Abstract
Introduction:
The incidence of posttraumatic stress disorder (PTSD) is common within the population and even more so among veterans. Current medication treatment is limited primarily to antidepressants. Such medicines have shown to produce low remission rates and may require 9 patients to be treated for 1 to have a response. Aside from the Veterans Affairs/Department of Defense guidelines, other guidelines do not recommend pharmacotherapy as a first-line option, particularly in the veteran population. Marijuana has been evaluated as an alternative and novel treatment option with 16 states legalizing its use for PTSD.
Methods:
A systematic search was conducted to evaluate the evidence for the use of marijuana for PTSD. Studies for the review were included based on a literature search from Ovid MEDLINE and Google Scholar.
Results:
Five studies were identified that evaluated the use of marijuana for PTSD. One trial was conducted in Israel and actively used marijuana. Three studies did not use marijuana in the treatment arm but instead evaluated the effects postuse. A retrospective chart review from New Mexico relied on patients to recall their change in PTSD symptoms when using marijuana. Three studies concluded there might be a benefit, but two discouraged its use. Although the two negative studies show a statistical difference in worse PTSD outcomes, clinical significance is unclear.
Discussion:
Conflicting data exist for the use of marijuana for PTSD; however, current evidence is limited to anecdotal experiences, case reports, and observational studies, making it difficult to make clinical recommendations.
Keywords: marijuana, cannabis, treatment, posttraumatic stress disorder (PTSD), pharmacotherapy
Introduction
The 12-month prevalence of posttraumatic stress disorder (PTSD) in the United States is 3.5%.1 This is even higher in the veteran population with an estimated incidence of 24%.2 Approximately 80% of people with PTSD have comorbid psychiatric disorders, and the associated mood, physical, and dissociative symptoms can impair functioning, employment, relationships, and self-care.3,4
Posttraumatic stress disorder is defined as a trauma- and stressor-related disorder. According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), diagnosis is based on the individual being exposed to a traumatic event (criterion A) and then meeting criteria B (intrusive symptoms), C (avoidance), D (negative alterations in cognitions and/or mood), and E (alterations in arousal and reactivity).1 Prior to 2013, per the DSM-IV, criteria C and D were grouped together into avoidance and numbing. The Clinician-Administered PTSD Scale-5 (CAPS-5) is the “gold standard” assessment and can be used for diagnosis. An adequate treatment response is a ≥15-point decrease in total severity score.5 The PTSD Checklist (PCL) is used more often in clinical practice due to its ease of administration, and it can provide a provisional diagnosis. There are multiple versions of the PCL, but only one is validated.6
Changes in pathophysiology have been observed in patients who have PTSD. Brain structural and physiologic abnormalities include increased activity in the amygdala (fear center of the brain), decreased volume in the prefrontal cortex (executive function of the brain), and decreased volume in the hippocampus (memory center of the brain), leading to an increase in fear response, intrusive thoughts, flashbacks, nightmares, impulsivity, and arousal. Additionally, during the trauma, there is a cortisol surge, which causes adrenal exhaustion, and results in dysfunction in the hypothalamic-pituitary axis. This leads to a decreased baseline cortisol level, which then results in an increase in the negative feedback system, leading to hyperarousal and hypervigilance. A dysregulation of neurotransmitters is also present, causing a failure in the stress response system to react, adapt, and recover from a situation. An increase in norepinephrine, decrease in serotonin, and increase in glutamate can contribute to physical, mental, and emotional symptoms of PTSD.2
To target the neurotransmitter imbalance, antidepressants are recommended to treat PTSD. According to the 2010 Veterans Affairs (VA)/Department of Defense (DoD) guidelines, psychotherapy and/or pharmacotherapy with selective serotonin reuptake inhibitors or serotonin and norepinephrine reuptake inhibitors are considered first-line treatment.4 However, the number needed to treat with preferred antidepressants for a response is up to 9 patients.7 Remission rates with pharmacotherapy have been reported to be 20% to 30%.8 A Cochrane review by Stein and colleagues9 showed that combat veterans are even more resistant to pharmacotherapy. The 2005 National Institute for Health and Clinical Excellence guidelines10 do not recommend pharmacotherapy as first-line treatment. Similarly, the 2009 American Psychiatric Association guidelines11 note that pharmacotherapy is not as effective for combat-related trauma compared to civilian PTSD. Given these limitations, the investigation for more effective treatment options has been underway, and the utility of marijuana in alleviating PTSD symptoms has become an area of interest.
