Abstract
Purpose
This randomized trial compared outcomes of passive scattering proton therapy (PSPT) versus intensity-modulated (photon) radiotherapy (IMRT), both with concurrent chemotherapy, for inoperable non–small-cell lung cancer (NSCLC). We hypothesized that PSPT exposes less lung tissue to radiation than IMRT and thereby reduces toxicity without compromising tumor control. The primary end points were grade ≥ 3 radiation pneumonitis (RP) and local failure (LF).
Patients and Methods
Eligible patients had stage IIB to IIIB NSCLC (or stage IV NSCLC with a single brain metastasis or recurrent lung or mediastinal disease after surgery) who were candidates for concurrent chemoradiation therapy. Pairs of treatment plans for IMRT and PSPT were created for each patient. Patients were eligible for random assignment only if both plans satisfied the same prespecified dose-volume constraints for at-risk organs at the same tumor dose.
Results
Compared with IMRT (n = 92), PSPT (n = 57) exposed less lung tissue to doses of 5 to 10 Gy(RBE), which is the absorbed Gy dose multiplied by the relative biologic effectiveness (RBE) factor for protons; exposed more lung tissue to ≥ 20 Gy(RBE), but exposed less heart tissue at all dose levels between 5 and 80 Gy(RBE). The grade ≥ 3 RP rate for all patients was 8.1% (IMRT, 6.5%; PSPT, 10.5%); corresponding LF rates were 10.7% (all), 10.9% (IMRT), and 10.5% (PSPT). The posterior probability of IMRT being better than PSPT was 0.54. Exploratory analysis showed that the RP and LF rates at 12 months for patients enrolled before versus after the trial midpoint were 21.1% (before) versus 18.2% (after) for the IMRT group (P = .047) and 31.0% (before) versus 13.1% (after) for the PSPT group (P = .027).
Conclusion
PSPT did not improve dose-volume indices for lung but did for heart. No benefit was noted in RP or LF after PSPT. Improvements in both end points were observed over the course of the trial.
INTRODUCTION
The standard of care for locally advanced non–small-cell lung cancer (NSCLC) is concurrent chemoradiation therapy, which produces a median survival time of 28.7 months.1 Radiation-induced toxicity to normal tissue, particularly radiation pneumonitis (RP), negatively affects both survival and quality of life.1,2 We have previously shown that the development of RP depends on the radiation dose to a threshold volume of lung (Vdose)3,4 and that mean lung dose (MLD) is highly predictive of RP.4,5 Advances in the planning and delivery of photon (x-ray) radiation, such as intensity-modulated radiation therapy (IMRT), have reduced the incidences of RP by minimizing both the radiation dose and the volume of lung exposed relative to three-dimensional conformal techniques.2,6 Proton therapy can also reduce exposure of the lung (and presumably RP) because of the differences in physical characteristics of photons and protons; theoretically, protons allow higher, more-focused radiation doses to be delivered to the tumor with less exposure to the surrounding tissues. These presumptions have led some to conclude that the superiority of protons over photons is so obvious that randomized trials to compare protons with photons are unnecessary, inappropriate, or unethical.7-9
Proton therapy is more costly than the best available photon technology. Evidence that demonstrates the clinical benefit of proton therapy is in increasing demand to justify the financial burden on the health care system. However, randomized trials that compare outcomes between various treatment technologies are practically nonexistent. Trials of proton versus photon therapy are no exception. The benefit of proton versus photon therapy is typically assessed from treatment plan comparisons, with the validation of results coming from retrospective analyses of small single-institution studies, meta-analyses of multi-institutional studies, or reviews of large databases. Although randomized controlled trials are not the only mechanism for producing high-level evidence, they are traditionally considered the gold standard.10
We hypothesized that proton therapy exposes significantly less lung tissue to radiation than photon therapy, which thus reduces toxicity without compromising tumor control. We tested this hypothesis in a Bayesian trial in which patients underwent adaptive random assignment to IMRT or three-dimensional passive scattering proton therapy (PSPT) for inoperable NSCLC. Adaptive randomization uses real-time assessment of accumulated outcome data to efficiently detect differences between arms and thereby adjust the ratio of patient allocation (on the basis of ongoing assessment of the risk of treatment failure) so that more patients are allocated to the better treatment plan if a difference is observed; if no difference exists, the ratio would converge to the classical 1:1 allocation.7,9,11,12
PATIENTS AND METHODS
Study Design and Patient Eligibility and Enrollment
This trial compared the toxicity and effectiveness of PSPT with that of standard IMRT, both with concurrent chemotherapy, for patients with locally advanced NSCLC (Data Supplement). Patients were treated at The University of Texas MD Anderson Cancer Center or Massachusetts General Hospital. The protocol was approved by the institutional review boards of both institutions. All participants provided written informed consent.
