Abstract
Objective
This study aimed to examine the biomechanical effects of the fixed functional appliances reinforced with miniscrews by finite elements analysis over the cranial and facial bones, temporomandibular joint, and maxillary-mandibular teeth, which are used for the treatment of Class II division 1 malocclusions characterized as mandibular retrognathia.
Methods
Three-dimensional (3-D) models of the cranial, mandibular, and maxillary bones were purchased from a company that produces 3-D models of the bones. Simulations of Forsus, screwed Forsus, Twin-Force and screwed Twin-Force appliances were conducted on the 3 D models. The miniscrew was placed in the inter-radicular area between the upper canine and first upper premolar teeth.
Results
It was observed in the models that the first upper molar tooth was the most affected. The compressive stress was observed in the anterior area of the mandibular condyle neck in the Forsus appliances; however, it was observed in the posterior area of the mandibular condyle neck in Twin-Force appliances.
Conclusion
It was observed that molar distalization and expansion decreases in the functional appliances with the support of miniscrew. The highest tension rates were determined in the areas of condylar and articular discs.
Keywords: Functional treatment, miniscrew, finite element analysis
INTRODUCTION
In the treatment of Class II division 1 malocclusions characterized by mandibular inadequacy, functional and fixed appliances are used that allow forward positioning of the mandibular to stimulate mandibular growth. In contrast to the removable functional appliances, fixed functional appliances provide advantages, such as not requiring patient cooperation, and they can be used along with brackets (1).
Fixed functional appliances are available in rigid, flexible, and semi-rigid models. The Forsus Fatigue Resistance Device (FRD; 3M Unitek Corp, Monrovia, Calif) and Twin-Force Bite Corrector (TFBC; Ortho Organizers Inc., Carlsbad, Calif) are semi-rigid fixed functional appliances and were developed to avoid the ruptures that can occur with flexible fixed functional appliances. Furthermore, rigid fixed functional appliances restrict mouth opening, which has been resolved with the use of semi-rigid fixed functional appliances. Therefore, the FRD and TFBC semi-rigid fixed functional appliances were used in our study. Previous studies using these appliances have reported distal and intrusive movement of the maxillary molars, mesial movement of the mandibular molars, retrusive movement of the maxillary incisors, labial tipping of the mandibular incisors, and skeletal effect with certain amounts (2–10).
Undesired dental effects also occur along with the desired skeletal effects with the usage of functional appliances. The use of miniscrews has increased in orthodontic practice to control these dental movements (11). Conversely, the functional appliance is not used by placing the miniscrews in the maxillary.
Hypothetically, with the use of FRD and TFBC in patients with normal maxillary and retrusive mandibular, it is possible to decrease the maxillary effect and increase the mandibular effect by increasing the maxillary dental anchorage using a miniscrew. The purpose of our study was to comparatively examine the effects of the FRD and TFBC therapy reinforced with miniscrews and conventional FRD and TFBC therapy over the dentofacial structures using finite elements analysis.
METHODS
This study was approved by the noninvasive clinical research ethics committee of Cumhuriyet University.
Class II division 1 malocclusion characterized by normal maxillary and retrognatic mandibular and the 7-mm overjet have been modeled.
The three-dimensional (3-D) models of the cranial, mandibular, and maxillary bones were purchased from a company (21st Century Solutions Ltd.; Suite 31, Don House, 30–38 Main Street, Gibraltar) that produces the 3-D models of these bones. The models were scanned using a 3-D optic surface scanner by the company, and all data were transferred to the computer (Figure 1). The Sobotta Anatomy Atlas was used and all teeth, periodontal ligaments, sutures (frontomaxillaris, zygomaticomaxillaris, pterigopalatina, zygomaticotemporalis, nasofrontalis, and zygomaticofrontalis), joint discs, and ligaments were modeled using the NX Advanced v10 (Siemens PLM Software, 5800 Granite Parkway, Suite 600, Plano, TX, ABD) software. The tetrahedral model was constructed using the NX Nastran (Siemens PLM Software, 5800 Granite Parkway, Suite 600, Plano, TX, ABD) software, thereby forming the finite elements model of the complete craniofacial structures.
