Abstract
Introduction:
The purpose of this study was to conduct a survey of North Carolina pharmacists' perceptions of their pharmacy training in mental health–related medication issues and how this influenced their perceived ability to address these issues in the provision of pharmaceutical care to their patients.
Methods:
A survey consisting of 17 questions was developed and emailed to licensed pharmacists in North Carolina. Surveys that were returned were analyzed to see if conclusions could be made regarding the pharmacists' perceptions about their mental health–related medication training and its influence on their practice.
Results:
A total of 848 pharmacists completed the survey (response rate of 7.9%). Of the survey participants, 489 (58.2%) reported that pharmacy school training adequately prepared them to provide basic pharmaceutical care to patients taking mental health–related medications. However, 350 (41.4%) reported feeling less comfortable providing medication counseling for mental health–related medications compared to cardiac medications.
Discussion:
Despite the volume of prescriptions that mental health–related medications represent in day-to-day practice, a significant portion of licensed pharmacists responding to our survey indicate that the emphasis on mental health in their training may have been inadequate.
Keywords: pharmacist, education, psychiatric medication
Introduction
Pharmacists must solve issues related to mental health medications in the same way they solve other medication issues with knowledge and skill acquired by training and experience. Approximately 26% of American adults suffer from a diagnosable mental illness in a given year, making mental illness comparable in frequency to the diagnosis of hypertension and more common than diabetes.1-3 A study conducted by the Centers for Disease Control and Prevention4 estimated that 22% of American adults had filled a prescription for anxiolytics, hypnotics, anticonvulsants, and antidepressants in the past 30 days, and 23.5% of American adults filled a prescription for antihypertensives. In addition, drugs used for treatment of conditions other than mental illness often have profound effects on the central nervous system (CNS).5 Symptoms of CNS toxicity, such as confusion, delirium, psychosis, and seizures, have been reported for nonpsychiatric medications, such as tizanidine and salicylates.5,6 Drug-induced depression has been attributed to representatives of such commonly used medical drug classes as lipid-lowering agents (simvastatin) and antihypertensives (beta-blockers). The elderly are particularly susceptible to drugs with CNS activity, and depression can be one of the consequences of treatment with these agents.7 Because a significant portion of prescription volume is comprised of drugs for mental illness and others with CNS activity, knowledge of these drugs, the conditions they treat, and the CNS effects they may produce should be a part of every pharmacist's skill set.
Didactic and experiential programs focusing on mental illnesses and the drugs to treat them vary greatly among schools and colleges of pharmacy. One survey of pharmacy institutions reported that only 9.5% of the didactic course content was dedicated to psychiatric topics. The authors reported that approximately 25% of pharmacy schools offered elective didactic courses in psychiatric pharmacy. Two schools required students to take a psychiatric advanced pharmacy practice experience (APPE; which is experiential education for pharmacy students building on previous introductory pharmacy practice experience and didactic courses with a goal to establish practitioners and expose students to the wide world of practice), and 92% offered psychiatric pharmacy as an elective APPE.8 The limited amount of psychiatric elective courses and APPEs may prevent students from receiving the knowledge needed to feel confident in offering mental health services.
Previous surveys suggest that some pharmacists, once in practice, feel they did not have an adequate amount of training in psychiatric medications. One survey9 of 100 community pharmacists and 40 fourth-year pharmacy students found that 63% of pharmacists and 60% of student pharmacists agreed or strongly agreed that they had adequate psychiatric pharmacy training throughout their pharmacy education, and 37% of pharmacists were neutral or disagreed. Another survey10 of 283 community pharmacists found that 24% of respondents felt that they received adequate education about mental health, and 61% reported that they had received adequate training in cardiovascular issues. The results of these studies suggest that mental health–related training in pharmacy schools may not receive the same emphasis as the training received in other areas. These findings are a cause for concern as pharmacists are accessible health care professionals and often encounter patients with mental illness. Pharmacists trained in mental health–related issues not only prevent negative outcomes, but also facilitate positive outcomes by promoting appropriate drug choices and regimen adherence.11 However, a recent qualitative study12 concluded that pharmacists are not practicing to their full scope of practice in mental health.
The purpose of the current study was to survey North Carolina licensed pharmacists about their perceptions of their pharmacy school training as it pertains to mental health–related medication issues.
