Abstract
Introduction:
Findings from previous studies indicated patients with mental illness feel pharmacists do not provide appropriate care. In addition, many patients with mental illness report not having a strong relationship with their pharmacist. The objective of this study was to determine the level of social distance of student pharmacists toward patients with mental illness.
Methods:
Student pharmacists completed an anonymous survey. Data were collected using the Bogardus Social Distance Scale (SDS). Level and correlates of social distancing were examined.
Results:
Incomplete surveys were excluded, resulting in 334 completed surveys. A total of 276 students (83%) had an SDS score ≥14, indicating social distancing. There was no statistical difference noted in social distancing between students and year of training (P = .482). The greatest social distancing was in relation to trusting someone with mental illness to “care for their child,” where less than 1 in 5 students (17%) were willing to do this. Most students (88%) were willing to work or be neighbors with someone with mental illness, indicating less social distancing in these domains. Regression analysis indicated a significant change in sum score with knowing someone or having a first-degree relative with mental illness.
Discussion:
Results indicate social distancing is prominent among pharmacy students. Results may be used in the future to help identify solutions for improving social distancing and increasing pharmacy student interaction to patients with mental illness. Further training related to mental illness may assist with decreasing social distancing among pharmacy students.
Keywords: social distancing, mental illness, pharmacy education
Introduction
Many pharmacists, especially those in the community setting, interact with patients with mental illness. Literature1,2 describes the benefits pharmacists may have for monitoring, recommendations, and patient education related to psychiatric conditions. Despite historically positive reviews, 75% of mental health patients reported not receiving effectiveness or safety monitoring education from their pharmacist. In the same survey, 43% of patients reported not having a strong relationship with their pharmacist.3 Social distance, stigma, and attitudes may affect clinical outcomes in the care of mental illness.4-6 Research7 has shown pharmacists endorsed social distance toward patients with mental illness. Increased education and training in mental health literacy and counseling can positively affect the quality of care offered by pharmacists.5,6 Therefore, investing resources into pharmacy training involving mental illness may be associated with increased comfort in providing care for those with mental illness, potentially leading to better health care outcomes.
Social distance is measured to distinguish the level of closeness or separation one group has for another. The Bogardus Social Distance Scale (SDS) is a psychologic test to empirically measure one's willingness to participate in social contacts of varying degrees of closeness with members of diverse racial and ethnic groups.8 This scale was used to assess social distancing among pharmacy students enrolled in psychiatric electives, which demonstrated improvement in social distance scores after course completion.9,10 Because pharmacy students are future health care providers, measuring their social distance may give an indication of educational opportunities necessary to improve care with patients with mental illness. Pharmacy education may increase student pharmacists' comfort working with and communicating effectively with patients with mental illness.
The purpose of this study is to determine the level of social distance of student pharmacists toward patients with mental illness. Secondary objectives include analyses on the effects of year of study and demographic variables on social distancing.
Methods
Design
This was a cross-sectional survey administered to student pharmacists within the P1 (first year), P2 (second year), P3 (third year), and P4 (fourth year) classes during the fall semester. Administration of the survey was approved by the Institutional Review Board (IRB No. 204569; August 24, 2015).
Questionnaire Development
Minimal demographic characteristics were collected to ensure anonymity. Students were asked questions pertaining to previous mental health experience (Table 1). The survey included questions from the SDS11:
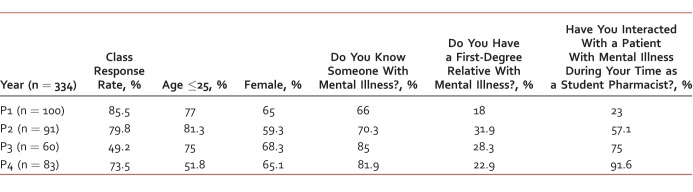
TABLE 1.
Demographic characteristics of the pharmacy student sample by year
Would you share a living space with someone with mental illness?