Eligible patients were older than 18 years of age, had a Karnofsky performance score ≥ 70, stage II to IIIB disease, stage IV disease with a single brain metastasis, or recurrent tumor after surgical resection that could be treated definitively with concurrent chemoradiation, and baseline pulmonary function of forced expiratory volume in 1 second ≥ 1 L. Patients who had received systemic chemotherapy (regardless of response before enrollment) also were eligible. Eligible patients consented to participate after they were evaluated and deemed suitable candidates for concurrent chemoradiation.
The primary end point was the first occurrence of severe (grade ≥ 3) RP or local failure (LF). The choice to use two primary end points emphasized the importance of being free of RP—a potentially lethal form of toxicity—in addition to local disease control. From our historical data,13,14 we assumed a 15% RP rate at 1 year in the IMRT group and a 5% RP rate in the PSPT group; we also assumed a 25% LF rate in both groups (because the prescribed dose to tumor was the same in both arms by design). With a maximum of 150 randomly assigned and evaluable patients we would have 81% power to detect such a difference with a one-sided type I error rate of ≤ 10%. The posterior probability of PSPT being better than IMRT on the basis of the primary end points was to be reported. The Bayesian adaptive design was constructed to possess the desirable frequentist properties. Detailed information on assumptions for the study design and trial operating characteristics can be found in the study protocol (Data Supplement).
Radiation Treatment Planning and Randomization
Each patient underwent standard radiation treatment planning procedures, which included four-dimensional computed tomography scanning for motion assessment and target delineation, and the development of pairs of IMRT and PSPT treatment plans for dosimetric comparison. Commercial treatment planning systems were used to create plans for each modality. Beginning in the first year of the protocol, the IMRT planning system was supplemented with an in-house automated optimization algorithm that improved plan quality.15
Both plans were evaluated according to prespecified dose-volume constraints developed for photon radiotherapy (Data Supplement). The prescribed tumor dose was 74 or 66 Gy(RBE), whichever could be achieved safely within these constraints. Gy(RBE) is the unit of absorbed dose of protons; it represents the absorbed dose for photons (Gy) multiplied by the relative biologic effectiveness (RBE) factor for protons. Patients were eligible for random assignment only if both plans satisfied the constraints on lung V20 and MLD. The initial 20 patients were randomly assigned equally to each arm; subsequent patients underwent adaptive random assignment, with the randomization probability proportional to the 1-year failure rate in each arm. Observed RP or LF events were updated as they occurred. Patients with unrandomizable plans (ie, those whose plans did not meet constraints) received PSPT or IMRT, whichever produced the acceptable plan (Fig 1A). All patients received standard platinum- and taxane-based chemotherapy concurrent with radiotherapy; pemetrexed was allowed for patients with adenocarcinoma. Our experience indicated that the use of different chemotherapy agents routinely prescribed for patients with NSCLC would not affect the primary end points tested in this study.16
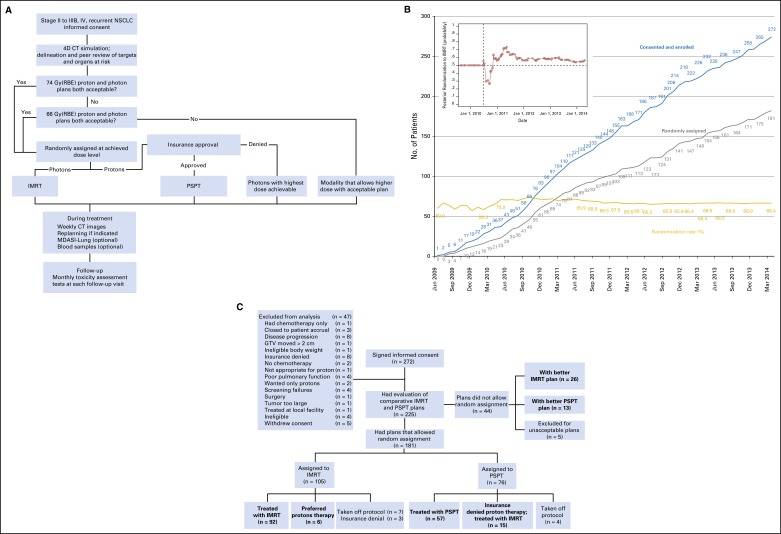
Fig 1.
