ABSTRACT
Background
Clinicians are increasingly sharing outpatient visit notes with patients through electronic portals. These open notes may bring about new educational opportunities as well as concerns to physicians-in-training and residency programs.
Objective
We assessed anticipatory attitudes about open notes and explored factors influencing residents' propensity toward note transparency.
Methods
Residents in primary care clinics at 4 teaching hospitals were surveyed prior to implementation of open notes. Main measures included resident attitudes toward open notes and the anticipated effect on patients, resident workload, and education. Data were stratified by site.
Results
A total of 176 of 418 (42%) residents responded. Most residents indicated open notes would improve patient engagement, trust, and education but worried about overwhelming patients, residents being less candid, and workload. More than half of residents thought open notes were a good idea, and 32% (56 of 176) indicated they would encourage patients to read these notes. More than half wanted note-writing education and more feedback, and 72% (126 of 175) indicated patient feedback on residents' notes could improve communication skills. Attitudes about effects of open notes on safety, quality, trust, and medical education varied by site.
Conclusions
Residents reported mixed feelings about the anticipated effects of sharing clinical notes with patients. They advocate for patient feedback on notes, yet worry about workload, supervision, and errors. Training site was correlated with many attitudes, suggesting local culture drives resident support for open notes. Strategies that address resident concerns and promote teaching and feedback related to notes may be helpful.
What was known and gap
The OpenNotes demonstration project detailed patient benefits to reading their clinicians' notes, although residents were not included in earlier survey studies.
What is new
Residents at 4 US training programs were surveyed prior to implementation of open notes about anticipated effects on their patients, workload, and education.
Limitations
Three of the 4 sites had faculty members who previously participated in the OpenNotes demonstration project (potentially influencing resident attitudes), and the resident survey response rate was 42%.
Bottom line
Residents received infrequent feedback on notes and identified benefits to patients and their education, which were tempered by concerns about workload.
Introduction
Following the year-long OpenNotes demonstration project, in which more than 100 primary care physicians invited 20 000 of their patients to read their clinical notes, health care organizations are increasingly making notes available to patients through electronic portals.1–3 To date, little is known about how these open notes will affect residents and their patients. Although younger physicians generally have more favorable attitudes about technology and transparency, a prior study found residents, when compared with faculty, were 30% less likely to support sharing medical records with patients.4 Additionally, trainees have detailed several note-transparency concerns in focus groups.5 For physicians-in-training, clinical notes serve as medical education tools,6 supporting information synthesis and faculty assessment and feedback.7–10 Because clinical notes are more than just documentation for learners, sharing these notes with patients may have unanticipated effects on learners and their practice.
Clinical note-writing is a nuanced skill that has important implications for patients, insurers, and medicolegal considerations, yet it is seldom taught and often is poorly supervised during residency.11 Residents receive little formal training on how to document sensitive issues, and primarily learn “on the job.” Electronic health records add challenges to effective note-writing with issues including “note bloat” from imported data and “copy forward” of prior notes, which may undermine clarity and accuracy.12–14 Residents and their preceptors face formidable time pressures, and meaningful feedback about notes often is lacking.15,16
As residency programs prioritize teaching transparency and patient engagement, open notes may offer unique educational opportunities.17 Conversely, inviting patients to read resident notes may have negative consequences on patients, residents, and their relationships. As open notes spread nationally, we sought to understand residents' perceptions of anticipated risks and benefits to their patients and to themselves, in terms of workload and education. We anticipated that a better understanding of these issues could help inform residency programs in the transparency era.
Methods
Study Design, Setting, and Participants
We conducted a cross-sectional survey of resident physicians at Beth Israel Deaconess Medical Center, Geisinger Health System, Harborview Medical Center, and the University of Colorado. Faculty at 3 of the 4 sites previously participated in the OpenNotes demonstration project.1 Residents in internal medicine participated at all 4 sites, and residents from family medicine participated at 2 sites with training programs (Geisinger Health System and University of Colorado).
Each participating program planned to implement open notes, with resident ambulatory notes available to patients by default through an electronic portal once signed by the resident and the faculty preceptor, unless the note was specifically withheld.
Surveys were conducted between April 2013 and March 2014. Residents did not have any personal experience with open notes and were surveyed prior to their department launching open notes.
This project was approved by the Institutional Review Board at each institution.
