ABSTRACT
Background
Geriatrics training is essential for future primary care providers. The Extension for Community Healthcare Outcomes (ECHO) model improves access to specialty care via case-based videoconferencing, but Project ECHO has not previously been designed to target residents.
Objective
We designed Project ECHO-Geriatrics to deliver geriatrics education to primary care trainees using the ECHO model and evaluated self-rated geriatrics competency of trainees from the University of Washington Family Medicine Residency Network programs who participated between January 2016 and March 2017.
Methods
We assessed outcomes of Project ECHO-Geriatrics through anonymous surveys. Participants rated didactics, case discussions, and geriatrics-specific knowledge before and after sessions on a 5-point scale (1, low, to 5, high). Participants were asked whether they planned to do anything differently in their practice and, if yes, to describe this change.
Results
Fifteen sessions were held with 204 unique participants from 12 sites, with an average of 28 (range, 13–41) participants per session. From the 9 of 29 (31%) Family Medicine Residency Network programs that enrolled, 63% percent (116 of 184) of eligible residents attended. Sessions were highly rated (89% of responses were 4 or 5). Self-reported geriatrics-specific knowledge increased significantly (before 3.3 [SD = 0.89] versus after 4.0 [SD = 0.60], P < .001). Sixty-five percent (118 of 181) of participants reported plans to change their practice.
Conclusions
Project ECHO-Geriatrics is an innovative, feasible way to train the future primary care workforce in geriatrics and grow the capacity to provide high-quality care to older adults.
What was known and gap
Geriatrics training is important in primary care. The Extension for Community Healthcare Outcomes (ECHO) video consultation model is an effective approach, but no ECHO program has been designed specifically for residents.
What is new
An educational innovation used case-based videoconference sessions to teach geriatrics topics to family medicine residents in 9 programs that are part of a regional residency network.
Limitations
Outcomes were limited to self-reported knowledge gains and plans for change.
Bottom line
The videoconferences are an innovative and feasible way to enhance geriatrics training in family medicine residents.
Introduction
The primary care workforce for the rapidly growing population of older adults cannot be derived solely from the dwindling numbers of board-certified geriatricians.1–5 Integrating geriatrics telementoring and telehealth into primary care training may mitigate the scarcity of geriatricians and support trainees and clinicians who are caring for medically complex older adults in underserved communities.
The Extension for Community Healthcare Outcomes (ECHO) model provides education, mentoring, and consultation through videoconferencing with primary care clinicians.6–9 Outcomes for rural patients with complex diseases such as hepatitis C have been improved via ECHO.8,10–13 Several geriatrics-related ECHOs throughout the country have improved patient outcomes such as avoiding rehospitalization or alleviating dementia-related behavioral problems in older adults.14,15 Other interventions using the ECHO model have successfully included trainees, but we know of none that was specifically created for resident physicians.15–19 There may be an advantage to training resident physicians with the ECHO model before they enter practice.
We launched Project ECHO-Geriatrics as part of the Northwest Geriatrics Workforce Enhancement Center (NWGWEC). The NWGWEC is funded through the Health Resources and Services Administration Geriatrics Workforce Enhancement Program, an initiative to improve primary care of older adults.20
Methods
Program Description
Project ECHO-Geriatrics consists of monthly, interactive videoconferencing sessions that connect attendees to a University of Washington (UW) interdisciplinary geriatrics specialist panel and to each other. The panel includes fellowship-trained geriatricians, a geriatric pharmacist, a geriatric psychiatrist, a clinical social worker, and NWGWEC partners at 2 Area Agencies on Aging21 (1 urban and 1 rural). Attributes that distinguish Project ECHO-Geriatrics from many other uses of the ECHO model include monthly (rather than weekly) sessions, a target audience of primary care trainees, and presence of community partners on the panel. Finally, instead of focusing on a single disease/condition, it covers the breadth of issues relevant to older adults in primary care.
We partnered with the UW Family Medicine Residency Network (FMRN), which includes 29 residency programs across the Washington, Wyoming, Alaska, Montana, and Idaho region. A needs assessment of the programs in the UW FMRN was performed, and invitations were extended. Meeting with our ECHO information technology (IT) specialist was required prior to a site's participation. Each site had a champion who assisted with attendance and evaluations.