(A) The adaptive randomization process. Eligibility criteria included stage II to IIIB non–small-cell lung cancer (NSCLC), or stage IV NSCLC with a single brain metastasis or isolated tumor recurrence after surgical resection; 50% of patients had disease progression after systemic chemotherapy before enrollment. All patients underwent four-dimensional computed tomography (4D CT)–based treatment simulation; target volume contours and preliminary plans were reviewed before patients were randomly assigned. The prescribed dose for both sets of treatment plans (intensity-modulated [photon] radiation therapy [IMRT] and passive scattering proton therapy [PSPT]) was 74 Gy (relative biologic effectiveness [RBE]). If one of the two plans did not meet prespecified dose constraints (Data Supplement), the prescribed dose was reduced to 66 Gy for a second pair of plans. Patients were randomly assigned only when both IMRT and PSPT plans met dose constraint standards. If one of the two plans did not meet dose constraints at 66 Gy(RBE), the patient was treated with the modality that produced the acceptable dose distribution. During treatment, weekly 4D CT scans were obtained for all patients and additional treatment plans were created as needed to account for anatomic changes. Patients were contacted weekly with a questionnaire to assess symptoms of pneumonitis to ensure that radiation pneumonitis events (toxicity assessment) were accurately noted. (B) Cumulative patient random assignment and enrollment over time. The inset shows posterior randomization probability to IMRT, with the vertical dashed line representing the last date (June 22, 2010) at which the randomization probability was 0.5. The first patient was randomly assigned on August 17, 2009, and the last patient was assigned on April 18, 2014; 60% to 67% of all patients who consented to participate were eligible for random assignment. (C) Trial profile. The final numbers of patients included in the analysis are shown in boldface. GTV, gross tumor volume; Gy(RBE), the absorbed radiation dose, in Gy, multiplied by the relative biologic effectiveness factor (RBE) for protons; MDSAI, MD Anderson Symptom Inventory.
Assessment of Primary End Points
RP was scored with the Common Terminology Criteria for Adverse Events (version 3.0). Factors required for a diagnosis of RP included receipt of radiation that included a certain volume of normal lung, radiographic changes that suggested inflammation consistent with the radiation dose distribution within 12 months after starting chemoradiation, and symptoms attributable to RP. LF was defined as treatment failure within the planning target volume plus a ≤ 1-cm margin. Images used to report LF were registered with radiation dose distribution to accurately assess the location of the failure. Biopsy to confirm LF was strongly recommended (Data Supplement). An internal outcomes review committee reviewed each event to ensure objectivity and consistency in reporting RP and LF. Final RP outcomes also were reviewed and approved by independent external experts.
Data Analysis
Associations of categorical variables were analyzed with Fisher’s exact tests. Differences in continuous variables between two groups were analyzed with Wilcoxon rank sum tests. Survival times were calculated from the date of protocol registration to the first occurrence of the considered event. A Cox proportional hazards regression model was used for univariable and multivariable analysis to assess the effect of patient, tumor, and other characteristics on the end points.
Data were analyzed in three ways: randomly assigned and treated accordingly (randomly assigned [n = 149]), intention to treat (n = 173), and could not be randomly assigned (n = 39). Figure 1C shows patient groupings according to treatment modality received. Herein, we present the results of the first group (randomly assigned) for analysis. Results for the intention-to-treat group and those who could not be randomly assigned are presented in the Data Supplement.
Competing-risks regression analysis was performed according to the method by Fine and Gray.17 For multivariable analyses, all factors with P ≤ .25 in the univariable analysis were included; backward elimination was performed with the most parsimonious multivariable model presented. Subhazard ratios for the failure events of primary interest (grade ≥ 3 RP and LF) are reported. Competing events for the primary end points were distant metastases and death as a result of disease or other causes. In exploratory analyses, we evaluated whether a learning curve (ie, improvements in the design or delivery of radiation with either method [IMRT or PSPT]) over the course of the study influenced outcomes by analyzing patients according to time of enrollment (before or after the trial midpoint—September 27, 2011).
RESULTS
Between June 2009 and March 2014, 272 patients consented to participate (Fig 1B); 47 patients were excluded before the planning process began (insurance coverage denial of proton treatment [n = 8], and other reasons shown in Fig 1C). A total of 225 enrolled patients completed the planning process with two plans each; 149 of the 181 patients who were randomly assigned were treated accordingly (IMRT [n= 92]; PSPT [n = 57]). Thirty two patients were not treated according to protocol allocation (insurance denial of PSPT [n = 15] and all of those patients received IMRT; insurance denial of the protocol [n = 3] and those patients were taken off protocol; patient preference for PSPT [n = 6]; or other reasons [n = 8]; Fig 1C). Plans for 44 patients did not allow random assignment and were treated with the modality that produced the acceptable dose distribution (IMRT [n= 26]; PSPT [n = 13]); five patients were not treated on protocol because a definitive radiation plan could not be achieved (Fig 1C). Patient- and tumor-related characteristics did not differ between groups (Table 1; Data Supplement).