Survey Design
A survey (provided as online supplemental material) was designed collaboratively by researchers with experience in patient engagement, medical education, health care delivery, and quality and safety. Items paralleled the original OpenNotes study survey,18 with added sections addressing education. The majority of questions used a 4-point Likert scale (eg, strongly agree, agree, disagree, strongly disagree) without a neutral option as in the original OpenNotes survey.18 The survey was modified for individual site terminology.
Recruitment
After program directors sent residents an e-mail introducing open notes and announcing the survey, residents received an e-mail from the study team containing a link to the survey. Nonresponders received 3 reminders. A nominal raffle prize was used at each site to incentivize participation.
Statistical Analysis
We used descriptive statistics to report results, dichotomizing responses into agree/disagree and concerned/not concerned. We compared responses among sites using the chi-square test. We excluded a small number of surveys (n = 5) with substantial missing data. To explore factors associated with actively encouraging patients to read their notes, we analyzed personal characteristics, residency program features, time management, and error concerns. A detailed description of our exploratory model is provided as online supplemental material.
Results
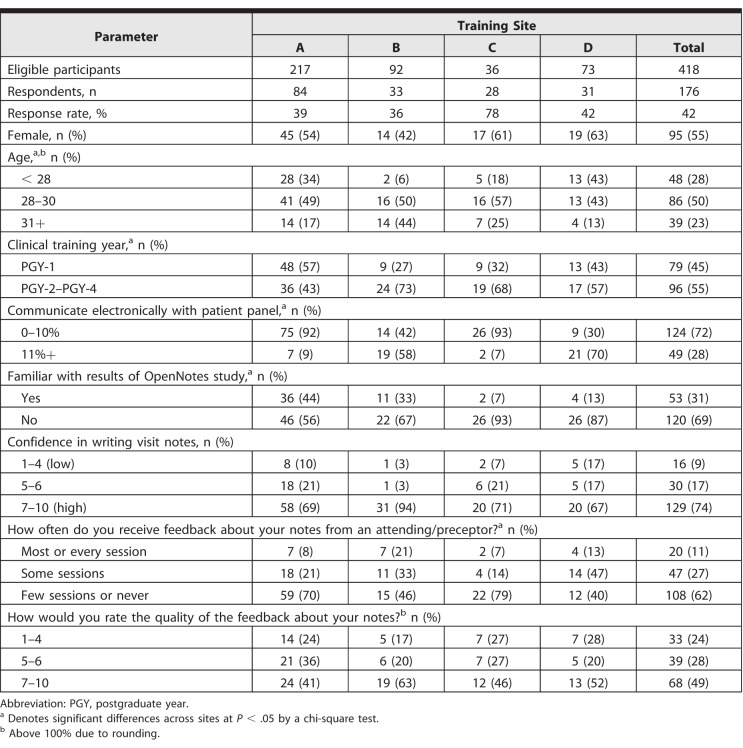
Across the 4 institutions, 418 residents were eligible and invited to participate; 176 responded and were included in the analysis (42% response rate). Table 1 describes resident characteristics by training site.
Table 1.
Demographics and Resident Characteristics by Training Site
Anticipated Effects on Resident Practice and Workload
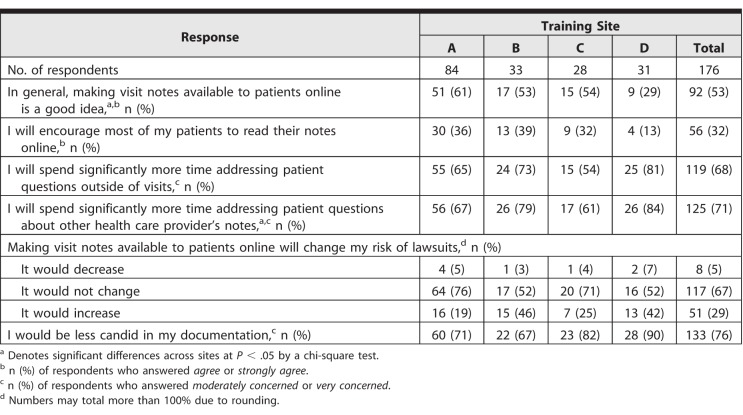
Slightly more than half of residents (53%, 92 of 175) thought open notes were a good idea (Table 2), and 32% (56 of 176) indicated they would encourage patients to read their notes online, while 68% (119 of 176) had concerns they would spend more time addressing patient questions about their notes outside of visits, including fielding patient questions about notes from other providers. Seventy-six percent of residents (133 of 176) reported they would be less candid if their notes were “open.”
Table 2.
