ABSTRACT
Background
Patients and families can make discriminatory comments leading to physician distress. Residents receive little training in appropriate responses to such comments and may be ill equipped to respond to intolerance without alienating the individual(s) making the comments.
Objective
We assessed whether a simulated curriculum would enhance pediatrics residents' ability to effectively respond to discriminatory comments.
Methods
In the 2016–2017 academic year, we modified an existing communication skills curriculum for senior pediatrics residents. Residents engaged a simulated parent who used discriminatory speech in 4 scenarios, followed by a group debriefing. We conducted anonymous surveys to assess residents' preparedness to respond to these comments before and immediately following participation and examined their experience with discriminatory comments in the workplace.
Results
The majority of residents reported prior experience with discriminatory comments (32 of 45 [71%] witnessed such comments, and 27 of 48 [56%] were targeted by such comments), most often regarding age, race, and ethnicity. Mean precourse scores ranged from 2.1 to 3.1 (on a 5-point scale) regarding ability to engage in a firm yet respectful dialogue, to reference the hospital code of conduct, to coach a learner to respond, and to facilitate a team debrief. Mean postcourse scores improved significantly for these questions (range 3.8–4.1). The greatest improvement was in referencing the code of conduct (2.1 versus 4.0, P < .001).
Conclusions
Immediately after participating in simulation, pediatrics residents reported a significant improvement in self-reported readiness to respond to discriminatory comments made by a parent and reported the simulation experience was beneficial.
What was known and gap
Residents report discrimination based on gender, race, and age and may lack training to appropriately respond when this occurs.
What is new
Pediatrics residents were exposed to simulation training with standardized parents in a scenario with discriminating comments about another member of the health care team.
Limitations
Small sample, self-reported efficacy data, and survey instrument without validity evidence may limit generalizability.
Bottom line
The simulation resulted in improvement in residents' self-reported readiness to respond to discriminatory comments.
Introduction
The Accreditation Council for Graduate Medical Education calls for an educational environment “that discourages discrimination and harassment by colleagues, supervisors, teachers, peers, other staff members, and patients.”1 Despite efforts to cultivate inclusive practice settings, residents report high rates of discrimination based on gender, race, and age, including a high incidence of discrimination from patients and their families.2 When surveyed, more than 60% of female medical residents reported experiencing gender-based discrimination by patients or their families.3 More than 35% of African-American, Hispanic, and Native American residents, and nearly 60% of Middle Eastern residents reported discrimination from patients.4 Discriminatory comments by patients or families may cause residents to feel disempowered and demoralized, which jeopardizes the therapeutic relationship, threatens an inclusive workplace, and compromises physician well-being.5
The American Academy of Pediatrics promotes resident training in culturally effective care.6 Ninety percent of 131 US pediatrics chairs surveyed incorporate cultural competency training into their residency programs.7 While the value of training residents to care for a diverse patient population is well established, we found no prior studies of interventions to address residents' readiness to respond appropriately to discriminatory comments. Some programs have identified strategies to help support residents when they encounter discriminatory comments in the workplace.8
To address this gap in education, we developed an experiential curriculum for pediatrics residents using simulated parents. We hypothesized that participating in this communication skills training would increase self-reported resident preparedness to address discriminatory comments in the clinical setting.
Methods
Setting and Participants
In this study, pediatrics residents participated in a series of simulated encounters that challenged them to confront discriminatory language and provided direct feedback to further develop communication skills. All pediatrics residents at the Children's Hospital of Pittsburgh, University of Pittsburgh Medical Center, participate in an annual communications course to simulate difficult conversations. Each group consisted of approximately 6 residents in the same postgraduate year (PGY), 2 faculty facilitators, and an actor portraying the simulated parent. Scenarios for each class were tailored to residents' level of training.
The study population consisted of PGY-2 pediatrics residents who participated in the communications course. PGY-3 residents served as a comparison group because they had previously participated in the course but had not practiced cases involving discriminatory comments. The PGY-3 group was used to separate the cumulative effect of residency experience from the effect of participation in the modified course.
Intervention
We modified the simulation for PGY-2 residents to have the simulated parent make discriminatory comments targeting members of the care team not present on rounds based on race, ethnicity, gender, or religion. The details of 4 such scenarios used in the course are included as online supplemental material.