Figure 1.
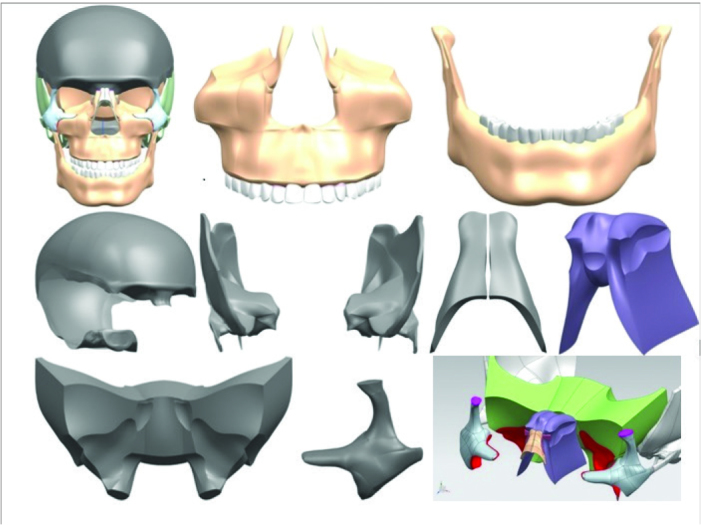
3-D model of the craniofacial complex (head, maxilla, mandibular, cranium, os temporale, os nasale, os ethmoidale, os sphenoidale, os zygomaticum, sutures)
Teeth, cortical bones, and trabecular bones were accepted as homogenous and linear elastic. The 1-mm cortical bone that covers the surface areas of the jaw bones where the teeth were, and beneath this layer was modeled as the trabecular bone. Furthermore, the areas without teeth were modeled as cortical bone (12). Brackets were modeled as the fixed ties and a 0.017×0.025″ stainless steel wire was used as the arc wire.
The Sabotta Anatomy Atlas was used for modeling of the sticking points of joint ligaments to the bone surfaces. The role of discal ligaments is to prevent divergence of the disc and condyle head; hence, discal ligaments were modeled through fixing the distance between some nodes on the disc and condyle head. In case of temporomandibular and capsular ligaments, they were modeled as arc elements by using the sticking points as the base. The auxiliary ligaments that have no effect on the movements of the mandibular were excluded from modeling. The arc rating of these modeled ligaments was adjusted as 272.4 N/m (13).
The appliances were modeled by measuring horizontal and vertical components of the FRD and TFBC using digital calipers (Figure 2, 3). Miniscrews were placed in the interradicular area, between the upper canine and first upper premolar teeth and their positions were 3 mm apically away from the cemento-enamel junction (14). The miniscrews were tied to both the upper lateral and upper first molar teeth in the screwed models. In the simulation of Forsus and screwed Forsus appliances, a two-sided pushing force of 200 gf was applied between the distal of the lower canine tooth and first upper molar tooth. In the simulation of Twin-Force and screwed Twin-Force appliances, a two-sided pushing force of 200 gf was applied to the arc wire between the first upper molar and second upper premolar teeth and to the arc wire between the lower canine tooth and the first lower premolar tooth.
Figure 2.
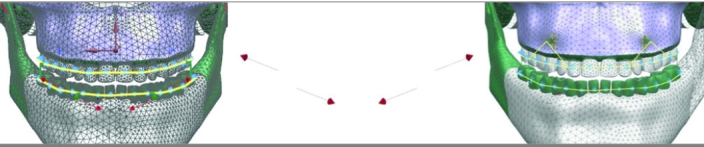
Model of the FRD and miniscrewed FRD
FRD: fatigue resistance device
Figure 3.
Model of the TFBC and miniscrewed TFBC
TFBC: twin-force bite corrector
Panigrahi et al. (15) modeled the entire skull and used a total 13590 elements and 18582 nodal points. In our study, the numbers of elements and nodal points were increased compared with previous studies, and the model of the skull was formed using 389,851 elements and 636,198 nodes.
Because our study did not include multiple patient groups, statistical analysis was not performed.