As of November 9, 2016, 28 states and the District of Columbia legalized medical marijuana with 16 states approving its use for PTSD.12 However, marijuana is still classified as a schedule I controlled substance federally, meaning it has no current accepted medical use and has a high potential for abuse.13 An addendum was passed by the US House of Representatives allowing VA providers to recommend and share information on medical marijuana in states with approved medical marijuana programs. As of April 2017, the bill is awaiting Senate approval.14 Other legislation has been proposed to remove marijuana from the schedule of controlled substances.15
Marijuana belongs to the Cannabaceae (hemp) plant family and is derived from the plant Cannabis sativa and Cannabis indica. It contains cannabinoids and 18 other classes of chemical compounds. The cannabinoid Δ 9-Tetrahydrocannabinol (THC) is a highly lipophilic alkaloid16,17 and is the primary psychoactive ingredient in marijuana.18 Marijuana can vary in THC content from 0.2% to 30% per plant and strain.19 Cannabidiol is another cannabinoid that produces no psychoactive effects, has antipsychotic properties, and works to minimize the “high” and side effects caused by THC. Cannabidiol has demonstrated neuroprotective, analgesic, sedating, antiemetic, antispasmodic, anti-inflammatory, and anxiolytic properties.16,17
Endogenous chemicals that act on the cannabinoids system are known as endocannabinoids.16 Stimulation of the cannabinoid receptors has been shown to increase stress coping behaviors as well as serotonin and norepinephrine firing in the midbrain.20 Presynaptic cannabinoid (CB)-1 receptors function in conjunction with the adrenergic, cholinergic, and dopaminergic systems by helping regulate the release of neurotransmitters from the axon terminals. THC has the ability to activate dopaminergic neurons in the ventral tegmental area as well as stimulate release of dopamine from the nucleus accumbens.21 Protein-coupled receptors regulate excitatory and inhibitory neurotransmission and, therefore, assist in the role of homeostasis and prevent extreme cortisol excitation.19,22 As cannabinoid receptors are absent in the brain stem, there is minimal risk of lethal overdose.21 The CB-1 receptors are located in the central nervous system and assist in modulating neurotransmitter networks involved in movement, learning and memory, pleasure, mood, pain, and other functions.16,18,19
Similarly, the endocannabinoid system may play a role in PTSD. An increase in availability and decreased agonism of CB-1 receptors has been found in patients with PTSD.13,20,23 Alterations in the receptors have been seen in depression. The stimulation of the receptors in the prefrontal cortex, amygdala, and hippocampus may alleviate anxiety as well as cause sensitization of CB-1 receptor–mediated G-protein signaling in the prefrontal cortex, which may play a role in suicide and suicidal behavior.20 Activating the CB-1 receptors in the amygdala can potentially decrease aversive memories, fear, and anxiety. Stimulating CB-1 receptors in the prefrontal cortex can increase serotonin and, therefore, display antidepressant properties. An increase in neurogenesis, mood, and memory as well as a decrease in hypervigilance, hyperarousal, and intrusive memories and a normalization of cortisol may be seen when CB-1 receptors are agonized in the hippocampus. By stimulating the limbic and paralimbic area, there may be a decrease in amygdala and hypothalamus activity. This could assist in regulating the hypothalamic-pituitary axis and cortisol and, therefore, decrease hypervigilance and hyperarousal.13,20-22 Since marijuana theoretically may be helpful for PTSD symptoms, provides a novel mechanism of action, and has started to gain approval for legal use on the state level, evaluating the literature to ensure effectiveness in PTSD is warranted. Anecdotal benefit has been reported with the use of marijuana for PTSD symptoms as well as suicidality.13,20-22,24
Methods
Between January 5 and March 1, 2016, a comprehensive literature search was conducted on MEDLINE and Google Scholar for published studies evaluating marijuana use for PTSD symptoms. Search items and medical subject headings (MeSH) terms used included “PTSD” or “posttraumatic stress disorder” or “anxiety” and “marijuana” or “medical marijuana” or “cannabis” or “medical cannabis.” From the gathered references, the primary author then identified additional literature that may have been deemed pertinent.
Articles that met inclusion criteria were clinical trials or observational studies that evaluated the effects of marijuana on PTSD symptoms. The studies had to be full-text articles written in the English language. Abstracts, conference presentations, editorials, opinion pieces, news articles, reviews, and studies that evaluated synthetic marijuana were all excluded from the review. The articles that were identified to meet the inclusion criteria were reviewed by the primary author and then analyzed by secondary authors to confirm clinical relevance.
