Abstract
Diesel exhaust particles (DEPs), a by-product of diesel engine exhaust (DEE), are known to produce pro-oxidative and pro-inflammatory effects, thereby leading to oxidative stress-induced damage. Given the key role of DEPs in inducing oxidative stress, we investigated the role of DEPs in disrupting the integrity and function of immortalized human brain microvascular endothelial cells (HBMVEC). To study this, HBMVEC cells were exposed to media containing three different concentrations of DEPs or plain media for 24 h. Those exposed to DEPs showed significantly higher oxidative stress than the untreated group, as indicated by the glutathione (GSH) and malondialdehyde (MDA) levels, and the glutathione peroxidase and glutathione reductase activities. DEPs also induced oxidative stress-related disruption of the HBMVEC cells monolayer, as measured by trans-epithelial electrical resistance. Taken together, these data suggest that DEPs induce cell death and disrupt the function and integrity of HBMVEC cells, indicating a potential role of DEPs in neurotoxicities.
Keywords: Diesel engine exhaust, Diesel exhaust particles, oxidative stress, reactive oxygen species, glutathione
1. Introduction
Diesel engine exhaust (DEE) is a complex mixture of organic and inorganic gases (NOx, SOx, CO), particulate matters (PMs), quinones, PAHs, and transition metals. Diesel exhaust particles (DEPs), a by-product of DEE, are one of the major components of airborne particulate matter in the urban environment. They are composed of carbon, heavy carbohydrates, hydrated sulfuric acid, polycyclic aromatic hydrocarbons (PAHs), and their derivatives: quinones, semi-quinones, and trace amounts of heavy metals such as iron, copper, chromium, and nickel (Bai et al., 2001; Vouk et al., 1983; Hartz et al., 2008). DEPs are easily respirable and capable of being deposited in the airways and the alveoli. They can pass through the respiratory tract to enter the circulation, reaching extra pulmonary tissues and having the potential to translocate to other tissues, including the brain by passing through the blood-brain barrier (BBB) (Oberdorster et al., 2002, 2004; Elder et al., 2006; Sugamata et al., 2006). It is believed that they can translocate to the brain via two routes, either through translocation along the olfactory nerve or by crossing the lung-blood barrier and the BBB (Oberdorster et al., 2005; Peters et al., 2006). Peters et al. (2006) have demonstrated that erythrocytes can uptake particles that range in size from 0.02µm to 0.20 µm. It is believed that these particles can penetrate circulating cells, like erythrocytes, and translocate to other organs, including the brain.
Translocation to and accumulation of ultrafine particles in the brain (Oberdorster et al., 2004) are a concern owing to their potential neurotoxic consequences. Epidemiological studies have demonstrated a positive association between particulate matter and a number of diseases that affect the respiratory and cardiovascular systems, as well as the central nervous system (CNS) (Dockery et al., 1993; Pope et al., 1995; Sarnat et al., 2001; Nel et al., 1998; Diaz-Sanchez, 1997; Li et al., 1996). Even though the effects of DEPs on the lungs and cardiovascular system are relatively well-known, and can be linked to oxidative stress in some cases, limited information is available on the effect of DEPs on CNS.
In the last few years, a body of evidence has indicated that ultra-fine particulate matter may cause neurodegenerative diseases like strokes, Parkinson’s, and Alzheimer’s. (Hirtz et al., 2007). Histological evidences indicate neurodegeneration in both canine and human brains that are exposed to high ambient PM levels. In addition, in vivo studies in mice have demonstrated the presence of oxidative stress, toxicity, and inflammation in brain tissue upon inhalation of particulate matter (Peters et al., 2006; Campbell et al., 2005; Elder et al., 2006; Kleinman et al., 2008; Veronesi et al., 2005; Oberdorster et al., 2004, 2005; Block et al., 2004; Hartz et al., 2008). This is further supported by in vitro studies that reported neurotoxic effects on specific brain cells and BBB disruption upon exposure to DEE particles (Block et al., 2004; Hartz et al., 2008; Long et al., 2007). In addition, free radical activity on the PM particle's surface has the potential to disrupt the tight junctions and facilitate particle translocation by damaging the BBB (Peters et al., 2006). Some of the chemical compounds in DEPs, such as quinones, PAHs, and transition metals, may induce reactive oxygen species (ROS) due to their ability to disrupt electron transfer in the inner mitochondrial membrane.
Translocation and accumulation of DEPs in the brain raises concerns about serious health consequences since free radical production and oxidative stress are implicated in the pathogenesis of different neurodegenerative disorders. The need for investigation of the role of DEPs in CNS damage is pressing because of rapidly increasing air pollution worldwide. In lieu of studies supporting the role of DEPs in oxidative stress-induced damage, we evaluated the role of DEPs in inducing oxidative stress in HBMVEC cells and disrupting their integrity and function.
2. Materials and methods
2.1. Materials
DEPs were purchased from NIST (SRM 1650b) (Gaithersburg, MD, USA). N-(1-pyrenyl)-maleimide (NPM) was obtained from Sigma-Aldrich (St. Louis, MO). High performance liquid chromatography (HPLC) grade solvents were purchased from Fisher Scientific (Fair Lawn, NJ). All other chemicals were bought from Sigma-Aldrich (St. Louis, MO).
2.2. Culture of human brain microvascular endothelial cells (HBMVEC) and toxicity studies
As an in vitro BBB model, immortalized human brain endothelial cells, HBMVEC (a gift from Dr. Pierre Courard), were seeded in 25 cm2 tissue culture flasks coated with type 1 rat tail collagen (Sigma-Aldrich, St. Louis, MO) and maintained in EBM-2 medium in humidified 5% CO2/95% air at 37 °C. Culture medium was changed twice a week and endothelial cells at passages 28–34 were used in this study. All assays were performed in triplicate and each experiment was repeated three times. EBM-2 medium (Lonza, Walkersville, MD) was supplemented with VEGF, IGF-1, EGF, basic FGF, hydrocortisone, ascorbate, gentamycin, and 2.5% fetal bovine serum (FBS), as recommended by the manufacturer. This fully supplemented medium was designated as Microvascular Endothelial Cell Medium-2 (EBM-2 MV, herein referred to as EBM-2 medium). For dosing cells with DEPs, we used serum-free and growth-factor-free medium for all experiments instead of the fully supplemented media described above. Cells were treated with DEPs for 24 h for all the studies except for intracellular ROS measurements (3h). DEPs were suspended in phosphate buffered saline (PBS), vortexed, and sonicated for 30 min to give a DEP stock solution concentration of 2mg/ml. In order to test dose-dependency, a DEP working solution was prepared by diluting the stock DEP solution in a serum-free EBM-2 medium. These concentrations of DEPs were selected based on the reconciliation of the in vivo PM exposures, measured in micrograms per cubic meter (µg/m3), with the tissue culture concentrations of DEP chemicals, and measured in micrograms per milliliter (µg/ml). The biologically relevant tissue culture concentration of DEP ranges from 0.2 to 20 µg/cm2 which corresponds to 1.4 to 143 µg/ml (Li et al., 2003). The DEP particle suspension in the tissue culture medium was reported to contain particles between 40 nm and 2.5µm, with a mean particulate diameter of approximately 400 nm (Carero et al. 2001). NIST reports the mean particle size diameter to be 180 nm after 24 h of sonication.