The elastic characteristics of the material were taken from previous studies (Table 1) (16–27). Mega-Pascal unit (MPa) was used to evaluate stress findings. The color scale at the left side of the figure indicates the stress ratings for each figure.
Table 1.
The physical properties of the materials
| Young’s modulus (MPa) | Poisson’s ratio | |
|---|---|---|
| Cortical Bone | 13700 | 0.3 |
| Trabecular Bone | 7900 | 0.3 |
| Teeth | 20290 | 0.3 |
| PDL | 7 | 0.49 |
| Cartilage | 0.79 | 0.49 |
| Articular Disc-Anterior | 10 | 0.4 |
| Articular Disc-İntermediate | 10.73 | 0.4 |
| Articular Disc-Posterior | 9 | 0.4 |
| Sutures | 7 | 0.49 |
| Orthodontic wire | 200000 | 0.3 |
| Miniscrew | 105000 | 0.33 |
| Connective Tissue | 0.49 | 0.49 |
| Ligament | 0.49 | 0.49 |
RESULTS
The areas with the minimum principal stresses, which get low negative ratings in the mandibular, were observed in the anterior area of the mandibular condyle neck in the FRD and screwed-FRD models. They were observed however in the posterior area of the mandibular condyle neck in the TFBC and screwed-TFBC models. The dominant type of stress in these areas was found to be compressive. The areas with the maximum principal stresses, which get high positive ratings, were observed in the posterior area of the mandibular condyle neck in the FRD and screwed-FRD models. They were observed however in the anterior area of the mandibular condyle neck in the TFBC and screwed-TFBC models.
In the simulation of the FRD appliance, the compressive stress (−0.767 MPa) occurred in the anterior area of the condylar neck and the tensile stress (0.871 MPa) occurred in the posterior area. Similarly, in the simulation of the screwed-FRD appliance, the compressive stress (−0.787 MPa) occurred in the anterior of condylar neck, and the tensile stress (0.962 MPa) occurred in the posterior area. However, in the simulation of the TFBC appliance compared with the FRD appliance, the tensile stress (8.77 MPa) occurred in the anterior of condylar neck, and the compressive stress (−6.611 MPa) occurred in the posterior area. In the simulation of the screwed-TFBC appliance, the tensile stress (9.07 MPa) occurred in the anterior of the condylar neck, and the compressive stress (−7.577 MPa) occurred in the posterior area.
The areas with the minimum principal stresses, which get low negative ratings in the articular disc, were observed in the anterior area of the surface of the articular disc facing the condyle in the FRD and screwed-FRD models. They were observed however in the posterior area of the disc facing the condyle in TFBC and screwed-TFBC models. The dominant type of stress in these areas is compressive. The areas with the maximum principal stresses, which get high positive ratings, were observed in the posterior area of the disc facing the condyle in the FRD and screwed-FRD models. They were observed however in the anterior area of the disc facing the condyle in the TFBC and screwed-TFBC models. The dominant type of stress in these areas is tensile.
In the simulations of the FRD and screwed-FRD models, the compressive stress (FRD: −0.190 MPa, screwed-FRD: −0.114 MPa) occurred in the anterior area of the disc facing the condyle, and the tensile stress (FRD: 0.247 MPa, screwed-FRD: 0.135 MPa) occurred in the posterior area. However, in the simulations of the TFBC and screwed-TFBC appliances, compared with the FRD appliance, the tensile stress (TFBC: 1.256 MPa, screwed-TFBC: 1.230 MPa) occurred in the anterior area of the disc facing the condyle, and the compressive stress (TFBC: −1.184 MPa, screwed-TFBC: −1.239 MPa) occurred in the posterior area.
In all the models, the areas with the minimum principal stresses, which get low negative ratings in the maxilla, were observed in the buccal area of the socket of the first upper molar. The dominant type of stress in these areas is compressive. The areas in the FRD, screwed-FRD, TFBC, and screwed-TFBC models with the maximum principal stresses, which get high positive ratings, were observed in the palatinal area of the first upper molar.