Sessions included a 15-minute primary care–focused geriatrics didactic,22 followed by 45 minutes of case consultations and discussion. Attendees volunteered to present deidentified cases. The expert panel and participants suggested management plans. Reminders to participants were sent 1 to 2 weeks before the session. Cases were not required to match the didactic topic. Session attendance was optional at most sites, and some sites included only residents on geriatrics rotations. After sessions, case presenters received written summaries of panel recommendations. Attendees were sent a link to resources discussed during the session (eg, evidence-based articles, community-based resources).
Program Evaluation
Attendance was tracked, and outcomes were assessed through anonymous print and electronic surveys participants completed after each session (provided as online supplemental material). Attendees rated their satisfaction with different aspects of the ECHO sessions, including the didactic, presenter, technology, and case discussion, as well as their self-assessed pre- and postsession knowledge of the didactic topic on a 5-point scale (1, low, to 5, high). Attendees were also asked whether they planned to change their clinical practice and, if yes, to describe the change. Several items probed for future topics and other comments. The project coordinator coded the case presentations to capture the content of the discussion. The codebook included geriatric topics central to primary care (eg, functional assessment, medication management). Case characteristics were obtained from deidentified case forms.
The UW Institutional Review Board (IRB) Worksheet for Human Subjects Research indicated that IRB review was not required.
Data Analysis
Descriptive statistics were used to summarize attendance, survey responses, and case forms. A Wilcoxon signed rank test was performed to assess differences between knowledge before and after sessions. Case presentations were coded using preset codes in a hybrid codebook that was open so we could add codes that emerged over time.23,24
Results
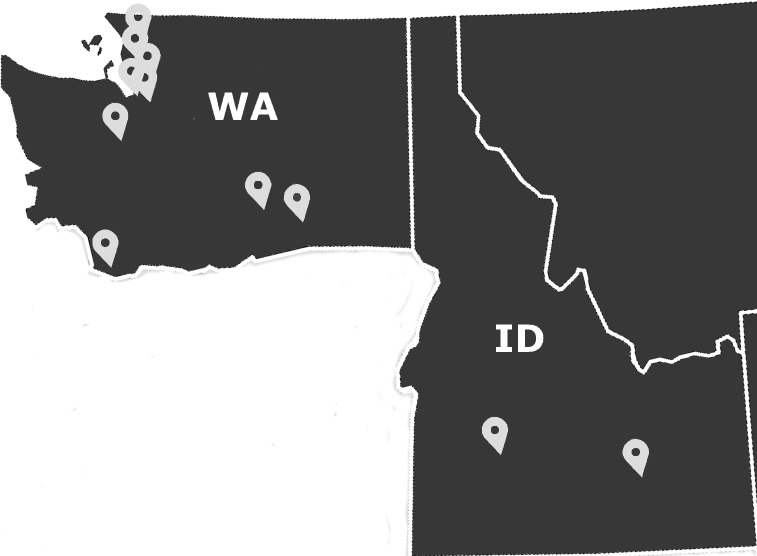
Between January 2016 and March 2017, 15 Project ECHO-Geriatrics sessions were held with 204 unique participants from 12 sites across Washington and Idaho (Figure 1), with an average of 28 (range, 13–41) participants per session. Attendees joined an average of 2.7 (SD = 1.84) sessions, and 54% (110 of 204) attended more than once. Nine sites were FMRN programs, while others included training programs at UW and practicing providers. From the 9 of 29 (31%) FMRN programs that enrolled, 63% (116 of 184) of eligible family medicine residents attended. The majority of participants were resident physicians (57%, 116 of 204); other attendees included faculty (14%, 29 of 204), other health professionals (fellows, practicing physicians, physician assistants, pharmacists; 11%, 22 of 204), medical students (10%, 20 of 204), and nurses (8%, 16 of 204).
Figure 1.