A total of 132 articles were identified with 5 meeting inclusion criteria for this review (Figure).
FIGURE.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram for the systematic review of the evidence of marijuana in the treatment of posttraumatic stress disorder (PTSD)
Results
One study identified actively used marijuana. Roitman and colleagues23 conducted a 3-week, open-label study in Israel of 10 subjects with chronic PTSD (5 combat related), evaluating safety, tolerance, and efficacy of THC on symptoms. Subjects were instructed to use up to 5 mg of THC olive oil sublingually twice daily. Women who were pregnant, nursing, or not using contraception and subjects with suicidal ideation, concurrent psychosis, alcohol use, substance use, or cannabis use within 6 months prior to study entry were excluded. However, 1 patient reported marijuana use and was still included. Urine drug screens were not used for confirmation. The participants were required to be on stable medications for 4 weeks prior to the start of the study. On average, an individual was on 4 different medications with 8 patients being on either clonazepam or lorazepam. The results indicate significant improvement in global symptom severity per the Clinical Global Impression Scale in severity (P < .02) and improvement (P < .03), sleep quality per the Pittsburgh Sleep Quality Index (P < .05), and the Nightmare Effects Survey (P < .002), frequency of nightmares per the Nightmare Frequency Questionnaire (P < .04), as well as hyperarousal per the CAPS (P < .02). Two patients reported complete remission of their nightmares. Mild adverse drug reactions were reported in 4 cases, which include dry mouth, headache, and dizziness.23
A strength of the study is active marijuana use. A limitation is the inclusion of a small sample of Israeli citizens; therefore, generalizability is unclear. The small sample size could have contributed to the lack of difference seen in the CAPS intrusion, avoidance, and total scores. Including individuals without conducting a urine drug screen could potentially bias the results as well, especially in those who are already using marijuana, therefore, making it difficult to control for the type, potency, dose, and frequency of use. Additionally, per the VA/DoD guidelines, using benzodiazepines is not recommended as they have been theorized to interfere with fear conditioning and response, which could potentially worsen recovery from trauma.4 This same concept may be applied to the Roitman study, which may be why a decrease in arousal was observed. Being an observational study is also a limitation given no comparison to placebo. The short duration of the study does not provide much insight into the long-term benefits or risks with the use of marijuana as well as the possibility of tolerance development.
The next 4 studies discussed were all conducted in the United States and subjects were not actively using cannabis. Rather, investigators were evaluating effects of PTSD symptoms postmarijuana use. Tull and colleagues25 conducted a prospective trial assessing the effects of marijuana on immediate emotional response. Included were 202 participants, with and without PTSD, admitted to a substance use disorder (SUD) treatment facility. The data collected were part of a larger study, and thus those included had co-occurring stimulant, cocaine, or alcohol use disorders. During the first session, baseline interviews were conducted evaluating the PTSD diagnosis, SUD, marijuana withdrawal, frequency of use, and other psychiatric disorders. Then participants were instructed to discuss in detail the traumatic event as well as their feelings during the experience, which was tape-recorded for the investigators to create a 1-minute script. During the second session, subjects listened to the script and were instructed to imagine the event taking place in real time. Subsequently, the emotional and biological reactivity was evaluated.25
No significant differences in baseline characteristics were reported between groups. Per the Negative Affect Scale, which is a subscale of the Positive and Negative Affect Scale, patients with PTSD and no history of marijuana use showed a statistically greater increase in negative affect pretrauma to posttrauma script compared to all other groups (P = .048) after controlling for age, number of anxiety disorders, number of potentially traumatic events, and borderline personality disorder. The marijuana-dependent group showed no significant difference in negative affect reactivity regardless of their PTSD status (P = .99). When evaluating biological reactivity, there was no significant difference seen in saliva cortisol levels regardless of diagnosis of PTSD or marijuana use. Vital signs were not measured through the course of the study. The authors concluded co-occurring PTSD and marijuana dependence may exhibit dampened subjective emotional response to trauma due to reduced amygdala activation.25
Some strengths of the study include having an active versus control design, including participants with co-occurring psychiatric conditions (with the exception of psychosis), making the study more externally valid; adjustment for confounders; and having no difference in PTSD symptoms or marijuana use within groups. Some disadvantages include having a controlled environment and, therefore, no active marijuana use. This may be the reason why cortisol levels were not affected as predicted. Also, a robust difference might not have been seen because the study was not powered to show a difference. Not all baseline characteristics were reported, which puts into question the internal validity. There may have also been variability on marijuana potency, content, components, and use patterns between users, which can result in variability in the amount of marijuana in the body. Additionally, the investigators did not fully account for factors affecting cortisol levels, such as medications, physical health, and collection time. Including patients with only substance use can affect external validity. Elderly individuals were excluded as well. Last, it was unclear if the investigators were blinded.