Methods
The survey questionnaire was constructed to answer the study question and revised by consultation from 2 experienced board-certified psychiatric pharmacy specialists. The questionnaire was pilot-tested with 6 pharmacists, who range in years of experience, practice site, and residency experience. Afterward, revisions were made to enhance the readability and clarity of the survey questions. The survey was intended to be short, user-friendly, and administered online. It was not subjected to formal validation. The 17-question survey consisted of demographical questions and questions to evaluate the pharmacists' experience with mental health–related medications and perceptions of how this related to their pharmacy school training. The response to 9 of the questions was “yes,” “no,” or “not sure.” One question was evaluated on a 3-point Likert scale (“more comfortable,” “just as comfortable,” or “less comfortable”). This study was exempt from approval by the institutional review board at W.G. (Bill) Hefner Veterans Affairs Medical Center. The North Carolina Board of Pharmacy agreed to email the instrument to North Carolina licensed pharmacists. In February 2014, a cover letter and link to the survey instrument was emailed to North Carolina licensed pharmacists. The results were analyzed in Microsoft Excel (Redmond, WA) using descriptive statistics.
Results
Of the 10,670 pharmacists who received the survey, 848 completed the survey (7.9% response rate). Some surveys were returned incomplete; therefore, the results for each question are based on the number of actual respondents to each specific item. The majority of respondents were women (517/846, 61.1%) and received a doctorate of pharmacy degree (509/846, 60.2%). Most pharmacists worked in the community (395/748, 52.8%), and 32.6% (242/748) worked in the hospital setting. The majority of the pharmacists (636/846, 75.2%) had been working for longer than 5 years.
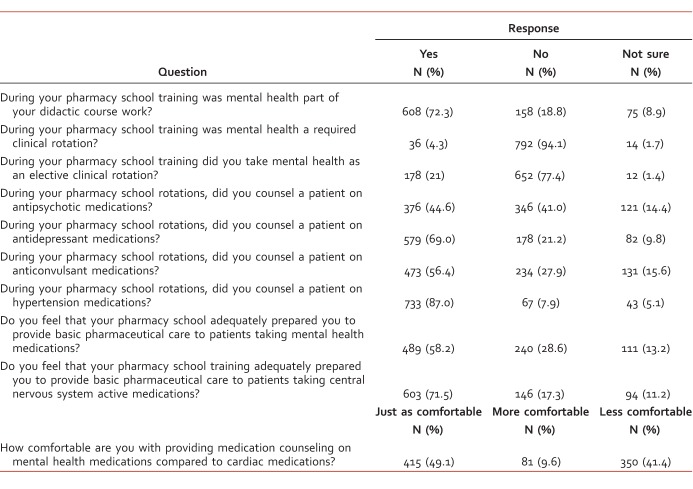
The Table describes pharmacists' experience and perceptions with mental health–related medication training during pharmacy school. Specifically, 608 (72.3%) pharmacists had mental health as part of their didactic course work, 36 (4.3%) reported that mental health was a required clinical rotation, and 178 (21%) indicated that they took an elective mental health rotation. Eighty-seven percent (733) counseled patients on hypertension medications, and 376 (44.6%) reported counseling patients on antipsychotics, 579 (69%) reported counseling patients on an antidepressant, and 473 (56.4%) reported counseling on anticonvulsants. Of the pharmacists who responded, 489 (58.2%) reported that pharmacy school adequately prepared them to provide basic pharmaceutical care to patients taking mental health medications, and 603 (71.5%) agreed when asked about CNS active medications. When asked how comfortable they are with providing counseling on mental health medications compared to cardiac medications, 415 (49.1%) stated they were just as comfortable, 81 (9.6%) were more comfortable, and 350 (41.4%) were less comfortable.
TABLE:
Survey results on pharmacists' perceptions of their pharmacy training in mental health–related medication issues
Discussion
The majority of pharmacists who responded to the survey endorsed feeling that pharmacy school adequately prepared them to provide care to patients taking mental health medications. These results are similar to results of a previous study,9 which reported that 63% of pharmacists strongly agreed or agreed that they had adequate education during pharmacy training on psychotherapeutic agents. However, 41.4% of participants admitted to being less comfortable counseling patients on mental health medications when compared to cardiac medications. The discrepancy in comfort level could be due to many additional causes besides pharmacy school training. Health care professionals, including pharmacists, have reported stigmatizing views of mental health patients.13 A survey10 of community pharmacists reported that pharmacists felt less comfortable discussing symptoms and medications with patients who have mental illness compared with patients who have cardiovascular problems, and therefore, those patients received fewer counseling services. The primary barriers included lack of privacy and a need for more training. This survey cannot differentiate the cause, but the implication is clear. There cannot be one standard of care for patients who are prescribed mental health medications and another for patients prescribed drugs for cardiac medications.