2.3. Determination of cell viability
The effect of DEPs on the viability of HBMVECs was assessed using the MTS assay (CellTiter 96® AQueous One Solution Cell Proliferation Assay, Promega, Madison, WI). MTS tetrazolium was reduced by mitochondrial dehydrogenase into a colored formazan product in proportion to the number of living cells. HBMVECs (3 × 104 cells/well) were seeded in a 96-well tissue culture plate for a day. The medium was then discarded, and the cells were treated with DEPs (10, 25, 50 µg/ml) in serum-free medium for 24 h. CellTiter 96® AQueous One Solution Reagent (20 ìL/well) was added to the wells and the plate was incubated at 37°C for 1 hr in a humidified atmosphere of 5% CO2/95% air, and then centrifuged to get rid of the DEPs. The MTS formazan product was measured by determining the absorbance of the supernatant (100 ìL) at 490 nm using a 96-well plate reader (FLUOstar, BMG Labtechnologies, Durham, NC, USA).
2.4. Intracellular ROS measurement
Intracellular ROS generation was measured using a well-characterized probe, 2’,7’-dichlorofluorescin diacetate (DCFH-DA) (Wang and Joseph, 1999). DCFH-DA was hydrolyzed by esterases to dichlorofluorescin (DCFH), which was trapped within the cell. This nonfluorescent molecule was then oxidized to fluorescent dichlorofluorescin (DCF) by the action of cellular oxidants. A DCFH-DA stock solution (in methanol) of 10 mM was diluted 500-fold in HBSS without serum or any other additive to yield a 20 µM working solution. Cells were washed twice with HBSS and then incubated with a DCFH-DA working solution for 1 h in a dark environment (37 °C incubator). The cells were washed twice with serum-free EBM-2 medium, and varying concentrations of DEPs (10, 25, 50 µg/ml) were added to cells for 3 h. After this the cells were washed twice with serum-free medium and 100µL of serum-free media was added to each well. Then, the fluorescence was determined at 485 nm excitation and 520 nm emission, using a microplate reader (FLUOstar, BMG Labtechnologies, Durham, NC, USA).
2.5. Determination of GSH
Intracellular endothelial cell GSH content was determined by reverse phase HPLC, according to the method developed in our laboratory (Ridnour et al., 1999). After treatment, HBMVEC cell samples were homogenized in SBB. Twenty microliters of this homogenate were added to 230 µl of HPLC grade water and 750 µl of NPM (1 mM in acetonitrile). The resulting solutions were incubated at room temperature for 5 min. The reaction was stopped by adding 5 µl of 2 N HCl. The samples were then filtered through a 0.45 µm filter (Advantec MFS, Inc. Dulin, CA, USA) and injected onto the HPLC system. An aliquot of 2.5 µl of the sample was injected for analysis using a Thermo Finnigan TM Spectra SYSTEM SCM1000 Vacuum Membrane Degasser, Finnigan TM SpectraSYSTEM P2000 Gradient Pump, Finnigan TM SpectraSYSTEM AS3000 Autosampler, and Finnigan™ SpectraSYSTEM FL3000 Fluorescence Detector (λex=330 nm and λem=376 nm). The HPLC column was a Reliasil ODS-1 C18 column (Column Engineering, Ontario, CA, USA). The mobile phase (70% acetonitrile and 30% water) was adjusted to a pH of 2.5 through the addition of 1 ml/L of both acetic and o-phosphoric acids. The NPM derivatives were eluted from the column isocratically at a flow rate of 1 ml/min.
2.6. Determination of malondialdehyde (MDA)
MDA content was determined as described by Draper et al. (1993). Briefly, the cell pellets were homogenized in SBB. To 0.350 ml of cell homogenate, 0.550 ml of 5% trichloroacetic acid (TCA) and 0.100 ml of 500 ppm butylated hydroxytoluene (BHT) in methanol were added. The samples were then heated in a boiling water bath for 30 min. After cooling on ice, the samples were centrifuged. The supernatant fractions were mixed 1:1 with saturated thiobarbituric acid (TBA). The samples were again heated in a boiling water bath for 30 min. After cooling on ice, 0.50 ml of each sample was extracted with 1 ml of n-butanol and centrifuged to facilitate the separation phases. The resulting organic layers were first filtered through a 0.45 µm filter and then analyzed using the Shimadzu HPLC system with a fluorescence detector. Excitation wavelength and emission wavelength were set at 515 nm and 550 nm, respectively. The column was 100×4.6 mm i.d. C18 column (3 µm packing material, Astec, Bellefonte, PA). Twenty microliter samples were injected for analysis. The mobile phase consisted of 69.4% 50 mM sodium phosphate buffer (pH 7.0), 30% acetonitrile, and 0.6% THF. The flow rate of the mobile phase was 1.0 ml/min. The concentrations of the TBA-MDA complex in the mixture were determined by using the calibration curve obtained from a malondialdehyde bis(dimethyl acetal) standard solution.
2.7. Determination of glutathione reductase activity
Glutathione reductase is the enzyme responsible for recycling GSSG into GSH via a reduction mechanism, utilizing both GSSG and NADPH as a substrate. The oxidation of NADPH to NADP+ was accompanied by a decrease in absorbance at 340 nm, providing a spectrophotometric means for monitoring the enzyme activity of GR. The activity of GR within the cells was determined by adding homogenate to a solution containing both GSSG and NADPH and then recording the absorbance as a function of time at 340 nm. The rate of decrease in the A340 was directly proportional to the GR activity in the sample.
2.8. Glutathione peroxidase activity assay
Glutathione peroxidase (GPx) protects mammals against oxidative damage by catalyzing the reduction of a variety of ROOH, or H2O2, using GSH as the reducing substance. The GPx 340™ assay (a test kit from OxisResearch) was used as an indirect measure of the activity of GPx. Oxidized glutathione (GSSG), produced upon reduction of an organic peroxide by GPx, was recycled to its reduced state by the enzyme glutathione reductase (GR): The oxidation of NADPH to NADP+ was accompanied by a decrease in absorbance at 340 nm (A340), providing a spectrophotometric means for monitoring GPx enzyme activity. The molar extinction coefficient for NADPH is 6220 M−1cm−1 at 340 nm. To measure the activity of GPx, cell homogenate was added to a solution containing glutathione, glutathione reductase, and NADPH. The enzyme reaction was initiated by adding the substrate, tert-butyl hydroperoxide, and the absorbance was recorded at A340. The rate of decrease in the A340 was directly proportional to the GPx activity in the sample.
