Abstract
Chikungunya virus is a vector-borne alphavirus transmitted by the bites of infected female Ae. aegypti and Ae. albopictus. In Brazil between 2014 and 2016 almost 320 thousand autochthonous human cases were reported and in Florida numerous imported CHIKV viremic cases (> 3,800) demonstrate the potential high risk to establishment of local transmission. In the present study, we carried out a series of experiments to determine the viral dissemination and transmission rates of different Brazilian and Florida populations of Ae. aegypti and Ae. albopictus at 2, 5, and 13 days post-infection for the emergent Asian genotype of CHIKV. Our results show that all tested populations of Ae. aegypti and Ae. albopictus have a high proportion (> 0.80) of individuals with disseminated infection as early as 2 days-post exposure. We found no significant treatment effects of mosquito population origin effects on viral dissemination rates. Transmission rates had a heterogeneous pattern, with US Ae. aegypti and Brazilian Ae. albopictus having the highest proportion of individuals with successful infection (respectively 0.50 and 0.82 as early as 2 days-post infection). Model results found significant effects of population origin, population origin x species, population origin x days post-infection and population origin x species x days post infection.
Author summary
Chikungunya is considered a serious mosquito-borne disease in many tropical and subtropical countries throughout the world. It is already an epidemic disease in Brazil and poses as a potential risk in Florida. It is mainly transmitted by mosquitoes Aedes aegypti and Aedes albopictus. These mosquito species are common and abundant throughout much of the year in Brazil and Florida. In this study, we determined two components of vector competence from Brazilian and Florida populations of both mosquitoes to the emergent Asian genotype of chikungunya virus: viral dissemination and transmission rates. Both Aedes populations exhibited a high proportion of disseminated infection as early as two days after ingestion of chikungunya virus infected blood. Transmission efficiency was higher in Ae. aegypti from Florida and Ae. albopictus from Brazil. Our findings suggest that mosquito-virus interactions of both Ae. aegypti and Ae. albopictus may vary by geographic population, which may impact public health measures and should be considered during outbreaks of this arboviral disease.
Introduction
Chikungunya fever is a vector-borne viral disease that originated in Africa and is caused by a virus (CHIKV; family Togaviridae, genus Alphavirus) transmitted by the bites of infected female Aedes mosquitoes, mainly Ae. aegypti and Ae. albopictus [1]. There are three genotypes of CHIKV, which apparently evolved independently in distinct geographic regions: Asian, West African, and East/Central/South African (ECSA) [2]. CHIKV is widespread worldwide and poses as a major public health problem in tropical and subtropical regions [3–6]. In the Americas, autochthonous transmission of CHIKV was first detected in St. Martin Island in October 2013 and quickly spread throughout the Americas in the following months [7–9]. The initial spread of autochthonous cases in the Americas was due to the Asian genotype, but the ECSA genotype was also detected circulating in Brazil in 2014 [10]. To date, local transmission of CHIKV has been documented in over 43 countries with more than 1,000,000 confirmed cases, where Brazil reported 314,834 until the 15th epidemiological week of 2017 [11–12].
Aedes aegypti and Ae. albopictus are the main vectors of CHIKV, and both are highly invasive species and closely associated with the human peridomestic environment [13, 14, 6]. Aedes aegypti is highly anthropophilic and exhibits endophilic behavior and is mostly associated with high human density. In contrast, Ae. albopictus shows an eclectic feeding behavior, preferentially feeding and resting in the peridomicile and is more common in vegetated and urban/urban forest transition habitats, especially where it is sympatric with Ae. aegypti [15–19]. In Africa, CHIKV is maintained via an enzootic cycle involving several species of arboreal mosquitoes, including Ae. africanus and Ae. furcifer, and non-human primates [20]. Epidemic transmission is maintained mainly by Ae. aegypti in urban environments, but a single-base mutation in a strain of the ECSA genotype during the outbreak in La Réunion Island enhanced vector competence of Ae. albopictus [21, 22]. A second mutation is associated with enhanced vector competence of Ae. albopictus during an outbreak in Kerala, India [23]. In fact, the acquisition of second-step Ae. albopictus-adaptive mutations by CHIKV strains might indicate even more efficient transmission by this invasive vector [24].
Vector competence studies are important to determine the potential of resident mosquito populations to transmit CHIKV. Vector competence is a phenotypic parameter that describes the ability of the vector to become infected, replicate and transmit a pathogen [25, 26]. Moreover, vector competence depends on vector and viral genetic characteristics [27] and environmental factors such as ambient temperature and diurnal temperature range [28–32]. It has been shown that vector competence of Ae. aegypti and Ae. albopictus for CHIKV is a complex interaction dependent on vector population, virus strain and temperature [33, 34]. The vector competence of Ae. aegypti for dengue virus (DENV) has been shown to have high variability and heterogeneity whether it is analyzed at city [35], country [36] or continental level [37].
Previous studies of CHIKV have characterized variation in vector competence among CHIKV genotypes, extrinsic incubation temperature, and geographic populations of Ae. aegypti and Ae. albopictus, and species-specific differences. In Florida, Ae. aegypti and Ae. albopictus were highly susceptible to infection and viral dissemination to ECSA and Asian genotypes of CHIKV, with some variation between strains [38, 39]. Pesko et al. (2009) [40] evaluated vector competence of Ae. aegypti and Ae. albopictus from Florida for infection with a La Réunion island ECSA isolate of CHIKV. Although both species were susceptible to high CHIKV doses, Ae albopictus was more susceptible to infection than Ae. aegypti. Richards et al. (2010) [33] assessed the effect of extrinsic incubation temperature on vector competence of Florida mosquitoes for CHIKV isolates from La Réunion and found highest infection, dissemination, and transmission rates in Ae. albopictus than in Ae. aegypti and Culex quinquefasciatus, but no effect on the extrinsic incubation period. Vega-Rúa et al. (2014) [31] working with three CHIKV genotypes and 35 populations of Ae. aegypti and Ae. albopictus mosquitoes from 10 American countries showed that all Aedes populations tested were susceptible to CHIKV infection by all three genotypes. However, CHIKV transmission was heterogeneous in American Ae. aegypti and Ae. albopictus populations, ranging from 11.1% to 96.7%. In this study, the Aedes populations from Rio de Janeiro showed high transmission rates, and Ae. albopictus from Florida were more competent vectors than Ae. aegypti.
Although Ae. aegypti is considered the primary epidemic vector of CHIKV and Ae. albopictus a potential vector in some areas [2, 21, 31], heterogeneous vector competence of both species may alter risk of disease transmission, as evidenced by the participation of Ae. albopictus in the outbreak in La Réunion Island [21]. Studies comparing vector competence in American populations of both species are necessary in a scenario where travel and global trade in endemic regions have increased the risk for spread of CHIKV, as evidenced by its introduction in the Americas [41]. Also, there is a real risk for the introduction of CHIKV strains with adaptive mutations to enhance vector competence of Ae. albopictus, an invasive species which is widespread in the Americas [24. With the aim to shed light on the causes and consequences of geographical variations in the transmission of arboviruses of public health concern, we carried out an experiment to determine the dissemination and transmission rates of Brazilian and Florida populations of Ae. aegypti and Ae. albopictus for the emergent Asian genotype of CHIKV.
