ABSTRACT
Background
Organization and efficiency are central to success on busy inpatient services and may be relevant to demonstrating certain milestones. Most residents adopt these skills by observing supervisors and peers. For some, this method of emulation and adaptation does not occur, with the potential for a negative effect on patient care and team morale. Information on effective strategies for remediating organization and efficiency deficits is lacking.
Objective
We explored the major themes of organization and efficiency referred to the University of Pennsylvania Department of Medicine Early Intervention and Remediation Committee (EIRC), and developed tools for their remediation.
Methods
Assessments of residents and fellows referred to the EIRC between July 2014 and October 2016 were reviewed for organization and efficiency deficits. Common areas were identified, and an iterative process of learner observations and expert input was used to develop remediation tools.
Results
Over a 2-year period, the EIRC developed remediation plans for 4% of residents (13 of 342 total residents), and for 1 internal medicine subspecialty fellow. Organization and efficiency was the primary or secondary deficit in more than half of those assessed. Most common deficiencies involved admitting a patient efficiently, performing effective prerounding, and composing daily progress notes/presentations. Remediation tools that provided deconstruction of tasks to their most granular and reproducible components were effective in improving performance.
Conclusions
Deficits in organization and efficiency can disproportionately affect resident performance and delay milestone achievement. Many residents would benefit from detailed frameworks and assistance with new approaches to basic elements of daily work.
Introduction
First-year residents are not typically given explicit instructions about how to organize their day or complete their work efficiently. Program directors assume that, with experience, they will learn to manage a task list and triage it appropriately, often by modeling the behavior of their supervising residents. However, many residents struggle with organization, efficiency, and time management.
A survey of US internal medicine (IM) program directors reported that among residents who are struggling, 41% had difficulty with organization and prioritization.1 Deficiencies in time management and organization were also commonly reported by the University of Colorado's remediation program2 and in an earlier survey of IM program directors.3 These deficits become apparent when residents are late for rounds, deliver disorganized presentations, produce poor-quality documentation, or are unable to reliably complete their daily to-do list. These residents may be mislabeled with deficits in clinical reasoning or professionalism, and there are implications for patient care and team morale when a member of the team struggles.
Organization and efficiency is not a recognized clinical competency, and there is little information on strategies for remediating these deficits. We sought to determine the major themes of organization and efficiency deficits at our institution and develop tools for their remediation.
Methods
At the University of Pennsylvania, residents and fellows in the department of internal medicine who are not meeting appropriate milestones are referred to the Early Intervention Remediation Committee (EIRC) by the IM Clinical Competency Committee or program director. The EIRC chair performs a comprehensive assessment of each learner that includes a review of inpatient and outpatient evaluations as well as a 60-minute interview with the referred individual. This assessment yields a diagnosis of a primary deficit in 1 of the following areas: medical knowledge, clinical reasoning, organization and efficiency, professionalism, or communication skills.
The committee then develops an individualized remediation plan that typically involves direct observation with structured feedback within the context of the learner's current clinical rotation. The written plan includes descriptions of the intervention, time line, and benchmarks for success. After the plan components are completed, reassessment is performed by the Clinical Competency Committee utilizing input from EIRC chairs and new clinical evaluations.
We reviewed the remediation plans of all residents and fellows referred to the EIRC between July 2014 and October 2016. The most common deficiencies in organization and efficiency involved admitting a patient efficiently, performing systematic prerounding, and composing accurate daily progress notes. The components of each task were then broken down into specific, observable activities. We developed tools to address these areas through an iterative process of learner observations and expert input. Volunteer senior residents, fellows, and faculty were trained as clinical coaches and conducted direct observation, which entailed shadowing residents on the wards, recording the timing of each outlined step within their tasks, and providing structured reflection and immediate feedback on performance. Use of self-assessment tracking tools depended on the nature of the deficit and availability of an external observer.
This project was deemed exempt by the University of Pennsylvania Health System Institutional Review Board.
Results
During the study period, the EIRC developed individualized remediation plans for 13 residents (4% of 342 total residents) who were not meeting developmental milestones, and 1 IM subspecialty fellow referred by the fellowship director. Of these trainees, 7 had organization and efficiency as the primary deficit, and for 1 it was the secondary deficit. Following intervention, 3 of the 14 learners received letters of poor performance, and no trainee is on probation or has been dismissed. All are currently in good standing in their respective programs.
