Abstract
A rise in reactive oxygen species (ROS) may contribute to cardiovascular disease by reducing nitric oxide (NO) levels, leading to loss of NO’s vasodilator and anti-inflammatory effects. Although primarily studied in larger conduit arteries, excess ROS release and a corresponding loss of NO also occur in smaller resistance arteries of the microcirculation, but the underlying mechanisms and therapeutic targets have not been fully characterized. We examined whether either of the two subunits of telomerase, telomerase reverse transcriptase (TERT) or telomerase RNA component (TERC), affect microvascular ROS production and peak vasodilation at baseline and in response to in vivo administration to angiotensin II (ANG II). We report that genetic loss of TERT [maximal dilation: 52.0 ± 6.1% with vehicle, 60.4 ± 12.9% with Nω-nitro-l-arginine methyl ester (l-NAME), and 32.2 ± 12.2% with polyethylene glycol-catalase (PEG-Cat) (P < 0.05), means ± SD, n = 9–19] but not TERC [maximal dilation: 79 ± 5% with vehicle, 10.7 ± 9.8% with l-NAME (P < 0.05), and 86.4 ± 8.4% with PEG-Cat, n = 4–7] promotes flow-induced ROS formation. Moreover, TERT knockout exacerbates the microvascular dysfunction resulting from in vivo ANG II treatment, whereas TERT overexpression is protective [maximal dilation: 88.22 ± 4.6% with vehicle vs. 74.0 ± 7.3% with ANG II (1,000 ng·kg−1·min−1) (P = not significant), n = 4]. Therefore, loss of TERT but not TERC may be a key contributor to the elevated microvascular ROS levels and reduced peak dilation observed in several cardiovascular disease pathologies.
NEW & NOTEWORTHY This study identifies telomerase reverse transcriptase (TERT) but not telomerase RNA component as a key factor regulating endothelium-dependent dilation in the microcirculation. Loss of TERT activity leads to microvascular dysfunction but not conduit vessel dysfunction in first-generation mice. In contrast, TERT is protective in the microcirculation in the presence of prolonged vascular stress. Understanding the mechanism of how TERT protects against vascular stress represents a novel target for the treatment of vascular disorders.
Keywords: angiotensin II, flow-mediated dilation, microcirculation, telomerase, telomerase reverse transcriptase
INTRODUCTION
Approximately one in every three deaths can be attributed to cardiovascular disease (22). Previous research seeking to lessen the cardiovascular disease burden has predominantly explored disease-related pathological changes (e.g., oxidative stress, inflammation, and remodeling) occurring in endothelial and smooth muscle cell layers of large conduit arteries. Small resistance arteries of the microcirculation have received less attention (10), despite provocative reports illustrating their pathophysiological (17, 18, 20) and prognostic (5, 27, 28) importance in cardiovascular disease.
A major role of the microvascular endothelium is regulation of vascular tone. Microvascular dilation is elicited through the release of a variety of endothelium-derived factors in response to chemical agonists or increases in blood flow. Nitric oxide (NO) is the dominant flow-induced vasodilator in the microcirculation of subjects free of cardiovascular disease, whereas H2O2 replaces NO in patients with coronary artery disease (20). Although H2O2 maintains dilation as NO levels drop, chronic and unopposed release of mitochondria-derived H2O2 (mtH2O2) from the microvascular endothelium, together with loss of anti-inflammatory actions of NO, is believed to elicit proinflammatory changes that contribute to disease development (6). Clarification of the cellular factors responsible for this microvascular transition from NO to H2O2 is needed to identify potential therapeutic targets to combat excessive reactive oxygen species (ROS) production and lessen microvascular dysfunction.
Existing evidence has established that loss of telomerase is closely associated with elevations in mitochondrial ROS production. Telomerase reverse transcriptase (TERT), the catalytic subunit of the telomerase holoenzyme, and the telomerase RNA component (TERC) are critical for canonical telomerase function (25). While TERT is largely studied in models of aging and cancer because of its telomere-lengthening effects in the nucleus, TERT also acts to counteract oxidative stress in the mitochondria of the microcirculation (1). Short-term ex vivo pharmacological inhibition of TERT increases, and short-term ex vivo pharmacological activation of TERT decreases, release of H2O2 during flow-mediated dilation (FMD) in human microvessels (2). The impact of prolonged, genetic loss of TERT and TERC on microvascular dilation and ROS release is unknown, as is the potential protective effect of TERT overexpression in vivo on the microvascular effects of established pathological factors that augment ROS formation in the microcirculation, such as elevated angiotensin II (ANG II). To explore the role of increased or decreased telomerase activity under pathological conditions, we used the well-defined model of ANG II infusion to induce ROS formation and endothelial dysfunction (4, 11, 13, 29).
