Abstract
Introduction:
Written medicine information (WMI) is a collection of facts for a specific medication, and it helps facilitate patient understanding of medication therapy. The primary objective of this study was to assess consumer satisfaction with National Alliance on Mental Illness (NAMI) WMI. A secondary objective was to assess health care professional satisfaction.
Methods:
National Alliance on Mental Illness WMI and surveys were offered to consumers, health care professionals, and trainees at 3 treatment centers with psychiatric services. All adults who received medication counseling were eligible for inclusion. Survey responses were evaluated using descriptive statistics.
Results:
Most consumers (82.4%) and providers (74.5%) reported overall satisfaction with NAMI WMI. Consumers were least satisfied with information on how to manage unwanted effects, drug-drug interactions, and readability (9.5%, 14.9%, 41.9% dissatisfaction).
Discussion:
Evaluation and feedback from consumers and health care professionals may influence decisions to refine NAMI WMI to meet consumer needs.
Keywords: medication adherence, medication education, written medicine information, psychotropics, quality improvement
Introduction
In 2013, approximately 12.5% (29.5 million) of American adults received prescription medications for mental health issues.1 Although adherence to medications is a key component of treatment for mental illness, the rate of adherence is estimated to be 50% or less in this population.2 In addition to behavioral, social, environmental, and financial factors, patient concerns, such as adverse effects and unclear treatment expectations, likely impair adherence.3 The positive impact of education on medication adherence has been well established; however, survey and observational data suggest the prescriber's role in this area is lacking.3-9 An analysis of health care visits from the Physician Patient Communication Project found that prescribers gave no medication instructions for up to 25% of new prescriptions and spent an average of only 49 seconds on medication education when it was provided. Interestingly, the overall quality of education for psychiatric medications was superior compared to other classes, but information on duration of therapy and adverse effects was omitted for 62% and 38% of psychotropics, respectively.4,5 This highlights the need for other high-quality forms of patient education. Written medicine information (WMI) is a collection of facts for a specific medication intended to help facilitate patient understanding of medication therapy. Written medicine information is helpful for reinforcing and supplementing verbal medication counseling delivered by health care professionals when presented in a patient-friendly manner.10
A primary focus of the National Alliance on Mental Illness (NAMI)11 is educating consumers, family members, and the community about mental illness and treatment. National Alliance on Mental Illness has partnered with the College of Psychiatric and Neurologic Pharmacists (CPNP) for more than a decade to prepare WMI for medications used to treat mental illness. College of Psychiatric and Neurologic Pharmacists members complete annual revisions to improve readability and provide up-to-date information, definitions, warnings, and instructions for use. National Alliance on Mental Illness WMI is freely available at www.nami.org and received more than 1 500 000 page views from April 2015 to April 2016.
To our knowledge, no systematic evaluation of NAMI WMI has been conducted. Given the important role of medication education in adherence, this pilot survey study sought to determine consumer satisfaction with NAMI WMI and to generate data to aid CPNP and NAMI in continual quality improvement. Written medicine information for selective serotonin reuptake inhibitors (SSRIs) were chosen for initial review. Secondary goals were to assess health care professional and trainee satisfaction via survey.