The program employed 3 simulated parents from a local acting guild who received descriptions of the scenarios 1 to 2 weeks prior to the course, along with sample scripts to use during role playing. A 1-hour practice simulation was held with 1 simulated parent and faculty leadership prior to the course. Two faculty members were present for each resident group, and all faculty participants completed a 1-hour group facilitator training held approximately 2 weeks prior to the course. The course sessions lasted 2 hours and were held during protected resident time, allowing all residents to participate.
Prior to beginning the role playing, facilitators reviewed the hospital's code of conduct, which prohibits racist or culturally offensive remarks, and encouraged its use as a tool to underscore the hospital's commitment to an inclusive environment. They also discussed specific techniques to convey empathy. During the scenario, each resident was encouraged to respond to the simulated parent in a respectful but firm manner, focusing on the inappropriate behavior rather than the individual, and redirecting the simulated parent to the shared goal of caring for his or her child. Additionally, facilitators encouraged residents to empathize with any emotional distress that may underlie the expression of intolerant views. Specific approaches recommended to residents during the communications course are provided as online supplemental material. By practicing their responses to discriminatory comments, residents developed scripts to utilize in real-life interactions. After completing their turns, residents shared self-reflections on the experience and received skill-focused feedback from facilitators, peers, and the simulated parent. At the completion of the course, the facilitators led the residents in a group debriefing.
All PGY-2 and PGY-3 residents were asked to participate in a voluntary online survey 1 week prior to the course. The authors developed the survey without further testing. No incentives were provided. PGY-2 residents were also asked to respond to a follow-up survey within 1 week after their participation in the course. Survey participation was anonymous, and no unique identifiers were retained to protect residents' privacy, maximizing the response rate and minimizing bias in self-reported data.
Outcomes
The assessment evaluated self-reported resident abilities using a 5-point ordinal scale, with 1 indicating “I do not feel prepared,” 3 indicating “I feel moderately well prepared,” and 5 indicating “I feel very well prepared.” The survey assessed the following abilities: (1) recognizing one's emotions during the interaction; (2) engaging in a respectful yet firm dialogue; (3) referencing the hospital's code of conduct; (4) coaching a medical student/intern on his or her response for future encounters; (5) providing feedback to a medical student/intern on his or her response; and (6) facilitating a team debriefing after an encounter with discriminatory comments. Residents were also asked to report how frequently they directly received or witnessed discriminatory comments from patients or families during residency.
The University of Pittsburgh Institutional Review Board declared this study exempt.
Analysis
We calculated mean and median scores for responses to the 5-point scales. Differences between responses for PGY-2 pre- and postcourse groups and PGY-2 and PGY-3 postcourse groups were assessed with a Mann-Whitney U test. Statistical significance was defined as P < .05. We used descriptive statistics to summarize residents' experiences with discriminatory comments during their training.
Results
Of 32 eligible PGY-2 residents, 28 (88%) responded to the precourse survey and 19 (59%) responded to the postcourse survey. The comparison group consisted of 20 of 31 (65%) eligible PGY-3 residents. Of 67 overall responses, 61 (91%) completed the entire survey. Of the 6 residents who did not complete the survey, 3 omitted 1 to 2 responses from the numeric scale questions and 3 did not complete the section regarding exposure to prejudice at work.
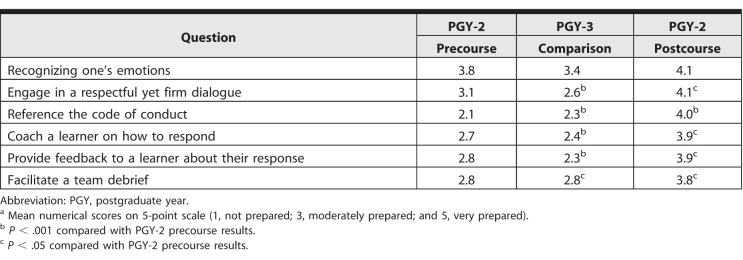
PGY-2 and PGY-3 residents reported significant prior exposure to discrimination in the workplace. Fifty-six percent (27 of 48) of responding residents reported being the target of at least 1 discriminatory comment during their residency, and 71% (32 of 45) had witnessed at least 1 discriminatory comment. Many indicated that they had personally experienced (33%, 16 of 48) or witnessed (53%, 24 of 45) 2 or more instances of discriminatory statements during their residency (Table 1). These discriminatory statements most often pertained to gender, race, ethnicity, or age (Table 2).