Understanding these in vivo relationships deepens our understanding of the potential pathophysiological effect of reduced TERT and/or TERC in the microcirculation and provides valuable information about the therapeutic role of TERT in the microcirculation in an in vivo setting.
We hypothesized that genetic loss of TERT or TERC increases flow-induced release of H2O2 in both coronary and mesenteric microcirculations of TERT and TERC knockout (KO) mice. We further hypothesized that TERT overexpression [TERT transgenic (Tg)] limits, whereas loss of TERT exacerbates, the damaging effects of in vivo ANG II administration on microvascular dilation.
MATERIALS AND METHODS
Overview.
To address our hypotheses, we used established genetic gain-of-function and loss-of-function models for TERT (TERT Tg and TERT KO) and a loss-of-function model for TERC (TERC KO). Later-generation TERT KO animals were also used to assess the effect of progressive loss of TERT on microvascular dilation. Microvascular phenotypes were examined using ex vivo video microscopy (overall dilation and contribution of NO vs. H2O2 to dilation), fluorescence detection (H2O2 release during dilation), and Western blot quantification of NO synthase (NOS) levels. We also evaluated the response to the commonly used vascular stressor ANG II to determine whether TERT modulates microvascular tone under pathological conditions.
General protocol in mice.
All experiments were performed according to the American Guidelines for the Ethical Care of Animals and were approved by our Institutional Animal Care and Use Committee. C57BL/6 TERT KO (TERT−/−) mice were obtained from Ronald DePinho (MD Anderson Cancer Center, Houston, TX). TERC KO (TERC−/−) mice were purchased from Jackson Laboratories (stock 004132 mTR−/−, Bar Harbor, ME). KO mice were bred as heterozygotes to generate first-generation KO mice. To generate third-generation KO mice, homozygous KO mice of the first generation were inbred for three consecutive generations. TERT Tg mice were provided by Dennis Bruemmer (University of Pittsburgh, Pittsburgh, PA). Both male and female mice were used in the experiments outlined in this study, and all animals were studied at 3–4 mo of age and compared with wild-type (WT) control mice of the same breeding line. When possible, arteries from the same mouse were used for multiple experiments (e.g., functional experiments and ROS evaluation).
All mice were housed and maintained at a temperature of 23°C with 12:12-h light-dark cycles and fed a solid standard diet (Na+ content: 0.4%) and water ad libitum. On the day of the experiment, mice were euthanized between 8 AM and 12 PM, and tissues (thoracic aorta, mesenteric resistance artery, and septal artery) were harvested and immediately placed in cold 4°C HEPES (containing 275 mM NaCl, 7.99 mM KCl, 4.9 mM MgSO4, 3.2 mM CaCl2·2H2O, 2.35 mM KH2PO4, 0.07 mM EDTA, 12 mM glucose, and 20 mM HEPES acid).
Cannulated arteriole preparation.
Third- or fourth-order branch arteries from the mesenteric artery (MA) and septal artery (SA) (~200-μm inner diameter) were cleaned of fat and connective tissue and prepared for continuous measurements of internal diameter as previously described (20, 21). In an organ chamber containing Krebs buffer, both ends of the vessel were cannulated with glass micropipettes and pressurized (60 mmHg) before stepwise increases in flow or administration of pharmacological agents, as we have previously described (14, 19, 23).
Vascular response to flow and pharmacological interventions.