Would you work with someone with mental illness?
Would you live next door to someone with mental illness?
Would you have someone with mental illness babysit your child?
Would you be comfortable with one of your children marrying a person with mental illness?
Would you introduce someone who has mental illness to a friend as a relationship partner?
Would you recommend someone with mental illness for a job?
With the SDS, students were asked to rate items 1 = definitely willing, 2 = willing, 3 = not willing, and 4 = definitely not willing. Responses added together provide a sum score. Social Distance Scale scores <14 suggest students are probably willing to interact with people with mental illness.12 Scores ≥14 suggest social distance to the mentally ill population. The highest possible score is 28.
Survey Administration
Students within the P1 to P3 years were asked to complete the anonymous paper survey during a class period. Students in the P4 year were emailed a link for an electronic survey through SurveyMonkey,13 which remained accessible for 8 days. Participation was voluntary. Students were prompted with instructions for survey completion. Quick responses to the questions were encouraged for initial reactions. The students were prompted to proceed through the survey without delay.11
Analytic Strategy
Data were entered into SPSS 21.0 (Chicago, IL), and descriptive statistics were obtained. Paired t tests were used for differences between classes and a P value below .05 was considered significant. Results were grouped for each year to assess for a difference in social distancing among student pharmacists in different years. Linear regression analysis was conducted to examine the correlation of social distance with demographic variables (age, sex, degree of relationship and interaction with someone with mental illness; Table 2). Linear regression analyzed variables with the continuous SDS sum score.
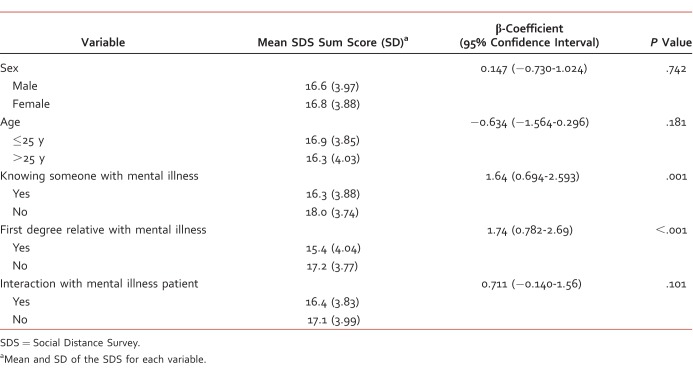
TABLE 2.
Linear regression analysis between variable and social distance
Results
Incomplete surveys (n = 39) were excluded, resulting in 334 students in the P1 to P4 years completing demographic information and SDS portions of the survey. Baseline characteristics are listed in Table 1. Most of the population was female, younger than 25 years, and knew someone with mental illness but was not related to him or her by first degree. More than half of the population reported that they interacted with patients with mental illness during their time as a student pharmacist.
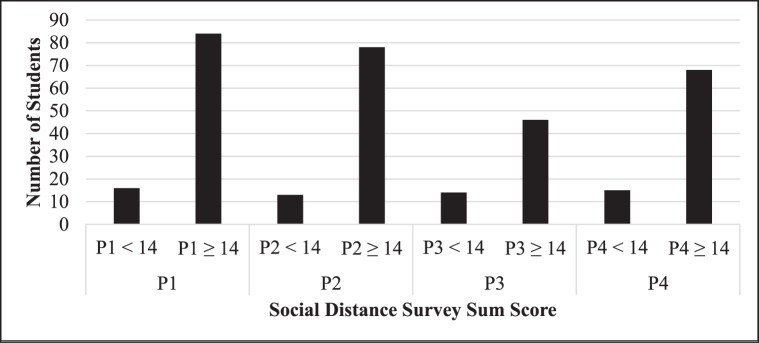
Social distancing (SDS score ≥14) was reported by 276 students (83%; Figure). When separating by class, 84% of the P1 class, 86% of the P2 class, 77% of the P3 class, and 82% of the P4 class suggest social distancing. No statistical difference was noted in the proportion of students in differing classes with SDS scores of >14 (P = .482). The P4 class indicated a high percentage (92%) of interacting with patients with mental illness (Table 1). Per linear regression, sex, age, year, and previous interaction with patients with mental illness were not associated with social distancing. However, knowing someone or being related to someone with a mental illness was associated with decreased social distancing (Table 2).