Several previous studies have examined ways for pharmacy schools to minimize mental illness–related stigma in students. Antistigma interventions with contact to mental health patients demonstrated the greatest benefit. A recent study14 demonstrated that consumer-based education was an effective teaching method to reduce mental illness–related stigma in students from 3 pharmacy schools in Canada. A consumer educator is a person who previously received mental health services and is currently stable.15 Another study16 surveyed students about social distance (the willingness of an individual to interact in varying degrees with patients with mental illness) before and after taking an elective class in mental health. The elective included multiple components, including interviewing a patient with a psychiatric diagnosis. The study showed that the elective had a positive impact on social distance in students who took the elective compared to the control group. Similar results were found in a study performed by DiPaula et al.17 Additionally, a consumer-led education intervention for pharmacy students showed sustained reduction in student's stigma at the 12-month follow-up.18 Pharmacy schools need to recognize that the traditional use of didactic lectures and clinical rotations does not significantly improve students' attitudes toward patients with mental illness.19 Information is not yet available regarding the inclusion in existing pharmacy school curricula of consumer-based education for mental illness stigma.
This study had several limitations. The low response rate was a significant drawback and could have skewed the data. A majority of the respondents practiced in a community pharmacy (52.8%) and were women (61.1%). In comparison, the national average shows that greater than 60% of pharmacists work in community or retail settings and 46% of pharmacists are women.20 Only 24.6% of respondents had been working for less than 5 years as a pharmacist. Therefore, recall bias could affect the results. Further, the survey may not reflect recent adjustments made to pharmacy school curriculums.
Conclusion
Our study supports findings in similar previous studies and adds to the growing body of knowledge suggesting improvements are needed in mental health–related pharmacy education. The survey indicates that in a group of experienced pharmacists (most having longer than 5 years practice experience) many did not feel comfortable counseling patients on mental health–related medications. Schools and colleges of pharmacy can use this feedback from the field to adjust curricula to meet the educational needs identified by practicing pharmacists. Requiring training that provides face-to-face interactions with mental health patients will help meet this need.
The present study was conducted in a population of practicing pharmacists. Although the findings have implications for pharmacy school training, how are the needs of the practicing pharmacist to be met? National, state, and local pharmacy organizations can reach out to board-certified psychiatric pharmacists who have the expertise to develop continuing education programs that build on the skills of practicing pharmacists and apply them to mental health–related scenarios. Patients with mental illness deserve no less than the highest level of pharmaceutical care from a pharmacist, who by nature of training and experience, has the necessary skills and knowledge to provide that care.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US Government.
Footnotes
Disclosures: Authors of this paper disclose concerning possible financial or personal relationships with commercial entities that may have a direct or indirect interest in the subject matter of this paper: All authors have nothing to disclose.