Greer and colleagues26 conducted a retrospective chart review evaluating the effects of marijuana on global PTSD symptoms. Eighty patients applying to the New Mexico medical marijuana program from mid-2009 to late 2011 were included if they were ≥18 years old; experienced a trauma; had several symptoms in criteria B, C, and D per DSM-IV; and reported significant relief of several major PTSD symptoms as well as lack of harm or problems in functioning with marijuana use. After subject selection, a telephone screen was conducted asking patients to answer questions based on the CAPS-IV retrospectively from a time when they were not using marijuana and a time when they were. The baseline total CAPS score was 98.8 ± 17.6 and then decreased to 22.5 ± 16.9 after marijuana use (average duration of marijuana use was not reported). The results showed a significant reduction in total CAPS score as well as criteria B, C, and D pre and post marijuana use (P < .0001). From this, the authors26 concluded marijuana use resulted in 75% reduction in all area clusters of PTSD criteria as well as total score.
The advantages of this study were that it was powered to show a significant difference, and the patients were their own controls. A major limitation is the selection bias of including individuals who reported significant relief of several major PTSD symptoms as well as lack of harm with marijuana use. This would lead the audience to expect a benefit and questions external applicability. Baseline characteristics were not provided, questioning the external and internal validity. Another disadvantage is the participants included did not have a PTSD diagnosis; rather they had to have several cluster symptoms. Additionally, the participants retrospectively assessed their symptoms pre and post marijuana use to generate CAPS scores leading to recall bias.
Two studies evaluated the effect of marijuana use on long-term PTSD symptoms. Bonn-Miller and colleagues27 conducted a prospective longitudinal study in 260 male combat veterans, not successfully treated outpatient and admitted to a residential rehabilitation program for PTSD at the VA Palo Alto Health Care System from 2000 to 2008. Throughout the course of the program, cognitive behavioral therapy was provided in a group setting. Relapse prevention was embedded into the curriculum, and those with SUD were encouraged to attend 12-step, self-help meetings. There was no difference found in baseline PCL scores between those with and without cannabis use disorder (CUD) with a baseline PCL-M score of 66.25 ± 10.3. The results indicated there was a significantly lower level of change in total PCL scores, criteria C, and criteria D in patients with CUD (P < .05 for all) with a difference in score of 4.25, 1.8, and 1.56, respectively. Therefore, the authors concluded that CUD was associated with worse PTSD treatment outcomes.27
The advantages of the study were that there was a comparison group, there was no difference in PTSD severity at baseline, and the investigators adjusted for variables (age, trauma severity, psychological distress, co-occurring SUD). The drawbacks were that there was no active marijuana use, making it difficult to connect marijuana with current PTSD symptoms. Additionally, last cannabis use was not reported, and withdrawal symptoms were not accounted for. As Bonn-Miller and colleagues27 conducted an observational study, causality cannot be determined by the results. Although statistical significance was reported, the change in PCL score was far less than 10 points, making the results not clinically significant. Other factors, such as participating in therapy or baseline severity of PTSD symptoms, are factors that can intensify symptoms. Some baseline characteristics were not reported between groups, which affects internal validity. It is possible that clinical significance was not found between groups in intrusive symptoms because power was not reached. External validity can be put into question as the patient population was only male veterans in California with severe PTSD.