FIGURE.
Social Distance Survey sum scores by class
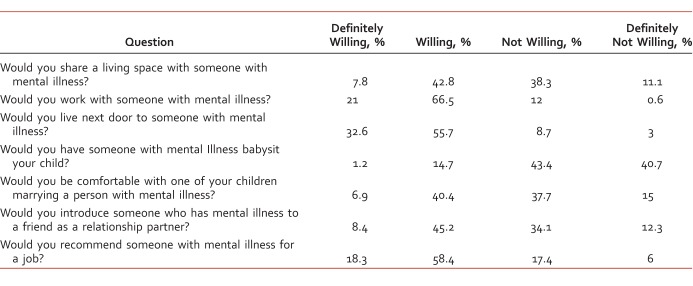
Greatest social distancing was related to trusting someone with mental illness to babysit his or her child. Most were not willing (n = 145; 43.4%) or definitely not willing (n = 136; 40.7%) to have someone with mental illness babysit his or her child. The least social distance involved working with (n = 292; 88%) and being neighbors with (n = 295; 88%) someone with mental illness, indicating these students were the most comfortable interacting with individuals in these capacities. Additional findings are noted in Table 3.
TABLE 3.
Social Distance Survey responses
Discussion
Key Findings
Results indicate social distancing is prominent among students, as evidenced by a score of ≥14. Knowing someone and having a first-degree relative with mental illness can be correlated with a decrease in SDS sum scores. This suggests those with no previous exposure to mental illness through family and friends may be a target for additional training that aims to reduce social distancing. Despite increased didactic mental health curriculum and increased experience with patients with mental illness, this study suggests there was no difference found in social distancing between classes. These findings suggest increasing contact alone is not sufficient to address social distance, and other interventions besides curricular changes may be required. The results of this study conflict with previous research that has demonstrated contact-based education has been shown to be an effective method of reducing stigma during pharmacy education.14 One possible explanation for the difference is the differing definitions of contact-based education; contact-based education in the previous study was designed in advance with structured goals and objectives, while contact-based education with this institution was only defined through personal experience or experiential education.14
Previous research15 has highlighted social contact as the most effective intervention to reduce short-term stigma. There is limited evidence for long-term benefits of social contact for decreasing stigma.15 Incorporation of mental health activities earlier in the program or an increase of availability for advanced practice rotations may provide short-term reduction in social distancing. Small changes using already designated hours for mental health within a curriculum may incorporate novel teaching techniques. Using a Web-based education tool, computer-mediated interventions, and active learning simulations have been shown to decrease stigma and social distancing for student pharmacy education.16-18
Strengths and Validity
A strength of this study was the high response rate. With regard to validity, results can be extrapolated to other colleges of pharmacy with a similar mental health curriculum. All students were offered the voluntary survey once and could opt out at their discretion. Students absent on the day of administration did not have another opportunity to take the survey. Results indicate the P3 class was less socially distant to patients with mental illness; however, only 50% of the student population completed the survey. In comparison with other classes, the participation rate was substantially lower (Table 1).