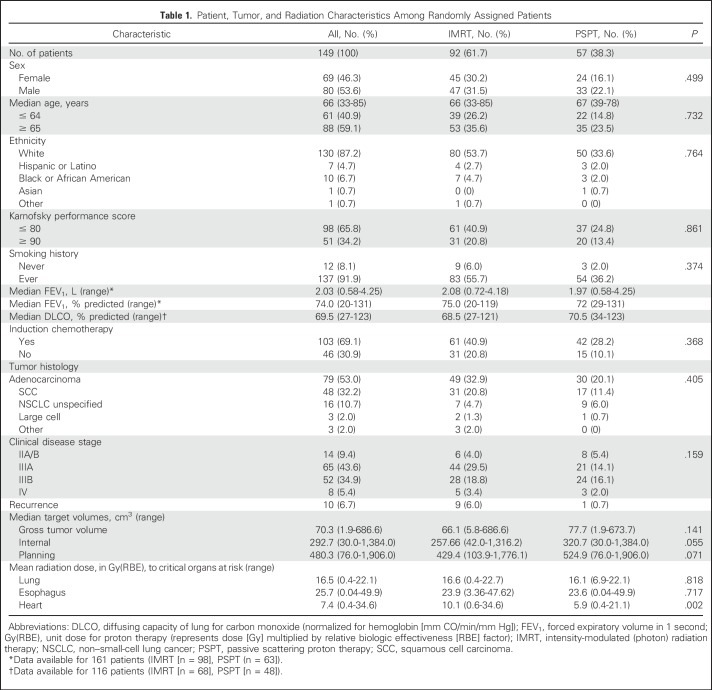
Table 1.
Patient, Tumor, and Radiation Characteristics Among Randomly Assigned Patients
Radiation Dose Metrics by Treatment Modality
PSPT significantly reduced the mean radiation dose to the heart (P = .002). No differences were found between IMRT and PSPT in the mean doses to the lung or esophagus (Table 1; Fig 2A; Data Supplement). Compared with IMRT, PSPT reduced the lung V5-10 but increased lung V20-80 (Fig 2B). PSPT spared more heart volume at all dose levels measured than did IMRT (Fig 2B). Comparisons for the intention-to-treat and the groups who could not be randomly assigned are shown in the Data Supplement.
Fig 2.
(A) Box plot of mean radiation doses to the lung, esophagus, and heart. Mean doses to the lung and esophagus were no different between the two treatment groups (intensity-modulated [photon] radiation therapy [IMRT] and passive scattering proton therapy [PSPT]), but the mean heart dose was lower for those treated with protons (P = .002). Whiskers indicate 1.5 times the interquartile range above and below the mean; dots represent outliers. (B) Box plot of distributions of dose-volume indices for the lung and heart. PSPT led to smaller volumes of lung being exposed to low volume doses (V5-10) and larger volumes of lung exposed to ≥ 20 Gy (relative biologic effectiveness [RBE]). PSPT reduced the volume of heart exposed to all dose levels measured (5 to 80 Gy [RBE]). Whiskers indicate 1.5 times the interquartile range above and below the mean; dots represent outliers.
Primary End Points by Treatment Modality
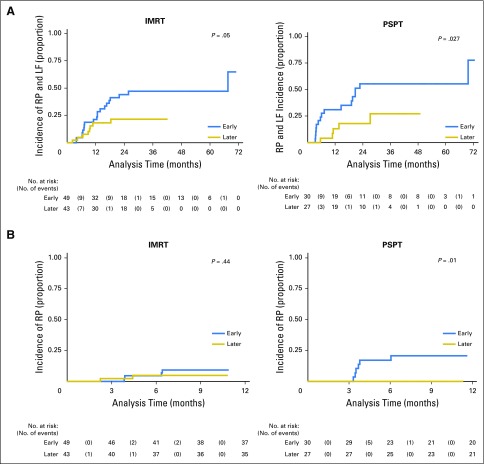
The median follow-up times for the IMRT group were 24.1 months for all patients and 36.4 months for patients alive at the time of analysis; corresponding median follow-up times for the PSPT group were 25.7 months (all patients) and 48.8 months (surviving patients). Twelve patients developed grade ≥ 3 RP (six in each group). At 1 year, the RP rates were 8.1% for all patients (IMRT, 6.5%; PSPT, 10.5%; P = .537). Two patients in the IMRT group had grade 5 RP; no patients in the PSPT group had grade 4 or 5 RP. Rates of LF at 12 months were 10.7% for all patients (IMRT, 10.9%; PSPT, 10.5%; P = 1.0); all LF rates were considerably lower than the 25% assumed in the trial design. Combined rates of RP and LF at 12 months were 17.4% after IMRT and 21.1% after PSPT (P = .175; Fig 3; Data Supplement). The median overall survival times were 29.5 months for patients in the IMRT group and 26.1 months for patients in the PSPT group (P = .297; Data Supplement). The posterior probability of IMRT being better than PSPT was 0.54. Results from the analyses of patients grouped as intention-to-treat and those who could not be randomly assigned were consistent with the results reported here (Data Supplement).