Admitting a Patient Efficiently
Residents who struggle with organization and efficiency often take several hours to complete a new patient admission. Despite peer advice, they may get bogged down at various stages of the admission process and become distracted by interruptions, such as pages or clinical status changes.
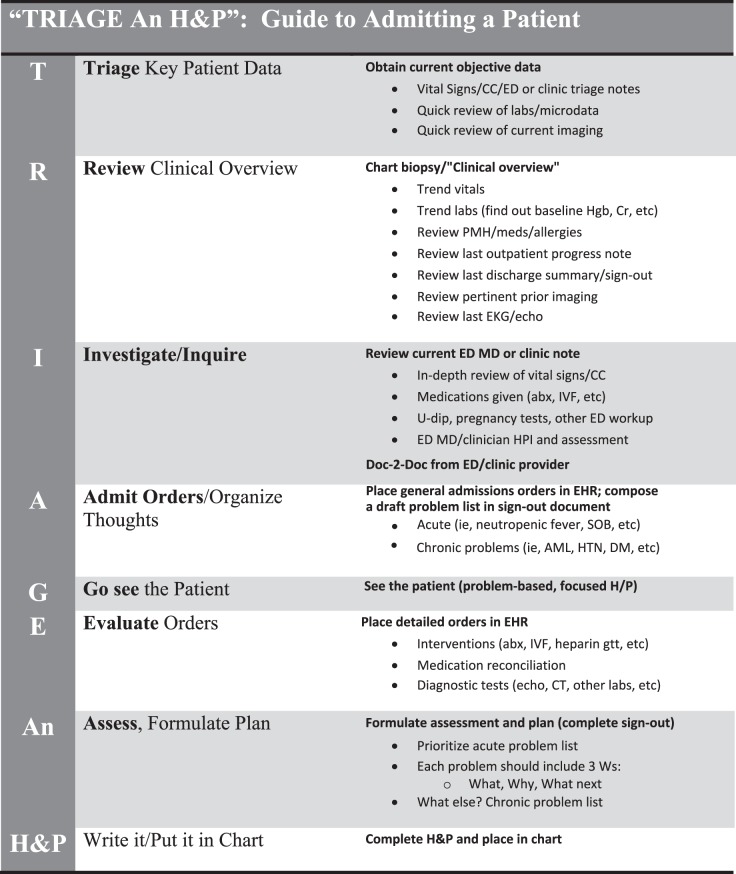
To help systematize this process, we developed TRIAGE An H&P (Figure 1). This mnemonic summarizes the steps involved in admitting a patient from the emergency department or the clinic, along with delineation of each step involved. A separate tracking spreadsheet was used to allow each task to be observed, timed, and marked for return when interruptions occur; this can also be used to facilitate reflection and review in later coaching sessions. Subsequent interventions may be tailored to the specific steps needed to address inefficiencies. The ordering of specific tasks can also be customized to the institution's specific clinical services or electronic health record system.
Figure 1.
TRIAGE An H&P mnemonic
Abbreviations: H&P, history and physical; CC, chief complaint; ED, emergency department; Hgb, hemoglobin; Cr, creatinine; PMH, past medical history; EKG, electrocardiogram; abx, antibiotics; IVF, intravenous fluid; U-dip, urine dip; HPI, history of present illness; EMR, electronic medical record; SOB, shortness of breath; AML, acute myeloid leukemia, HTN, hypertension, DM, diabetes mellitus; CT, computed tomography.