Similarly, Wilkinson and colleagues28 conducted a retrospective, longitudinal, observational study evaluating the effects of long-term marijuana use on PTSD symptoms. Those included were 2276 veterans admitted to intensive PTSD VA treatment programs from 1992 to 2011 with severe PTSD. Patients were classified into 4 groups based on marijuana use before and after discharge: never users, stoppers, continuing users, and starters. Participants were evaluated at baseline and then again 4 months postdischarge. After adjusting for covariates, it was found that starting marijuana worsened PTSD symptoms by a moderate effect size of +0.34, and stopping marijuana improved PTSD with a small effect size of –0.18. There was a significant association between the days marijuana was used and change in PTSD symptoms per the Mississippi Scale for Combat-Related PTSD (P < .001); severity of violent behavior on the 4-item, self-reported questionnaire from the National Vietnam Veterans' Readjustment Study (P = .0054); alcohol use per the Addiction Severity Index (ASI) (P < .001), and drug abuse per the ASI (P < .001). At follow-up, stoppers and never users had lower levels of PTSD symptoms, and starters had the highest levels of violent behavior.28
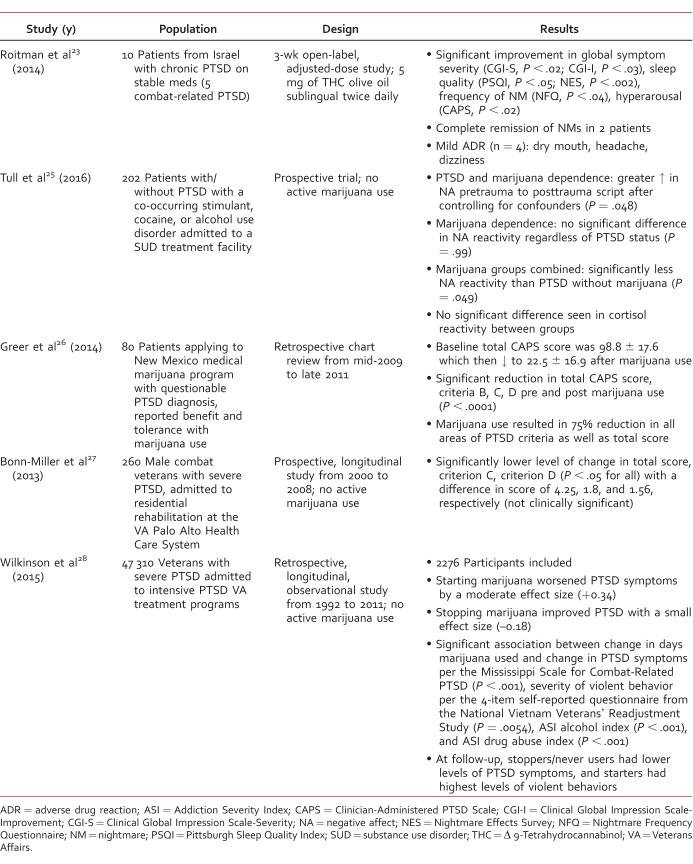
Having a large sample size, a longitudinal design, and a nationwide population were strengths of the study. However, external validity is questionable as primarily older white male veterans with severe PTSD and no other SUD were included. Other limitations include being an observational study and no active marijuana use, making it difficult to associate marijuana to study results. Additionally, drug use was a self-reported measure and not verified by urine drug screens; therefore, patients in all groups could have been using substances in addition to marijuana. The authors did not account for marijuana withdrawal during the treatment program period, which may have an effect on PTSD symptoms. Because the study was retrospective, it was based on chart reviews, and therefore, the potential for lack of documentation is a concern. Last, the study outcomes assessed may have been biased. The ASI questionnaire includes marijuana as a substance, which suggests that those who used marijuana have a SUD. Although statistical significance was seen with less improvement in PTSD symptoms with marijuana use, clinical significance is questionable as values between groups differed by a maximum of 3.03 points out of a 55-point scale. Rather, the large number of participants in the study may explain the statistical significance seen. The Table summarizes the studies discussed.
Table.
Summary of current studies evaluating marijuana for posttraumatic stress disorder (PTSD)
Discussion
Currently available literature examining marijuana use in PTSD suggests potential benefit for a variety of PTSD symptoms. However, all studies have major limitations as none have yet been randomized, controlled, clinical trials with active marijuana use. Because marijuana is a schedule I controlled substance, conducting clinical trials has been extremely difficult.15,18 One would need approval from the Drug Enforcement Administration, US Food and Drug Administration, and local institutional review board as well as the University of Mississippi National Institute on Drug Abuse to receive federally grown marijuana. Bonn-Miller and colleagues29 have been granted approval to conduct a placebo-controlled, triple-blind, randomized crossover pilot study evaluating the safety and efficacy of five potencies of smoked or vaporized marijuana in 76 veterans with chronic PTSD. This would be the first study of its kind.
