Abstract
Introduction.
Rapid eye movement (REM) sleep-related bradyarrhythmia syndrome is characterized by pathological asystoles during the REM sleep phase. It is a rare rhythm disorder, being reported only few times in the literature. Due to non-specific symptoms, REM sleep-related bradyarrhythmia might be often underdiagnosed. Other cardiac diseases associated with pathological sinus arrests must be excluded to establish the correct diagnosis of and appropriate therapy for REM sleep-related bradyarrhythmia. We report a case of this syndrome followed by hypertension and diastolic heart failure.
The case.
A 49-year-old male with severe hypertension presented for a cardiologist’s consultation. His main complaints were palpitations, fatigue, dyspnoea, and snoring. Polysomnography test revealed a normal sleep structure with episodes of bradycardia and increased parasympathetic activity during phasic events of REM sleep. Heart rate variability Poincare plot analysis demonstrated similar results. REM sleep-related bradyarrhythmia syndrome was diagnosed and patient was treated with dual chamber heart pacemaker implantation.
Discussion.
Various components of the autonomic nervous system influence the development of REM sleep-related bradyarrhythmia syndrome. The main factor is likely an increased vagal tone during the phasic REM sleep with the absence of normal compensatory sympathetic activity. Concomitant hypertension in REM sleep-related bradyarrhythmia syndrome is caused by a paradoxically abnormal control of the autonomic nervous system and can be explained through the acetylcholine metabolism pathway. Best suited diagnostic and treatment options for REM sleep-related bradyarrhythmia syndrome are discussed.
Conclusions.
Patients with REM sleep-related bradyarrhythmia syndrome often present with indistinct symptoms. Polysomnography is an essential diagnostic test for the differential diagnosis of various nocturnal arrhythmias and sleep disorders. Severe hypertension is a common complication of sleep disorders and requires appropriate treatment of the underlying condition. An implantation of a heart pacemaker is the first-choice treatment for patients with REM sleep-related bradyarrhythmia syndrome.
Keywords: rapid eye movement sleep-related bradyarrhythmia syndrome, autonomic nervous system, acetylcholine, hypertension, polysomnography
Abstract
ITIN RETAS REM MIEGO FAZĖS BRADIARITMIJOS SINDROMAS SU GRETUTINE SUNKAUS LAIPSNIO HIPERTENZIJA: KLINIKINIO ATVEJO PRISTATYMAS IR LITERATŪROS APŽVALGA
Santrauka
Įvadas. Greito akių judėjimo (REM) miego bradiaritmijos sindromo išskirtinis bruožas – patologinės asistolės REM miego fazės metu. Tai retas ritmo sutrikimas, mokslinėje literatūroje aprašytas vos keliolika kartų. REM miego bradiaritmijos sindromui nebūdingi specifiniai simptomai, todėl jis gali būti dažnai klaidingai nenustatomas. Prieš patvirtinant galutinę diagnozę ir gydymą, būtina atmesti bet kokia kitą širdies patologijos diagnozę, susijusią su sinusinėmis pauzėmis. Straipsnyje pristatome šio sindromo atvejį, kuris komplikavosi hipertenzija ir diastoliniu širdies nepakankamumu.
Atvejis. Keturiasdešimt devynerių metų vyras su sunkia hipertenzija atvyko kardiologo konsultacijai. Pagrindiniai paciento nusiskundimai buvo: širdies permušimai, nuovargis, dusulys ir knarkimas. Polisomnografijos tyrimas parodė normalią miego eigą su bradikardijos epizodais ir padidėjusia parasimpatinės nervų sistemos veikla REM miego fazės metu. Diagnozuotas REM miego bradiaritmijos sindromas, pacientas gydytas implantuojant dviejų kamerų širdies stimuliatorių.
Aptarimas. REM miego bradiaritmijos sindromą išsivystyti skatina įvairūs autonominės nervų sistemos komponentai. Pagrindinis veiksnys – padidėjęs klajoklio nervo aktyvumas REM miego fazės metu be kompensacinės simpatinės nervų sistemos veiklos. Paradoksaliai nenormali autonominės nervų sistemos veikla skatina gretutinės hipertenzijos išsivystymą, kurį galima paaiškinti acetilcholino apykaitos ypatumais.