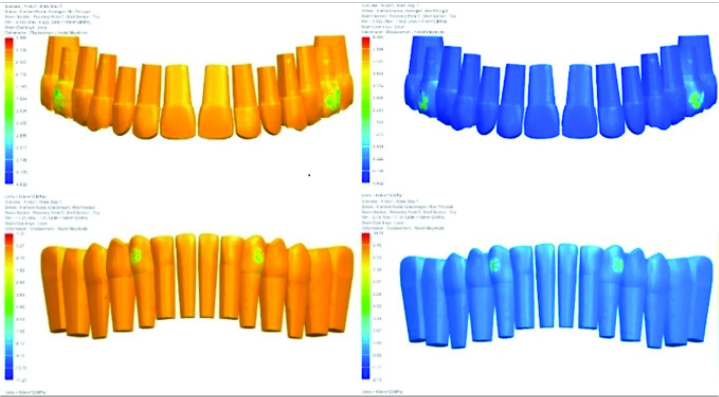
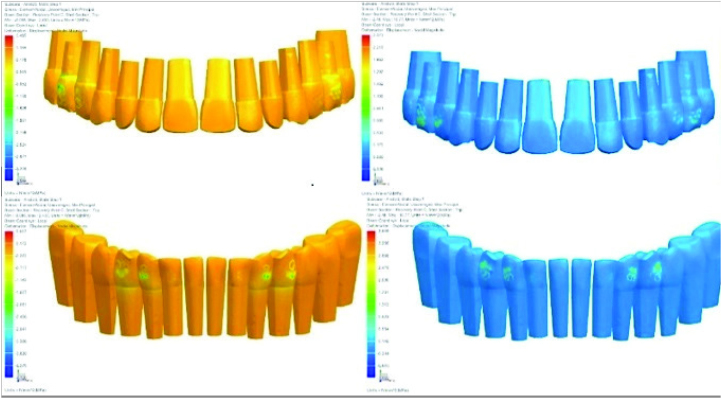
It was observed in all the models that the intensities of minimum and maximum principal stresses in the neck areas of the first upper molar were increased. In the screwed models, particularly in the screwed-FRD model, the minimum and maximum principal stresses in the upper lateral teeth were significantly high (Figure 4, 5).
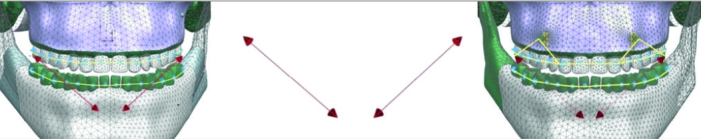
Figure 4.
The minimum principal and maximum principal stress ratings of maxillary and mandibular teeth in the model of the FRD appliance (in order of from left to right)
FRD: fatigue resistance device
Figure 5.
The minimum principal and maximum principal stress ratings of maxillary and mandibular teeth in the model of the TFBC appliance (in order of from left to right)
TFBC: twin-force bite corrector
DISCUSSION
In a study by Gupta et al. (27), the highest post mandibular protraction stress was observed in the posterior area and posterio-superior areas of the condyle, and the stress was determined in this area to be tensile. Compressive stress occurred in the anterio-superior areas of the condyle and a resorptive area developed in this region. Similarly, Zhou et al. (25) examined the cartilage structures of the condyle using 3-D finite element analysis (FEM) after the mandibular protraction. After simulation of the mandibular protraction, they reported that tensile stresses occurred in the posterior areas of cartilage surfaces of the condyle. In our study, similar to these two studies, we observed the highest tensile stress in the posterior area of the condyle and the highest compressive stress in the anterior area of the condyle for the FRD and screwed-FRD appliances. We reached different conclusions in the models of TFBC and screwed-TFBC and we this difference is attributed to the appliance’s more vertical components and consequently, to the application of more vertical force.