Materials and methods
Ethics statement
Chikungunya virus (Asian lineage, GenBank accession: KJ451624) used was isolated from the serum of an infected human in the British Virgin Islands in 2013 by other investigators. Subsequently, this isolate was archived with the Centers for Disease Control and Prevention. We requested an isolate of this virus for use in this study and so the sample was already present in an already-existing collection (Centers for Disease Control and Prevention, Arboviral Diseases Branch). The virus sample was anonymized and Institutional Review Board approval was not needed for receipt and use of the sample in this study. No entomological gathering was done on private land or in private residence for this study.
Mosquito collections and rearing
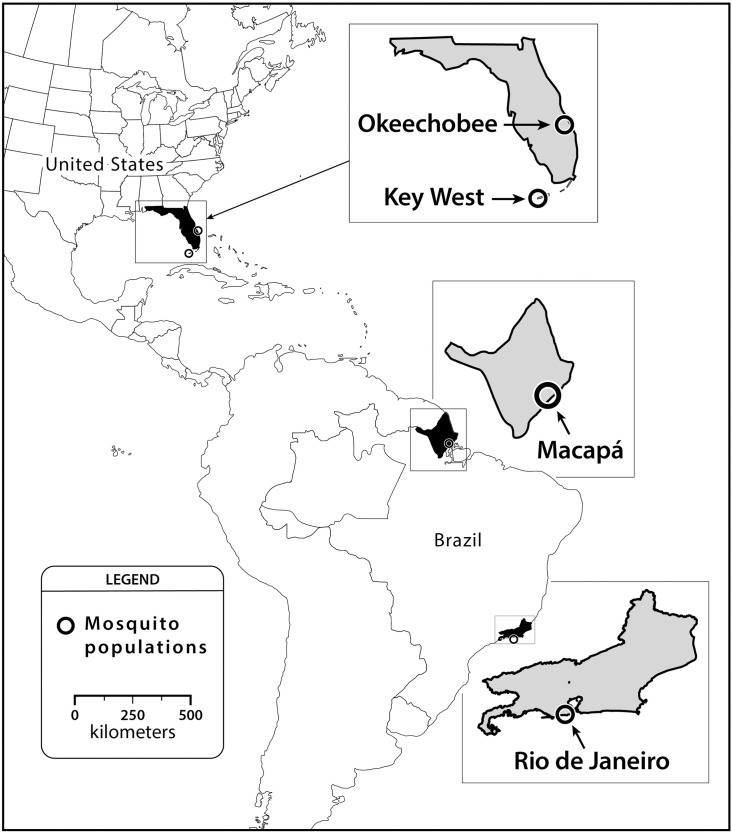
The Ae. aegypti and Ae. albopictus populations used in this experiment were collected in Rio de Janeiro (RJ) and Macapá (MC)—Brazil, Key West (KW) and Okeechobee (OK), Florida—United States (Fig 1, Table 1). All gathering of entomological samples were done on public land. We chose collection sites based on allopatric Ae. aegypti to Ae. albopictus (MC and KW) and sympatric populations (RJ and OK). Some of these areas report local transmission of chikungunya cases (RJ and MC) while others are located near regions in Florida where local transmission has occurred (Miami-Dade, Palm Beach, St. Lucie, and Broward Counties) (KW and OK) [12, 42]. In Brazil, eggs of both species were obtained from oviposition traps during a routine entomological survey. Aedes albopictus from a sympatric population (RJ) were obtained at the Oswaldo Cruz Foundation campus, in the Manguinhos neighborhood in March 2015 from 50 oviposition traps using methods described elsewhere [16]. Aedes aegypti eggs from an allopatric population (MC) were collected with oviposition traps by personnel from the Amapá State Health Secretary in May 2015. In United States, eggs of allopatric Ae. aegypti (KW) were collected in March 2015 with oviposition traps by personnel of Florida Keys Mosquito Control District. Immatures of sympatric Ae. albopictus (OK) were collected from tires in October 2015.
Fig 1. Location of Ae. aegypti and Ae. albopictus collected from allopatric and sympatric populations in Brazil and United States.
Table 1. Mosquito populations used in this study by country of collection from Brazil and the United States.
| Country | Location | coordinates | Species | Climate | Strain | Generation tested |
|---|---|---|---|---|---|---|
| Brazil | Macapá, Amapá | 0°02'N 51°04' W | Ae. aegypti | Tropical Wet | Allopatric | F3 |
| Brazil | Manguinhos, Rio de Janeiro | 22°52’S 43°14’W | Ae. albopictus | Tropical Wet and Dry | Sympatric | F3 |
| United States | Key West, Florida | 24°33'N 81°46'W | Ae. aegypti | Tropical savanna | Allopatric | F3 |
| United States | Okeechobee, Florida | 27°14'N 80°50'W | Ae. albopictus | Humid subtropical | Sympatric | F2 |
Field-collected mosquitoes (eggs or larvae) were reared in pans containing 1 L of tap water (100 larvae per pan) to adulthood on a diet with 0.6 g of equal amounts of brewer’s yeast and lactalbumin. Mosquitoes were held in a climate controlled room at 26–28°C and a photoperiod of 14:10 hours light:dark. Upon pupation, pupae were collected daily and placed in vials with a cotton seal until eclosion after which adult mosquitoes were identified to species. Adults were transferred to 0.3m3 cages and provided with 10% sucrose solution and water from cotton wicks and allowed to feed on bovine blood once per week using an artificial feeding system with hog intestine membranes. Females and males were held together for eleven days after which females were transferred to cylindrical cages (ht. by dia., 10 cm by 10 cm, 50 females/cage) with mesh screening one day before being fed CHIKV infected blood. The F2 (Okeechobee) and F3 (Rio de Janeiro, Macapá and Key West) generations progeny of field-collected Ae. aegypti and Ae. albopictus were used for the CHIKV infection study.
Virus and mosquito oral infection
The strain of CHIKV (Asian lineage, GenBank accession: KJ451624) used was isolated from the serum of an infected human in the British Virgin Islands in 2013. The Centers for Disease Control and Prevention was the source of the virus strain used in this study. The CHIKV isolate was passaged twice in culture using African green monkey (Vero) cells and viral titer was determined in 6-well plates seeded with Vero cells (American Type Culture Collection, ATCC) by plaque assay using a modified procedure by Kaur et al. (2016) [43].