Methods
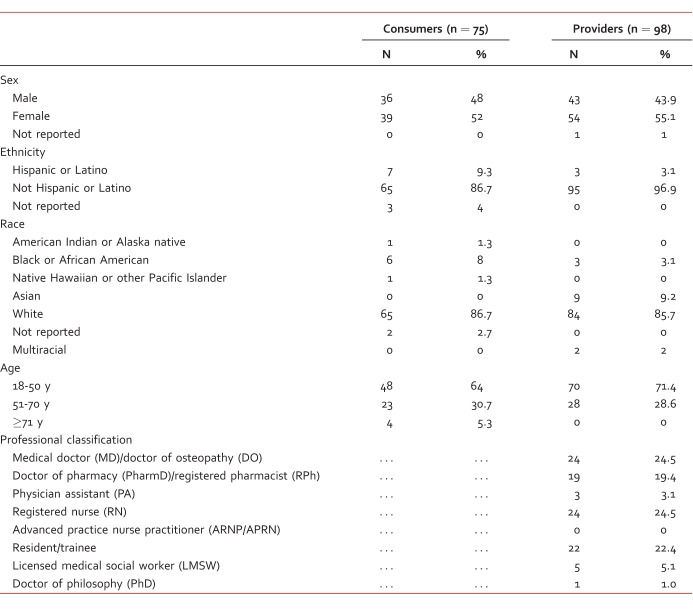
The study was approved by the institutional review boards of all sites where surveys were distributed. Study investigators developed consumer and provider surveys. Investigators selected questions from 2 validated tools for the assessment of WMI that were most applicable to NAMI WMI. The complete validated tools were not included in an attempt to minimize the length of study surveys and likelihood of survey completion. Additional questions were authored by study investigators to assess readability and overall satisfaction with NAMI WMI. Consumers and providers were asked to respond with a 5-point Likert scale (“strongly agree,” “agree,” “neutral,” “disagree,” “strongly disagree”). In order to use a matching Likert scale for each survey, questions from validated tools were modified to mirror the sentence structure of the authors' original survey questions. The final question on consumer and provider surveys asked how NAMI WMI could best be improved with space for written feedback. Both surveys also included a section of demographic questions (Table 1).
TABLE 1:
Self-reported demographics of consumers and providers surveyed
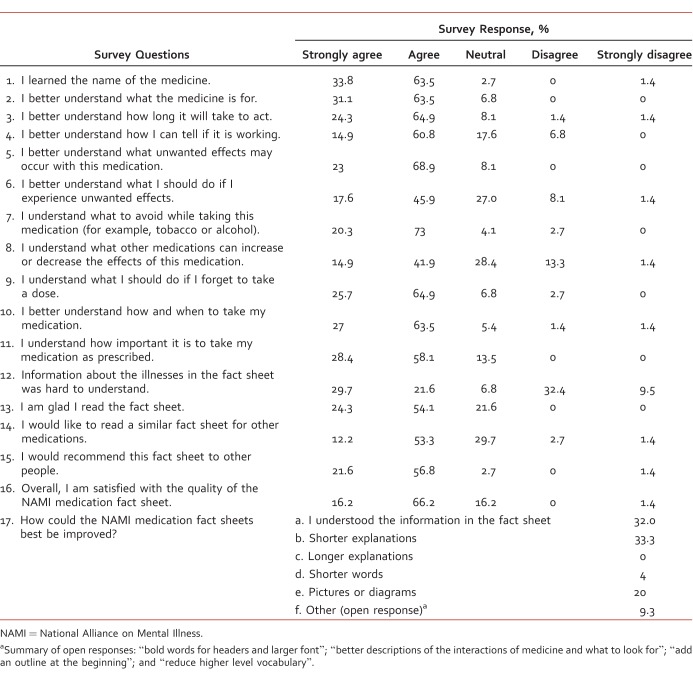
Consumer surveys included 17 items (Table 2). Survey items 1 through 10 were derived from the Satisfaction with Information about Medicines Scale.12 Five items addressed information about actions and administration of the medication (eg, “I better understand what the medicine is for”), and 5 items addressed information about potential problems of the medication (eg, “I better understand what unwanted effects may occur”). Survey items 11 through 16 were written by investigators to assess patient perceived readability (eg, “Information about the illness in the fact sheet was hard to understand”) and overall satisfaction (eg, “I would recommend this fact sheet to other people”).