Išvados. Pacientams, sergantiems REM miego bradiaritmijos sindromu, nebūdingi išskirtiniai simptomai. Polisomnografija yra svarbiausias diagnostinis testas, atliekant miego sutrikimų ir naktinių aritmijų sindromų diferencinę diagnostiką. Sunki hipertenzija yra dažna miego sutrikimų komplikacija, reikalaujanti atitinkamo predisponuojančios priežasties gydymo. Širdies stimuliatoriaus implantacija yra pirmo pasirinkimo REM miego bradiaritmijos sindromo gydymo metodas.
Raktažodžiai: greito akių judėjimo fazės miego bradiaritmijos sindromas, autonominė nervų sistema, acetilcholinas, hipertenzija, polisomnografija
INTRODUCTION
Night-time arrhythmia and its complications remain an ambiguous scientific and therapeutic field of cardiology. The autonomic nervous system and various pathologic conditions are the key regulators of the cardiac rhythm during sleep (1). Although most sleep-related arrhythmias are detected incidentally on Holter recordings and are benign, some, like rapid eye movement (REM) sleep-related bradyarrhythmia syndrome, are associated with serious adverse effects (2). REM sleep-related bradyarrhythmia is a very rare syndrome characterized by bradyarrhythmic episodes and asystoles during REM sleep, and is not associated with sleep apnoea or hypoxia (3). Since its first description by Guilleminault et al. in 1984, only few cases were reported in worldwide medical literature. Due to non-specific daytime symptoms such as faintness, light-headedness, and atypical thoracic pain, patients suffering from REM-related bradyarrhythmia are often underdiagnosed (3). However, early recognition and appropriate therapy of REM sleep-related bradyarrhythmia can help prevent life-threatening consequences. We report a case of REM sleep-related bradyarrhythmia syndrome followed by hypertension and diastolic heart failure.
CASE REPORT
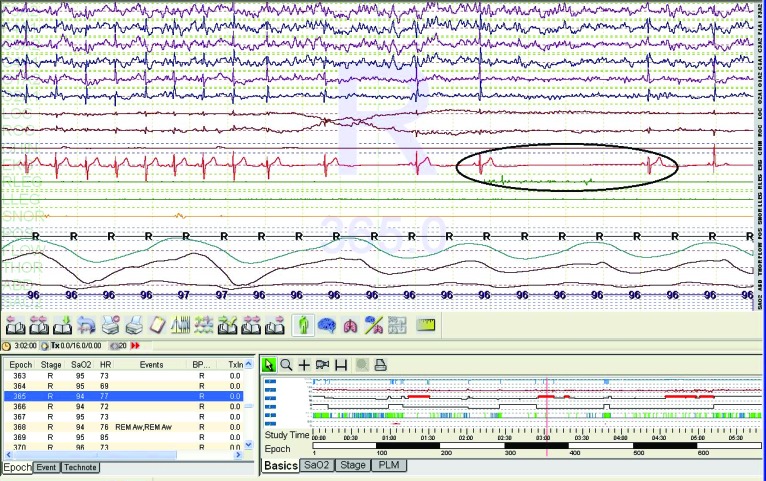
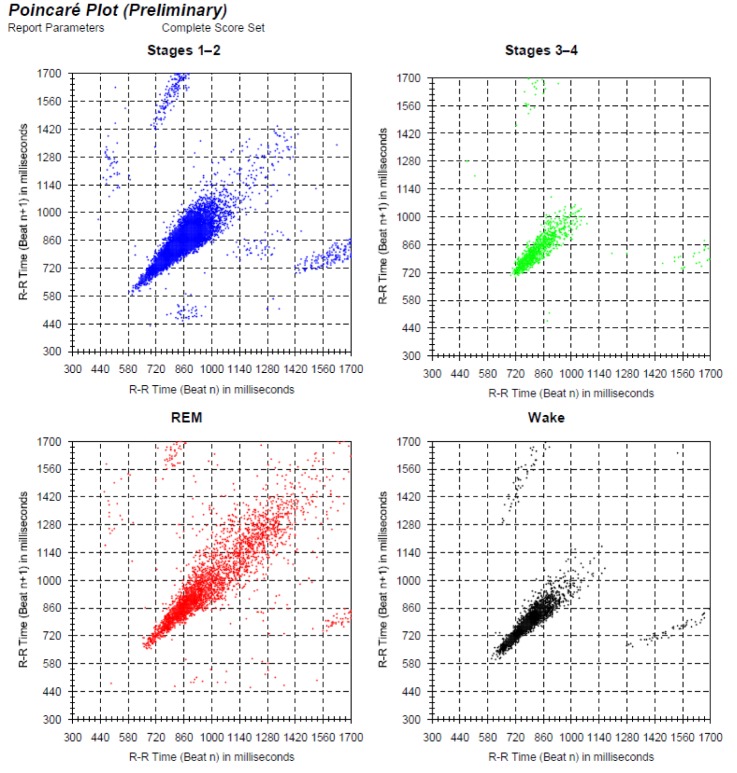
A 49-year-old male was referred to the Cardiology Department due to frequent paroxysmal tachisystolic episodes of atrial fibrillation, dyspnoea, and snoring at night. The patient was overweight (BMI 33.9 kg/m2) and suffered from severe hypertension (blood pressure (BP) at rest 215/110 mmHg, mean 24 h BP 184/105 mmHg). He was treated with Valsartan/Hydrochlorothiazide 160/12.5 mg in the morning and Valsartan/Amlodipine 160/10 mg in the evening, and Torasemide 10 mg three times a week. Echocardiography revealed left ventricle (LV) hypertrophy (MMI-135 g/m2) and diastolic dysfunction (mean E/E’ ratio 