For preparation of the virus suspension, monolayers of Vero cells were inoculated with dilute stock CHIKV at a multiplicity of infection of 0.1 followed by a one-hour incubation at 37°C and 5% carbon dioxide atmosphere. The American Type Culture Collection was the source of Vero cells used in this study. After the inoculation procedure, each flask received 24 ml media (M199 medium supplemented with 10% fetal bovine serum, penicillin/streptomycin and mycostatin) and was left to incubate for an additional 47-hours. Adult females aged 10–11 days were offered CHIKV infected defibrinated bovine blood (Hemostat, Dixon, CA) using an artificial feeding system with hog intestine membranes (Hemotek, Lancashire, United Kingdom). Samples of blood were taken of the virus-blood suspension at the time of feeding to determine the concentration of CHIKV ingested by the adult mosquitoes. Blood meal titers ranged from log10 7.3 to 8.3 plaque forming unit equivalents (pfue)/mL. Fully engorged females were held in cylindrical cages along with an oviposition substrate and maintained at a 14:10 hour light:dark photoperiod and 28°C.
Virus transmission potential using saliva assays was determined at 2, 5, and 13 days after feeding on infected blood. Mosquitoes were deprived of sucrose for 1-day and then individually transferred to plastic tubes fitted with a removable screen lid (37-mL 8 by 3 cm). Honey was dyed with blue food coloring (McCormick) and impregnated on filter paper (1 cm diameter) and fastened to the inside lid of the tube. Mosquitoes that fed on the honey deposited saliva and the blue food coloring was visualized in the crop with aid of an incandescent flashlight. Mosquitoes were examined for blue in the crop after 24 and 48-hours during the transmission assay. Only mosquitoes that fed on honey were used to assess transmission potential. Additionally, saliva was collected from another subset of mosquitoes in capillary tubes with immersion oil as described previously [44,32, 39]. Mosquitoes were stored at -80°C after the transmission assay and later dissected to test the legs and saliva for the presence of CHIKV RNA by qRT-PCR [32]. The sequence of primers targeting a nonstructural polyprotein gene was as follows: forward, 5'-GTACGGAAGGTAAACTGGTATGG-3': reverse, 5'-TCCACCTCCCACTCCTTAAT-3'. The probe sequence was: 5'-/56-FAM/TGCAGAACCCACCGAAAGGAAACT/3BHQ_1/-3' (Integrated DNA Technologies, Coralville, IA). Detection of CHIKV RNA in the legs of a mosquito is considered a proof that the virus infection has disseminated from the midgut, and we use the number of mosquitoes with a disseminated infection over the number of mosquitoes fully engorged on a viraemic blood-meal, as the virus dissemination rate. Detection of CHIKV RNA in mosquito saliva is considered a proof that the mosquito can transmit virus when feeding, and we use the proportion of mosquitoes with virus in saliva among all mosquitoes with a disseminated infection as our expression of transmission rate.
For each mosquito, legs were triturated in 1.0 mL of media (GIBCO Media 199). Saliva from mosquitoes was combined with 300 μL of media. RNA isolation on a 140 μL sample of mosquito legs and saliva homogenate was achieved using the QIAamp viral RNA mini kit (Qiagen, Valencia, CA) and eluted in 50 μL of buffer according to the manufacturer’s protocol. Viral RNA was detected using the Superscript III One-Step qRT-PCR with Platinum Taq kit by Invitrogen (Invitrogen, Carlsbad, CA) using methods described elsewhere [32, 39]. Quantitative RT-PCR was performed with the CFX96 Real-Time PCR Detection System (Bio-Rad Laboratories, Hercules, CA) with the following program: 50°C for 30 minutes, 94°C for 2 minutes, 39 cycles at 94°C for 10 seconds and 60°C for 1 minute, and 50°C for 30 seconds. The expression of viral titer in mosquito-derived samples used a standard curve method comparing cDNA synthesis for a range of serial dilutions of CHIKV in parallel with plaque assays of the same dilutions of virus, expressed as plaque forming unit equivalents (pfue)/ml [45].
Statistical analyses
We were interested in analyzing the relationship between the presence or absence of CHIKV in the legs and saliva (dependent variables) and the following independent variables: mosquito species (Ae. aegypti and Ae. albopictus), population origin (Brazil and USA), days post-infection (dpi, 2, 5 and 13), and a three-way interaction of species by population origin by days post-infection. Exploratory analyses were done using chi-square tests to verify possible relationships between both dependent variables (presence or absence of CHIKV in the legs and saliva) and each of the independent variables. We modeled this relationship using two separate binomial generalized linear models: one focused on the viral dissemination to the legs, and the other focused on the viral infection of saliva. To account for numerical problems in the viral dissemination binomial model, we used a Firth's Bias-Reduced Logistic Model [46]. We also analyzed the relationship between the viral titer of legs and saliva and the aforementioned main effects using a Gaussian generalized linear model. All analyses were done using R [47] and RStudio [48], with the libraries ggplot2 [49], logistf [46] and lsmeans [50].
Accession numbers
Chikungunya virus (Asian lineage, GenBank accession: KJ451624, repository: Centers for Disease Control and Prevention).
Results
Chikungunya virus disseminated infection by species, population origin and days post-infection
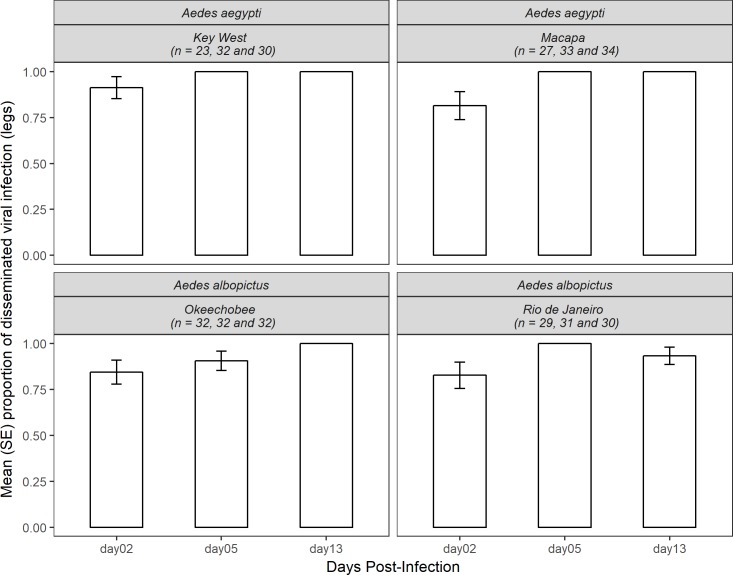
Chikungunya virus dissemination rates were measured by the proportion of mosquitoes that had infected legs from the total that fully engorged on infected blood. A total of 358 Aedes mosquitos were tested for disseminated infection (172 Ae. aegypti and 186 Ae. albopictus). Overall, our results showed the proportion of individuals of both species with disseminated infection significantly increased with each of the days post-infection analyzed (2-dpi, 0.847 ± 0.034; 5-dpi, 0.977 ± 0.013; and 13 dpi, 0.984 ± 0.011) (χ2 = 24.35, df = 2, p<0.0001). Aedes aegypti had higher dissemination rates than Ae. albopictus (mean ± SE, 0.960 ± 0.014 and 0.919 ± 0.020, respectively), although not significant (χ2 = 2.09, df = 1, p = 0.148). Both US and Brazilian populations of Ae. aegypti (0.976 ± 0.016 and 0.946 ± 0.023, respectively) had higher dissemination rates when compared to Ae. albopictus (0.915 ± 0.028 and 0.922 ± 0.028, respectively), but this difference was also not significant (χ2 = 0.03, df = 1, p = 0.857).