References
- 1. National Institute of Mental Health. The number count: mental disorders in America [cited 2014. Feb 4]. Available from: http://www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america/index.shtml
- 2. Egan BM, Zhao Y, Axon RN. . US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010; 303 20: 2043- 50. DOI: 10.1001/jama.2010.650. PubMed PMID: 20501926. [DOI] [PubMed] [Google Scholar]
- 3. Li C, Balluz LS, Okoro CA, Strine TW, Lin J-MS, Town M, et al. Surveillance of certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2009. MMWR Surveill Summ. 2011; 60 9: 1- 250. PubMed PMID: 21849967. [PubMed] [Google Scholar]
- 4. Center for Disease Control and Prevention. Prescription drug use in the past 30 days, by sex, age, race and Hispanic origin: United States, selected years 1988-1994 through 2007-2010 [cited 2014. Feb 2]. Available from: http://www.cdc.gov/nchs/data/hus/2012/092.pdf
- 5. Ruha A-M, Levine M. . Central nervous system toxicity. Emerg Med Clin North Am. 2014; 32 1: 205- 21. DOI: 10.1016/j.emc.2013.09.004. PubMed PMID: 24275175. [DOI] [PubMed] [Google Scholar]
- 6. Barry JD, Wills BK. . Neurotoxic emergencies. Neurol Clin. 2011; 29 3: 539- 63. DOI: 10.1016/j.ncl.2011.05.006. PubMed PMID: 21803209. [DOI] [PubMed] [Google Scholar]
- 7. Kotlyar M, Dysken M, Adson DE. . Update on drug-induced depression in the elderly. Am J Geriatr Pharmacother. 2005; 3 4: 288- 300. PubMed PMID: 16503326. [PubMed] [Google Scholar]
- 8. Cates ME, Monk-Tutor MR, Drummond SO. . Mental health and psychiatric pharmacy instruction in US colleges and schools of pharmacy. Am J Pharm Educ. 2007; 71 1: 4 PubMed PMID: 17429504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McKee BD, Larose-Pierre M, Rappa LR. . A survey of community pharmacists and final-year student pharmacists and their perception of psychotherapeutic agents. J Pharm Pract. 2015; 28 2: 166- 74. DOI: 10.1177/0897190013515709. PubMed PMID: 24346959. [DOI] [PubMed] [Google Scholar]
- 10. Phokeo V, Sproule B, Raman-Wilms L. . Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatric Serv. 2004; 55 12: 1434- 6. DOI: 10.1176/appi.ps.55.12.1434. PubMed PMID: 15572574. [DOI] [PubMed] [Google Scholar]
- 11. Bell S, McLachlan AJ, Aslani P, Whitehead P, Chen TF. . Community pharmacy services to optimise the use of medications for mental illness: a systematic review. Aust New Zealand Health Policy. 2005; 2: 29 DOI: 10.1186/1743-8462-2-29. PubMed PMID: 16336646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Murphy AL, Phelan H, Haslam S, Martin-Misener R, Kutcher SP, Gardner DM. . Community pharmacists' experiences in mental illness and addictions care: a qualitative study. Subst Abuse Treat Prev Policy. 2016; 11 1: 6 DOI: 10.1186/s13011-016-0050-9. PubMed PMID: 26821700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schulze B. . Stigma and mental health professionals: a review of the evidence on an intricate relationship. Int Rev Psychiatry. 2007; 19 2: 137- 55. DOI: 10.1080/09540260701278929. PubMed PMID: 17464792. [DOI] [PubMed] [Google Scholar]
- 14. Patten SB, Remillard A, Phillips L, Modgill G, Szeto AC, Kassam A, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ. 2012; 12: 120 DOI: 10.1186/1472-6920-12-120. PubMed PMID: 23216787; PubMed Central PMCID: PMC3533989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rubio-Valera M, Chen TF, O'Reilly CL. . New roles for pharmacists in community mental health care: a narrative review. Int J Environ Res Public Health. 2014; 11 10: 10967- 90. DOI: 10.3390/ijerph111010967. PubMed PMID: 25337943; PubMed Central PMCID: PMC4211017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gable KN, Muhlstadt KL, Celio MA. . A mental health elective to improve pharmacy students' perspectives on mental illness. Am J Pharm Educ. 2011; 75 2: 34 PubMed PMID: 21519423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dipaula BA, Qian J, Mehdizadegan N, Simoni-Wastila L. . An elective psychiatric course to reduce pharmacy students' social distance toward people with severe mental illness. Am J Pharm Educ. 2011; 75 4: 72 PubMed PMID: 21769148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O'Reilly CL, Bell JS, Chen TF. . Consumer-led mental health education for pharmacy students. Am J Pharm Educ. 2010; 74 9: 167 PubMed PMID: 21301601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bell JS, Johns R, Chen TF. . Pharmacy students' and graduates' attitudes towards people with schizophrenia and severe depression. Am J Pharm Educ. 2006; 70 4: 77 PubMed PMID: 17136196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Department of Health and Human Services Health Resources and Services Administration Bureau of Health Professionals [Internet]. A study of the supplement demand for pharmacy; 2000. [cited 2016 Jan 12]. Available from: http://bhpr.hrsa.gov/healthworkforce/reports/pharmaciststudy.pdf