15). The exercise stress test was normal. Twentyfour-hour Holter ECG monitoring exhibited 40 episodes of bradycardia with minimal heart rate (HR) – 21 beats/min and nine sinus arrest episodes with a maximal pause of 5.5 s. HR varied from 46–128 beats/min (avg. 95 beats/min). Episodes of bradycardia were frequent at night-time and tachycardia presented during day hours. Based on the complaints and preliminary test results, a diagnosis of obstructive sleep apnoea was suspected. However, polysomnography tested negative. The test showed a normal sleep structure with no evidence of hypoxia or sleep-apnoea (Apnoea-Hypopnoea Index (AHI) 1.8 events/h). Importantly, episodes of bradycardia were documented only during phasic events of REM sleep (Fig. 1). Poincare plot analysis of heart rate variability revealed an increased parasympathetic activity in the REM sleep phase compared to wakefulness, and NREM sleep stages 1–3 (Fig. 2). REM sleep-related bradyarrhythmia syndrome was diagnosed. The patient was treated with dual chamber heart pacemaker implantation. Beta-blockers were added for rhythm control. Treatment resulted in improvement of the patient’s condition. His office BP lowered to 145/80 mmHg, mean 24 h BP reduced to 138/82 mmHg. Antihypertensive treatment regime remained unchanged.
DISCUSSION
Although REM sleep-related bradyarrhythmia syndrome has drawn attention of sleep medicine specialists and arrhythmologists, the rareness of this syndrome results in poor literature data. To date, only 18 cases of REM sleep-related sinus arrest were identified according to a review published in 2011 (4). However, intermittent nocturnal sinus arrest can be found in up to 39% of healthy asymptomatic adults, which suggests that REM sleep-related bradyarrhythmia may be a much more common entity than currently believed. Similarly to our case, the majority of identified cases of REM-related bradyarrhythmia syndrome were reported in young or middle-aged men. However, it is not yet known whether this reflects a sampling bias or indicates a physiological gender difference (4).
The most common complication of sleep disorders is hypertension (5). For example, 50–56% of individuals with obstructive sleep apnoea (OSA) are hypertensive, and an estimated 30–40% of hypertensive subjects have OSA (6–9). However, no cases of concomitant hypertension were previously described in REM sleep-related bradyarrhythmia syndrome. Instead, the most common complications include syncopes and an imminent threat of sudden cardiac death (2).
Fig. 1.