Fig 3.
Cumulative incidence of severe (grade 3) radiation pneumonitis (RP) and local failure (LF) according to treatment among patients who were randomly assigned and treated according to random assignment. (A) Cumulative incidence of RP and LF for patients treated with intensity-modulated (photon) radiation therapy (IMRT) or passive scattering proton therapy (PSPT). (B) Cumulative incidence of RP. (C) Cumulative incidence of LF. Results were similar when patients were analyzed by intention to treat or by treatment received (data not shown).
Primary End Points by Time of Enrollment
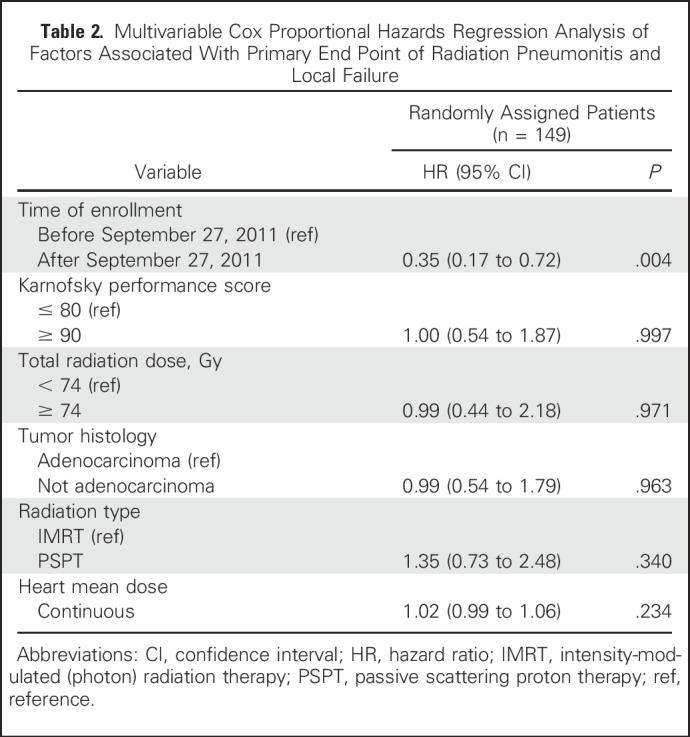
In an exploratory analysis to assess the potential effect of the time of enrollment we grouped patients as having enrolled before the study midpoint of September 27, 2011 (early), or after (later). No differences in clinical characteristics were noted between patients grouped as early versus later in the IMRT group. In the PSPT group, more patients in the later group had adenocarcinoma (14% v 6% in the early group; P < .001), and the later group had considerably smaller gross tumor volumes (56.0 v 150.6 cm3 in the early group; P = .01; Data Supplement). The combined rates of grade ≥ 3 RP and LF at 12 months also differed according to time of enrollment. In the IMRT group, those rates were 21.1% for the early group and 18.2% for the later group (P = .047). In the PSPT group, the rates of grade ≥ 3 RP and LF at 12 months were 31.0% for the early group versus 13.1% for the later group (P = .027; Fig 4A; Data Supplement). Of note, all six grade ≥ 3 RP events in the PSPT group occurred in the early group, whereas in the IMRT group, grade ≥ 3 RP occurred throughout the trial (Fig 4B; Data Supplement).
Fig 4.
(A) Cumulative incidence of radiation pneumonitis (RP) and local failure (LF) among patients who were randomly assigned and treated according to time of enrollment (early indicates enrollment before the midpoint of the trial [September 27, 2011; median follow-up, 29 months]; later indicates enrollment after the midpoint [median follow-up, 23 months]). Patients in the later group had lower rates of RP and LF. Similar results were found when patients were analyzed by intention to treat or by treatment received (data not shown). (B) Cumulative incidence of RP among patients who were randomly assigned and treated according to time of enrollment. In the intensity-modulated (photon) therapy (IMRT) group, RP occurred in both the early and the later groups; in the passive scattering proton therapy (PSPT) group, RP occurred only in the early group. The results suggest the existence of a learning curve for the delivery of PSPT, with corresponding improvements in PSPT over the course of the trial.