TABLE 2:
Consumer survey results (n = 74)
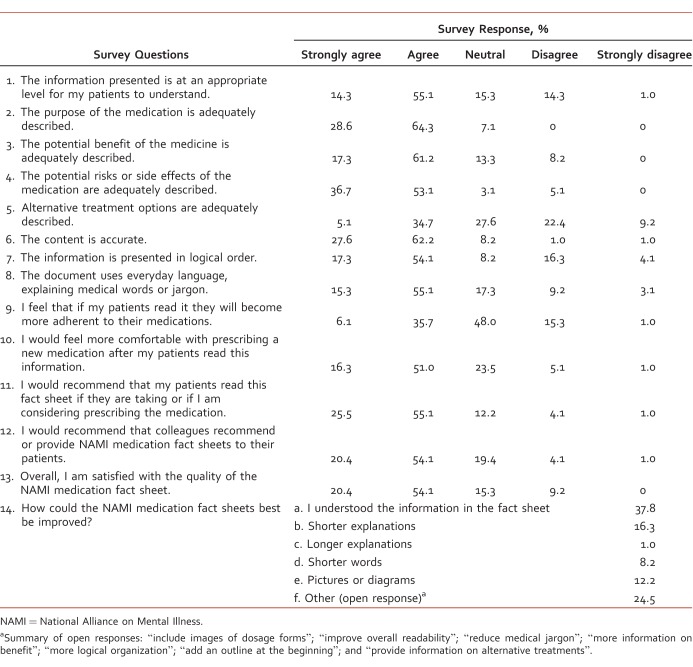
Provider surveys included 14 items to assess satisfaction with NAMI WMI (Table 3). Six items were derived from the Ensuring Quality Information for Patients tool.13 Similar to consumer surveys, items addressed specific aspects of medication therapy, such as “The purpose of the medication is adequately described” and “The potential risks or side effects of the medication are adequately described.” Remaining items assessed readability and overall satisfaction. Three additional informational questions were included with demographic questions to evaluate providers' knowledge and use of NAMI WMI prior to survey completion.
TABLE 3:
Provider survey results (n = 98)
Surveys were distributed to consumers, providers, and trainees between December 2012 and February 2013 at 3 sites with psychiatric services: a Department of Veterans Affairs hospital, an academic medical center, and a private psychiatric hospital.
A paper survey was offered to any inpatient or outpatient ≥18 years old who was given NAMI WMI for an SSRI by a clinical pharmacist during medication counseling. Selective serotonin reuptake inhibitors were chosen for evaluation as these are among the most commonly prescribed psychotropic medications at the study sites. Consumers were excluded if the clinical pharmacist distributing NAMI WMI determined they were unable to independently complete the survey. A paper or electronic survey along with NAMI WMI for fluoxetine was distributed to licensed health care professionals and trainees practicing in psychiatric settings. Evaluation of multiple SSRIs for consumers and a single SSRI (fluoxetine) for providers was felt to be appropriate considering that information included in NAMI WMI varies little among individual medications within each class with the exception of medication-specific information, such as administration instructions and drug-drug interactions. All surveys were anonymous and voluntary.
Results
Completed survey response rates were 54.8% for consumers (n = 74) and 23.4% for providers (n = 98). One consumer who provided demographic data was excluded from primary analysis due to an incomplete survey. The majority of participants were 18 to 50 years of age (consumers 64.9%, providers 74.5%) and white (consumers 88%, providers 85.7%). There was a similar disposition of men and women in each group with 51.4% and 55.1% female consumers and providers, respectively. There was a small Hispanic/Latino representation in each group (consumers 9.5%, providers 3%; Table 1). Spanish handouts were not provided, but participants were excluded if they could not independently complete the survey. Survey recipients had a variety of mental health diagnoses, including affective, anxiety, personality, and thought disorders. The majority of consumers (82.4%) and providers (74.5%) reported overall satisfaction with the quality of the NAMI WMI, and survey responses were similar between the two groups (Tables 2 and 3). Based on distribution of consumer survey results, the 3 items with the highest level of dissatisfaction (defined by ratings of “disagree” or “strongly disagree”) were identified as opportunities for improvement. For consumers, these included management of unwanted effects, information on drug-drug interactions, and readability of information about illnesses (9.5%, 14.9%, 41.9% dissatisfaction).
Providers were least satisfied with readability (12.3% and 15.3 % dissatisfaction with the level of information for patients and use of medical jargon, respectively) and information on alternative treatment options (31.6% dissatisfaction). Although only 27.6% of providers had given or recommended NAMI WMI to patients prior to the survey, more than 70% indicated they would recommend it to patients or colleagues after participation in this study.