Polysomnography test. Paradoxical bradycardia and 5.5 s asystole in REM sleep stage
Our patient presented with night-time arrhythmias recorded during phasic events of REM sleep. In general, the nocturnal heart rate is determined by the interaction between parasympathetic and sympathetic nervous systems. The latter acts upon sleep state cycles, whereas the parasympathetic system is influenced by circadian rhythms (10). Studies on healthy human volunteers suggest that stages of NREM sleep represent a continuum of increasing parasympathetic dominance from waking to deep sleep (11). In contrast, REM sleep is characterized by sympathetic dominance and suppression of the parasympathetic nervous system indicated by significantly reduced heart rate variability (12). REM sleep bradyarrhythmia is most likely caused by abnormal autonomic modulation: an increased vagal tone during phasic REM sleep with absence of normal compensatory sympathetic activity.
We hypothesize that our patient’s hypertension was caused by a paradoxically abnormal autonomic nervous system control and explain it through the acetylcholine metabolism pathway. The main neurotransmitter of the parasympathetic nervous system is acetylcholine, which is produced from the interaction of choline and acetyl coenzyme A (CoA). The latter is produced in the glucose breakdown cycle; therefore, hypoglycaemia is one of the causes that lead to cholinergic deficit (13). The combination of increased nocturnal vagal activity and nightly fasting may contribute to cholinergic depletion and subsequent autonomic dysregulation. Therefore, bradyarrhythmic episodes manifest due to increased vagal activity during REM sleep, and hypertension is caused by a paradoxical sympathetic overactivity with aberrant inhibition of parasympathetic system at the rest of the time. Our patient’s increased mean 24 h heart rate and sinus tachycardia, as well as an effective beta-blocker therapy may confirm the hypothesis.
Although many sleep disorders can be diagnosed using medical history alone, our case of REM sleep-related bradyarrhythmia syndrome proves that common symptoms of sleep disorders overlap and REM sleep-related bradyarrhythmia might be confused with OSA. Our patient’s Holter ECG test revealed sinus arrest episodes persisting up to 5.5 seconds. Long-lasting cardiac pauses are associated with REM sleep-related bradyarrhythmia syndrome and with OSA syndrome, which should therefore be ruled out when investigating nightly pauses (14). However, REM sleep-related sinus arrests and atrioventricular (AV) blocks are not linked with episodes of apnoea or hypopnea. Therefore, overnight polysomnography is useful in assessing and distinguishing such disorders as OSA and REM sleep-related bradyarrhythmia syndrome (15). Accurate differential diagnosis between OSA and REM sleep-related bradyarrhythmia syndrome is crucial in determining the right treatment strategy for the underlying disease and its complications.
Fig. 2.
Sleep-time heart rate variability analysis by Poincaré plot illustrates an increased parasympathetic activity in REM sleep stage and sympathetic overactivity during the rest of the day
Many patients with REM sleep-related bradyarrhythmia syndrome are relatively asymptomatic and there currently is no standardized treatment for this condition (4). Several drugs like atropine, protriptyline and amitriptyline that block vagal-cardiac input have been tried in a limited number of patients, but the success rate was elusive (16). All patients treated with atropine or an anticholinergic agent had the drug discontinued due to adverse side effects (4). Few experimental treatment options like selective vagotomy exist, but there currently is no reported data of its efficacy in humans (17). Our patient was treated with the implantation of dual chamber heart pacemaker. The use of implantable cardiac pacemakers is the most common treatment strategy for REM sleep-related bradyarrhythmia syndrome (4). According to the American College of Cardiology/American Heart Association guidelines (18), pacemaker implantation is the only recommended class I indication for documented periods of asystole greater than or equal to 3.0 s, or any escape rate less than 40 beats per minute in awake, symptom-free patients with high-grade atrioventricular block and generally discouraged in the case of asymptomatic sinus arrests.
According to the literature, of the eight reported cases of REM-related sinus arrest, 75% were treated with implantable cardiac pacemakers. Of five patients with long-term follow-up, all were asymptomatic at a mean follow-up of 3.7 years (4, 14, 19). After pacemaker implantation, our patient’s condition also improved as episodes of night dyspnoea disappeared.
CONCLUSIONS
REM sleep-related bradyarrhythmia syndrome often displays indistinct features, but it can also be asymptomatic. Autonomic nervous system derangements and acetylcholine metabolism disturbances influence the development of hypertension in REM sleep-related bradyarrhythmia syndrome. Implantation of heart pacemaker is an effective treatment for REM sleep-related bradyarrhythmia syndrome. Recognition and appropriate management of concomitant pathologies is crucial in achieving good outcomes for patients with REM sleep-related bradyarrhythmia syndrome.