2.9. Dextran permeability study
HBMVEC cells were seeded onto collagen-coated inserts with a pore size of 0.4 µm at densities of 3 × 104 cells/well, and allowed to culture until a monolayer formed. The cell monolayer was then treated with varying concentrations of DEPs (10 µg/ml, 25 µg/ml, and 50 µg/ml) for 24 h. After this, the medium was removed to ensure that there were no dead cells on the membrane. It was then replaced with 150 µl of FITC labeled dextran, and the insert was transferred to a fresh plate well, containing 500 µl of serum-free medium. The plates were incubated for 30 min at room temperature, and 100 µl of the plate well solution were removed and transferred to a 96-well plate. Fluorescence was read with a 485 nm excitation and 530 nm emission wavelengths using a microplate reader (FLUOstar, BMG Labtechnologies, Durham, NC, USA).
2.10. Trans-endothelial electric resistance (TEER) measurement
Trans-endothelial electric resistance (TEER) measurement by EVOM voltohmmeter (World Precision Instrument, Sarasota, FL, USA) assessed the tightness of the HBMVEC monolayer. HBMVEC cells were seeded onto collagen-coated inserts with a pore size of 0.4 µm at densities of 3 × 104 cells/well, and allowed to culture until a monolayer formed (4–7 days). The cell monolayer was then treated with 10, 25, or 50 µg/ml DEPs for 24 h. After this, the old medium was replaced with 150 µl of fresh serum-free medium to get rid of any dead cells. The insert containing the cell monolayer was then transferred to a fresh plate containing 500 µl of fresh serum-free medium. The TEER reading was recorded immediately and TEER values were calculated as: Resistance×0.32 cm2 (insert surface area). Thus, resistance is proportional to the effective membrane. The final TEER value was obtained by subtracting the resistance of collagen coated inserts from the resistance obtained in the presence of the endothelial cells.
2.11. Determination of protein
Protein levels of the cell samples were measured by the Bradford method (Bradford, 1976). Bovine serum albumin was used as the protein standard.
2.12. Statistical analysis
All reported values are represented as the mean ± S.D. of triplicates. Statistical analysis was performed using the GraphPad Prism software (GraphPad, San Diego, CA). Statistical significance was ascertained by one way analysis of variance, followed by Tukey’s multiple comparison tests. Values of p<0.05 were considered significant. In the figures and table, a represents a significant difference in comparison with the control group, b represents a significant difference in comparison with the 10 µg/ml [DEP] group, and c represents a significant difference in comparison with the 25 µg/ml [DEP] group.)
3. Results
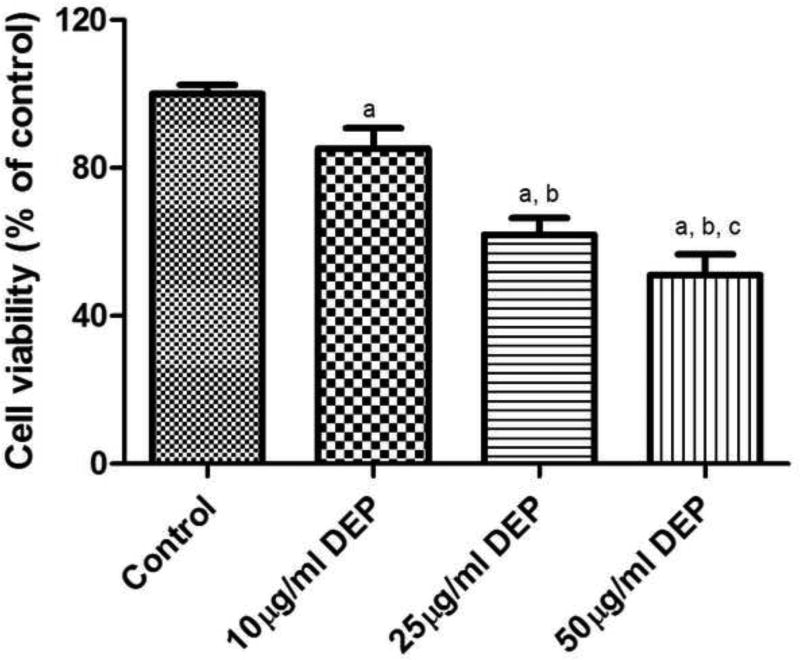
3.1. Effect of DEPs on cell viability
A dose-dependent decrease in cell viability was observed in HBMVEC cells upon exposure to DEPs for 24 h (Fig. 1) which was confirmed using a MTS assay. Cell viability decreased by about 14% in the presence of 10 µg/ml of DEPs which further decreased by 38% and 50% upon increasing the DEPs concentration to 25 µg/ml and 50 µg/ml, respectively.
Fig. 1.
Cytotoxicity of DEPs on HBMVEC cells. Cells were treated with various concentrations of DEPS (10 µg/ml, 25 µg/ml, and 50 µg/ml). After 24 h of treatment, the cell viability was assessed by MTS assay. Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
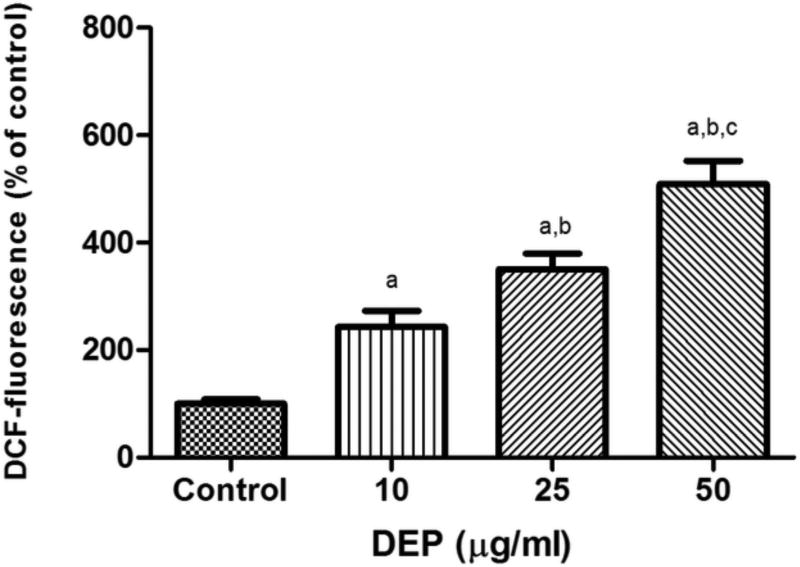
3.2. Effect of DEPs on intracellular ROS levels
To substantiate the hypothesis that DEPs were causing HBMVEC cell death through oxidative stress, ROS levels were measured after the exposure of cells to DEPs for 3 h. An increase in the production of ROS in HBMVEC cells, ranging from 140% to 400%, was seen with exposure to DEPs (Fig. 2). These data indicated that DEPs exposure to HBMVEC cells caused a dose-dependent increase in ROS, leading to severe oxidative stress and cell death.
Fig. 2.