When analyzing the dissemination rates per species, population origin and days post-infection interaction, Ae. aegypti reached 100% of individuals at the 5th and 13th days, but the US population had higher dissemination rates at the 2nd day when compared to the Brazilian population (0.913 ± 0.06 and 0.814 ± 0.07, respectively) (Fig 2). These differences, however, were not significant (χ2 = 0.07, df = 2, p = 0.961). For Ae. albopictus, both US and Brazilian populations had similar dissemination rates at the 2nd day (0.843 ± 0.065 and 0.827 ± 0.071). At the 5th day, the US population had a lower dissemination rate when compared to the Brazilian population (0.906 ± 0.052 and 1.0, respectively). At the 13th day, the A. albopictus US population had a higher dissemination rate (1.0) than the Brazilian population (0.933 ± 0.046). The dissemination rate did not significantly differ between population origins (χ2 = 0.36, df = 2, p = 0.834) (Fig 2).
Fig 2. Mean (SE) dissemination rate of CHIKV in Ae. aegypti and Ae. albopictus of Key West, Macapá, Okeechobee and Rio de Janeiro populations at 2, 5 and 13 days post-infection.
Columns lacking error bars display 100% infection.
The three-way interaction Firth's bias-reduced logistic model results show that none of the main effects or the interactions were significant for disseminated infection rates (Table 2).
Table 2. Estimated effects of the population origin, species and days post-infection on dissemination rates and viral titer of chikungunya virus in Ae. aegypti and Ae. albopictus.
Bold entries indicate statistical significance (p < 0.05).
| Response | Effect | Estimate | Standard Error | 95% CI | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Disseminated infection | (Intercept) | 2.499 | 0.73 | 1.465 | 4.835 |
| Origin:US | 0.646 | 1.287 | -1.763 | 5.149 | |
| Species: Ae. albopictus | 0.069 | 1.03 | -2.252 | 2.306 | |
| Days:05 | 2.639 | 2.586 | 0.204 | 10.686 | |
| Days:13 | 2.659 | 2.578 | 0.011 | 10.7 | |
| Origin:US x Species: Ae. albopictus | -0.551 | 1.644 | -4.67 | 2.552 | |
| Origin:US x Days:05 | -0.666 | 3.743 | -9.026 | 7.305 | |
| Origin:US x Days:13 | -0.729 | 3.75 | -8.72 | 7.631 | |
| Species: Ae. albopictus x Days:05 | -0.111 | 3.67 | -8.47 | 7.874 | |
| Species: Ae. albopictus x Days:13 | -1.84 | 2.873 | -9.92 | 2.482 | |
| Origin: US x Species: Ae. albopictus x Days:05 | -1.413 | 4.7 | -9.85 | 7.025 | |
| Origin: US x Species: Ae. albopictus x Days:13 | 2.365 | 4.732 | -6.072 | 10.803 | |
| Viral titer in the legs | (Intercept) | 2.181 | 0.287 | 1.619 | 2.743 |
| Origin:US | 0.468 | 0.423 | -0.361 | 1.297 | |
| Species: Ae. albopictus | 0.378 | 0.399 | -0.404 | 1.159 | |
| Days:05 | 1.430 | 0.387 | 0.672 | 2.188 | |
| Days:13 | 1.938 | 0.384 | 1.185 | 2.691 | |
| Origin:US x Species: Ae. albopictus | -1.261 | 0.570 | -2.378 | -0.144 | |
| Origin:US x Days:05 | 0.210 | 0.562 | -0.891 | 1.311 | |
| Origin:US x Days:13 | -0.456 | 0.564 | -1.562 | 0.649 | |
| Species: Ae. albopictus x Days:05 | -0.017 | 0.546 | -1.087 | 1.052 | |
| Species: Ae. albopictus x Days:13 | -0.774 | 0.546 | -1.845 | 0.296 | |
| Origin: US x Species: Ae. albopictus x Days:05 | 0.324 | 0.776 | -1.197 | 1.846 | |
| Origin: US x Species: Ae. albopictus x Days:13 | 1.203 | 0.780 | -0.324 | 2.731 | |
When analyzing the viral titers in the mosquito legs, Gaussian model results show that days post-infection had a significant positive effect, and the interaction of species and population origin had a significant negative effect (Table 2). Overall, both populations of Ae. aegypti had lower levels of viral titer (expressed in log10 pfue/mL) in their legs at 2nd day post-infection, which increased and peaked at the 5th and 13th days (US; 2nd day = 2.884 ± 0.453, 5th day = 4.289 ± 0.179 and 13th day = 4.131 ± 0.053; and Brazilian 2nd day = 2.668 ± 0.411, 5th day = 3.610 ± 0.277 and 13th day = 4.119 ± 0.110). The same pattern was observed for Ae. albopictus for both US (2nd day = 2.060 ± 0.290, 5th day = 4.074 ± 0.263 and 13th day = 3.676 ± 0.244) and Brazilian populations (2nd day = 3.086 ± 0.362, 5th day = 3.971 ± 0.241 and 13th day = 3.988 ± 0.183) (S1 Fig).