Risk Factors
In univariable analyses, combined RP and LF rates were associated with time of enrollment (early v later), MLD, and lung V5-20. RP was associated with time of enrollment, age, MLD, total gross tumor volume, and lung volume that received 5 to 10 Gy(RBE). LF was associated only with time of enrollment. In multivariable Cox proportional hazards regression analyses, the only significant adverse factor for RP and LF combined (and for RP and LF individually) was time of enrollment (Table 2). Because the time of enrollment may have been a surrogate for smaller tumors and lower prescribed radiation dose (Data Supplement), we repeated the multivariable Cox proportional hazards regression analyses with the exclusion of time of enrollment. Results showed that MLD (P = .044) and lung V10 (P = .008) were adverse factors for RP and LF combined. Factors associated with RP were patient age (≤ 64 v ≥ 65 years of age), MLD, and planning target volume. No factors were associated with LF when time of enrollment was excluded. Competing-risk analyses that considered locoregional recurrence, high-grade RP, distant metastasis, cancer-related death, and other death as competing events showed no differences between IMRT and PSPT in terms of RP or LF.
Table 2.
Multivariable Cox Proportional Hazards Regression Analysis of Factors Associated With Primary End Point of Radiation Pneumonitis and Local Failure
DISCUSSION
On the basis of both Bayesian and frequentist analyses, this prospective randomized study, which to our knowledge, is the first to directly compare IMRT with PSPT, revealed no statistically significant difference in our primary end points (grade ≥ 3 RP or LF) after IMRT or PSPT for patients with locally advanced NSCLC. Considerably fewer events occurred in this trial than expected, especially grade ≥ 3 RP after IMRT (6.5% v 15% in historical data).2,18 LF rates at 12 months also were lower than expected after IMRT or PSPT (25% expected v 10.7% actual). Reasons for these improvements in outcome are being investigated. For example, to determine whether a learning curve for proton plans was truly present we generated new treatment plans for the six patients who developed RP in the early PSPT group to see whether the dose distribution could be further optimized from the delivered plan. Early findings from this exercise suggest that the MLD in three of the six patients was lower in the new plans (data not shown), which supports the existence of a learning curve.
Advantages on the basis of dose distributions have often been used to justify new technologies in radiation therapy. Many treatment plan comparison–studies have suggested that proton therapy could reduce the volume of normal tissue exposed to various dose levels relative to photon therapy.19 However, conclusions drawn from planning studies may not always be reliable. In the current study with similar MLD between groups, PSPT reduced the low-dose bath (lung V5-10), but exposed significantly larger volumes to higher doses (lung V20-80).
The fact that PSPT was associated with larger high-dose lung volumes presumably reflected the use of relatively large safety margins for the three-dimensional scattering proton beams. The high-dose volumes may have contributed to the higher-than-expected rates of RP after proton therapy. The results also imply that the dose-volume constraints (derived from photon therapy) may not apply to the drastically different dose distribution patterns of PSPT—either a different set of constraints is needed to guide proton treatment planning or a unified set of constraints that applies to both photons and protons may emerge. One possibility would be to use the effective dose concept20 when evaluating proton lung plans or when comparing proton versus photon dose distributions.
Proton therapy has changed considerably over the past three decades with the introduction of hospital-based facilities with rotational gantries that allow treatment of tumors at any anatomic site, improvements in treatment planning capability, and the development of pencil beam scanning with intensity modulation. Nevertheless, the state-of-the-art of proton therapy had not advanced significantly during that time, perhaps because of the higher cost of proton therapy. Meanwhile, major improvements in IMRT have occurred over the past decade as evidenced by the lower-than-anticipated number of RP events in the IMRT arm. Specifically, the introduction of an automated IMRT optimization system during the first year after trial activation led to significant improvement in the potential clinical effectiveness of IMRT plans.15 The current findings suggest that the evolution of technology and increasing experience in its use over the course of a technology-based trial can influence outcomes and, thus, pose substantial challenges to demonstrate the clinical benefit of a new modality.
The allocation of patients was 0.58 to 0.42, with a higher probability of being randomly assigned to the IMRT arm. The Bayesian adaptive randomization design relies on event information being updated in real time so that the ratio of allocation to treatment arms can be adjusted before the next patient is randomly assigned. However, the median time to the development of the events observed in this study was approximately 5 months. In the meantime, the allocation between study arms had to continue according to the adaptive randomization parameters that already had been set. The Bayesian randomization also gave greater importance to more-recent events. Thus, patient allocation did not consider improvements in experience with the techniques or technologic evolution over the course of the trial.
