calculations (24). Because CBCT is reliable in volumetric calculations of the teeth (46), it can be used to measure root resorption.
Repair of root resorption
It is thought that active orthodontic forces have an important role in the continuity of root resorption; therefore, the repair process begins after the release of the orthodontic force or decrease in the magnitude of the force at a certain level. The repair is first observed around the resorption lacunae. This process shows similarity to the early cementogenesis during the development of the teeth (47). Resorption lacunae are recovered with the accumulation of new cementum and formation of a new periodontal ligamentum (48). Owmann-Moll et al. (49) stated that the possible repair level in resorption cavities that can be histologically observed can be summarized as follows:
Partial Repair: Part of the surface of the resorption cavity is covered with reparative cementum (cellular or acellular cementum).
Functional Repair: The total surface of the resorption cavity is covered with reparative cementum without the re-establishment of the original root contour (cellular cementum).
Anatomic Repair: The total surface of the resorption cavity is covered with reparative cementum to an extent such that the original root contour is re-established.
Cheng et al. (10) found that resorption continued for 4 weeks after the stop of the orthodontic force. After four-week light force application which was followed by 4-week retention, there was continuous and regular repair, while most of the repair occurred where the heavy force was applied in 4 weeks, which was followed by the 4-week retention.
CONCLUSION
The etiology of root resorption associated with orthodontic therapy is complex. Several factors, alone or in combination, may contribute to root resorption. Root resorption may compromise the continued existence and functional capacity of the affected tooth, depending on its magnitude. However, the process of root resorption during orthodontic treatment is usually smooth and stops when the force is removed. In this review, root resorption was discussed from different viewpoints.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.D.; Design - F.D.; Supervision - F.D., S.D.; Resources - F.D.; Materials - F.D.; Data Collection and/or Processing - F.D.; Analysis and/or Interpretation - F.D., S.D.; Literature Search - F.D.; Writing Manuscript - F.D.; Critical Review - F.D., S.D.; Other - F.D., S.D.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Ramanathan C, Hofman Z. Root resorption in relation to orthodontic tooth movement. Acta Medica (Hradec Kralove) 2006;49:91–5. [PubMed] [Google Scholar]
- 2.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–46. doi: 10.1016/S0889-5406(05)81763-9. https://doi.org/10.1016/S0889-5406(05)81763-9. [DOI] [PubMed] [Google Scholar]
- 3.Ketcham AH. A preliminary report of an investigation of apical root resorption of permanent teeth. Int J Orthod. 1927;13:97–127. https://doi.org/10.1016/s0099-6963(27)90316-0. [Google Scholar]
- 4.Vlaskalic V, Boyd RL. Root resorptions and tissue changes during orthodontic treatment. In: Bishara SE, editor. Textbook of orthodontics. W B Saunders Co.; Philadelphia: 2001. pp. 463–72. [Google Scholar]
- 5.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–76. doi: 10.1016/j.ajodo.2009.06.021. https://doi.org/10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson O. Clinical significance of root resorption. Am J Orthod. 1952;38:687–96. https://doi.org/10.1016/0002-9416(52)90206-6. [Google Scholar]
- 7.Kalkwarf KL, Krejci RF, Pao YC. Effect of apical root resorption on periodontal support. J Prosthet Dent. 1986;56:317–19. doi: 10.1016/0022-3913(86)90011-9. https://doi.org/10.1016/0022-3913(86)90011-9. [DOI] [PubMed] [Google Scholar]