Effect of DEPs on intracellular ROS levels. After treatment with various concentrations of DEPs (10 µg/ml, 25 µg/ml, and 50 µg/ml) for 3 h, the intracellular ROS level increased, as determined by the evaluation of the DCF fluorescence. Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
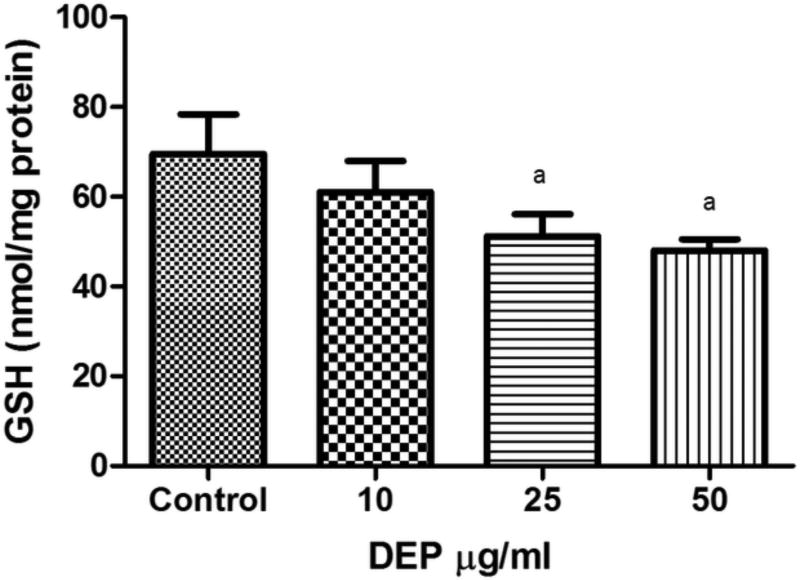
3.3. Effect of DEPs on intracellular GSH, GR, and GPx activity
To further elucidate the mechanism by which DEPs induce cell death and damage we investigated their effects on GSH and the critical antioxidant enzymes, glutathione peroxidase (GPx), and glutathione reductase (GR). GSH is one of the major intracellular thiol antioxidants in a cell. GSH levels were measured in HBMVEC cells exposed to DEPs. DEPs decreased the GSH levels in HBMVEC cells in a dose-dependent manner (Fig. 3). A lower dose of DEPs at 10 µg/ml did not decrease the GSH level significantly, but treatment with 25 µg/ml and 50 µg/ml of DEPs for 24 h showed marked decreases in the GSH level. This indicated that DEPs induced oxidative stress via depletion of GSH within the cells. Since GPx and GR activities are important in cell’s defense against oxidative stress, we further evaluated their role by measuring their activities in each of our treatment and control groups. The results demonstrated that exposure to DEPs resulted in a decrease in GPx and GR activities (Table 1).
Fig. 3.
Effect of DEPs on intracellular GSH levels in HBMVEC cells. GSH levels were measured after 24 hours of treatment with various concentrations of DEPs (10 µg/ml, 25 µg/ml, and 50 µg/ml). Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
Table 1.
Effect of DEPs on the activity of GPx, GR, and MDA level
| Groups | GPx (mU/mg protein) |
GR (mU/mg protein) |
MDA (nM/100 mg protein) |
|---|---|---|---|
| Control | 63.0 ± 1.93 | 49.5 ± 8.22 | 95.6 ± 5.05 |
| 10 µg/ml DEPs | 56.9 ± 2.52 | 28.6 ± 4.15a | 109 ± 6.87 |
| 25 µg/ml DEPs | 53.2 ± 2.79a | 23.9 ± 4.21a | 154± 10.0a,b |
| 50 µg/ml DEPs | 43.7 ± 4.55a,b,c | 19.6 ± 4.12a | 192 ± 4.23a,b,c |
Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
3.4. Effect of DEPs on lipid peroxidation byproduct MDA
MDA levels were determined in cells exposed to DEPs for 24 h. Cells treated with10 µg/ml, 25 µg/ml, and 50 µg/ml DEPs had nearly 14%, 62%, and 101% increases in MDA levels, respectively, when compared to that of the control (Table 1).
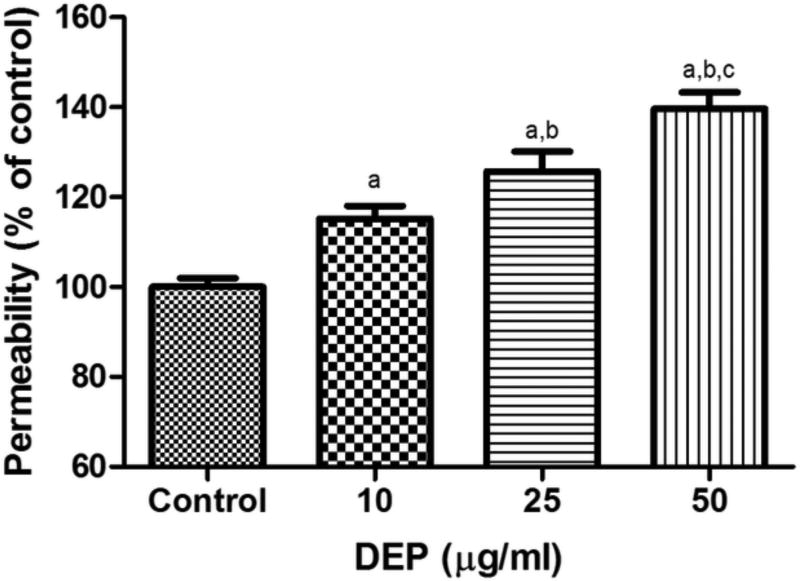
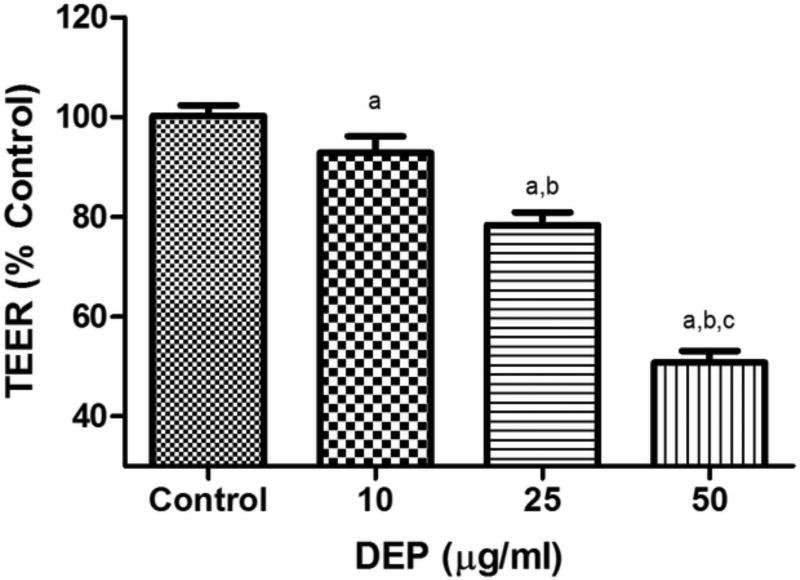
3.5. TEER and cell permeability assay
The cell permeability assay and TEER were done to determine DEPs potential to disrupt the integrity of the HBMVEC cells. Permeability studies showed that exposure to DEPs increased permeability by approximately 15–40% with an increase in the concentration of DEPs from 10 µg/ml to 50 µg/ml (Fig. 4). To further evaluate the cellular integrity of the HBMVEC cells, trans-epithelial electrical resistance (TEER) was measured. Measurement of TEER provided information on tight junction existence and stability. Reductions in TEER reflected early cell damage. We found that HBMVEC exposure to DEPs significantly decreased TEER, compared to controls (Fig. 5). As in the permeability study, TEER results also indicated a compromised HBMVEC monolayer. Exposure to DEPs resulted in a decrease in TEER in a concentration-dependent manner. A decrease of about 50% in the TEER value was observed in the case of exposure to 50 µg/ml of DEPs.