Conducting Meaningful and Efficient Prerounds
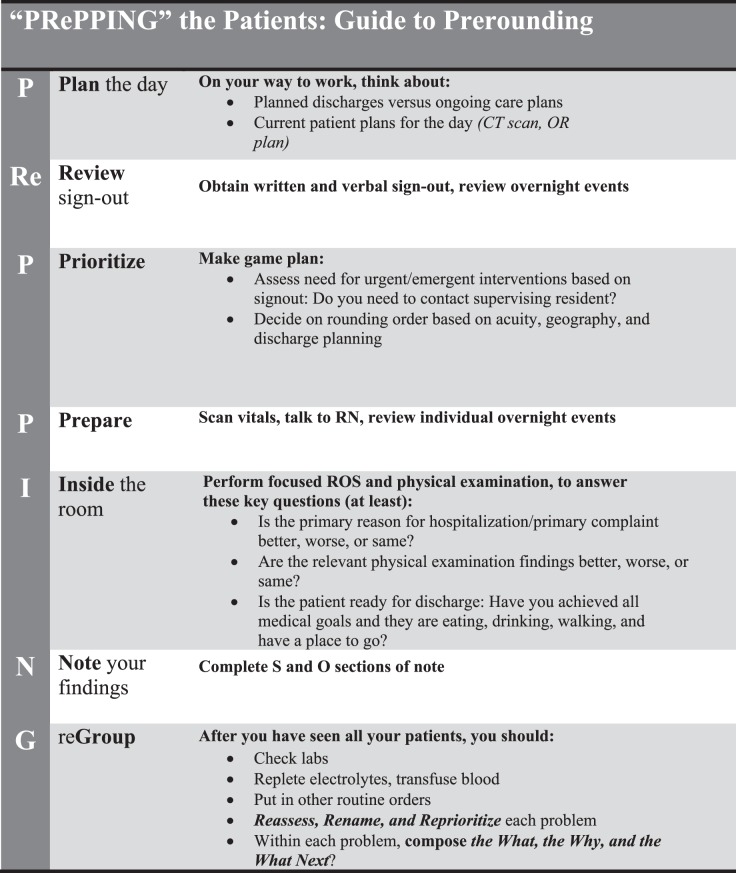
The time between morning arrival at the hospital and attending-run patient care rounds can cause residents struggling with organization and efficiency to feel pressured. We developed the PRePPING the Patient tool (Figure 2), which outlines the specific tasks involved in managing an active list of patients. Ideally, the process begins before arrival at the hospital and includes conscious preparation and mindfulness. Better time allocation for each task helps residents overcome logistical barriers, and specific expectations outline what must be accomplished during each patient interaction.
Figure 2.
PRePPING the Patient tool
Abbreviations: CT, computed tomography; OR, operating room; RN, registered nurse; ROS, review of systems; S and O, subjective and objective.
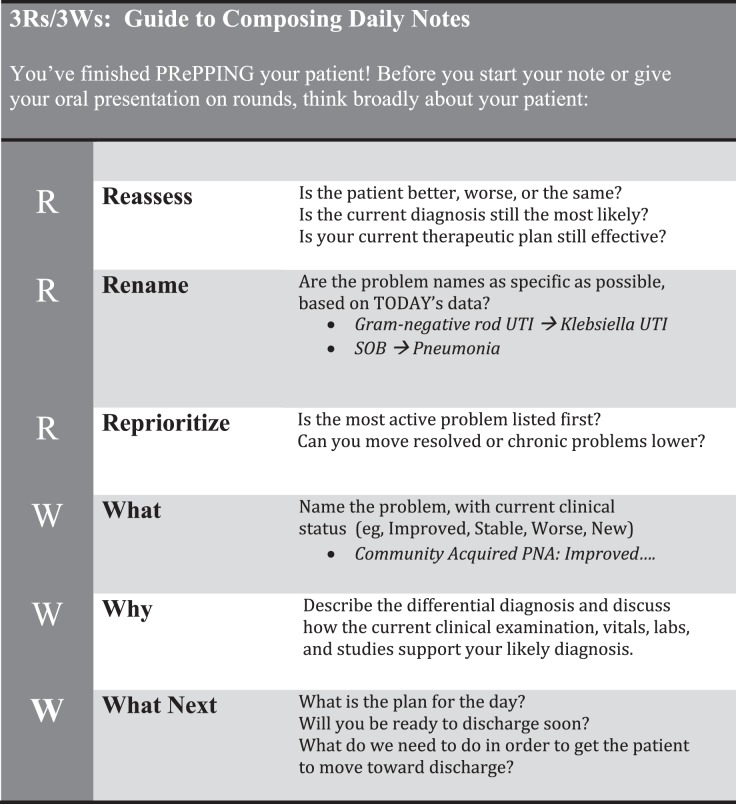
Organizing Oral Presentations and Written Progress Notes
Composing daily progress notes and summative oral presentations are significant components of a resident's daily work, and these should reflect accurate synthesis of all patient data. The pitfalls of cut-and-paste errors4 are well described, and many residents struggling with organization and efficiency rely heavily on previous documentation due to time constraints. We developed the 3Rs/3Ws framework (Figure 3) as a guide for composing updated and error-free progress notes and presentations. Each day, a resident should Reassess, Rename, and Reprioritize a patient's problems. Then, within each problem, the resident should address the What, Why, and What Next. This framework underscores the importance of thoughtful and timely formulation of a patient's daily assessment and plan, incorporating the most recent findings and events. The overwhelmed resident is provided with a structure by which to think critically and systematically demonstrate clinical reasoning.