- 8.Harris DA, Jones AS, Darendeliler MA. Physical properties of root cementum: part 8. Volumetric analysis of root resorption craters after application of controlled intrusive light and heavy orthodontic forces: a microcomputed tomography scan study. Am J Orthod Dentofacial Orthop. 2006;130:639–47. doi: 10.1016/j.ajodo.2005.01.029. https://doi.org/10.1016/j.ajodo.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 9.Barbagallo LJ, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: Part 10. Comparison of the effects of invisible removable thermoplastic appliances with light and heavy orthodontic forces on premolar cementum. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2008;133:218–27. doi: 10.1016/j.ajodo.2006.01.043. https://doi.org/10.1016/j.ajodo.2006.01.043. [DOI] [PubMed] [Google Scholar]
- 10.Cheng LL, Turk T, Elekdağ-Türk S, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: Part 13. Repair of root resorption 4 and 8 weeks after the application of continuous light and heavy forces for 4 weeks: a microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:320.e321–310. doi: 10.1016/j.ajodo.2008.05.014. https://doi.org/10.1016/j.ajodo.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Paetyangkul A, Türk T, Elekdağ-Türk S, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: part 14. The amount of root resorption after force application for 12 weeks on maxillary and mandibular premolars: a microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:492.e491–499. doi: 10.1016/j.ajodo.2009.03.008. https://doi.org/10.1016/j.ajodo.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Ballard DJ, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: part 11. Continuous vs intermittent controlled orthodontic forces on root resorption. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:8.e1–8. doi: 10.1016/j.ajodo.2007.07.026. https://doi.org/10.1016/j.ajodo.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 13.Aras B, Cheng LL, Turk T, Elekdag-Turk S, Jones AS, Darendeliler MA. Physical properties of root cementum: part 23. Effects of 2 or 3 weekly reactivated continuous or intermittent orthodontic forces on root resorption and tooth movement: a microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2012;141:e29–37. doi: 10.1016/j.ajodo.2011.07.018. https://doi.org/10.1016/j.ajodo.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Beck BW, Harris EF. Apical root resorption in orthodontically treated subjects: analysis of edgewise and light wire mechanics. Am J Orthod Dentofacial Orthop. 1994;105:350–61. doi: 10.1016/S0889-5406(94)70129-6. https://doi.org/10.1016/S0889-5406(94)70129-6. [DOI] [PubMed] [Google Scholar]
- 15.Han G, Huang S, Von den Hoff JW, Zeng X, Kuijpers-Jagtman AM. Root resorption after orthodontic intrusion and extrusion: an intraindividual study. Angle Orthod. 2005;75:912–18. doi: 10.1043/0003-3219(2005)75[912:RRAOIA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Parker RJ, Harris EF. Directions of orthodontic tooth movements associated with external apical root resorption of the maxillary central incisor. Am J Orthod Dentofacial Orthop. 1998;114:677–83. doi: 10.1016/s0889-5406(98)70200-8. https://doi.org/10.1016/S0889-5406(98)70200-8. [DOI] [PubMed] [Google Scholar]
- 17.Li W, Chen F, Zhang F, Ding W, Ye Q, Shi J, et al. Volumetric measurement of root resorption following molar mini-screw implant intrusion using cone beam computed tomography. PloS One. 2013;8:e60962. doi: 10.1371/journal.pone.0060962. https://doi.org/10.1371/journal.pone.0060962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jimenez-Pellegrin C, Arana-Chavez VE. Root resorption in human mandibular first premolars after rotation as detected by scanning electron microscopy. Am J Orthod Dentofacial Orthop. 2004;126:178–84. doi: 10.1016/j.ajodo.2003.06.020. https://doi.org/10.1016/j.ajodo.2003.06.020. [DOI] [PubMed] [Google Scholar]