Fig. 4.
Effects of DEPs on FITC-Dextran permeability in HBMVEC cells. HBMVEC cells were seeded onto a collagen-coated insert with a pore size of 0.4 µm at a density of 15×103 cells/well and allowed to grow until a monolayer was formed. The cell monolayer was then treated with various concentrations of DEPs (10 µg/ml, 25 µg/ml, and 50 µg/ml) for 24 h. Fluorescence was read with a 485 nm and 530 nm filter set. Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
Fig. 5.
Effects of DEPs on TEER in HBMVEC cells. HBMVEC cells were seeded onto a collagen-coated insert with a pore size of 0.4 µm at a density of 15×103 cells/well, and allowed to culture until a monolayer formed. The cell monolayer was then treated with various concentrations of DEPs (10 µg/ml, 25 µg/ml, and 50 µg/ml) for 24 h. Cells treated with DEPs had decreased TEER values as compared to the control group. Values represent mean±SD. All experiments were performed in triplicates, and the values reported are mean ± SD. (a: different from control group, b: different from 10 µg/ml [DEP] group, and c: different from 25 µg/ml [DEP] group, p<0.05).
4. Discussion
The brain microvascular endothelial cells, situated at the interface of the blood and the brain, perform the essential functions of shielding the brain from toxic substances in the blood stream, transporting micro and macro nutrients, leukocyte trafficking, and osmoregulation (Banks et al., 2006; Persidsky et al., 1997). Due to the unique regulatory function of the BBB, these endothelial cells possess several modifications (tight junctions), which are important for maintaining the integrity of these membranes. Loss of BBB integrity has been reported to be critical in the development and progression of neurological diseases like Alzheimer's (Fiala et al., 2002), human immunodeficiency virus-1 (HIV-1) encephalitis (Dallasta et al., 1999), multiple sclerosis (Bar-Or et al., 2003), stroke (Ilzecka, 1996), and traumatic brain injury (Morganti-Kossmann et al., 2002).
DEPs have been reported to alter BBB function through oxidative stress at the tissue, cellular, and molecular levels (Hartz et al., 2008). DEPs potential to induce oxidative stress in conjunction with reports that they can pass through the BBB and accumulate in the brain, indicate that they may play a key role in neurotoxicities.
Although the role of oxidative stress in DEPs-induced toxicity is well-known, little is known about how DEPs-induced oxidative stress affects the BBB. In this study, we determined the oxidative stress parameters in the HBMVEC cells exposed to DEPs, and measured levels of GSH, lipid peroxidation byproduct (MDA), and ROS formation, and the activity of the antioxidant enzymes GPx and GR. We also investigated the role of DEPs in inducing oxidative stress and disrupting the permeability of the HBMVECs in vitro.
Results from our study showed that HBMVEC cells treated with DEPs experienced a significant decrease in cell viability and GSH levels, indicating oxidative stress. Glutathione (GSH, ã-glutamyl-cysteinyl-glycine), an intracellular thiol, is one of the important factors that is critical for maintaining the integrity of the BBB (Agarwal and Shukla, 1999). Even though the mechanism by which GSH depletion leads to the dysfunction of the BBB is not known, GSH has been reported to be a direct scavenger of ROS, and its depletion may lead to oxidative stress (Yamamoto and Zhu, 1998). GSH functions as a direct scavenger of ROS and as a cofactor in its metabolic detoxification; therefore, a decrease in GSH is suggestive of oxidative stress (Foga et al., 1997).
Results from our study showed that HBMVEC cells treated with DEPs experienced significant decrease in cell viability and GSH levels, indicating that the increase in oxidative stress due to the decrease in GSH levels was responsible for reduced cell viability. A possible explanation for the decrease in GSH levels under oxidative stress is the reduced activity of the enzymes involved in GSH synthesis and/or GR activity. Some studies have indicated that loss of GSH will directly affect the activity of the GSH-dependent enzyme GR. This enzyme plays an important role in GSH homeostasis: it regenerates GSH from GSSG (Barker et al., 1996). It has been reported that under oxidative stress, protein sulfhydryl (protein–SH) groups are lost (Wu et al., 2004) which are believed to be essential for enzyme activity (Agarwal and Shukla, 1999). Under such circumstances, GSH is not regenerated; thus, depletion of cellular GSH indicates that the cells are undergoing oxidative stress (DeLeve and Kaplowitz, 1991). Decreased activity of GR seen in our experiments upon DEP treatment, supports our hypothesis of GSH depletion as a mechanism for cell death in DEP-treated HBMVECs. Decreased GSH levels in normal human bronchial epithelial cells and in the GSH/GSSG ratio in the macrophage cell line upon exposure to DEPs have been previously reported (Li et al., 2002; Xiao et al., 2003). This indicates that low levels of GSH may render individuals susceptible to the deleterious effects of exposure to inhaled toxicants and may also perpetuate inflammatory responses.
Further, depletion of intracellular GSH has been reported to increase production of ROS in cells (Penugonda et al., 2005). To investigate this, ROS levels were measured using a peroxide-sensitive dye, DCF. DEPs-treated cells were found to have significant increases in ROS accumulation, as compared to that of the controls. Increases in ROS levels, upon DEPs exposure, have been observed in previous studies (Hartz et al., 2008; Block et al., 2004; Li et al., 2002). Increases in ROS and nitric oxide have been reported in human umbilical vein endothelial cells (HUVEC) cells upon exposure to particulate matter (Montiel-Davalos et al., 2010, Sumanasekera et al., 2007).
An important target of oxidative damage is brain microvessel endothelial cells because they are rich in polyunsaturated fatty acids (Tayarani et al., 1987). The double bonds in these fatty acids undergo lipid peroxidation in the presence of free radicals and form stable by-products, such as malondialdehyde (MDA), which are used as markers of lipid peroxidation (Belghmi et al., 1988; Janero, 1990). HBMVEC cells that were exposed to DEPs had increased levels of MDA, compared to those of the controls, indicating increased lipid peroxidation in the BBB cells. Lipid peroxidation is one of the key mechanisms by which ROS induce cell death. It has been postulated that radicals attack membrane lipids and initiate a chain of events leading to lipid peroxidation (Thornalley et al., 1983; Comporti 1987; Masaki et al., 1989). Concomitant reduction of GSH levels (a substrate for glutathione peroxidase) might have hampered the decomposition of lipid peroxides in DEPs-treated cells, thus increasing the MDA levels. Lipid peroxidation is deleterious as it impacts the cellular functions negatively, resulting in cell death, thereby lowering cell viability. ROS damage the cell membranes through lipid peroxidation and the production of lipid aldehydes such as MDA and 4-hydroxynonenal. An increased level of MDA is not only a marker of oxidative stress but also an indicator of elevated toxicity.