Finally, although this trial was not designed to test survival, the median overall survival time of 28.8 months is consistent with a benchmark established by the Radiation Therapy Oncology Group (RTOG) protocol 0617 (ClinicalTrial.gov identifier: NCT00533949).1 This finding is encouraging because the patients enrolled in the current protocol had less-favorable disease than those in RTOG 0617. Our chemoradiation trial included patients with stage IV disease and patients with recurrent disease after surgery; approximately 50% of the patients had experienced disease progression during systemic therapy. In RTOG 0617, heart V5 and V35 independently predicted overall survival. In our study, PSPT reduced the heart volume exposed to all radiation dose levels relative to IMRT. The importance of heart sparing for overall survival is being evaluated in a phase III randomized lung trial, RTOG 1308 (ClinicalTrials.gov identifier: NCT01993810), which will provide much-needed level 1 evidence on proton therapy for lung cancer. Another important trial, a phase II study of IMRT compared with the next-generation proton technique intensity-modulated proton therapy, is ongoing (ClinicalTrials.gov identifier: NCT01629498). Findings from these two trials will be critical for addressing the issues identified here and for providing additional evidence of the efficacy of proton beam therapy relative to photons.
In conclusion, we note no benefit in grade ≥ 3 RP or LF after PSPT presumably because PSPT was not associated with improved lung dose-volume indices. PSPT significantly reduced heart exposure in terms of both radiation dose and heart volume, and its influence on cardiac toxicity and overall survival is under active investigation. Outcomes after both IMRT and PSPT improved over the course of the trial, but the magnitude of improvement in RP was greater and statistically more significant in the PSPT arm.
ACKNOWLEDGMENT
We thank the patients who volunteered to participate in this trial, our colleagues, and research staff—Jaques B. Bluett for outstanding work developing the dosimetric plans, Mark Munsell for his endless real-time statistical support in conducting this trial, Mike Hernandez for his statistical support, and Jeffrey Bradley, MD, Maria Werner-Wasik, MD, and Charles Simone, MD, who served on the external review board. We also thank Christine Wogan for her editorial guidance in the development and finalization of the article.
Footnotes
Supported by National Cancer Institute Grants No. P01 CA021230, U19 CA021239, and P30 CA016672.
Clinical trial information: NCT00915005.
See accompanying Editorial on page 1777
AUTHOR CONTRIBUTIONS
Conception and design: Zhongxing Liao, J. Jack Lee, Ritsuko Komaki, Daniel R. Gomez, Michael S. O’Reilly, Frank V. Fossella, George R. Blumenschein Jr, Pamela K. Allen, Noah Chan Choi, Thomas F. DeLaney, Stephen M. Hahn, James D. Cox, Charles S. Lu, Radhe Mohan
Financial support: Radhe Mohan
Administrative support: Radhe Mohan
Provision of study materials or patients: Ritsuko Komaki, Daniel R. Gomez, Michael S. O’Reilly, Ara A. Vaporciyan, Stephen G. Swisher, James D. Cox, Radhe Mohan
Collection and assembly of data: Zhongxing Liao, Daniel R. Gomez, Michael S. O’Reilly, Frank V. Fossella, George R. Blumenschein Jr, Noah Chan Choi, Thomas F. DeLaney, Stephen M. Hahn, Charles S. Lu, Radhe Mohan
Data analysis and interpretation: Zhongxing Liao, J. Jack Lee, John V. Heymach, Ara A. Vaporciyan, Stephen G. Swisher, Pamela K. Allen, Radhe Mohan
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Bayesian Adaptive Randomization Trial of Passive Scattering Proton Therapy and Intensity-Modulated Photon Radiotherapy for Locally Advanced Non–Small-Cell Lung Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Zhongxing Liao
Honoraria: Varian Medical Systems
Speakers’ Bureau: Varian Medical Systems
Travel, Accommodations, Expenses: Varian Medical Systems
J. Jack Lee
No relationship to disclose
Ritsuko Komaki
No relationship to disclose
Daniel R. Gomez
Honoraria: Merck
Consulting or Advisory Role: AstraZeneca
Speakers’ Bureau: Bristol-Myers Squibb
Research Funding: Merck
Michael S. O’Reilly
No relationship to disclose
Frank V. Fossella
No relationship to disclose
George R. Blumenschein Jr
Honoraria: AbbVie, Genentech, Bayer AG, Bristol-Myers Squibb, Celgene
Consulting or Advisory Role: Bristol-Myers Squibb, Bayer AG, Celgene, Clovis Oncology, AbbVie, ARIAD Pharmaceuticals, AstraZeneca, Merck
Research Funding: Merck, AstraZeneca, Celgene, AbbVie, Genentech, Xcovery, Novartis, Bayer Schering Pharma, Bristol-Myers Squibb, GlaxoSmithKline
John V. Heymach
Stock or Other Ownership: Cardinal Spine & Pain Medicine, Bio-Tree Systems
Consulting or Advisory Role: AstraZeneca, AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Medivation, ARIAD Pharmaceuticals, Synta, Oncomed, Novartis, Genentech, Calithera Biosciences
Research Funding: AstraZeneca (Inst)
Ara A. Vaporciyan
No relationship to disclose