Acknowledgments
We thank Professor Rimgaudas Nemickas from the Lithuanian Hypertension Society for technical assistance and for providing in kind the necessary equipment for the examination of our patient described in this article.
Gabrielius Jakutis, Vytautas Juknevičius, Jūratė Barysienė, Dalia Matačiūnienė, Birutė Petrauskienė, Žaneta Petrulionienė, Aleksandras Laucevičius
References
- Gula LJ Krahn AD Skanes AC Yee R Klein GJ. . Clinical relevance of arrhythmias during sleep: guidance for clinicians. Heart. 2004; 90(3): 347–52. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duba AS, Jasty S, Mahajan A, Kodadhala V, Khan R, Rai P, Ghazvini M. Rare case of rapidly worsening rem sleep induced bradycardia. Case Rep Cardiol. 2015; . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini A Dolso P Gigli GL et al. . Rem sleep brady-arrhythmias: An indication to pacemaker implantation? Sleep Med. 2012; 13(6): 759–2. . [DOI] [PubMed] [Google Scholar]
- Holty JEC, Guilleminault C. REM-related bradyarrhythmia syndrome. Sleep Med Rev. 2011; 15(3): 143–51. . [DOI] [PubMed] [Google Scholar]
- Calhoun DA Harding SM. . Sleep and Hypertension. Chest. 2010; 138(2): 434–43. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB. Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med. 1985; 103(2): 190–5. . [DOI] [PubMed] [Google Scholar]
- Lavie P Ben-Yosef R Rubin AE. . Prevalence of sleep apnea syndrome among patients with essential hypertension. Am Heart J. 1984; 108(2): 373–6. . [DOI] [PubMed] [Google Scholar]
- Worsnop CJ, Naughton MT, Barter CE, Morgan TO, Anderson AILA, Pierce RJ. The prevalence of obstructive sleep apnea in hypertensives. Am J Respir Crit Care Med. 1998; 157(1): 111–5. . [DOI] [PubMed] [Google Scholar]
- Drager LF Genta PR Pedrosa RP et al. . Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol. 2010; 105(8): 1135–9. . [DOI] [PubMed] [Google Scholar]
- Burgess HJ, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol. 1997; 273(4 Pt 2): H1761–8. [DOI] [PubMed] [Google Scholar]
- Colten HR, Altevogt BM. Sleep disorders and sleep deprivation: an unmet public health problem. Chapter 2: Sleep Physiology. [PubMed] [Google Scholar]
- Elsenbruch S, Harnish MJ, Orr WC. Heart rate variability during waking and sleep in healthy males and females. SLEEP. 1999; 22(8): 1067–71. [DOI] [PubMed] [Google Scholar]
- Hshieh TT, Fong TG, Marcantonio ER, Inouye SK. Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol A Biol Sci Med Sci. 2008; 63(7): 764–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssens W, Willems R, Pevernagie D, Buyse B. REM sleep-related brady-arrhythmia syndrome. Sleep Breath. 2007; 11(3): 195–9. . [DOI] [PubMed] [Google Scholar]
- Ramar K, Olson EJ. Management of common sleep disorders. Am Fam Physician. 2013; 88(4): 231–8. [PubMed] [Google Scholar]
- Coccagna G, Capucci A, Pierpaoli S. A case of sinus arrest and vagal overactivity during REM sleep. Clin Auton Res. 1999; 9(3): 135–8. . [DOI] [PubMed] [Google Scholar]
- Viola AU Simon C Doutreleau S et al. . Abnormal heart rate variability in a subject with second degree atrioventricular blocks during sleep. Clin Neurophysiol. 2004; 115(4): 946–50. . [DOI] [PubMed] [Google Scholar]
- Epstein AE DiMarco JP Ellenbogen KA et al. . ACC/AHA/HRS 2008 Guidelines for device-based therapy of cardiac rhythm abnormalities. Heart Rhythm. 2008; 5(6): 934–955. . [DOI] [PubMed] [Google Scholar]
- Osuna E, Patiño G. REM sleep-related complete heart block: Is it a specific sleep-related disorder? Sleep Med. 2006; 7(4): 387–388. . [DOI] [PubMed] [Google Scholar]