Table 1.
Frequency of Pediatrics Residents' Exposure to Discriminatory Commentsa
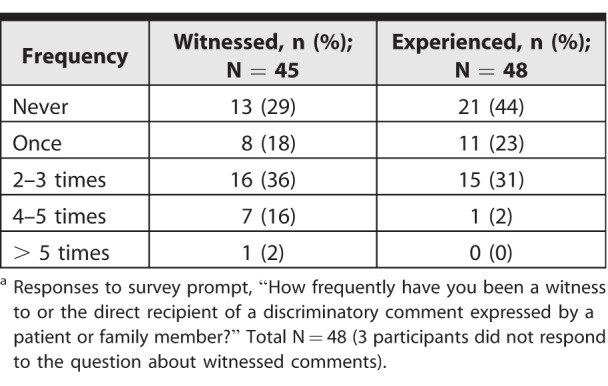
Table 2.
Types of Discriminatory Comments Reported by Pediatrics Residentsa
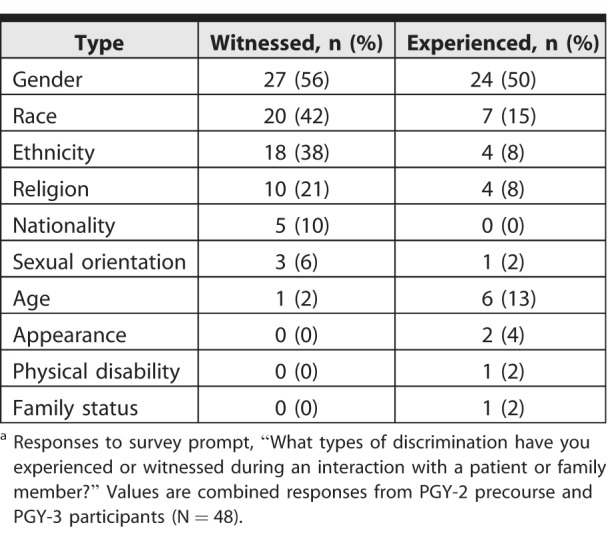
Overall, postcourse PGY-2 respondents reported improved levels of preparedness to confront discriminatory statements compared with precourse PGY-2 and PGY-3 respondents for all survey questions. Mean responses for precourse PGY-2 and PGY-3 residents ranged from 2.1 to 3.8 and 2.3 to 3.4, respectively (Table 3). With the exception of the first question regarding recognizing one's emotions, the remaining questions garnered mean responses of 3.1 or lower, representing less than moderately well prepared. Mean responses for postcourse PGY-2 respondents were substantially improved, ranging from 3.8 to 4.1. Improvements in immediate self-reported readiness for the PGY-2 postcourse group compared with both precourse PGY-2 and PGY-3 residents were statistically significant for questions 2 to 6 (Table 3).
Table 3.
Mean Preparedness Scores Before and After Course Participationa
For all questions, more than 60% of postcourse PGY-2 respondents reported themselves more than moderately prepared for the competencies queried (scores of 4 or 5). In contrast, for questions 2 through 6, only 15% to 35% of precourse PGY-2 respondents and 10% to 15% of PGY-3 respondents gave similarly favorable responses. Responses to question 1, regarding residents' preparation to recognize their own emotions, showed no significant change after the simulation.
Discussion
The results indicate that formal training with an experiential communications course increased pediatrics residents' perceived preparedness to manage discriminatory comments in clinical encounters. All postcourse respondents reported being at least moderately prepared to engage in a respectful yet firm dialogue in response to discriminatory comments and to coach a junior trainee through the experience, including providing constructive feedback. Residents reported being moderately to well prepared to recognize their own emotions before and after the course, which may reflect their reported prior exposure to this type of discrimination.
The majority of respondents reported either directly being the target of discriminatory comments or witnessing such comments directed toward others. The high rate of exposure to prejudice from patients or their families underscores the value of training that acknowledges the pervasiveness of these encounters and prepares residents to navigate them. Such efforts support a diverse and inclusive workforce and enhance physician well-being. Residents who feel prepared to confront discriminatory comments are less likely to avoid these critical interactions.