In all the models, the minimum principal stress (FRD: −2.025 MPa, screwed-FRD: −1.627 MPa, TFBC: −1.525 MPa, and screwed-TFBC: −1.074 MPa) in the buccal neck of the first upper molar is more active; hence, the compressive stress is observed in the buccal of the first upper molar teeth. In these models, the maximum principal stress (FRD: 1.749 MPa, screwed-FRD: 1.370 MPa, TFBC: 0.686 MPa, and screwed-TFBC: 0.481 MPa) in the palatinal neck of the first upper molar is more active and hence the tensile stress is observed in the palatinals of the first upper molar teeth. It is suggested that these stresses occur in the neck area of the first upper molar due to the expansive force applied to the tooth by appliances. According to the principal stress ratings, the FRD appliance has more expansive effect than the TFBC appliance. Furthermore, the FRD appliance has a more expansive effect than the screwed-FRD appliance, and the TFBC appliance has more expansive effect than the screwed-TFBC appliance. According to these results, it is suggested that the support of miniscrews decreases the undesired expansive effect that occurs on the first upper molar tooth.
In all the models, the minimum principal stress (FRD: −1.594 MPa, screwed-FRD: −1.043 MPa, TFBC: −0.852MPa, screwed-TFBC: −0.570 MPa) in the distal neck of the first upper molar is more active and hence the compressive stress is observed in the distal of the first upper molar teeth. We believe that these stresses on the first upper molar tooth occur due to the distalization force applied by the appliances on the tooth. According to the principal stress ratings, the FRD appliance has more effect than the TFBC appliance, which causes molar distalization. We believe that the reason for this outcome is that the FRD appliance applies a primarily horizontal and direct force on the first upper molar tooth and the TFBC appliance applies a primarily vertical force on the arc wire. Furthermore, the FRD appliance causes greater distalization than the screwed-FRD appliance, and TFBC appliance has more effect to cause distalization than the screwed-TFBC appliance. According to these results, it is suggested that the support of miniscrews decreases the undesired distalization that occurs on the first upper molar tooth.
In all models, the minimum principal stress (FRD: −0.79 MPa, screwed-FRD: −0.90 MPa, TFBC: −1.162 MPa, and screwed-TFBC: −1.487 MPa) is more effective in the buccal neck of the lower canine and hence the compressive stress is observed in the buccal neck of the canine teeth. This compressive stress occurs in the lower canine teeth because of the force resulting in the protrusion of the lower incisors. According to the data, maximum protrusion of lower incisors is observed in the screwed-TFBC model, minimum protrusion of the lower incisors are observed in the FRD model, and the TFBC appliance causes more protrusion of the lower incisors than the FRD appliance. This result is considered to occur because the molar distalization is less with the TFBC appliance. Unscrewed appliances cause less protrusion of the lower incisors than the screwed appliances. This result is considered to have occurred because the anchorage rating has increased in the maxillary teeth due to the miniscrews.
In a clinical study, Aslan et al. (28) compared the FRD and screwed-FRD appliances. They placed miniscrews between the lower canine and the first lower premolar teeth and secured the miniscrew into the lower canine tooth. The first upper molar distalization of 1.45 mm was observed with the FRD appliance; however, the first upper molar distalization of approximately 2.11 mm was observed in the screwed-FRD appliance. In this study, the anchorage of the mandibular dental arc increased and the molar distalization observed in the screwed-FRD appliance was more than the FRD appliance. Although the mandibulary anchorage was observed to be increased in the study by Aslan et al., the maxillary anchorage was increased in our study and in the screwed models; the upper molar distalization is increased in the study by Aslan et al. (28), whereas protrusion of the lower incisors was increased in our study. The result of this study was consistent with our findings.
It is determined that screwed Forsus and screwed Twin-Force appliances can be used to prevent unwanted molar distalization and expansion of the upper molars, but precautions should be taken for lower incisor protrusions. Our study showed that miniscrews can be inserted into the mandible to prevent lower incisors protrusion.
CONCLUSION
The FRD appliance has more expansive effect on the upper molar area than the TFBC appliance. Furthermore, unscrewed models have more expansive effect than the screwed models. Based on these conclusions, the undesired expansive effect on the first upper molar tooth can be decreased through miniscrew support.
High stress ratings were observed in the condyle neck.