Despite possible benefit, safety with marijuana use needs to be considered. There is a concern with developing CUD, especially in such a vulnerable population in which substance use and addiction is common. There is currently a high prevalence of marijuana use in those with PTSD. A national retrospective review by Cougle and colleagues30 showed that out of 5672 US adults, 65% with PTSD versus 41% without PTSD used marijuana. In 2009, 30% of veterans within the VA with a PTSD diagnosis also had CUD; however, cannabis was not approved in any state for medical use at that time.27
As the growth and distribution of marijuana is currently poorly regulated, there is large variability in pharmacokinetics and pharmacodynamics depending on the strain, potency, and route of administration used.17 This is a concern as dosing cannot be standardized and, therefore, is difficult to recommend. The variability potentially makes side effects unpredictable. There are cardiovascular adverse effects with marijuana that include an increase in heart rate and cardiac output as well as decrease in blood pressure and peripheral vascular resistance. Although there are conflicting reports, possible large airway obstruction and cellular inflammatory abnormalities in bronchial epithelium as well as respiratory symptoms may occur.19 The potential for cognitive adverse reactions that are known with marijuana use could hinder recovery. Some of these effects include decrease in psychomotor activity and response, short-term memory, motivation, and ability to learn new concepts. Theoretically, those cognitive effects could contribute to numbing and avoidance and mimic a benzodiazepine-like effect. There is also a risk of psychotic disorders in patients with high-risk genotypes as well as increase in psychotic symptoms in patients with schizophrenia and like disorders. In individuals with bipolar disorder, marijuana has shown to increase time in affective episode, risk of rapid cycling, and manic symptoms as well as decrease global functioning and remission.19,31 The long-term effects of marijuana are still unknown.16,19
Obtaining marijuana is another barrier as eligibility for medicinal use varies between states. There is no consistency regarding authorized prescribers. Some states do not require a patient-physician relationship to prescribe. Similarly, with the dispensaries, qualifications of authorized personnel to distribute or own a shop are not standardized. There is also a financial barrier to prescribing marijuana as it is not covered by insurance.16,19
Although there are many variables in using natural marijuana, a CB-1 receptor agonist, nabilone, shows promise in improving PTSD symptoms. An open-label clinical trial was conducted to evaluate the effects of nabilone on 47 PTSD patients with treatment-resistant nightmares. Adjunctive use of nabilone resulted in 72% of participants experiencing significant subjective improvement in nightmare intensity, sleep time, quality of sleep, and daytime flashbacks.32 A retrospective evaluation of 104 male inmates with serious mental illness also showed significant improvement in PTSD-associated symptoms, such as nightmares and insomnia.33 Additionally, a randomized, double-blind, placebo-controlled crossover study was conducted to determine nabilone's ability to reduce the frequency and intensity of PTSD-associated nightmares in 10 military personnel. At the end of nabilone treatment, 70% of subjects were considered much improved by study criteria.34 These positive results are indicative of the potential benefit that the mechanism of CB-1 receptor agonism can have on PTSD symptoms.
In summary, a high percentage of patients do not tolerate and/or respond to conventional treatment options for PTSD. The cannabinoid system plays a role in PTSD and may be a novel mechanism for treatment. Marijuana use in patients with PTSD is common and may be associated with self-medicating. It has been theorized that medical marijuana may help with global improvement of PTSD symptoms. Currently, marijuana is not legal for medical purposes on the federal level; however, it is approved for PTSD in various states. Although some positive data exists for the use of marijuana in PTSD, current evidence is limited to anecdotal experiences, case reports, and observational studies, which leads to a lack of quality evidence to currently support the use of marijuana to treat PTSD.
Footnotes
Disclosures: Nothing to disclose concerning possible financial or personal relationships with commercial entities that may have a direct or indirect interest.
References
- 1. American Psychiatric Association. Trauma- and stressor-related disorders: posttraumatic stress disorder. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): American Psychiatric Publishing; 2013. p 271- 80. [Google Scholar]
- 2. Ravindran LN, Stein MB. . Pharmacotherapy of PTSD: premises, principles, and priorities. Brain Res. 2009; 1293: 24- 39. DOI: 10.1016/j.brainres.2009.03.037. PubMed PMID: 19332035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Najavits LM, Ryngala D, Back SE, Bolton E, Mueser KT, Brady KT. . Treatment of PTSD and comorbid disorders. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress studies. New York: Guilford Press; 2009. p 508- 35. [Google Scholar]
- 4. The Management of Post-Traumatic Stress Working Group. VA/DoD clinical practice guideline for management of post-traumatic stress. Washington: Office of Quality and Performance, Department of Veterans Affairs; 2010. [Google Scholar]
- 5. Weathers FW, Keane TM, Davidson JR. . Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001; 13 3: 132- 56. PubMed PMID: 11387733. [DOI] [PubMed] [Google Scholar]
- 6.Weathers FW, Litz, BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2017 [Internet; cited. Oct 11]. Available from: www.ptsd.va.gov.