- 19.Segal GR, Schiffman PH, Tuncay OC. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–8. doi: 10.1111/j.1601-6343.2004.00286.x. https://doi.org/10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 20.Phillips JR. Apical root resorption under orthodontic therapy. Angle Orthod. 1955;25:1–22. [Google Scholar]
- 21.Mandall N, Lowe C, Worthington H, Sandler J, Derwent S, Abdi-Oskouei M, et al. Which orthodontic archwire sequence? A randomized clinical trial. Eur J Orthod. 2006;28:561–66. doi: 10.1093/ejo/cjl030. https://doi.org/10.1093/ejo/cjl030. [DOI] [PubMed] [Google Scholar]
- 22.Reukers EA, Sanderink GC, Kuijpers-Jagtman AM, van’t Hof MA. Radiographic evaluation of apical root resorption with 2 different types of edgewise appliances. Results of a randomized clinical trial. J Orofac Orthop. 1998;59:100–09. doi: 10.1007/BF01340644. https://doi.org/10.1007/BF01340644. [DOI] [PubMed] [Google Scholar]
- 23.Scott P, DiBiase AT, Sherriff M, Cobourne MT. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2008;134:470.e1–8. doi: 10.1016/j.ajodo.2008.04.018. https://doi.org/10.1016/j.ajodo.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 24.Dindaroglu F, Dogan S. Evaluation and comparison of root resorption between tooth-borne and tooth-tissue borne rapid maxillary expansion appliances: A CBCT study. Angle Orthod. 2016;86:46–52. doi: 10.2319/010515-007.1. https://doi.org/10.2319/010515-007.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwasaki L, Crouch LD, Nickel J. Genetic factors and tooth movement. Semin Orthod. 2008;14:135–45. https://doi.org/10.1053/j.sodo.2008.02.004. [Google Scholar]
- 26.Al-Qawasmi RA, Hartsfield JK, Jr, Everett ET, Flury L, Liu L, Foroud TM, et al. Genetic predisposition to external apical root resorption. Am J Orthod Dentofacial Orthop. 2003;123:242–52. doi: 10.1067/mod.2003.42. https://doi.org/10.1067/mod.2003.42. [DOI] [PubMed] [Google Scholar]
- 27.Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part II. Treatment factors. Am J Orthod Dentofacial Orthop. 2001;119:511–15. doi: 10.1067/mod.2001.113410. https://doi.org/10.1067/mod.2001.113410. [DOI] [PubMed] [Google Scholar]
- 28.Murata N, Ioi H, Ouchi M, Takao T, Oida H, Aijima R, et al. Effect of allergen sensitization on external root resorption. J Dent Res. 2013;92:641–47. doi: 10.1177/0022034513488787. https://doi.org/10.1177/0022034513488787. [DOI] [PubMed] [Google Scholar]
- 29.Mirabella AD, Artun J. Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients. Eur J Orthod. 1995;17:93–9. doi: 10.1093/ejo/17.2.93. https://doi.org/10.1093/ejo/17.2.93. [DOI] [PubMed] [Google Scholar]
- 30.Spurrier SW, Hall SH, Joondeph DR, Shapiro PA, Riedel RA. A comparison of apical root resorption during orthodontic treatment in endodontically treated and vital teeth. Am J Orthod Dentofacial Orthop. 1990;97:130–4. doi: 10.1016/0889-5406(90)70086-R. https://doi.org/10.1016/0889-5406(90)70086-R. [DOI] [PubMed] [Google Scholar]
- 31.Kaneko S, Ohashi K, Soma K, Yanagishita M. Occlusal hypofunction causes changes of proteoglycan content in the rat periodontal ligament. J Periodontal Res. 2001;36:9–17. doi: 10.1034/j.1600-0765.2001.00607.x. https://doi.org/10.1034/j.1600-0765.2001.00607.x. [DOI] [PubMed] [Google Scholar]
- 32.Motokawa M, Terao A, Kaku M, Kawata T, Gonzales C, Darendeliler MA, et al. Open bite as a risk factor for orthodontic root resorption. Eur J Orthod. 2013;35:790–5. doi: 10.1093/ejo/cjs100. https://doi.org/10.1093/ejo/cjs100. [DOI] [PubMed] [Google Scholar]
- 33.Baumrind S, Korn EL, Boyd RL. Apical root resorption in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;110:311–20. doi: 10.1016/s0889-5406(96)80016-3. https://doi.org/10.1016/S0889-5406(96)80016-3. [DOI] [PubMed] [Google Scholar]