Limitations
This descriptive study explored the first step of identifying social distancing at this institution. Social distance toward mental illness is difficult to measure objectively. The survey was designed to give the first reaction when posed with a social situation. The term mental illness can be interpreted in different ways, and participants may have been affected by their own knowledge or experiences with mental illness. Investigators chose to leave the term mental illness undefined in order to obtain a more instinctual response to the questions regarding preconceived notions of mental illness. Another limitation includes the SDS score threshold. Consistent with a previous study,12 the investigators chose 14 as a SDS score threshold indicating social distance. The investigators recognize a score of 14 conveys students are “willing” to engage in social activities, but it assumes there is still a degree of hesitancy to select “definitely willing” on the survey. Another limitation relates to challenges equating social distancing to pharmacy practice. Although the SDS is a validated and reliable tool, it cannot be used as a surrogate marker for quality of care.12,19 A final limitation is that this project was conducted in a single school in one geographic location, and the generalizability to other schools or locations is unknown.
Future Direction
Because results identified a high percentage of students who were socially distant to patients with mental illness, future studies will examine whether more experiences and/or novel teaching modalities will decrease social distancing relating to mental illness. Possible considerations for change include incorporation of mental health education and interaction through audiovisual materials, documentaries, guest speakers, or contact-based education in the P1 or P2 years. An elective is currently offered for P3 students to increase knowledge of mental illness and treatment considerations. The incorporation of further training programs may be considered to adequately train students on how to respond and communicate with patients with mental illness.20,21 Training related to mental illness may assist with decreasing social distancing among pharmacy students, including specifically targeting those with no previous exposure to mental illness through family and friends, where the greatest social distancing was reported.
Conclusion
This study assessed the level of social distancing within student pharmacists at one institution. Survey results indicate that social distancing is prominent among student pharmacists at this institution. No differences were noted between students in earlier versus later professional program years. Knowing someone and having a first-degree relative correlated with a statistically significant change in SDS score. Results serve as a baseline for future studies to examine whether teaching modalities decrease social distancing related to mental illness, allowing opportunities to improve patient care.
Footnotes
Disclosures: The authors have nothing to disclose.
References
- 1. Bell S, McLachlan AJ, Aslani P, Whitehead P, Chen TF. . Community pharmacy services to optimise the use of medications for mental illness: a systematic review. Aust New Zealand Health Policy. 2005; 2: 29 DOI: 10.1186/1743-8462-2-29. PubMed PMID: 16336646; PubMed Central PMCID: PMC1345690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bostwick JR, Burghardt K, Choe HM, Deneke E, Fluent T. . Opportunities to partner with clinical pharmacists in ambulatory psychiatry. Curr Psychiatr. 2014; 13 7: 23- 9. [Google Scholar]
- 3. National Alliance on Mental Illness [Internet]. Arlington (VA): c2016 [updated 2012. December 13; cited 2015 Sept 10]. Available from https://www.nami.org/Press-Media/Press-Releases/2012/NAMI-CPNPF-Survey-Finds-75-Percent-of-Individuals
- 4. Rickles NM, Dube GL, McCarter A, Olshan JS. . Relationship between attitudes toward mental illness and provision of pharmacy services. J Am Pharm Assoc. 2010; 50 6: 704- 13. DOI: 10.1331/JAPhA.2010.09042. PubMed PMID: 21071314. [DOI] [PubMed] [Google Scholar]