Antioxidant enzymes are involved in the detoxification of lethal peroxides inside the cells. A significant reduction in the activity of GPx, observed after DEPs exposure, may have been partially due to diminished GSH levels that GPx needs as a substrate. We previously reported decreased GPx activity, due to METH, in human brain microvascular endothelial cell culture (Zhang et al., 2009). Decreased activity of GPx in DEPs-treated cells, which was observed in our study, indicates that the cells were overwhelmed by ROS and that GPx levels were inadequate to combat ROS-mediated damage. A significant increase in MDA levels also supports this hypothesis. If an increase in antioxidant enzyme activities was observed, MDA levels would not increase. In other words, enzymes would scavenge ROS before they could attack macromolecules, including DNA, proteins, and lipids.
Under physiological conditions, the integrity of the BBB is protected from oxidative stress because the BBB has high levels of antioxidant enzymes (Plateel et al., 1995). Oxidative stress is one of the important mechanisms responsible for the disruption of the BBB. This disruption allows the passage of toxic substances into the brain, leading to development and progression of various neurological diseases (Dallasta et al., 1999; Fiala et al., 2002; Bar-Or et al., 2003). Some studies have indicated disruption of endothelial tight junctions in the brain by ROS (Fischer et al., 2005, Lee et al., 2004, Yamagata et al., 2004). It was, therefore, crucial to determine DEP’s potential for altering the HBMVECs permeability, which is an integral part of the BBB. DEPs induced decrease in TEER, indicating their potential for disrupting cellular homeostasis and BBB integrity under severe oxidative stress conditions. Increased permeability of HBMVEC cells in our study is also supported by similar increase in human aortic endothelial cells (HAEC) upon exposure to a similar concentrations of DEPs (Li et al., 2010). Our results with decreased TEER values are also in accordance with those reported by Lehmann et al. (2009). However, an increase in TEER and a decrease in permeability were observed in HUVEC upon DEP exposure for 15 min by Sumanasekera et al., 2007. This difference could be due to the short term DEP exposure in this study. All of these results collectively indicate that DEPs induced oxidative stress in HBMVEC cells and altered the permeability of BBB.
In conclusion, data from the present study indicate that DEPs cause oxidative stress to BBB cells, as demonstrated by decreased intracellular GSH, increased MDA levels and intracellular ROS production, and decreased GPx and GR activities. In addition, DEPs treatment also increased the permeability of the cells. Although brain endothelial cells possess high intracellular levels of antioxidant defense mechanisms, such as GSH, exposure to DEPs may render the BBB susceptible to toxic damage and change its specific functions. We believe that the damaging effect of DEPs would be more than predicted by our data as the volatile and semivolatile fractions were absent from the resuspended DEPs. Considering the potential of DEPs to disrupt the BBB, further studies should be conducted to determine the role of DEPs in inducing neurotoxicities and also to investigate and establish their role in the onset of neurodegenerative diseases like Parkinson's and Alzheimer's, which have been linked to air pollution.
Highlights.
Exposure to DEPs induced higher oxidative stress in HBMVEC cells.
DEPs induce cell death and disrupt the function and integrity of HBMVEC cells
Data indicate a potential role of DEPs in neurotoxicities.
Acknowledgments
Dr. Ercal was supported by 1 R15DA023409-01A2 from the NIDA, NIH and the contents of this paper are solely the responsibility of the authors and do not necessarily represent official views of the NIDA or NIH. The authors appreciate the editorial efforts of Barbara Harris.
Abbreviations
- CNS
central nervous system
- DEE
Diesel engine exhaust
- DEPs
Diesel exhaust particles
- GSH
glutathione
- GPx
glutathione peroxidase
- H2DCFDA
2’ 7’ –dichlorofluorescein diacetate
- MDA
malondialdehyde
- NPM
N-(1-pyrenyl)-maleimide
- PBS
phosphate buffered saline
- ROS
reactive oxygen species
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors declare that there were no conflicts of interests.
References
- Agarwal R, Shukla GS. Potential role of cerebral glutathione in the maintenance of blood-brain barrier integrity in rat. Neurochem. Res. 1999;24:1507–1514. doi: 10.1023/a:1021191729865. [DOI] [PubMed] [Google Scholar]
- Bai Y, Suzuki AK, Sagai M. The cytotoxic effects of diesel exhaust particles on human pulmonary artery endothelial cells in vitro: role of active oxygen species. Free Radic. Biol. Med. 2001;30:555–562. doi: 10.1016/s0891-5849(00)00499-8. [DOI] [PubMed] [Google Scholar]
- Banks WA, Ercal N, Price TO. The blood-brain barrier in neuroAIDS. Curr. HIV Res. 2006;4:259–266. doi: 10.2174/157016206777709447. [DOI] [PubMed] [Google Scholar]
- Barker JE, Heales SJ, Cassidy A, Bolaños JP, Land JM, Clark JB. Depletion of brain glutathione results in a decrease of glutathione reductase activity: an enzyme susceptible to oxidative damage. Brain Res. 1996;716:118–122. doi: 10.1016/0006-8993(96)00003-0. [DOI] [PubMed] [Google Scholar]
- Bar-Or A, Nuttall RK, Duddy M, Alter A, Kim HJ, Ifergan I, Pennington CJ, Bourgoin P, Edwards DR, Yong VW. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain. 2003;126:2738–2749. doi: 10.1093/brain/awg285. [DOI] [PubMed] [Google Scholar]
- Belghmi K, Nicolas JC, Crastes de Paulet A. Chemiluminescent assay of lipid hydroperoxides. J. Biolumin. Chemilumin. 1988;2:113–119. doi: 10.1002/bio.1170020302. [DOI] [PubMed] [Google Scholar]
- Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506–516. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block ML, Wu X, Pei Z, Li G, Wang T, Qin L, Wilson B, Yang J, Hong JS, Veronesi B. Nanometer size diesel exhaust particles are selectively toxic to dopaminergic neurons: the role of microglia, phagocytosis, and NADPH oxidase. FASEB J. 2004;18:1618–1620. doi: 10.1096/fj.04-1945fje. [DOI] [PubMed] [Google Scholar]
- Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- Campbell A, Oldham M, Becaria A, Bondy SC, Meacher D, Sioutas C, Misra C, Mendez LB, Kleinman M. Particulate matter in polluted air may increase biomarkers of inflammation in mouse brain. Neurotoxicology. 2005;26:133–140. doi: 10.1016/j.neuro.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Carero DP, Hoet PHM, Verschaeve L, Schoeters G, Nemery B. Genotoxic Effects of Carbon Black Particles, Diesel Exhaust Particles, and Urban Air Particulates and Their Extracts on a Human Alveolar Epithelial Cell Line (A549) and a Human Monocytic Cell Line (THP-1) Environ. Mol. Mutagen. 2001;37:155–163. doi: 10.1002/em.1023. [DOI] [PubMed] [Google Scholar]