- 34.Lundgren D, Owman-Moll P, Kurol J. Early tooth movement pattern after application of a controlled continuous orthodontic force. A human experimental model. Am J Orthod Dentofacial Orthop. 1996;110:287–94. doi: 10.1016/s0889-5406(96)80013-8. https://doi.org/10.1016/S0889-5406(96)80013-8. [DOI] [PubMed] [Google Scholar]
- 35.Casa MA, Faltin RM, Faltin K, Sander FG, Arana-Chavez VE. Root resorptions in upper first premolars after application of continuous torque moment. Intra-individual study. J Orofac Orthop. 2001;62:285–95. doi: 10.1007/pl00001936. https://doi.org/10.1007/PL00001936. [DOI] [PubMed] [Google Scholar]
- 36.Leach HA, Ireland AJ, Whaites EJ. Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190:16–22. doi: 10.1038/sj.bdj.4800870. [DOI] [PubMed] [Google Scholar]
- 37.Sameshima GT, Asgarifar KO. Assessment of root resorption and root shape: periapical vs panoramic films. Angle Orthod. 2001;71:185–9. doi: 10.1043/0003-3219(2001)071<0185:AORRAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 38.Borg E, Kallqvist A, Gröndahl K, Gröndahl HG. Film and digital radiography for detection of simulated root resorption cavities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:110–4. doi: 10.1016/s1079-2104(98)90159-7. https://doi.org/10.1016/S1079-2104(98)90159-7. [DOI] [PubMed] [Google Scholar]
- 39.Kravitz LH, Tyndall DA, Bagnell CP, Dove SB. Assessment of external root resorption using digital subtraction radiography. J Endod. 1992;18:275–84. doi: 10.1016/s0099-2399(06)80954-4. https://doi.org/10.1016/S0099-2399(06)80954-4. [DOI] [PubMed] [Google Scholar]
- 40.Chan EK, Darendeliler MA. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7:64–70. doi: 10.1111/j.1601-6343.2004.00280.x. https://doi.org/10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 41.Harry MR, Sims MR. Root resorption in bicuspid intrusion. A scanning electron microscope study. Angle Orthod. 1982;52:235–58. doi: 10.1043/0003-3219(1982)052<0235:RRIBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 42.Wierzbicki T, El-Bialy T, Aldaghreer S, Li G, Doschak M. Analysis of orthodontically induced root resorption using micro-computed tomography (Micro-CT) Angle Orthod. 2009;79:91–6. doi: 10.2319/112107-546.1. https://doi.org/10.2319/112107-546.1. [DOI] [PubMed] [Google Scholar]
- 43.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–30. doi: 10.1016/j.cden.2008.05.005. https://doi.org/10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 44.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol. 2004;33:83–6. doi: 10.1259/dmfr/28403350. https://doi.org/10.1259/dmfr/28403350. [DOI] [PubMed] [Google Scholar]
- 45.Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–7. doi: 10.1016/j.ajodo.2008.10.014. https://doi.org/10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 46.Maret D, Telmon N, Peters OA, Lepage B, Treil J, Inglèse JM, et al. Effect of voxel size on the accuracy of 3D reconstructions with cone beam CT. Dentomaxillofac Radiol. 2012;41:649–55. doi: 10.1259/dmf/81804525. https://doi.org/10.1259/dmfr/81804525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brudvik P, Rygh P. Transition and determinants of orthodontic root resorption-repair sequence. Eur J Orthod. 1995;17:177–88. doi: 10.1093/ejo/17.3.177. https://doi.org/10.1093/ejo/17.3.177. [DOI] [PubMed] [Google Scholar]
- 48.Langford SR, Sims MR. Root surface resorption, repair, and periodontal attachment following rapid maxillary expansion in man. Am J Orthod. 1982;81:108–15. doi: 10.1016/0002-9416(82)90034-3. https://doi.org/10.1016/0002-9416(82)90034-3. [DOI] [PubMed] [Google Scholar]
- 49.Owman-Moll P, Kurol J, Lundgren D. Repair of orthodontically induced root resorption in adolescents. Angle Orthod. 1995;65:403–8. doi: 10.1043/0003-3219(1995)065<0403:ROOIRR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]