Chikungunya virus saliva infection by species, population origin and days post-infection
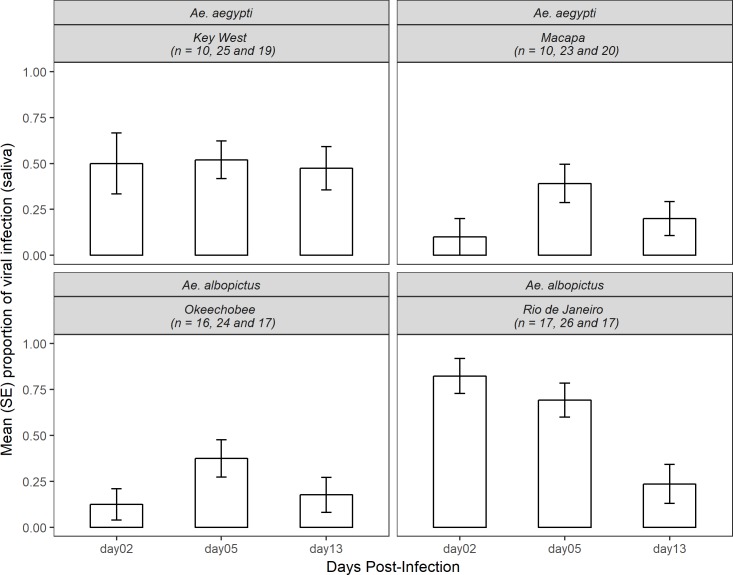
Chikungunya virus infection rates were measured by the proportion of mosquitoes that had infected saliva from the total that presented viral dissemination. A total of 224 Aedes mosquitoes that had positive leg infections were tested for saliva infection (107 Ae. aegypti and 117 Ae. albopictus). Overall, we found a significant effect of days post-infection and infection rates when analyzing both species (χ2 = 8.88, df = 2, p<0.05) (Fig 3). The infection rates reached a peak at the 5th day post-infection and decreased at the 13th day (2-dpi, 0.415 ± 0.068; 5-dpi, 0.500 ± 0.050; and 13-dpi, 0.274 ± 0.053). We also found a significant relationship between infection rates per species and population origin (χ2 = 11.55, df = 1, p<0.0001); US Ae. aegypti had higher infection rates when compared to the Brazilian (Ae. aegypti, 0.5 ± 0.068; Ae. albopictus, 0.264 ± 0.061). For Ae. albopictus, the US population had lower infection rates when compared to Brazilian conspecifics (0.245 ± 0.057 and 0.6 ± 0.063, respectively). The analysis of infection rates per species, population origin and days post-infection for Ae. aegypti showed that the US population had similar rates in all days (2-dpi, 0.5 ± 0.166; 5-dpi, 0.52 ± 0.101; 13-dpi, 0.473 ± 0.117). The Brazilian population had a lower infection rate when compared with the US population at all day’s post-infection (0.1 ± 0.1, 0.391 ± 0.2 and 0.104 ± 0.091, respectively), although this difference was not significant (χ2 = 1.32, df = 2, p = 0.67). For Ae. albopictus, the US population had a lower infection rate at the 2nd and 13th days (0.125 ± 0.085 and 0.176 ± 0.095, respectively) and higher infection rates at the 5th day (0.375 ± 0.1). The Brazilian population however had high infection rate at the 2nd day (0.823 ± 0.095), decreasing at the 5th day (0.692 ± 0.092) and finally decreasing further at the 13thday (0.235 ± 0.106). The Brazilian population had a higher infection rate at all day’s post-infection when compared to the US population, but this difference was not significant (Fig 2, χ2 = 3.05, df = 2, p = 0.238) (Fig 3).
Fig 3. Mean (SE) proportion of CHIKV saliva infection in Ae. aegypti and Ae. albopictus of Key West, Macapá, Okeechobee and Rio de Janeiro populations at 2, 5 and 13 days post-infection.
The three-way interaction logistic model results showed a significant effect of population origin, and the interactions between population origin x species, population origin x days post-infection and the three-way interaction of population origin x species x days post infection were significant for saliva infection rates (Table 3).
Table 3. Estimated effects of the population origin, species and days post-infection on the saliva infection rates and viral titer of caribbean CHIKV in Ae. aegypti and Ae. albopictus.
Bold entries indicate statistical significance (p < 0.05).
| Response | Effect | Estimate | Standard Error | 95% CI | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Saliva infection | (Intercept) | -2.197 | 1.054 | -5.112 | -0.526 |
| Origin:US | 2.197 | 1.2292 | 0.058 | 5.3 | |
| Species: Ae. albopictus | 3.738 | 1.2311 | 1.658 | 6.86 | |
| Days:05 | 1.755 | 1.1373 | -0.151 | 4.755 | |
| Days:13 | 0.811 | 1.1931 | -1.284 | 3.864 | |
| Origin:US x Species: Ae. albopictus | -5.684 | 1.5771 | -9.289 | -2.851 | |
| Origin:US x Days:05 | -1.675 | 1.3615 | -4.935 | 0.776 | |
| Origin:US x Days:13 | -0.916 | 1.4264 | -4.253 | 1.704 | |
| Species: Ae. albopictus x Days:05 | -2.485 | 1.3707 | -5.771 | -0.052 | |
| Species: Ae. albopictus x Days:13 | -3.53 | 1.468 | -6.946 | -0.873 | |
| Origin: US x Species: Ae. albopictus x Days:05 | 3.84 | 1.7856 | 0.534 | 7.745 | |
| Origin: US x Species: Ae. albopictus x Days:13 | 4.041 | 1.9345 | 0.392 | 8.172 | |
| Viral titer in the saliva | (Intercept) | 0.066 | 0.264 | -0.450 | 0.582 |
| Origin:US | 0.831 | 0.373 | 0.101 | 1.561 | |
| Species: Ae. albopictus | 0.836 | 0.332 | 0.185 | 1.487 | |
| Days:05 | 0.603 | 0.316 | -0.015 | 1.222 | |
| Days:13 | 0.217 | 0.323 | -0.415 | 0.850 | |
| Origin:US x Species: Ae. albopictus | -1.386 | 0.479 | -2.324 | -0.447 | |
| Origin:US x Days:05 | -0.677 | 0.444 | -1.546 | 0.193 | |
| Origin:US x Days:13 | -0.444 | 0.458 | -1.342 | 0.454 | |
| Species: Ae. albopictus x Days:05 | -0.464 | 0.409 | -1.265 | 0.338 | |
| Species: Ae. albopictus x Days:13 | -0.811 | 0.431 | -1.656 | 0.034 | |
| Origin: US x Species: Ae. albopictus x Days:05 | 0.593 | 0.586 | -0.554 | 1.741 | |
| Origin: US x Species: Ae. albopictus x Days:13 | 0.850 | 0.618 | -0.361 | 2.062 | |
The Gaussian model to analyze the viral titer in the saliva of the tested mosquitoes did not detect significant main effects or interactions of the treatment factors (Table 3). The US population of Ae. aegypti had similar levels of viral titer in the saliva at all three time-points tested (respectively 1.794 ± 0.593, 1.516 ± 0.247 and 1.351 ± 0.171 pfue/mL), while the Brazilian population had a peak at the 5th day and decreasing at the 13th day (respectively 1.659 ± 0.376 and 1.300 ± 0.429 pfue/mL). The US population of Ae. albopictus had higher viral titer in their saliva at the 2nd day, decreasing with each passing time point (2.290 ± 0.730, 1.036 ± 0.247 and 0.810 ± 0.228 pfue/mL). For the Brazilian population of this species, viral titer peaked at 5th days, decreasing at the 13th (respectively 1.095 ± 0.140, 1.501 ± 0.245 and 1.058 ± 0.458 pfue/mL) (S2 Fig).
Discussion
This study tested the vector competence of two populations of Ae. aegypti and Ae. albopictus from Brazil and Florida for an emergent Asian lineage of CHIKV. We carried out a series of experiments to determine two fundamental characteristics of this phenotypic trait: viral dissemination into the haemocoel of the tested mosquitos and saliva infection. These measurements characterize midgut and salivary gland barriers and are determinants of the vector competence of a mosquito population [26]. While viral dissemination indicates its propagation in the midgut and subsequent spread of the infection to other tissues, saliva infection is needed for the mosquito to successfully transmit the arbovirus by bite to a vertebrate host. Our results shed light on important questions regarding vector competence of Aedes mosquito populations of the Americas. The lack of statistical significance when comparing species and populations shows that viral dissemination occurs equally in these treatment conditions. In fact, more than 90% of all individuals have successful viral dissemination in their bodies, despite heterogeneity in species and population origin. This conclusion is further supported by the model results, which shows that none of the tested effects and interactions were statistically significant. Because high rates of disseminated infection were observed under these conditions, we had greater potential to detect treatment-dependent reductions in disseminated infection and less ability to identify treatment enhanced disseminated infection.