The contribution of NO or H2O2 to dilation was assessed in TERT KO, TERC KO, and TERT Tg mice using FMD as previously described by Kuo et al. (16). Adjustment of the height of each reservoir in equal and opposite directions was used to generate flow via generation of a pressure gradient without changes in intraluminal pressure (16). Diameter at a given pressure gradient was recorded and expressed as percent maximal diameter. Two flow-response curves were generated for each vessel comparing untreated (vehicle) with effects of pharmacological inhibitors [NO inhibitor Nω-nitro-l-arginine methyl ester (l-NAME; 100 mM) and H2O2 scavenger polyethylene glycol-catalase (PEG-Cat; 500 U/ml)]. All pharmacological agents represent final concentrations in the organ bath and were added at volumes of <1% of the total bath volume.
Arteries were constricted with norepinephrine (10 μM for MA) or the thromboxane A2 analog U-46619 (100 nM for SA) to achieve a 20–70% stable reduction in passive diameter. Dose-response curves to acetylcholine (ACh; 1 nM−10 mM) and flow gradient (5–100 cmH2O) were performed to evaluate endothelium-dependent dilation. At the end of each experiment, the endothelium-independent dilator papaverine (Pap; 100 µM) was used to determine the maximal (passive) diameter at 60 mmHg.
Measurement of mitochondrial ROS.
Mito Peroxy Yellow 1 (mitoPY1) (7) was used as a secondary means to assess microvessel generation of mtH2O2 after loss of TERT. After cannulation in a warmed chamber (37°C) containing HEPES buffer at pH 7.4, MAs from TERT KO mice or from WT mice were perfused intraluminally with mitoPY1 (5 µM, 1 h) at low levels of flow below the threshold for dilation until the luminal surface was bathed in mitoPY1-containing buffer. Next, the pressure gradient was changed to 0–100 cmH2O. Experiments were performed in the presence or absence of the H2O2 scavenger PEG-Cat (500 U/ml). Fluorescence was evaluated with a Nikon Eclipse TE200 microscope using a krypton/argon laser at excitation wavelength of 488 nm and measured emission between 530 and 590 nm. For any given experiment, baseline fluorescence was established without flow. After 30 min of incubation with mitoPY1, each vessel was compared with no-flow conditions as a measure of flow-induced H2O2 production. In separate experiments, the specificity of the probe was confirmed with PEG-Cat (H2O2 scavenger) present at any time during the experiment. Levels of mtH2O2 are expressed as relative average fluorescence intensity normalized to background fluorescence and presented as percent change from baseline. All comparisons were made using arteries studied at the same session with constant microscope image display settings.
Microvascular response to ANG II.
Nonpressor dose (400 ng·kg−1·min−1) or fast pressor dose (1,000 ng·kg−1·min−1) of ANG II as previously described (15) was administered via osmotic minipumps for 14 days to induce prolonged in vivo microvascular stress in WT, TERT KO, and TERT Tg mice.
Western blot analysis.
Protein expression was analyzed as previously described (9). Briefly, total protein (30 μg) from MA (6–8 pooled arteries/mouse) lysates was loaded and separated using SDS-PAGE and then transferred into a polyvinylidene difluoride membrane. The membrane was incubated with one of the following primary antibodies: rabbit monoclonal anti-phosphorylated (Ser1177) endothelial NOS (eNOS; dilution 1:1,000, catalog no. MA5-14957, Invitrogen), rabbit polyclonal anti-total eNOS (dilution 1:1,000, catalog no. PA5-16887, Invitrogen), or mouse monoclonal anti-GAPDH (dilution 1:10,000, catalog no. ab8245, Abcam). Protein bands were detected with X-ray film exposure and quantified by ImageJ software.
Materials.
Norepinephrine and ANG II were obtained from Sigma-Aldrich, and U-46619 was obtained from Cayman Chemical. PEG-Cat was made by Quanta BioDesign (Plain City, OH), and l-NAME was purchased from Sigma-Aldrich. mitoPY1 (Tocris) was prepared in DMSO, and other agents were prepared in distilled water or Krebs buffer. All concentrations represent the final concentrations in the organ bath.
Statistical methods.
Data are presented as means ± SD. For all concentration-response curves, differences between groups at each concentration were determined using two-way repeated-measures ANOVA. A post hoc Tukey test was used for comparison of >2 means after ANOVA. P values of < 0.05 were deemed statistically significant. For fluorescence experiments and changes in gene/protein expression, either a t-test or one-way ANOVA with a post hoc Tukey test was used as appropriate.
RESULTS
Loss of TERT affects the magnitude of microvascular but not conduit vessel dilation in first-generation mice.