Map of Participating Project Extension for Community Healthcare Outcomes (ECHO)–Geriatrics Sites in Washington and Idaho
Evaluations were completed by 181 attendees (89%). The vast majority (> 85%) of respondents rated each aspect of the ECHO sessions highly (ie, in the 4–5 range). Self-reported geriatrics knowledge increased significantly (before sessions, 3.3 [SD = 0.89]; after sessions, 4.0 [SD = 0.60]; P < .001). Of the respondents, 65% (118 of 181) planned to change their practice as a result of the sessions. Furthermore, 59% of attendees (107 of 181) described what they planned to change in their practice (provided as online supplemental material), such as “offer better resources to caregivers,” “discuss shared goals with patients, and not go by risk score by itself,” and “check and recheck medication list for side effects and Beers criteria (medications to avoid in older adults).”25
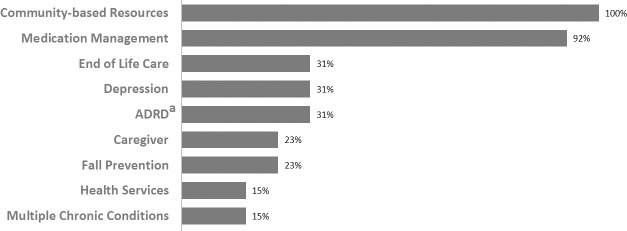
Nineteen cases were presented (by 10 residents, 4 geriatrics fellows, and 3 others; 2 residents presented twice) with the following patient characteristics: 74% (14 of 19) women, 63% (12 of 19) 80+ years old, 47% (9 of 19) with dementia, 47% (9 of 19) with 8 or more chronic conditions, 42% (8 of 19) with 10 or more medications, and 37% (7 of 19) skilled nursing facility residents. Almost every case discussion included themes around medication management and review of community-based resources (Figure 2).
Figure 2.
Percentages of Most Common Themes Among 13 Qualitatively Coded Case Presentations and Discussions
a ADRD, Alzheimer's disease and related dementias.
Discussion
This is the first time the ECHO model has been applied specifically to train resident physicians in the full breadth of geriatrics primary care. Project ECHO-Geriatrics was well-received, and we demonstrated that the ECHO model can improve self-reported geriatrics knowledge of primary care trainees. Project ECHO-Geriatrics demonstrates that the telementoring relationship in the ECHO model may be readily extended to medical residents and other health professions trainees.
Challenges faced included involving sites outside our time zone, actively engaging participants in classrooms of 15 or more trainees, and encouraging participants to submit and present cases. We utilized polling and more direct questioning of the group during sessions as tools to address engagement. Case submissions increased when sites were asked to sign up in advance or by directly e-mailing champions at sites that had not recently presented.
The cost to implement a similar program may vary, depending on local resources and session frequency. Our institution is an ECHO hub; this provided use of a videoconferencing room along with access to experienced IT personnel, well-documented best practices for start-up and coordination, and ongoing mentorship. Salary expenses included time for a medical director, project coordinator, and IT specialist. Project ECHO offers substantial training and resources for new ECHO sites (https://echo.unm.edu). Other costs included a distribution list management program and videoconferencing license.
Limitations of this educational innovation include the use of self-reported survey data, which did not allow us to determine which aspect of ECHO improved self-reported knowledge or planned practice change. Survey data were subject to both nonresponse and response bias, and our sample size was small.
Future plans for the program include recruiting more sites and participants, continuing to innovate ways to incentivize case presentations, and more rigorously evaluating program impact on practice. This project is ongoing, with enthusiastic participation of a growing number of sites, but it will require support for geriatrics-trained faculty and program support personnel to be sustained.
Conclusion
Project ECHO-Geriatrics is an innovative, feasible strategy to provide geriatrics education and consultation for future primary care providers across a geographic region and expand the capacity to provide high-quality care to the rapidly growing older adult population.
Supplementary Material
References
- 1. Callahan KE., Tumosa N., Leipzig RM. Big “G” and little “g” geriatrics education for physicians. J Am Geriatr Soc. 2017; 65 10: 2313– 2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Leipzig RM., Hall WJ., Fried LP. Treating our societal scotoma: the case for investing in geriatrics, our nation's future, and our patients. Ann Intern Med. 2012; 156 9: 657. [DOI] [PubMed] [Google Scholar]
- 3. Hazzard WR. General internal medicine and geriatrics: collaboration to address the aging imperative can't wait. Ann Intern Med. 2003; 139 7: 597– 598. [DOI] [PubMed] [Google Scholar]
- 4. Administration on Aging; Administration for Community Living; US Department of Health and Human Services. A Profile of Older Americans: 2016. https://www.acl.gov/sites/default/files/Aging and Disability in America/2016-Profile.pdf. Accessed April 9, 2018.