Discussion
Results from this multisite pilot survey study revealed a high level of satisfaction with NAMI WMI for SSRIs among a diverse mental health population in a variety of psychiatric treatment settings. For the primary study objective, consumers identified readability, information on drug-drug interactions, and management of side effects as potential areas for improvement.
At the time of the survey, each medication fact sheet listed interacting medications categorized by the SSRI's propensity to decrease or increase the effects of those medications. There was also a description of risk and symptoms of serotonin syndrome with concomitant serotonergic agents. Adding clinical symptoms that may occur as a result of “increased” and “decreased” effects secondary to other listed drug-drug interactions may improve consumer satisfaction with NAMI WMI. Information about side effects has been the most commonly requested medication information by patients with mental illnesses.3 Per survey results, approximately 10% of consumers were dissatisfied with information on how to manage side effects. Side effects in NAMI WMI were listed as “common,” “rare,” or “serious” and included a statement that common side effects often improve over the first weeks of treatment. To better meet this consumer need, a recommendation to contact the prescriber or present to the emergency room for management of rare or severe side effects could be added. WMI could also consider an electronic link to a regularly updated guide for managing common side effects. As a consumer, reading a list of potential side effects can be concerning. Increased knowledge has been shown to improve consumer comfort with taking prescribed medications.10 Health care professionals should remember to provide specific and practical guidance on how to recognize and handle pertinent unwanted effects when providing verbal or written medication information. This may help improve adherence and safety of medication therapy. Health literacy limitations have been associated with poorer health outcomes in patients with depression and multiple chronic disease states.14,15 A significant proportion of consumers reported the information about mental illness in NAMI WMI was hard to understand. Prior to survey completion, the Flesch-Kincaid Grade Level (FKGL) score was reduced from 13.3 to 11, and information about depression was reorganized from paragraph to bullet format with the goal of improving readability.16 Readability evaluation tools, including the FKGL score, typically measure characteristics such as average syllables per word and sentence length; therefore, medical terms and drug names often falsely elevate grade level scores.10 When developing any form of WMI, efforts can be made to define medical jargon when it cannot be avoided. It should be noted that readability assessments alone are insufficient to fully evaluate the ability of WMI to inform consumers.10 Written medicine information evaluation tools such as the Consumer Information Rating Form provide a more thorough assessment of comprehensibility and utility and could be considered for future evaluations of NAMI WMI.17 In November 2013, study investigators presented recommendations to the CPNP task force for further improvements to consider when revising NAMI WMI for SSRIs based on study results. Since that time, efforts were made to improve information on drug-drug interactions by reformatting interacting agents from paragraph to bullet form and clarifying the potential for SSRIs to increase the effect of other medications that can cause bleeding. Recommendations that may still be considered for future revision include addition of descriptions of clinical symptoms that may indicate a significant drug-drug interaction has occurred, an electronic link to a side effect management guide, or guidance to seek medical attention based on the severity of the side effect. These improvements may increase the usability of WMI, more effectively educate patients on their medications, and potentially decrease 1 component linked with nonadherence. Reanalysis of consumer and provider satisfaction with current NAMI WMI may be useful to assess the impact of changes to FKGL score, formatting, and drug-drug interaction information since pilot survey completion.
There were several limitations to this study. The return rate of completed surveys was suboptimal, and there were likely consumers with important feedback who did not participate. Limiting the number of survey questions may result in a higher response rate in future evaluations. Although the majority of survey items were derived from previously validated tools for assessing satisfaction with written health care information, items used to determine overall satisfaction and readability were written by the authors and have not been validated. As mentioned previously, use of a validated comprehensibility evaluation tool, such as the Consumer Information Rating Form, may provide valuable assessment of NAMI WMI in the future.
Conclusion
This pilot survey study allowed us to evaluate consumer and provider satisfaction with NAMI WMI for SSRIs. Health care professionals' perceptions of NAMI WMI effectiveness as an educational tool echoed that of consumers and also provided valuable guidance for future revisions. Survey results allowed us to make recommendations for further improvements for the CPNP task force to consider when revising these resources. Future studies could involve additional treatment facilities, feedback from families or caregivers, reevaluation of WMI for SSRIs since revision, or evaluation of WMI for other medication classes.