Impact of Open Notes on Residents and Their Practice
Anticipated Effects on Patients
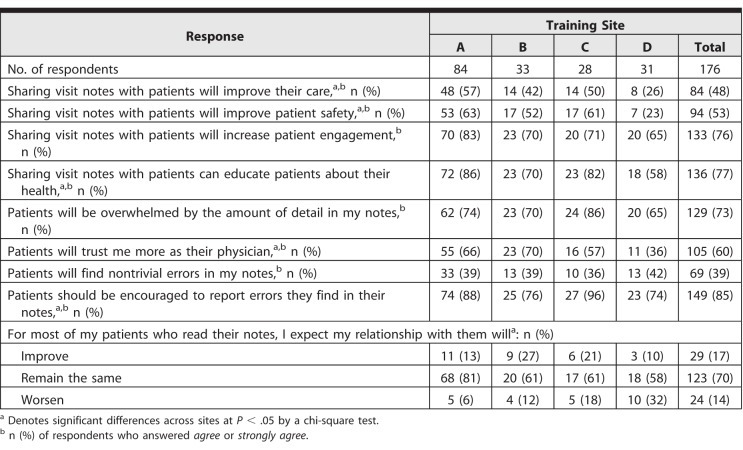
The majority of residents (76%, 133 of 176) agreed open notes would promote patient engagement and educate patients about their health, and approximately half thought that notes would improve care and patient safety (Table 3). However, 73% (129 of 176) worried patients would be overwhelmed by the amount of detail in their notes, 39% (69 of 176) thought patients might find nontrivial errors in their notes, and 85% (149 of 176) indicated patients should be encouraged to report errors. Sixty percent (105 of 176) indicated patients would trust them more as their physician because of sharing notes.
Table 3.
Anticipated Impact of Open Notes on Residents' Patients
Anticipated Effects on Education
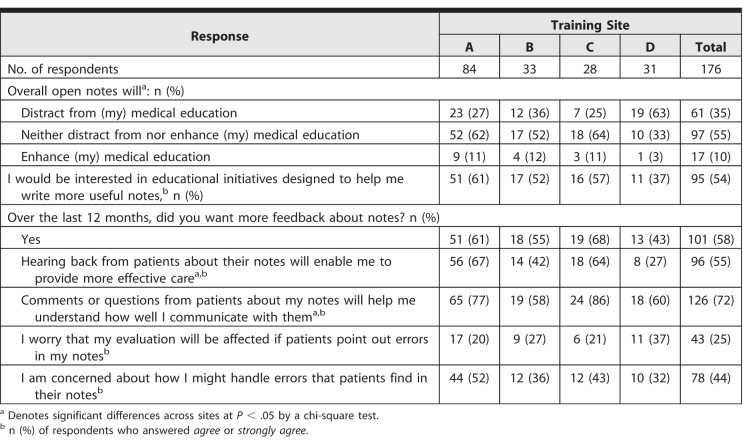
Overall, 62% of residents (108 of 175) reported they received limited faculty feedback on their notes, and 24% (33 of 140) rated the quality of feedback as a 4 or less on a scale from 1 to 10 (Table 4). Most residents were interested in educational interventions to help them write more useful notes and wanted more feedback from faculty on their notes. In addition, 72% of residents (126 of 175) agreed patient feedback on their notes might help them assess their communication with patients, and 55% (96 of 175) thought patient feedback would help them provide more effective care.
Table 4.
Open Notes and Medical Education
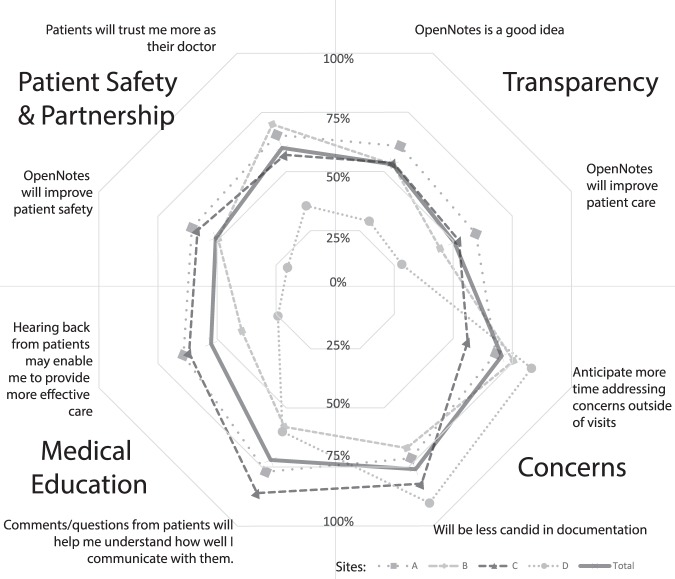
Beyond these overall expectations, Tables 1 to 4 show differences in resident responses across most survey items by site, and the Figure illustrates resident responses by site for 8 representative questions.