- 7. Jonas DE, Cusack K, Forneris CA, Wilkins TM, Sonis J, Middleton JC, et al. . Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). Rockville (MD): Agency for Healthcare Research and Quality; 2013. April Report No.: 13-EHC011-EF. [PubMed] [Google Scholar]
- 8. Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontenelle LF, Marmar CR, et al. . Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review. Prog Neuropsychopharmacol Biol Psychiatry. 2009; 33 2: 169- 80. DOI: 10.1016/j.pnpbp.2008.12.004. PubMed PMID: 19141307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stein DJ, Ipser JC, Seedat S. . Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2006; 1: CD002795 DOI: 10.1002/14651858.CD002795.pub2. PubMed PMID: 16437445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Collaborating Center for Mental Health commissioned by the National Institute for Clinical Excellence. Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care [Internet]. National Clinical Practice Guideline 25; 2005. [cited 2016 Feb 27]. Available from: https://www.nice.org.uk/guidance/CG26/chapter/1-Guidance#the-treatment-of-ptsd
- 11. American Psychiatric Association. Practice guidelines for the treatment of patients with acute stress disorder and posttraumatic stress disorder [Internet]. Arlington (VA): American Psychiatric Association, 2004. [cited 2017 Jan 8]. Available from: http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd.pdf [Google Scholar]
- 12. Medical Marijuana [Internet]. ProCon.org: explore pros & cons of controversial issues [updated 2016. February 26; cited 2016 Nov 11]. Available from: http://medicalmarijuana.procon.org
- 13. Belendiuk KA, Baldini LL, Bonn-Miller MO. . Narrative review of the safety and efficacy of marijuana for the treatment of commonly state-approved medical and psychiatric disorders. Addict Sci Clin Pract. 2015; 10: 10 DOI: 10.1186/s13722-015-0032-7. PubMed PMID: 25896576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Military Construction and Veterans Affairs and Related Agencies Appropriations Act of 2017. H. Amdt. 1062 to H.R.4974 [cited 2016. Nov 11]. Available from: https://www.congress.gov/amendment/114th-congress/house-amendment/1062?q=%7B%22search%22%3A%5B%22marijuana+and+veteran%22%5D%7D&r=5
- 15. Marijuana legislation [Internet]. Congress.gov [cited 2016. Nov 11]. Available from: https://www.congress.gov/search?q={%22congress%22%3A%22114%22%2C%22source%22%3A%22legislation%22%2C%22search%22%3A%22Marijuana%20%22
- 16. Horowitz S. . The medical use of marijuana: issues and indications. Altern Complementary Ther. 2014; 20 6: 320- 7. DOI: 10.1089/act.2014.20601. [Google Scholar]
- 17. Huestis MA. . Human cannabinoid pharmacokinetics. Chem Biodivers. 2007; 4 8: 1770- 804. DOI: 10.1002/cbdv.200790152. PubMed PMID: 17712819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tambaro S, Bortolato M. . Cannabinoid-related agents in the treatment of anxiety disorders: current knowledge and future perspectives. Recent Pat CNS Drug Discov. 2012; 7 1: 25- 40. DOI: 10.2174/157488912798842269. PubMed PMID: 22280339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bostwick JM. . Blurred boundaries: the therapeutics and politics of medical marijuana. Mayo Clin Proc. 2012; 87 2: 172- 86. DOI: 10.1016/j.mayocp.2011.10.003. PubMed PMID: 22305029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Krumm BA. . Cannabis for posttraumatic stress disorder. Nurse Pract. 2016; 41 1: 50- 4. DOI: 10.1097/01.NPR.0000434091.34348.3c. [DOI] [PubMed] [Google Scholar]
- 21. Iversen L. . Cannabis and the brain. Brain. 2003; 126 6: 1252- 70. DOI: 10.1093/brain/awg143. PubMed PMID: 12764049. [DOI] [PubMed] [Google Scholar]