In our study, viral dissemination occurred rapidly, with around 85% of all individuals with positive legs at the 2nd day post-infection, and more than 98% of mosquitoes tested positive at the 13th day-post infection. Rapid viral dissemination together with a short extrinsic incubation period, as observed by saliva infection assays, may have important consequences for CHIKV epidemiology, especially given that both these Aedes species exhibit gonotrophic discordance [51, 52]. For instance, females will remain infectious for longer periods during the adult stage after ingesting CHIKV than pathogens with longer EIPs. Moreover, mosquito adult survival, EIP and host feeding strongly contribute to vectorial capacity which describes the number of infective bites received daily by a single host [53, 6]. A more thorough analysis showed that both populations of Ae. aegypti had similar levels of viral dissemination, reaching 100% of all tested individuals at the 5th day post-infection. For Ae. albopictus, we found a similar pattern with an increasing proportion of individuals with disseminated infection with each passing day post-infection. However, only the US population reached 100% of individuals with disseminated infection. This high number of individuals of both species and populations with disseminated infection might suggest a lack of substantial midgut escape barriers for the CHIKV strain used [31].
It is unclear whether differences in disseminated infection rates may be observed among these invasive Aedes mosquitoes if lower titer CHIKV infected blood were ingested. Studies have shown differences in susceptibility of Aedes vectors to CHIKV depending the dose of virus ingested [54, 55, 39]. Differences in susceptibility of Ae. aegypti and Ae. albopictus from Florida to infection and transmission of two lineages of CHIKV (Indian Ocean and Asian genotype) were tested [39]. In this study, Ae. aegypti tested with a lower dose of CHIKV Asian genotype in two different temperatures (25°C and 30°C) did not have significant differences in viral dissemination and transmission (100% to 40% and 33.3% to 0%, respectively). The low infection rates were attributed to a relatively low dose of CHIKV in blood meals (5.8 log10 pfue/ml). On the other hand, all populations of Ae. aegypti and Ae. albopictus presented higher susceptibility to infection and transmission for these two tested lineages of CHIKV at high titers [39, 54] determined the relative susceptibility of selected strains of Ae. aegypti and Ae. albopictus fed on a viremic monkey to infection with Southeast Asian strain of CHIKV. The results showed that strains of Ae. albopictus, regardless of their geographical origin, were more susceptible to infection (range, 72–97%) and dissemination (36–80%) with CHIKV than Ae. aegypti (infection rate, 12–25% and dissemination 8–25%) even though some strains presented lower infection rates in mosquitoes that ingested the lower dose (104.2–4.6 pfu/ml). Coffey et al. (2014) [55] summarizes numerous chikungunya virus infection with Ae. aegypti and Ae. albopictus, stating lower and higher doses used in infected blood meals. In this review, the authors showed that infection, dissemination, and transmission rates of both Aedes vectors can vary according to the geographic sources of mosquitoes and the titer of the ingested bloodmeal. For instance, using bloodmeal titers of > 7 log10 pfu/ml (high dose) presented 80% of Ae. aegypti from all locations develop disseminated infection. For Ae. albopictus, more than half became infected or develop disseminated infection. The infection and dissemination rates for US Ae. albopictus are dose-dependent and seem to increase with the titer of the ingested bloodmeal [21, 40, 55]. Vega-Rúa et al. (2014) [31] assessed 35 American Ae. aegypti and Ae. albopictus for three CHIKV genotypes with the titer of 107.5 pfu/ml, including mosquitoes populations from Brazil and Florida. Their study demonstrated that all 35 populations of both Aedes vectors were susceptible to CHIKV infection by all genotypes tested and that CHIKV transmission efficiency was highly heterogeneous in American mosquitoes ranging from 11.1% to 96.7%. Indeed, Ae. albopictus from Rio de Janeiro showed high transmission efficiencies even between geographically close populations, i.e., with some populations being able to transmit infectious viral particles as early as 2 days post-infection. However, the vector competence of Ae. aegypti and Ae. albopictus from Vero Beach was not tested for the Asian lineage of CHIKV, but for Indian Ocean and ancestral ECSA genotypes showed that transmission efficiencies were low (<30%).
The proportion of individuals with saliva infection was substantially lower than those with viral dissemination, suggesting salivary gland barrier(s) [31, 39]. Interestingly, US Ae. aegypti had almost twice as many infected individuals when comparing with the Brazilian population. A contrasting relation was observed for Ae. albopictus, with the Brazilian population reaching 60% of infected individuals against 24.5% from the US population. Thus, observed inherent differences in mosquito-virus interactions for both Ae. aegypti and Ae. albopictus might depend on geographic origin, which might impact disease transmission and contribute to its establishment in areas endemic for DENV and/or ZIKV. It is not clear whether heterogeneity exists in other traits that compose vector capacity, such as adult survival and biting rates, adult density, feeding behavior, and others, which would further influence CHIKV transmission and epidemiology in such areas [6]. Also, we observed that saliva infection declined with length of infection suggesting impaired transmission efficiency among older mosquitoes, most likely attributable to virus modulation of the infection as observed in other studies [56, 57]. Further studies on vector competence of Ae. aegypti and Ae. albopictus should be done to analyze the heterogeneity of dissemination and transmission of CHIKV among different populations of endemic or receptive areas for this arbovirus using a range of viral titers.
Supporting information
(TIF)
(TIF)
Acknowledgments
We thank Ricardo Lourenço-de-Oliveira for the valuable comments in the original postdoctoral project. We thank N. Nishimura, and S. Ortiz, for assistance maintaining mosquito colonies and in performing the experiments. We thank Ricardo Lourenço-de-Oliveira, Márcia Gonçalves de Castro, Célio Pinel and Ademir Martins for help with mosquito sampling in the field. We thank J. Newman for preparation of the Fig 1. We thank C. Pruszynski from the Florida Keys Mosquito Control District for providing us with Aedes aegypti eggs, and L.P. Lounibos from the Florida Medical Entomology Laboratory for providing us with Ae. albopictus larvae. The Asian lineage of chikungunya virus was graciously provided by the Centers for Disease Control and Prevention.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was funded by the Florida Department of Agriculture and Consumer Services, contract number 021802, BWA and LPL, http://www.freshfromflorida.com/. This study was also supported in part by the National Institutes of Health (NIAID, 1R21AI128188-01) as well as the CNPq—Science without Borders Program (Grant 206402/2014). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Weaver SC. Chikungunya in the New World: prospects for spread and health impact. PloS Negl Trop Dis. 2014;8(6):e2921 10.1371/journal.pntd.0002921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Volk SM, Chen R, Tsetsarkin KA, Adams AP, Garcia TI, Sall AA, et al. Genome-scale phylogenetic analyses of chikungunya virus reveal independent emergences of recent epidemics and various evolutionary rates. J Virol. 2010;84:6497–6504. 10.1128/JVI.01603-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pialoux G, Gauzère BA, Jauréguiberry S, Strobel M. Chikungunya, an epidemic arbovirosis. Lancet Infect Dis. 2007;7:310–327. 10.1016/S1473-3099(07)70107-X [DOI] [PubMed] [Google Scholar]
- 4.Weaver SC, Reisen WK. Present and future arboviral threats. Antiviral Res. 2010;85:328–345. 10.1016/j.antiviral.2009.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Honório NA, Câmara DCP, Calvet GA, Brasil P. Chikungunya: uma arbovirose em estabelecimento e expansão no Brasil. Cad Saúde Pública. 2015;31(5):1–3. 10.1590/0102-311XPE020515 [DOI] [PubMed] [Google Scholar]
- 6.Lounibos LP, Krammer LD. Invasiveness of Aedes aegypti and Aedes albopictus and vectorial capacity for chikungunya virus. JID. 2016;214(S5):S453–458. 10.1093/infdis/jiw285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leparc-Goffart I, Nougairede A, Cassadou S, Prat C, de Lamballerie X. Chikungunya in the Americas. Lancet. 2014. 383:514 10.1016/S0140-6736(14)60185-9 [DOI] [PubMed] [Google Scholar]
- 8.Lanciotti RS, Valadere AM. Transcontinental movement of Asian genotype chikungunya virus. Emerg Infect Dis. 2014;20(8):1400–1402. https://dx.doi.org/10.3201%2Feid2008.140268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan American Health Organization. 2015. Chikungunya. http://www.paho.org/hq/index.php?option=com_content&view=article&id=9053&Itemid=39843. Cited 10 April 2017.