Figure.
Representative Survey Questions (% of Respondents in Agreement With Statement), Grouped According To Domain
Note: Responses are stratified by site. Solid line denotes aggregate of all 4 sites.
Factors Influencing Residents' Propensity Toward Open Notes
In an exploratory analysis examining factors associated with residents' willingness to encourage patients to read notes, we found no significant differences by age, sex, training year, familiarity with the OpenNotes demonstration study results, confidence in note-writing, or frequency/quality of note feedback from faculty (provided as online supplemental material). We observed that residents who agreed that patients would find errors in notes were more likely to encourage patients to read notes.
Discussion
In this study of internal medicine and family medicine residents at 4 US academic medical centers, respondents saw unique and innovative opportunities for medical education and patient engagement with open notes. They also reported concerns about time pressures, candid documentation, errors, and overwhelming patients with information. Prior to implementation of open notes, respondents were divided about whether sharing notes with patients was a good idea. Our study suggested that thoughtful approaches to open notes, coupled with greater resident support, may yield new educational innovations. Our findings also highlighted 3 areas for medical educators to consider: (1) the need for increased mentorship and feedback on notes; (2) the influence of faculty role-modeling on residents; and (3) the opportunity to help learners prepare for a future of transparency in medicine.
Residents Need More Real-Time Feedback on Note-Writing
Similar to other studies,19,20 our findings confirmed residents rarely received consistent feedback from faculty preceptors on their notes, and most desired more feedback and specific educational initiatives to improve note-writing. Sharing notes with patients may highlight these deficiencies, and motivate faculty to provide more supervision. This highlights an opportunity to revamp resident education about note-writing and patient engagement. The majority of residents reported patient feedback would help them assess their listening and communication skills, offering an innovative approach to teach patient engagement through patient-centered education, touted by experts as the “next revolution in medical education.”17,21
Faculty Attitudes and Local Culture Shape Resident Perspectives
Our findings suggest resident perspectives toward open notes may be influenced by faculty attitudes. Our data show that resident attitudes varied by site, and local institutional culture shaped by the faculty may account for these differences. Since negative role models may have an unintended impact, creating highly visible, positive role models and leaders committed to transparency may help engage residents in open notes.22
Despite the concerns raised by this study, residents appear to be at least as accepting of open notes as their faculty counterparts. In our study, 58% of residents at the original study sites supported open notes as a good idea compared to 61% to 80% of faculty primary care physicians who volunteered to participate at these sites in the original OpenNotes study.18 The majority of primary care physicians declined participation in the original OpenNotes study, and among these, only 16% to 33% supported open notes as a good idea. Considering that participation was mandatory for residents in their clinical practice, their attitudes may be more receptive of transparent notes overall than faculty perspectives. This finding can be explained by generational differences toward transparency and information sharing. However, we also observed strong attitudes about issues that are more specific to residents, such as responding to queries about other providers' notes and being less candid, which are issues requiring organizational attention.
The majority of residents in our study were not familiar with the original OpenNotes study, which showed patient benefits and abatement of physician concerns after implementation.23,24 Sharing these results and data about unchanged e-mail traffic, safety opportunities, and enhanced patient-physician relationships may help offset residents' anticipatory concerns.25–29
Preparing Residents for a Future of Transparency in Medicine
As health information transparency spreads, now with more than 20 million patients able to access notes across the United States,30 medical educators have a duty to help learners develop skills for transparency in medicine. Although patients have had the legal right to access their records since 1996, recent emphasis on transparency and patient engagement has accelerated the need for residents to develop competencies in this area.31 Developing skills for educating and engaging patients in their care strengthens core competencies focused on patient-centered care, and will serve residents well beyond graduation.