- 22. Passie T, Emrich HM, Karst M, Brandt SD, Halpern JH. . Mitigation of post-traumatic stress symptoms by Cannabis resin: a review of the clinical and neurobiological evidence. Drug Test Anal. 2012; 4 7-8: 649- 59. DOI: 10.1002/dta.1377. PubMed PMID: 22736575. [DOI] [PubMed] [Google Scholar]
- 23. Roitman P, Mechoulam R, Cooper-Kazaz R, Shalev A. . Preliminary, open-label, pilot study of add-on oral Δ9-tetrahydrocannabinol in chronic post-traumatic stress disorder. Clin Drug Investig. 2014; 34 8: 587- 91. DOI: 10.1007/s40261-014-0212-3. PubMed PMID: 24935052. [DOI] [PubMed] [Google Scholar]
- 24. Bonn-Miller MO, Babson KA, Vandrey R. . Using cannabis to help you sleep: heightened frequency of medical cannabis use among those with PTSD. Drug Alcohol Depend. 2014; 136: 162- 5. DOI: 10.1016/j.drugalcdep.2013.12.008. PubMed PMID: 24412475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tull MT, McDermott MJ, Gratz KL. . Marijuana dependence moderates the effect of posttraumatic stress disorder on trauma cue reactivity in substance dependent patients. Drug Alcohol Depend. 2016; 159: 219- 26. DOI: 10.1016/j.drugalcdep.2015.12.014. PubMed PMID: 26790822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Greer GR, Grob CS, Halberstadt AL. . PTSD symptom reports of patients evaluated for the New Mexico Medical Cannabis Program. J Psychoactive Drugs. 2014; 468 1: 73- 7. DOI: 10.1080/02791072.2013.873843. PubMed PMID: 24830188. [DOI] [PubMed] [Google Scholar]
- 27. Bonn-Miller MO, Boden MT, Vujanovic AA, Drescher KD. . Prospective investigation of the impact of cannabis use disorders on posttraumatic stress disorder symptoms among veterans in residential treatment. Psychol Trauma. 2013; 5 2: 193- 200. DOI: 10.1037/a0026621. [Google Scholar]
- 28. Wilkinson ST, Stefanovics E, Rosenheck RA. . Marijuana use is associated with worse outcomes in symptom severity and violent behavior in patients with posttraumatic stress disorder. J Clin Psychiatry. 2015; 76 9: 1174- 80. DOI: 10.4088/JCP.14m09475. PubMed PMID: 26455669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bonn-Miller MO, Paula R. . Placebo-controlled triple-blind, randomized crossover pilot study of the safety and efficacy of five different potencies of smoked or vaporized marijuana in 76 veterans with chronic, treatment-resistant posttraumatic stress disorder (PTSD) [Internet]. Multidisciplinary Association for Psychedelic Studies (MAPS) 2015. [cited 2016 Nov 20]. Available from: http://www.maps.org/research-archive/mmj/MJP1-Protocol-Amend4-oct-13-2015.pdf
- 30. Cougle JR, Bonn-Miller MO, Vujanovic AA, Zvolensky MJ, Hawkins KA. . Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychol Addict Behav. 2011; 25 3: 554- 8. DOI: 10.1037/a0023076. PubMed PMID: 21480682. [DOI] [PubMed] [Google Scholar]
- 31. Beech RD. . Medical marijuana: the pitfalls and the pendulum. J Addict Res Ther. 2015; 6: e132 DOI: 10.4172/2155-6105.1000e132. [Google Scholar]
- 32. Fraser GA. . The use of a synthetic cannabinoid in the management of treatment-resistant nightmares in posttraumatic stress disorder (PTSD). CNS Neurosci Ther. 2009; 15 1: 84- 8. DOI: 10.1111/j.1755-5949.2008.00071.x. PubMed PMID: 19228182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cameron C, Watson D, Robinson J. . Use of a synthetic cannabinoid in a correctional population for posttraumatic stress disorder-related insomnia and nightmares, chronic pain, harm reduction, and other indications: a retrospective evaluation. J Clin Psychopharmacol. 2014; 34 5: 559- 64. DOI: 10.1097/JCP.0000000000000180. PubMed PMID: 24987795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jetly R, Heber A, Fraser G, Boisvert D. . The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: a preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology. 2015; 51: 585- 8. DOI: 10.1016/j.psyneuen.2014.11.002. PubMed PMID: 25467221. [DOI] [PubMed] [Google Scholar]