References
- 1. Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-49, HHS Publication No. (SMA) 14-4887. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2014
- 2. Julius RJ, Novitsky MA, Dubin WR. . Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009; 15 1: 34- 44. DOI: 10.1097/01.pra.0000344917.43780.77. PubMed PMID: 19182563. [DOI] [PubMed] [Google Scholar]
- 3. Zwaenepoel L, Bilo R, De Boever W, De Vos M, Reyntens J, Hoorens V, et al. Desire for information about drugs: a survey of the need for information in psychiatric in-patients. Pharm World Sci. 2005; 27 1: 47- 53. PubMed PMID: 15861935. [DOI] [PubMed] [Google Scholar]
- 4. Tarn DM, Paterniti DA, Kravitz RL, Heritage J, Liu H, Kim S, et al. How much time does it take to prescribe a new medication? Patient Educ Couns. 2008; 72 2: 311- 9. DOI: 10.1016/j.pec.2008.02.019. PubMed PMID: 18406562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. . Physician communication when prescribing new medications. Arch Intern Med. 2006; 166 17: 1855- 62. DOI: 10.1001/archinte.166.17.1855. PubMed PMID: 17000942. [DOI] [PubMed] [Google Scholar]
- 6. Hornung WP, Kieserg A, Feldmann R, Buchkremer G. . Psychoeducational training for schizophrenic patients: background, procedure and empirical findings. Patient Educ Couns. 1996; 29 3: 257- 68. PubMed PMID: 9006241. [DOI] [PubMed] [Google Scholar]
- 7. Macpherson R, Jerrom B, Hughes A. . A controlled study of education about drug treatment in schizophrenia. Br J Psychiatry. 1996; 168 6: 709- 17. PubMed PMID: 8773813. [DOI] [PubMed] [Google Scholar]
- 8. Katon W, von Korff M, Lin E, Simon G, Walker E, Unützer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999; 56 12: 1109- 15. PubMed PMID: 10591288. [DOI] [PubMed] [Google Scholar]
- 9. Katon W, von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995; 273 13: 1026- 31. PubMed PMID: 7897786. [PubMed] [Google Scholar]
- 10. Luk A, Aslani P. . Tools used to evaluate written medicine and health information: document and user perspectives. Health Educ Behav. 2011; 38 4: 389- 403. DOI: 10.1177/1090198110379576. PubMed PMID: 21490309. [DOI] [PubMed] [Google Scholar]
- 11. About NAMI. . National Alliance on Mental Illness Web site [Internet]. Arlington (VA): NAMI; c2015 [cited 2015 Nov 30]. Available from: http://www.nami.org/About-NAMI
- 12. Horne R, Hankins M, Jenkins R. . The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Qual Health Care. 2001; 10 3: 135- 40. PubMed PMID: 11533420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moult B, Franck LS, Brady H. . Ensuring quality information for patients: development and preliminary validation of a new instrument to improve the quality of written health care information. Health Expect. 2004; 7 2: 165- 75. DOI: 10.1111/j.1369-7625.2004.00273.x. PubMed PMID: 15117391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bauer AM, Schillinger D, Parker MM, Katon W, Adler N, Adams AS, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the diabetes study of Northern California (DISTANCE). J Gen Intern Med. 2013; 28 9: 1181- 7. DOI: 10.1007/s11606-013-2402-8. PubMed PMID: 23512335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Berkman ND, DeWalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, et al. Literacy and health outcomes (AHRQ Publication No. 04-E007-2). Rockville (MD): Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- 16. Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. . Derivation of new readability formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy enlisted personnel. Research Branch report 8-75. Memphis: Naval Air Station; 1975. [Google Scholar]
- 17. Koo MM, Krass I, Aslani P. . Evaluation of written medicine information: validation of the consumer information rating form. Ann Pharmacother. 2007; 41 6: 951- 6. DOI: 10.1345/aph.1K083. PubMed PMID: 17488832. [DOI] [PubMed] [Google Scholar]