- 5. O'Reilly CL, Bell JS, Kelly PJ, Chen TF. . Exploring the relationship between mental health stigma, knowledge and provision of pharmacy services for consumers with schizophrenia. Res Social Adm Pharm. 2015; 11 3: e101- 9. DOI: 10.1016/j.sapharm.2013.04.006. PubMed PMID: 23632161. [DOI] [PubMed] [Google Scholar]
- 6. Liekens S, Vandael E, Roter D, Larson S, Smits T, Laekeman G, et al. Impact of training on pharmacists' counseling of patients starting antidepressant therapy. Patient Educ Couns. 2014; 94 1: 110- 5. DOI: 10.1016/j.pec.2013.09.023. PubMed PMID: 24169022. [DOI] [PubMed] [Google Scholar]
- 7. Liekens S, Smits T, Laekeman G, Foulon V. . Factors determining social distance toward people with depression among community pharmacists. Eur Psychiatry. 2012; 27 7: 528- 35. DOI: 10.1016/j.eurpsy.2010.12.009. PubMed PMID: 21392945. [DOI] [PubMed] [Google Scholar]
- 8. Wark C, Galliher JF. Bogardus Emory. and the origins of the Social Distance Scale. Am Soc. 2007; 38 4: 383- 95. DOI: 10.1007/s12108-007-9023-9. [Google Scholar]
- 9. Dipaula BA, Qian J, Mehdizadegan N, Simoni-Wastila L. . An elective psychiatric course to reduce pharmacy students' social distance toward people with severe mental illness. Am J Pharm Educ. 2011; 75 4: 72 DOI: 10.5688/ajpe75472. PubMed PMID: 21769148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gable KN, Muhlstadt KL, Celio MA. . A mental health elective to improve pharmacy students' perspectives on mental illness. Am J Pharm Educ. 2011; 75 2: 34 DOI: 10.5688/ajpe75234. PubMed PMID: 21519423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bogardus ES. . A social distance scale. Sociol Soc Res. 1933; 17: 265- 71. [Google Scholar]
- 12. Corrigan PW, Edwards AB, Green A, Diwan SL, Penn DL. . Prejudice, social distance, and familiarity with mental illness. Schizophr Bull. 2001; 27 2: 219- 25. DOI: 10.1093/oxfordjournals.schbul.a006868. PubMed PMID: 11354589. [DOI] [PubMed] [Google Scholar]
- 13.SurveyMonkey. 2016 [Internet]. Palo Alto (CA): c1999-2016. [cited. Nov 11]. Available from: http://www.surveymonkey.com.
- 14. Patten SB, Remillard A, Phillips L, Modgill G, Szeto AC, Kassam A, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ. 2012; 12: 120 DOI: 10.1186/1472-6920-12-120. PubMed PMID: 23216787; PubMed Central PMCID: PMC3533989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016; 387 10023: 1123- 32. DOI: 10.1016/S0140-6736(15)00298-6. PubMed PMID: 26410341. [DOI] [PubMed] [Google Scholar]
- 16. Finkelstein J, Lapshin O. . Reducing depression stigma using a web-based program. Int J Med Inform. 2007; 76 10: 726- 34. DOI: 10.1016/j.ijmedinf.2006.07.004. PubMed PMID: 16996299. [DOI] [PubMed] [Google Scholar]
- 17. Finkelstein J, Lapshin O, Wasserman E. . Randomized study of different anti-stigma media. Patient Educ Couns. 2008; 71 2: 204- 14. DOI: 10.1016/j.pec.2008.01.002. PubMed PMID: 18289823. [DOI] [PubMed] [Google Scholar]
- 18. Bamgbade BA, Ford KH, Barner JC. . Impact of a mental illness stigma awareness intervention on pharmacy student attitudes and knowledge. Am J Pharm Educ. 2016; 80 5: 80 DOI: 10.5688/ajpe80580. PubMed PMID: 27402983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Corrigan PW, Green A, Lundin R, Kubiak MA, Penn DL. . Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001; 52 7: 953- 8. DOI: 10.1176/appi.ps.52.7.953. PubMed PMID: 11433114. [DOI] [PubMed] [Google Scholar]
- 20. Mental Health First Aid USA [Internet]. Washington: National Council for Behavioral Health; c 2013. [cited 2016 10 Aug]. Available from: http://www.mentalhealthfirstaid.org/cs/.
- 21. O'Reilly CL, Bell JS, Kelly PJ, Chen TF. . Impact of mental health first aid training on pharmacy students' knowledge, attitudes and self-reported behaviour: a controlled trial. Aust N Z J Psychiatry. 2011; 45 7: 549- 57. DOI: 10.3109/00048674.2011.585454. PubMed PMID: 21718124. [DOI] [PubMed] [Google Scholar]