- 10.Teixeira MJ, Andrade A, Costa MN, Castro J, Oliveira F, Goes CS, et al. East/Central/South/ African genotype chikungunya virus, Brazil, 2014. Emerg Infect Dis. 2015;21(5):906–907. 10.3201/eid2105.141727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan American Health Organization. 2017. Chikungunya. http://www2.paho.org/hq/?Itemid=40931. Cited 29 March 2017.
- 12.Secretaria de Vigilância em Saúde. 2017. Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vίrus Zika até a Semana Epidemiológica 15, 2017. http://portalarquivos.saude.gov.br/images/pdf/2017/maio/05/Monitoramento-dos-casos-de-dengue-febre-de-chikungunya-e-febre-pelo-virus-Zika-ate-a-Semana-Epidemiologica.pdf. Cited 20 May 2017.
- 13.Lounibos LP. Invasions by insect vectors of human disease. Annu Rev Entomol. 2002;47:233–266. 10.1146/annurev.ento.47.091201.145206 [DOI] [PubMed] [Google Scholar]
- 14.Agarwal A, Dash PK, Singh AK, Sharma S, Gopalan N, Rao PVL, et al. Evidence of experimental vertical transmission of emerging novel ECSA genotype of chikungunya virus in Aedes aegypti. PLoS Negl Trop Dis. 2014;8(7):e2990 10.1371/journal.pntd.0002990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawley WA. The biology of Aedes albopictus. J Am Mosq Control Assoc. 1988;1(Suppl.):S1–S39. [PubMed] [Google Scholar]
- 16.Braks MAH, Honório NA, Lourenço-de-Olveira R, Juliano SA, Lounibos LP. Convergent habitat segregation of Aedes aegypti and Aedes albopictus (Diptera: Culicidae) in Southeastern Brazil and Florida. J Med Entomol. 2003;40(6):785–794. 10.1603/0022-2585-40.6.785 [DOI] [PubMed] [Google Scholar]
- 17.Juliano AS, Lounibos LP, O’Meara GF. A field test for competitive effects of Aedes albopictus on A. aegypti in South Florida: differences between sites of coexistence and exclusion? Oecologia. 2004;139:583–593. https://dx.doi.org/10.1007%2Fs00442-004-1532-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lima-Camara TN, Honório NA, Lourenço-de-Oliveira R. Frequência e distribuição especial de Aedes aegypti e Aedes albopictus (Diptera: Culicidae) no Rio de Janeiro, Brasil. Cad Saúde Pública. 2006;22:2079–2084. 10.1590/S0102-311X2006001000013 [DOI] [PubMed] [Google Scholar]
- 19.Honório NA, Castro MG, Barros FS, Magalhães MAFM, Sabroza PC. The spatial distribution of Aedes aegypti and Aedes albopictus in a transition zone, Rio de Janeiro, Brazil. Cad Saúde Pública. 2009;25(6):1203–1214. 10.1590/S0102-311X2009000600003 [DOI] [PubMed] [Google Scholar]
- 20.Jupp PG, McIntosh BM. Chikungunya virus diseases In: TP Monath. The arboviruses: epidemiology and ecology, Vol. II Florida: CRC Press; 1988. Pp. 137–157. [Google Scholar]
- 21.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;12:e201 https://doi.org/10.1371/journal.ppat.0030201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vazeille M, Moutailler S, Coudrier D, Rousseaux C, Khun H, Huerre M, et al. Two Chikungunya isolates from the outbreak of La Réunion (Indian Ocean) exhibit different patterns of infection in the mosquito, Aedes albopictus. PLoS One. 2007;11:e1168 10.1371/journal.pone.0001168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsetsarkin KA, Chen R, Sherman MB, Weaver SC. Chikungunya virus: Evolution and genetic determinants of emergence. Curr Opin Virol. 2011;1(4):310–317. 10.1016/j.coviro.2011.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsetsarkin KA, Chen R, Yun R, Rossi SL, Plante KS, Guerbois M, et al. Multi-peaked adaptive landscape for chikungunya virus evolution predicts continued fitness optimization in Aedes albopictus mosquitoes. Nat Commun. 2014;5:4084 10.1038/ncomms5084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clements NA. The biology of mosquitoes Volume 3 Transmission of viruses and interactions with bacteria. Wallingford: CABI publishing; 2012 [Google Scholar]
- 26.Tabachnick WJ. Nature, nurture and evolution of intra-species variation in mosquito arbovirus transmission competence. Int J Environ Res Public Health. 2013;10:249–277. 10.3390/ijerph10010249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lambrechts L, Chevillon C, Albright RG, Thaisomboonsuk B, Richardson JH, Jarman RG, Scott TW. Genetic specificity and potential for local adaptation between dengue viruses and mosquito vectors. BMC Evol Biol. 2009;9:160 https://dx.doi.org/10.1186%2F1471-2148-9-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hardy JL, Houk EJ, Kramer LD, Reeves WC. Intrinsic factors affecting vector competence of mosquitoes for arboviruses. Ann Rev Entomol. 1983;28:229–262. 10.1146/annurev.en.28.010183.001305 [DOI] [PubMed] [Google Scholar]
- 29.Lambrechts L, Paaijmans KP, Fansiri T, Carrington LB, Kramer LD, Thomas MB, Scott TW. Impact of daily temperature fluctuations on dengue virus transmission by Aedes aegypti. Proc Natl Acad Sci USA. 2011;108:7460–7465. https://dx.doi.org/10.1073%2Fpnas.1101377108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lefevre T, Vantaux A, Dabire KR, Mouline K, Cohuet A. Non-genetic determinants of mosquito competence for malaria parasites. PLoS Pathog. 2013;9:e1003365 https://dx.doi.org/10.1371%2Fjournal.ppat.1003365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vega-Rúa A, Zouache K, Girod R, Failloux A-B, Lourenco-de-Oliveira R. High vector competence of Aedes aegypti and Aedes albopictus from ten American countries as a crucial factor of the spread of Chikungunya. J Virol. 2014;88(11):6294–306. 10.1371/journal.ppat.0030201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alto BW, Wiggins K, Eastmond B, Ortiz S, Zirbel K, Lounibos LP. Diurnal temperature range and chikungunya virus infection in invasive mosquito vectors. J Med Entomol. 2018;55(1):217–224. 10.1093/jme/tjx182 [DOI] [PubMed] [Google Scholar]