In the fixed functional appliances, the miniscrew support can decrease the maxillary dental effect and increase the mandibular effect.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Cumhuriyet University.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - H.A., C.D.; Design - H.A., C.D.; Supervision - H.A., C.D.; Resources - H.A., C.D.; Materials - H.A., C.D.; Data Collection and/or Processing - H.A., C.D.; Analysis and/or Interpretation - H.A., C.D.; Literature Search - H.A., C.D.; Writing Manuscript - H.A., C.D.; Critical Review - H.A., C.D.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.O’Brien K, Wright J, Conboy F, Sanjie Y, Mandall N, Chadwick S, et al. Effectiveness of treatment for Class II malocclusion with the Herbst or Twinblock appliances: a randomized, controlled trial. Am J Orthod Dentofacial Orthop. 2003;124:128–37. doi: 10.1016/j.ajodo.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Ruf S, Pancherz H. Herbst/multibracket appliance treatment of Class II Division 1 malocclusions in early and late adulthood. A prospective cephalometric study of consecutively treated subjects. Eur J Orthod. 2006;28:352–60. doi: 10.1093/ejo/cji116. [DOI] [PubMed] [Google Scholar]
- 3.Pangrazio-Kulbersh V, Berger JL, Chermak DS, Kaczynski R, Simon ES, Haerian A. Treatment effects of the mandibular anterior repositioning appliance on patients with Class II malocclusion. Am J Orthod Dentofacial Orthop. 2003;123:286–95. doi: 10.1067/mod.2003.8. [DOI] [PubMed] [Google Scholar]
- 4.Karacay S, Akın E, Olmez H, Gurton AU, Sagdıc D. Forsus Nitinol Flat Spring and Jasper Jumper corrections of Class II division 1 malocclusions. Angle Orthod. 2006;76:666–72. doi: 10.1043/0003-3219(2006)076[0666:FNFSAJ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Jones G, Buschang PH, Kim KB, Oliver DR. Class II nonextraction patients treated with the Forsus fatigue resistant device versus intermaxillary elastics. Angle Orthod. 2008;78:332–8. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 6.Heinig N, Göz G. Clinical application and effects of the Forsus spring. A study of a new Herbst hybrid. J Orofac Orthop. 2001;62:436–50. doi: 10.1007/s00056-001-0053-6. [DOI] [PubMed] [Google Scholar]
- 7.El-Sheikh MM, Godfrey K, Manosudprasit M, Viwattanatipa N. Force deflection characteristics of the fatigue-resistant device spring: an in vitro study. World J Orthod. 2007;8:30–6. [PubMed] [Google Scholar]
- 8.Aras A, Ada E, Saracoglu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–25. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 9.Günay EA, Arun T, Nalbantgil D. Evaluation of the immediate dentofacial changes in late adolescent patients treated with the FRDTM FRD. Eur J Dent. 2011;5:423–32. [PMC free article] [PubMed] [Google Scholar]
- 10.Oztoprak MO, Nalbantgil D, Uyanlar A, Arun T. A cephalometric comparative study of class II correction with Sabbagh Universal Spring (SUS2) and Forsus (FRD) appliances. Eur J Dent. 2012;6:302–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Janssen KI, Raghoebar GM, Vissink A, Sandham A. Skeletal anchorage in orthodontics-a review of various systems in animal and human studies. Int J Oral Maxillofac Implants. 2008;23:75–88. [PubMed] [Google Scholar]
- 12.Farnsworth D, Rossouw PE, Ceen RF, Buschang PH. Cortical bone thickness at common miniscrew implant placement sites. Am J Orthod Dentofacial Orthop. 2011;139:495–503. doi: 10.1016/j.ajodo.2009.03.057. [DOI] [PubMed] [Google Scholar]
- 13.Chen J, Akyuz U, Xu L, Pidaparti R. Stress analysis of the human temporomandibular joint. Med Eng Phys. 1998;20:565–72. doi: 10.1016/S1350-4533(98)00070-8. [DOI] [PubMed] [Google Scholar]