Stephen G. Swisher
No relationship to disclose
Pamela K. Allen
No relationship to disclose
Noah Chan Choi
No relationship to disclose
Thomas F. DeLaney
No relationship to disclose
Stephen M. Hahn
No relationship to disclose
James D. Cox
No relationship to disclose
Charles S. Lu
No relationship to disclose
Radhe Mohan
Patents, Royalties, Other Intellectual Property: The University of Texas MD Anderson Cancer Center MDA09-097 patent pending
REFERENCES
- 1.Bradley JD, Paulus R, Komaki R, et al. : Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): A randomised, two-by-two factorial phase 3 study. Lancet Oncol 16:187-199, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liao ZX, Komaki RR, Thames HD, Jr, et al. : Influence of technologic advances on outcomes in patients with unresectable, locally advanced non-small-cell lung cancer receiving concomitant chemoradiotherapy. Int J Radiat Oncol Biol Phys 76:775-781, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Liao ZX, Travis EL, Tucker SL: Damage and morbidity from pneumonitis after irradiation of partial volumes of mouse lung. Int J Radiat Oncol Biol Phys 32:1359-1370, 1995 [DOI] [PubMed] [Google Scholar]
- 4.Wang S, Liao Z, Wei X, et al. : Analysis of clinical and dosimetric factors associated with treatment-related pneumonitis (TRP) in patients with non-small-cell lung cancer (NSCLC) treated with concurrent chemotherapy and three-dimensional conformal radiotherapy (3D-CRT). Int J Radiat Oncol Biol Phys 66:1399-1407, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Marks LB, Bentzen SM, Deasy JO, et al. : Radiation dose-volume effects in the lung. Int J Radiat Oncol Biol Phys 76:S70-S76, 2010. (suppl 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murshed H, Liu HH, Liao Z, et al. : Dose and volume reduction for normal lung using intensity-modulated radiotherapy for advanced-stage non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 58:1258-1267, 2004. [Erratum: Int J Radiat Oncol Biol Phys 59:921, 2004] [DOI] [PubMed] [Google Scholar]
- 7.Glimelius B, Montelius A: Proton beam therapy - Do we need the randomised trials and can we do them? Radiother Oncol 83:105-109, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Goitein M, Cox JD: Should randomized clinical trials be required for proton radiotherapy? J Clin Oncol 26:175-176, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Bentzen SM: Randomized controlled trials in health technology assessment: Overkill or overdue? Radiother Oncol 86:142-147, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bothwell LE, Podolsky SH: The emergence of the randomized, controlled trial. N Engl J Med 375:501-504, 2016 [DOI] [PubMed] [Google Scholar]
- 11.Suit H, Goldberg S, Niemierko A, et al. : Proton beams to replace photon beams in radical dose treatments. Acta Oncol 42:800-808, 2003 [DOI] [PubMed] [Google Scholar]
- 12.Lee JJ, Chen N, Yin G: Worth adapting? Revisiting the usefulness of outcome-adaptive randomization. Clin Cancer Res 18:4498-4507, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yom SS, Liao Z, Liu HH, et al. : Initial evaluation of treatment-related pneumonitis in advanced-stage non-small-cell lung cancer patients treated with concurrent chemotherapy and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 68:94-102, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Sejpal S, Komaki R, Tsao A, et al. : Early findings on toxicity of proton beam therapy with concurrent chemotherapy for nonsmall cell lung cancer. Cancer 117:3004-3013, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Zhang X, Li X, Quan EM, et al. : A methodology for automatic intensity-modulated radiation treatment planning for lung cancer. Phys Med Biol 56:3873-3893, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Jin H, Tucker SL, Liu HH, et al. : Dose-volume thresholds and smoking status for the risk of treatment-related pneumonitis in inoperable non-small cell lung cancer treated with definitive radiotherapy. Radiother Oncol 91:427-432, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fine JP, Gray RJ: A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496-509, 1999 [Google Scholar]
- 18.Jiang ZQ, Yang K, Komaki R, et al. : Long-term clinical outcome of intensity-modulated radiotherapy for inoperable non-small cell lung cancer: The MD Anderson experience. Int J Radiat Oncol Biol Phys 65:1087-1096, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Chang JY, Zhang X, Wang X, et al. : Significant reduction of normal tissue dose by proton radiotherapy compared with three-dimensional conformal or intensity-modulated radiation therapy in stage I or stage III non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 65:1087-1096, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Tucker SL, Mohan R, Liengsawangwong R, et al. : Predicting pneumonitis risk: A dosimetric alternative to mean lung dose. Int J Radiat Oncol Biol Phys 85:522-527, 2013 [DOI] [PubMed] [Google Scholar]