- 33.Richards SL, Anderson SL, Smartt C. Vector competence of Florida mosquitoes for chikungunya virus. J Vector Ecol. 2010;35(2):439–443. https://dx.doi.org/10.1111%2Fj.1948-7134.2010.00105.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zouache K, Fontaine A, Vega-Rua A, Mousson L, Thiberge JM, Lourenço-de-Oliveira R, et al. Three-way interactions between mosquito population, viral strain and temperature underlying chikungunya virus transmission potential. Proc Biol Sci. 2014;281(1792): 20141078 10.1098/rspb.2014.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonçalves CM, Melo FF, Bezerra JMT, Chaves BA, Silva BM, Silva LD, et al. Distinct variation in vector competence among nine field populations of Aedes aegypti from a Brazilian dengue-endemic risk city. Parasit Vectors. 2014;7:320 10.1186/1756-3305-7-320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lourenço-de-Oliveira R, Vazeille M, Filipis AMB, Failloux A-B. Aedes aegypti in Brazil: genetically differentiated populations with high susceptibility to dengue and yellow fever viruses. Trans R Soc Trop Med Hyg. 2004;98:43–54. 10.1016/S0035-9203(03)00006-3 [DOI] [PubMed] [Google Scholar]
- 37.Bennett KE, Olson KE, Muñoz ML, Fernández-Salas I, Farfán JA, Higgs S, et al. Variation in vector competence for dengue 2 virus among 24 collections of Aedes aegypti from Mexico and the United States. Am J Trop Med Hyg. 2002;67:85–92. 10.4269/ajtmh.2002.67.85 [DOI] [PubMed] [Google Scholar]
- 38.Reiskind MH, Pesko K, Westbrook CJ, Mores CN. Susceptibility of Florida mosquitoes to infection with chikungunya virus. Am J Trop Med Hyg. 2008;78(3):422–425. 10.4269/ajtmh.2008.78.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alto BW, Wiggins K, Eastmond B, Velez D, Lounibos LP, Lord CC. Transmission risk of two chikungunya lineages by invasive mosquito vectors from Florida and the Dominican Republic. PLoS Negl Trop Dis. 2017;11(7):e0005724 10.1371/journal.pntd.0005724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pesko K, Westbrook CJ, Mores CN, Lounibos LP, Reiskind MH. Effects of infectious virus dose and bloodmeal delivery method on susceptibility of Aedes aegypti and Aedes albopictus to chikungunya virus. J Med Entomol. 2009;46(2):395–399. 10.1603/033.046.0228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kraemer MUG, Sinka ME, Duda KA, Mylne AQN, Shearer FM, Barker CM, et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. eLife. 2015;4:e08347 https://dx.doi.org/10.7554%2FeLife.08347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. 2014. Press release. https://www.cdc.gov/media/releases/2014/p0717-chikungunya.html. Cited 24 May 2017.
- 43.Kaur P, Lee RCH, Chu JJH. Infectious viral quantification of chikungunya virus—virus plaque assay In: Chu J.J.H. and Ang S.K., editors. Chikungunya virus: Methods in Molecular Biology, vol. 1426 New York: Springer; 2016. pp. 93–103. [DOI] [PubMed] [Google Scholar]
- 44.Alto BW, Bettinardi D. Temperature and dengue virus infection in mosquitoes: Independent effects on the immature and adult stages. Am J Trop Med Hyg. 2013;88:497–505. 10.4269/ajtmh.12-0421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bustin S. Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol. 2000;25:169–193. 10.1677/jme.0.0250169 [DOI] [PubMed] [Google Scholar]
- 46.Heinze G, Ploner M. logistf: Firth's Bias-Reduced Logistic Regression. R package version 1.22. 2016. Available: https://cran.r-project.org/web/packages/logistf/index.html
- 47.R Core Team. R: A language and environment for statistical computing. 2016. https://www.r-project.org/
- 48.RStudio Team. RStudio: Integrated Development for R. 2012. https://www.rstudio.com/
- 49.Wickham H. ggplot2: Elegant Graphics for Data Analysis NewYork: Springer-Verlag; 2009. [Google Scholar]
- 50.Lenth RV. Least-Squares Means: The R Package lsmeans. J Stat Softw. 2016;69(1):1–33. 10.18637/jss.v069.i01 [DOI] [Google Scholar]
- 51.Braks MAH, Juliano SA, Lounibos LP. Superior reproductive success on human blood without sugar is not limited to highly anthropophilic mosquito species. Med Vet Entomol. 2006;20:53–59. https://dx.doi.org/10.1111%2Fj.1365-2915.2006.00612.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Farjana T, Tuno N. Multiple blood feeding and host-seeking behavior in Aedes aegypti and Aedes albopictus (Diptera: Culicidae). J Med Entomol. 2013;50:838–846. 10.1603/ME12146 [DOI] [PubMed] [Google Scholar]
- 53.Reisen WK. Estimation of vector capacity: introduction. Bull Soc Vect Ecol. 1989;14:39–40. [Google Scholar]
- 54.Turell MJ, Beaman JR, Tammariello RJ. Susceptibility of selected strains of Aedes aegypti and Aedes albopictus (Diptera: Culicidae) to chikungunya virus. J Med Entomol. 1992;29:49–53. 10.1093/jmedent/29.1.49 [DOI] [PubMed] [Google Scholar]
- 55.Coffey LL, Failloux AB, Weaver SC. Chikungunya virus-vector interactions. Viruses 2014;6:4628–4663. https://dx.doi.org/10.3390%2Fv6114628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salazar MI, Richardson JH, Sánchez-Vargas I, Olson KE, Beaty BJ. Dengue virus type 2: replication and tropisms in orally infected Aedes aegypti mosquitoes. BMC Microbiol. 2007;7:9 https://dx.doi.org/10.1186%2F1471-2180-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sánchez-Vargas I, Scott JC, Poole-Smith BK, Franz AWE, Barbosa-Solomieu V, Wilusz J, et al. Dengue virus type 2 infections of Aedes aegypti are modulated by the mosquito’s RNA Interference pathway. PLoS Path. 2009;5(2):e1000299 10.1371/journal.ppat.1000299 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.