- 14.Pan F, Kau CH, Zhou H, Souccar N. The anatomical evaluation of the dental arches using cone beam computed tomography-an investigation of the availability of bone for placement of mini-screws. Head Face Med. 2013;9:13. doi: 10.1186/1746-160X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panigrahi P, Vineeth V. Biomechanical effects of fixed functional appliance on craniofacial structures. Angle Orthod. 2009;79:668–75. doi: 10.2319/052708-281.1. [DOI] [PubMed] [Google Scholar]
- 16.Katada H, Katada H, Isshiki Y. Changes in orthodontic cephalometric reference points on application of orthopedic force to jaw: three-dimensional finite element analysis. Bull Tokyo Dent Coll. 2005;46:59–65. doi: 10.2209/tdcpublication.46.59. [DOI] [PubMed] [Google Scholar]
- 17.del Pozo R, Tanaka E, Tanaka M, Kato M, Iwabe T, Hirose M, et al. Influence of friction at articular surfaces of the temporomandibular joint on stresses in the articular disk: a theoretical approach with the finite element method. Angle Orthod. 2003;73:319–27. doi: 10.1043/0003-3219(2003)073<0319:IOFAAS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Tanne K, Hiraga J, Kakiuchi K, Yamagata Y, Sakuda M. Biomechanical effect of anteriorly directed extraoral forces on the craniofacial complex: a study using the finite element method. Am J Orthod Dentofacial Orthop. 1989;95:200–7. doi: 10.1016/0889-5406(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 19.Lee NK, Baek SH. Stress and displacement between maxillary protraction with miniplates placed at the infrazygomatic crest and the lateral nasal wall: a 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 2012;141:345–51. doi: 10.1016/j.ajodo.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 20.Beek M, Koolstra J, Van Ruijven L, Van Eijden T. Three-dimensional finite element analysis of the cartilaginous structures in the human temporomandibular joint. J Dent Res. 2001;80:1913–8. doi: 10.1177/00220345010800101001. [DOI] [PubMed] [Google Scholar]
- 21.Erkmen E, Şimşek B, Yücel E, Kurt A. Three-dimensional finite element analysis used to compare methods of fixation after sagittal split ramus osteotomy: setback surgery-posterior loading. Br J Oral Maxillofac Surg. 2005;43:97–104. doi: 10.1016/j.bjoms.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Geramy A, Hassanpour M, Emadian Razavi ES. Asymmetric Outer Bow Length and Cervical Headgear Force System: 3D Analysis Using Finite Element Method. J Dent (Tehran) 2015;12:216–25. [PMC free article] [PubMed] [Google Scholar]
- 23.Tanaka E, Rodrigo D, Tanaka M, Kawaguchi A, Shibazaki T, Tanne K. Stress analysis in the TMJ during jaw opening by use of a three-dimensional finite element model based on magnetic resonance images. Int J Oral Maxillofac Surg. 2001;30:421–30. doi: 10.1054/ijom.2001.0132. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka E, Tanne K, Sakuda M. A three-dimensional finite element model of the mandible including the TMJ and its application to stress analysis in the TMJ during clenching. Med Eng Phys. 1994;16:316–22. doi: 10.1016/1350-4533(94)90058-2. [DOI] [PubMed] [Google Scholar]
- 25.Zhou X, Zhao Z, Zhao M. Analysis of the condyle in the state on the mandibular protraction by means of the three-dimensional finite element method. Zhonghua Kou Qiang Yi Xue Za Zhi. 1999;34:85–7. [PubMed] [Google Scholar]
- 26.Hyung SY, Baik HS, Sung SJ, Kim KD, Cho YS. Three-dimensional finite-element analysis of maxillary protraction with and without rapid palatal expansion. Eur J Orthod. 2007;29:118–25. doi: 10.1093/ejo/cjl057. [DOI] [PubMed] [Google Scholar]
- 27.Gupta A, Kohli VS, Hazarey PV, Kharbanda OP, Gunjal A. Stress distribution in the temporomandibular joint after mandibular protraction: a 3-dimensional finite element method study. Part 1. Am J Orthod Dentofacial Orthop. 2009;135:737–48. doi: 10.1016/j.ajodo.2007.12.025. [DOI] [PubMed] [Google Scholar]
- 28.Aslan BI, Kucukkaraca E, Turkoz C, Dincer M. Treatment effects of the Forsus Fatigue Resistant Device used with miniscrew anchorage. Angle Orthod. 2013;84:76–87. doi: 10.2319/032613-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]