- Comporti M. Glutathione depleting agents and lipid peroxidation. Chem. Phys. Lipids. 1987;45:143–169. doi: 10.1016/0009-3084(87)90064-8. [DOI] [PubMed] [Google Scholar]
- Dallasta LM, Pisarov LA, Esplen JE, Werley JV, Moses AV, Nelson JA, Achim CL. Blood-brain barrier tight junction disruption in human immunodeficiency virus-1 encephalitis. Am. J. Pathol. 1999;155:1915–1927. doi: 10.1016/S0002-9440(10)65511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeve LD, Kaplowitz N. Glutathione metabolism and its role in hepatotoxicity. Pharmacol. Ther. 1991;52:287–305. doi: 10.1016/0163-7258(91)90029-l. [DOI] [PubMed] [Google Scholar]
- Diaz-Sanchez D, Tsien A, Fleming J, Saxon A. Combined diesel exhaust particulate and ragweed allergen challenge markedly enhances human in vivo nasal ragweed-specific IgE and skews cytokine production to a T helper cell 2-type pattern. J. Immunol. 1997;158:2406–2413. [PubMed] [Google Scholar]
- Dockery DW, Pope CA3, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BGJ, Speizer FE. An association between air pollution and mortality in six U.S. cities. N. Engl. J. Med. 1993;329:1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- Draper HH, Squires EJ, Mahmoodi H, Wu J, Agarwal S, Hadley M. A comparative evaluation of thiobarbituric acid methods for the determination of malondialdehyde in biological materials. Free Radic. Biol. Med. 1993;15:353–363. doi: 10.1016/0891-5849(93)90035-s. [DOI] [PubMed] [Google Scholar]
- Elder A, Gelein R, Silva V, Feikert T, Opanashuk L, Carter J, Potter R, Maynard A, Ito Y, Finkelstein J, Oberdörster G. Translocation of inhaled ultrafine manganese oxide particles to the central nervous system. Environ. Health Perspect. 2006;114:1172–1178. doi: 10.1289/ehp.9030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiala M, Liu QN, Sayre J, Pop V, Brahmandam V, Graves MC, Vinters HV. Cyclooxygenase-2-positive macrophages infiltrate the Alzheimer's disease brain and damage the blood-brain barrier. Eur. J. Clin. Invest. 2002;32:360–371. doi: 10.1046/j.1365-2362.2002.00994.x. [DOI] [PubMed] [Google Scholar]
- Fischer S, Wiesnet M, Renz D, Schaper W. H2O2 induces paracellular permeability of porcine brain-derived microvascular endothelial cells by activation of the p44/42 MAP kinase pathway. Eur. J. of Cell Biol. 2005;84:687–697. doi: 10.1016/j.ejcb.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Foga IO, Nath A, Hasinoff BB, Geiger JD. Antioxidants and dipyridamole inhibit HIV-1 gp120-induced free radical-based oxidative damage to human monocytoid cells. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 1997;16:223–229. doi: 10.1097/00042560-199712010-00001. [DOI] [PubMed] [Google Scholar]
- Hartz AMS, Bauer B, Block ML, Hong J, Miller DS. Diesel exhaust particles induce oxidative stress, proinflammatory signaling, and P-glycoprotein up-regulation at the blood-brain barrier. FASEB J. 2008;22:2723–2733. doi: 10.1096/fj.08-106997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the "common" neurologic disorders? Neurology. 2007;68:326–337. doi: 10.1212/01.wnl.0000252807.38124.a3. [DOI] [PubMed] [Google Scholar]
- Iłzecka J. The structure and function of blood-brain barrier in ischaemic brain stroke process. Ann. Univ. Mariae Curie Sklodowska Med. 1996;51:123–127. [PubMed] [Google Scholar]
- Janero DR. Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic. Biol. Med. 1990;9:515–540. doi: 10.1016/0891-5849(90)90131-2. [DOI] [PubMed] [Google Scholar]
- Kleinman MT, Araujo JA, Nel A, Sioutas C, Campbell A, Cong PQ, Li H, Bondy SC. Inhaled ultrafine particulate matter affects CNS inflammatory processes and may act via MAP kinase signaling pathways. Toxicol. Lett. 2008;178:127–130. doi: 10.1016/j.toxlet.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann AD, Blank F, Baum O, Gehr P, Rothen-Rutishauser BM. Diesel exhaust particles modulate the tight junction protein occludin in lung cells in vitro. Part. Fibre Toxicol. 2009;6:26. doi: 10.1186/1743-8977-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HS, Namkoong K, Kim DH, Kim KJ, Cheong YH, Kim SS, Lee WB, Kim KY. Hydrogen peroxide-induced alterations of tight junction proteins in bovine brain microvascular endothelial cells. Microvas. Res. 2004;68:231–238. doi: 10.1016/j.mvr.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Li N, Wang M, Oberley TD, Sempf JM, Nel AE. Comparison of the pro-oxidative and proinflammatory effects of organic diesel exhaust particle chemicals in bronchial epithelial cells and macrophages. J. Immunol. 2002;169:4531–4541. doi: 10.4049/jimmunol.169.8.4531. [DOI] [PubMed] [Google Scholar]
- Li N, Hao M, Phalen RF, Hinds WC, Nel AE. Particulate air pollutants and asthma. A paradigm for the role of oxidative stress in PM-induced adverse health effects. Clin. Immunol. 2003;109:250–265. doi: 10.1016/j.clim.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Li R, Ning Z, Cui J, Yu F, Sioutas C, Hsiai T. Diesel exhaust particles modulate vascular endothelial cell permeability: implication of ZO-1 expression. Toxicol. Lett. 2010;197:163–168. doi: 10.1016/j.toxlet.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li XY, Gilmour PS, Donaldson K, MacNee W. Free radical activity and pro-inflammatory effects of particulate air pollution (PM10) in vivo and in vitro. Thorax. 1996;51:1216–1222. doi: 10.1136/thx.51.12.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long TC, Tajuba J, Sama P, Saleh N, Swartz C, Parker J, Hester S, Lowry GV, Veronesi B. Nanosize titanium dioxide stimulates reactive oxygen species in brain microglia and damages neurons in vitro. Environ. Health Perspect. 2007;115:1631–1637. doi: 10.1289/ehp.10216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montiel-Davalos A, Ibarra-Sanchez Mde J, Ventura-Gallegos JL, Alfaro-Moreno E, Lopez-Marure R. Oxidative stress and apoptosis are induced in human endothelial cells exposed to urban particulate matter. Toxicol. in vitro. 2010;24:135–141. doi: 10.1016/j.tiv.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Masaki N, Kyle ME, Farber JL. tert-butyl hydroperoxide kills cultured hepatocytes by peroxidizing membrane lipids. Arch. Biochem. Biophys. 1989;269:390–399. doi: 10.1016/0003-9861(89)90122-7. [DOI] [PubMed] [Google Scholar]
- Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T. Immune and Inflammatory Responses in the Nervous System. Oxford,. UK: University Press, UK: University Press Oxford; 2002. Inflammatory responses to traumatic brain injury: an overview for the new millennium; pp. 106–126. [Google Scholar]
- Nel AE, Diaz-Sanchez D, Ng D, Hiura T, Saxon A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J. Allergy Clin. Immunol. 1998;102:539–554. doi: 10.1016/s0091-6749(98)70269-6. [DOI] [PubMed] [Google Scholar]
- Oberdörster G, Oberdörster E, Oberdörster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ. Health Perspect. 2005;113:823–839. doi: 10.1289/ehp.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberdörster G, Sharp Z, Atudorei V, Elder A, Gelein R, Kreyling W, Cox C. Translocation of inhaled ultrafine particles to the brain. Inhal. Toxicol. 2004;16:437–445. doi: 10.1080/08958370490439597. [DOI] [PubMed] [Google Scholar]
- Oberdörster G, Sharp Z, Atudorei V, Elder A, Gelein R, Lunts A, Kreyling W, Cox C. Extrapulmonary translocation of ultrafine carbon particles following whole-body inhalation exposure of rats. J. Toxicol. Environ. Health A. 2002;65:1531–1543. doi: 10.1080/00984100290071658. [DOI] [PubMed] [Google Scholar]
- Penugonda S, Mare S, Goldstein G, Banks WA, Ercal N. Effects of N-acetylcysteine amide (NACA), a novel thiol antioxidant against glutamate-induced cytotoxicity in neuronal cell line PC12. Brain Res. 2005;1056:132–138. doi: 10.1016/j.brainres.2005.07.032. [DOI] [PubMed] [Google Scholar]
- Persidsky Y, Stins M, Way D, Witte MH, Weinand M, Kim KS, Bock P, Gendelman HE, Fiala M. A model for monocyte migration through the blood-brain barrier during HIV-1 encephalitis. J. Immunol. 1997;158:3499–3510. [PubMed] [Google Scholar]
- Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, Reed W, Rothen-Rutishauser B, Schürch S, Schulz H. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part. Fibre Toxicol. 2006;3:13. doi: 10.1186/1743-8977-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plateel M, Dehouck MP, Torpier G, Cecchelli R, Teissier E. Hypoxia increases the susceptibility to oxidant stress and the permeability of the blood-brain barrier endothelial cell monolayer. J. Neurochem. 1995;65:2138–2145. doi: 10.1046/j.1471-4159.1995.65052138.x. [DOI] [PubMed] [Google Scholar]
- Pope CA3, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE, Heath CWJ. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am. J. Respir. Crit. Care Med. 1995;151:669–674. doi: 10.1164/ajrccm/151.3_Pt_1.669. [DOI] [PubMed] [Google Scholar]
- Ridnour LA, Winters RA, Ercal N, Spitz DR. Measurement of glutathione, glutathione disulfide, and other thiols in mammalian cell and tissue homogenates using high-performance liquid chromatography separation of N-(1-pyrenyl)maleimide derivatives. Methods Enzymol. 1999;299:258–267. doi: 10.1016/s0076-6879(99)99025-0. [DOI] [PubMed] [Google Scholar]
- Sarnat JA, Schwartz J, Suh HH. Fine particulate air pollution and mortality in 20 U.S. cities. N. Engl. J. Med. 2001;344:1253–1254. doi: 10.1056/NEJM200104193441614. [DOI] [PubMed] [Google Scholar]
- Schrade A, Sade H, Couraud PO, Romero IA, Weksler BB, Niewoehner J. Expression and localization of claudins-3 and-12 in transformed human brain endothelium. Fluids and barriers of the CNS. 2012;9:6. doi: 10.1186/2045-8118-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugamata M, Ihara T, Takano H, Oshio S, Takeda K. Maternal Diesel Exhaust Exposure Damages Newborn Murine Brains. J. Health Sci. 2006;52:82–84. [Google Scholar]
- Sumanasekera WK, Ivanova MM, Johnston BJ, Dougherty SM, Sumanasekera GU, Myers SR, Ali Y, Kizu R, Klinge CM. Rapid effects of diesel exhaust particulate extracts on intracellular signaling in human endothelial cells. Toxicology letters. 2007;174:61–73. doi: 10.1016/j.toxlet.2007.08.014. [DOI] [PubMed] [Google Scholar]
- Tayarani I, Chaudiere J, Lefauconnier JM, Bourre JM. Enzymatic protection against peroxidative damage in isolated brain capillaries. J. Neurochem. 1987;48:1399–1402. doi: 10.1111/j.1471-4159.1987.tb05677.x. [DOI] [PubMed] [Google Scholar]
- Thornalley PJ, Trotta RJ, Stern A. Free radical involvement in the oxidative phenomena induced by tert-butyl hydroperoxide in erythrocytes. Biochim. Biophys. Acta. 1983;759:16–22. doi: 10.1016/0304-4165(83)90183-6. [DOI] [PubMed] [Google Scholar]
- Veronesi B, Makwana O, Pooler M, Chen LC. Effects of subchronic exposures to concentrated ambient particles. VII. Degeneration of dopaminergic neurons in Apo E−/ − mice. Inhal. Toxicol. 2005;17:235–241. doi: 10.1080/08958370590912888. [DOI] [PubMed] [Google Scholar]
- Vouk VB, Piver WT. Metallic elements in fossil fuel combustion products: amounts and form of emissions and evaluation of carcinogenicity and mutagenicity. Environ. Health Perspect. 1983;47:201–225. doi: 10.1289/ehp.8347201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Joseph JA. Quantifying cellular oxidative stress by dichlorofluorescein assay using microplate reader. Free Radic. Biol. Med. 1999;27:612–616. doi: 10.1016/s0891-5849(99)00107-0. [DOI] [PubMed] [Google Scholar]
- Weksler BB, Subileau EA, Perriere N, Charneau P, Holloway K, Leveque M, Tricoire-Leignel H, Nicotra A, Bourdoulous S, Turowski P, Male DK, Roux F, Greenwood J, Romero IA, Couraud PO. Blood-brain barrier-specific properties of a human adult brain endothelial cell line. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2005;19:1872–1874. doi: 10.1096/fj.04-3458fje. [DOI] [PubMed] [Google Scholar]
- Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J. Nutr. 2004;134:489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- Xiao GG, Wang M, Li N, Loo JA, Nel AE. Use of proteomics to demonstrate a hierarchical oxidative stress response to diesel exhaust particle chemicals in a macrophage cell line. J. Biol. Chem. 2003;278:50781–50790. doi: 10.1074/jbc.M306423200. [DOI] [PubMed] [Google Scholar]
- Yamagata K, Tagami M, Takenaga F, Yamori Y, Itoh S. Hypoxia-induced changes in tight junction permeability of brain capillary endothelial cells are associated with IL-1beta and nitric oxide. Neurobiology of disease. 2004;17:491–499. doi: 10.1016/j.nbd.2004.08.001. [DOI] [PubMed] [Google Scholar]
- Yamamoto BK, Zhu W. The effects of methamphetamine on the production of free radicals and oxidative stress. J. Pharmacol. Exp. Ther. 1998;287:107–114. [PubMed] [Google Scholar]
- Zhang X, Banerjee A, Banks WA, Ercal N. N-Acetylcysteine amide protects against methamphetamine-induced oxidative stress and neurotoxicity in immortalized human brain endothelial cells. Brain Res. 2009;1275:87–95. doi: 10.1016/j.brainres.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]