Curricula to teach communication skills have been used in training programs to foster effective physician-patient/parent interactions.9,10 Programs that use role playing with simulated parents to help residents develop skills to navigate difficult encounters, such as giving bad news, have been shown to increase perceived self-efficacy and performance on objective evaluations.9–12
A simulation-based communications course similar to the one described here could be implemented in other training settings. Key elements enabling the success of simulation-based training include access to qualified, simulated parents; faculty preparation and participation; and dedicated resident time.
Resident satisfaction with the course was not measured directly. During the group debriefing exercise after completion of the course, residents generally reported that the experience was emotionally challenging yet helpful in preparing them for real-world experiences. Residents actively participated in identifying other scenarios to test these skills. For example, several residents requested simulation practice in responding to discriminatory comments directed toward themselves.
The generalizability of this study is limited by participation of a small number of residents from a single residency program. In addition, the response rate to the postcourse survey was approximately 50%, and the survey had no supporting validity evidence; thus, residents may not have interpreted questions as intended. The survey may have also been limited by response bias. Finally, we measured self-reported improvements and did not gather more objective measures of residents' communications skills.
Further research should examine the durability of effects of this intervention beyond the immediate postsimulation period and assess residents' abilities to respond to discriminatory comments with actual patients and families. This may prove challenging due to the random occurrence of such events.
Conclusion
Pediatrics residents reported a high prevalence of encountering discriminatory comments from patients and families and limited preparation to navigate these encounters. Residents reported increased perceived readiness to address discriminatory comments and generally found the experience to be emotionally challenging yet useful.
Supplementary Material
References
- 1. Accreditation Council for Graduate Medical Education. Non-discrimination policy. http://www.acgme.org/About-Us/Legal/Non-Discrimination-Policy. Accessed April 12, 2018.
- 2. Fnais N., Soobiah C., Chen MH., et al. Harassment and discrimination in medical training: a systematic review and meta-analysis. Acad Med. 2014; 89 5: 817– 827. [DOI] [PubMed] [Google Scholar]
- 3. Cook DJ., Liutkus JF., Risdon CL., et al. Residents' experiences of abuse, discrimination, and sexual harassment during residency training. CMAJ. 1996; 154 11: 1657– 1665. [PMC free article] [PubMed] [Google Scholar]
- 4. Baldwin DC, Jr,, Daugherty SR., Rowley BD. Racial and ethnic discrimination during residency: results of a national survey. Acad Med. 1994; 69 suppl 10: 19– 21. [DOI] [PubMed] [Google Scholar]
- 5. Reynolds KL., Cowden JD., Brosco JP., et al. When a family requests a white doctor. Pediatrics. 2015; 136 2: 381– 386. [DOI] [PubMed] [Google Scholar]
- 6. Committee on Pediatric Workforce. Enhancing pediatric workforce diversity and providing culturally effective pediatric care: implications for practice, education and policy making. Pediatrics. 2013; 132 4: e1105– e1116. [DOI] [PubMed] [Google Scholar]
- 7. Mendoza FS., Walker LR., Stoll BJ., et al. Diversity and inclusion training in pediatric departments. Pediatrics. 2015; 135 4: 707– 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whitgob EE., Blankenburg RL., Bogetz AL. The discriminatory patient and family: strategies to address discrimination towards trainees. Acad Med. 2016; 91 suppl 11: 64– 69. [DOI] [PubMed] [Google Scholar]
- 9. Peterson EB., Bolan KA., Bryant KA., et al. Development of a comprehensive communication skills curriculum for pediatric residents. J Grad Med Educ. 2016; 8 5: 739– 746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith S., Hanson JL., Tewksbury LR., et al. Teaching patient communication skills to medical students: a review of randomized controlled trials. Eval Health Prof. 2007; 30 1: 3– 21. [DOI] [PubMed] [Google Scholar]
- 11. Nikendei C., Bosse HM., Hoffmann K., et al. Outcome of parent-physician communication skills training for pediatric residents. Patient Educ Couns. 2011; 82 1: 94– 99. [DOI] [PubMed] [Google Scholar]
- 12. Gough JK., Frydenberg AR., Donath SK., et al. Simulated parents: developing paediatric trainees' skills in giving bad news. J Paediatr Child Health. 2009; 45 3: 133– 138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.