Educators can leverage open notes to promote patient safety through transparency, as advocated by national experts.32 This approach may provide a “win-win” for programs, directly responding to 1 of our study's findings: residents' support for patients reporting note errors and providing opportunities to improve record accuracy. Emphasizing safety, educators can help reduce copy/paste behaviors and propagation of erroneous information in notes.33,34 We were intrigued that residents who agreed that patients would find errors in their notes were more likely to encourage patients to read notes, suggesting some residents may already connect the dots of transparency and safety.35,36
Limitations of this study include a response rate of less than 50%, with the potential that residents with strong attitudes for or against open notes were more likely to respond. In addition, objections to open notes may reflect more global resistance to new initiatives by overwhelmed residents rather than objections to open notes.37 While we retained many of the same questions as in the original OpenNotes survey (which was tested extensively), we did not pretest the instrument with residents, and respondents may not have interpreted questions as intended. We surveyed internal medicine and family medicine residents at 4 programs with diverse characteristics and patient populations, yet results may not generalize to all programs. Finally, resident attitudes are anticipatory and do not reflect actual experience with open notes. A follow-up study after implementation of open notes is needed to determine whether anticipatory concerns and unique opportunities materialize.
Conclusion
Residents at 4 US institutions reported mixed attitudes about the anticipated effects of open clinical notes. Prior to actually sharing notes with patients, some residents perceived open notes would enhance patient education, engagement, and trust and offer unique opportunities in their own education, while residents also worried about personal workload and overwhelming patients. Most residents reported low frequency and quality of preceptor feedback on their notes. While some resident attitudes mirror faculty physician experiences, unique resident concerns merit focused attention and further research.
Supplementary Material
References
- 1. Delbanco T., Walker J., Darer JD., et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010; 153 2: 121– 125. [DOI] [PubMed] [Google Scholar]
- 2. Walker J., Darer JD., Elmore JG., et al. The road toward fully transparent medical records. N Engl J Med. 2014; 370 1: 6– 8. [DOI] [PubMed] [Google Scholar]
- 3. Ross SE., Lin CT. The effects of promoting patient access to medical records: a review [ published correction in J Am Med Inform Assoc. 2003; 10 3: 294]. J Am Med Inform Assoc. 2003; 10 2: 129– 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Keplinger LE., Koopman RJ., Mehr DR., et al. Patient portal implementation: resident and attending physician attitudes. Fam Med. 2013; 45 5: 335– 340. [PMC free article] [PubMed] [Google Scholar]
- 5. Crotty BH., Anselmo M., Clarke DN., et al. Opening residents' notes to patients: a two-institution qualitative study of resident and faculty physician attitudes on open notes implementation in graduate medical education. Acad Med. 2016; 91 3: 418– 426. [DOI] [PubMed] [Google Scholar]
- 6. Yanoff KL., Burg FD. Types of medical writing and teaching of writing in US medical schools. J Med Educ. 1988; 63 1: 30– 37. [DOI] [PubMed] [Google Scholar]
- 7. Reddy ST., Endo J., Gupta S., et al. A case for caution: chart-stimulated recall. J Grad Med Educ. 2015; 7 4: 531– 535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schipper S., Ross S. Structured teaching and assessment: a new chart-stimulated recall worksheet for family medicine residents [in English and French]. Can Fam Physician. 2010; 56 9: 958– 959, e352–e954. [PMC free article] [PubMed] [Google Scholar]
- 9. Swing SR., Clyman SG., Holmboe ES., et al. Advancing resident assessment in graduate medical education. J Grad Med Educ. 2009; 1 2: 278– 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shaughnessy AF., Chang KT., Sparks J., et al. Assessing and documenting the cognitive performance of family medicine residents practicing outpatient medicine. J Grad Med Educ. 2014; 6 3: 526– 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Oxentenko AS., West CP., Popkave C., et al. Time spent on clinical documentation: a survey of internal medicine residents and program directors [ published correction appears in Arch Intern Med. 2010; 170 7: 639]. Arch Intern Med. 2010; 170 4: 377– 380. [DOI] [PubMed] [Google Scholar]