Figure 3.
3Rs/3Ws framework
Abbreviations: UTI, urinary tract infection; SOB, shortness of breath; PNA, pneumonia.
Feasibility and Acceptability
Remediating a learner struggling with organization and efficiency is time intensive. The time spent remediating each referred resident and fellow varied from 25 to 75 hours, depending on the duration and intensity of the process required for the assessed deficits. The EIRC is composed of 14 faculty experts in remediation, led by 2 physician faculty members (graduate and undergraduate, each receiving 0.2 full-time equivalent). Funding is provided by an intraentity transfer from the medical school and the department of internal medicine budget. Nine residents and fellows served as peer organization and efficiency coaches. The EIRC strived to facilitate direct observation by the attending physician in the continuity clinic or inpatient setting. The majority of faculty and residents rated the overall process as positive.
Discussion
The assessment of residents referred to EIRC found that more than half of these learners struggled with organization and efficiency as a primary or secondary deficit. All learners were successfully remediated through a structured process that deconstructed complex tasks for routine clinical settings into precise steps, with direct observation tied to feedback. The program was feasible for a large residency and/or fellowship program, and it was acceptable to all participants.
Organization and efficiency is a critical element of a resident's performance. Most residents should be able to easily adopt these skills if modeled by supervisors and peers, but we know from the literature and from our own experience that many residents struggle with organization and efficiency. Efficient medical admissions during a busy hospital day, prerounding on existing patients within time constraints, and formulating a synthesized and accurate plan of care were areas of greatest challenge. Since this study's completion, the remediation program is still in existence, and organization and efficiency has remained the most common reason for referral.
We suspect organization and efficiency deficits are pervasive, even among those not requiring formal remediation, and many students, residents, and fellows would benefit from the fundamental approach of deconstructing complicated tasks to their granular components. This approach not only helped our struggling residents acquire and refine fundamental skills but also empowered them to engage in self-reflection and self-directed learning.5
Limitations of this study include that it was conducted at a single institution with a small sample, which limits generalizability. Without a comparison group, we do not know if the improvements seen were due to the intervention or if they were the results of usual resident maturation during training.
These tools and the remediation framework can be adapted by clinical educators in other programs and institutions. Next steps for research in this area include appropriate timing for interventions as well as further evaluation of the tools' effectiveness.
Conclusion
Deficits in organization and efficiency can disproportionately impact resident performance and may delay milestone achievement. Many residents would benefit from detailed frameworks and assistance with new approaches to basic elements of daily work.
References
- 1. Dupras DM., Edson RS., Halvorsen AJ., et al. “Problem residents”: prevalence, problems and remediation in the era of core competencies. Am J Med. 2012; 125 4: 421– 425. [DOI] [PubMed] [Google Scholar]
- 2. Guerrasio J., Garrity MJ., Aagaard EM. Learner deficits and academic outcomes of medical students, residents, fellows, and attending physicians referred to a remediation program, 2006–2012. Acad Med. 2014; 89 2: 352– 358. [DOI] [PubMed] [Google Scholar]
- 3. Yao DC., Wright SM. National survey of internal medicine residency program directors regarding problem residents. JAMA. 2000; 284 9: 1099– 1104. [DOI] [PubMed] [Google Scholar]
- 4. Weir CR., Hurdle JF., Felgar MA., et al. Direct text entry in electronic progress notes. An evaluation of input errors. Methods Inf Med. 2003; 42 1: 61– 67. [PubMed] [Google Scholar]
- 5. Nothnagle M., Anandarajah G., Goldman RE., et al. Struggling to be self-directed: residents' paradoxical beliefs about learning. Acad Med. 2011; 86 12: 1539– 1544. [DOI] [PubMed] [Google Scholar]