- 5. National Academies of Sciences. Retooling for an Aging America: Building the Health Care Workforce. 2008. http://www.nationalacademies.org/hmd/reports/2008/retooling-for-an-aging-america-building-the-health-care-workforce.aspx. Accessed April 9, 2018. [PubMed]
- 6. Arora S., Kalishman S., Dion D., et al. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff. 2011; 30 6: 1176– 1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arora S., Thornton K., Komaromy M., et al. Demonopolizing medical knowledge. Acad Med. 2014; 89 1: 30– 32. [DOI] [PubMed] [Google Scholar]
- 8. Arora S., Thornton K., Jenkusky SM., et al. Project ECHO: linking university specialists with rural and prison-based clinicians to improve care for people with chronic hepatitis C in New Mexico. Public Health Rep. 2007; 122 suppl 2: 74– 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arora S., Kalishman S., Thornton K., et al. Project ECHO (Project Extension for Community Healthcare Outcomes): a national and global model for continuing professional development. J Contin Educ Health Prof. 2016; 36 suppl 1: 48– 49. [DOI] [PubMed] [Google Scholar]
- 10. Arora S., Kalishman S., Thornton K., et al. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010; 52 3: 1124– 1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scott JD., Unruh KT., Catlin MC., et al. Project ECHO: a model for complex, chronic care in the Pacific Northwest region of the United States. J Telemed Telecare. 2012; 18 8: 481– 484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katzman JG., Galloway K., Olivas C., et al. Expanding health care access through education: dissemination and implementation of the ECHO Model. Mil Med. 2016; 181 3: 227– 235. [DOI] [PubMed] [Google Scholar]
- 13. Wood BR., Unruh KT., Martinez-Paz N., et al. Impact of a telehealth program that delivers remote consultation and longitudinal mentorship to community HIV providers. Open Forum Infect Dis. 2016; 3(3):ofw123. [DOI] [PMC free article] [PubMed]
- 14. Catic AG., Mattison MLP., Bakaev I., et al. ECHO-AGE: an innovative model of geriatric care for long-term care residents with dementia and behavioral issues. J Am Med Dir Assoc. 2014; 15 12: 938– 942. [DOI] [PubMed] [Google Scholar]
- 15. Vanka A., Farris G., Bortinger J., et al. Mind the gap: a novel care transitions curriculum for hospitalists and residents. J Grad Med Educ. 2015; 7 2: 277– 278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Knight P., Bonney A., Teuss G., et al. Positive clinical outcomes are synergistic with positive educational outcomes when using telehealth consulting in general practice: a mixed-methods study. J Med Internet Res. 2016; 18 2: e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mazzuoccolo LD., Marciano S., Echeverría CM. Implementation of a telementoring model of medical education in psoriasis. Medicina (B Aires). 2016; 76 6: 359– 361. [PubMed] [Google Scholar]
- 18. Sunderji N., Crawford A., Jovanovic M. Telepsychiatry in graduate medical education: a narrative review. Acad Psychiatry. 2015; 39 1: 55– 62. [DOI] [PubMed] [Google Scholar]
- 19. Sanders D., Welk DS. Strategies to scaffold student learning: applying Vygotsky's Zone of Proximal Development. Nurse Educ. 2005; 30 5: 203– 207. [DOI] [PubMed] [Google Scholar]
- 20. Busby-Whitehead J., Flaherty E., Potter J. The Geriatrics Workforce Enhancement Program: a major eldercare initiative. J Am Soc Aging. 2016; 40 1: 122– 125. [Google Scholar]
- 21. Administration for Community Living. Area Agencies on Aging. https://www.acl.gov/programs/aging-and-disability-networks/area-agencies-aging. Accessed April 9, 2018.
- 22. Northwest Geriatrics Workforce Enhancement Center. Project ECHO-Geriatrics Archived Didactics. http://www.nwgwec.org/activities/project-echo-geriatrics/#didactics. Accessed April 9, 2018.
- 23. Moustakas C. Phenomenological Research Methods. Thousand Oaks, CA: SAGE Publications; 1994. [Google Scholar]
- 24. Murray M., Chamberlain K. Qualitative Health Psychology: Theories and Methods. Thousand Oaks, CA: SAGE Publications; 1999. [Google Scholar]
- 25. Samuel MJ. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015; 63 11: 2227– 2246. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.