- 12. Embi PJ., Yackel TR., Logan JR., et al. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc. 2004; 11 4: 300– 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Atwater AR., Rudd M., Brown A., et al. Developing teaching strategies in the EHR era: a survey of GME experts. J Grad Med Educ. 2016; 8 4: 581– 586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fanucchi L., Yan D., Conigliaro RL. Duly noted: lessons from a two-site intervention to assess and improve the quality of clinical documentation in the electronic health record. Appl Clin Inform. 2016; 7 3: 653– 659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schum TR., Krippendorf RL., Biernat KA. Simple feedback notes enhance specificity of feedback to learners. Ambul Pediatr. 2003; 3 1: 9– 11. [DOI] [PubMed] [Google Scholar]
- 16. Kim D., Spellberg B. Does real-time feedback to residents with or without attendings improve medical documentation? Hosp Pract (1995). 2014; 42 3: 123– 130. [DOI] [PubMed] [Google Scholar]
- 17. Weinberger SE., Johnson BH., Ness DL. Patient- and family-centered medical education: the next revolution in medical education? Ann Intern Med. 2014; 161 1: 73– 75. [DOI] [PubMed] [Google Scholar]
- 18. Walker J., Leveille SG., Ngo L., et al. Inviting patients to read their doctors' notes: patients and doctors look ahead: patient and physician surveys [ published correction appears in Ann Intern Med. 2012; 157 1: 80]. Ann Intern Med. 2011; 155 12: 811– 819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Delva D., Sargeant J., Miller S., et al. Encouraging residents to seek feedback. Med Teach. 2013; 35 12: e1625– e1631. [DOI] [PubMed] [Google Scholar]
- 20. Reddy ST., Zegarek MH., Fromme HB., et al. Barriers and facilitators to effective feedback: a qualitative analysis of data from multispecialty resident focus groups. J Grad Med Educ. 2015; 7 2: 214– 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Weisser RJ, Jr,, Medio FJ. The patient as teacher. J Med Educ. 1985; 60 1: 63– 65. [DOI] [PubMed] [Google Scholar]
- 22. Martinez W., Hickson GB., Miller BM., et al. Role-modeling and medical error disclosure: a national survey of trainees. Acad Med. 2014; 89 3: 482– 489. [DOI] [PubMed] [Google Scholar]
- 23. Delbanco T., Walker J., Bell SK., et al. Inviting patients to read their doctors' notes: a quasi-experimental study and a look ahead [ published correction appears in Ann Intern Med. 2015; 162 7: 532]. Ann Intern Med. 2012; 157 7: 461– 470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hanauer DA., Preib R., Zheng K., et al. Patient-initiated electronic health record amendment requests. J Am Med Inform Assoc. 2014; 21 6: 992– 1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bell SK., Mejilla R., Anselmo M., et al. When doctors share visit notes with patients: a study of patient and doctor perceptions of documentation errors, safety opportunities and the patient-doctor relationship. BMJ Qual Saf. 2017; 26 4: 262– 270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nazi KM., Turvey CL., Klein DM., et al. VA OpenNotes: exploring the experiences of early patient adopters with access to clinical notes. J Am Med Inform Assoc. 2015; 22 2: 380– 389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. deBronkart D., Walker J. Open visit notes: a patient's perspective and expanding national experience. J Oncol Pract. 2015; 11 4: 287– 288. [DOI] [PubMed] [Google Scholar]
- 28. Wright E., Darer J., Tang X., et al. Sharing physician notes through an electronic portal is associated with improved medication adherence: quasi-experimental study. J Med Internet Res. 2015; 17 10: e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Klein JW., Jackson SL., Bell SK., et al. Your patient is now reading your note: opportunities, problems, and prospects. Am J Med. 2016; 129 10: 1018– 1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. OpenNotes Team. OpenNotes. https://www.opennotes.org. Accessed April 16, 2018.
- 31. Blumenthal D., Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010; 363 6: 501– 504. [DOI] [PubMed] [Google Scholar]
- 32. National Patient Safety Foundation's Lucian Leape Institute. Shining a Light: Safer Health Care Through Transparency. Boston, MA: National Patient Safety Foundation; 2015. [Google Scholar]
- 33. Holmboe ES., Prince L., Green M. Teaching and improving quality of care in a primary care internal medicine residency clinic. Acad Med. 2005; 80 6: 571– 577. [DOI] [PubMed] [Google Scholar]
- 34. Singh R., Naughton B., Taylor JS., et al. A comprehensive collaborative patient safety residency curriculum to address the ACGME core competencies. Med Educ. 2005; 39 12: 1195– 1204. [DOI] [PubMed] [Google Scholar]
- 35. Voss JD., May NB., Schorling JB., et al. Changing conversations: teaching safety and quality in residency training. Acad Med. 2008; 83 11: 1080– 1087. [DOI] [PubMed] [Google Scholar]
- 36. Wong BM., Etchells EE., Kuper A., et al. Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med. 2010; 85 9: 1425– 1439. [DOI] [PubMed] [Google Scholar]
- 37. Dyrbye LN., West CP., Satele D., et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014; 89 3: 443– 451. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.