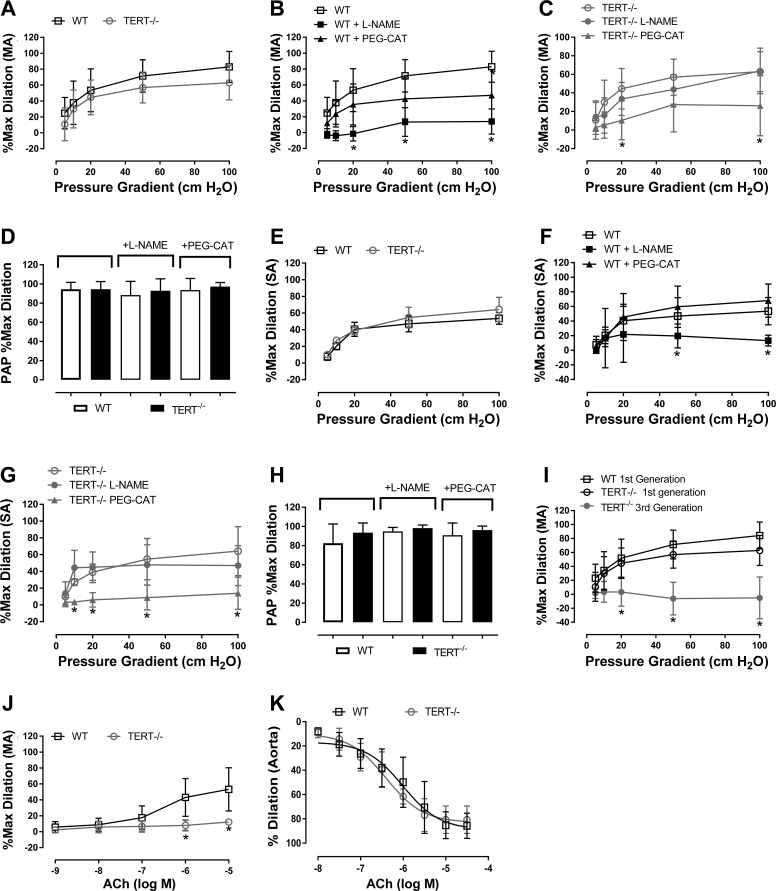
To examine whether the dilation in isolated arteries is impaired by the genetic loss of telomerase, we compared the overall peak dilation to flow (FMD) and to ACh in both mesenteric (MA) and septal (SA) microvessels and in the aorta. The overall magnitude of FMD was similar in MAs and SAs of TERT KO and WT mice [Fig. 1, A and E; maximal dilation: 77.4 ± 7.1% in the WT-MA group (n = 18), 53.6 ± 7.1% in the WT-SA group (n = 7), 52.0 ± 6.1% in the TERT KO-MA group (n = 18), and 64.2 ± 14.6% in the TERT KO-SA group (n = 5)]. The magnitude of overall peak dilation was similar between male and female mice [maximal dilation: 68 ± 17% in female WT mice (n = 7) and 42 ± 17% in TERT KO mice (n = 4) vs. 76 ± 6% in male WT mice (n = 7) and 54 ± 9% in TERT KO mice (n = 4), P = not significant; data not shown]. After intercrossing TERT KO mice to obtain third-generation mice, microvascular vasodilation to flow in the MA was eliminated (Fig. 1I).
Fig. 1.
Effect of telomerase deficiency on microvascular dilation to flow and acetylcholine (ACh) in first-generation mice. A: magnitude of flow-mediated dilation (FMD) in wild-type (WT) and telomerase reverse transcriptase knockout (TERT KO; TERT−/−) mice (n = 18 mice). The mechanism of FMD in WT (B) and TERT KO (C) mice was investigated after incubation with Nω-nitro-l-arginine methyl ester (l-NAME; nitric oxide synthase inhibitor) or polyethylene glycol-catalase (PEG-Cat; H2O2 scavenger) in isolated mesenteric arteries (MAs) (n = 7 mice). *P < 0.05 vs. control at specific pressure gradients. D: dilation to papaverine (Pap) in MAs treated with l-NAME and PEG-Cat. E−G: magnitude and mechanism of FMD in septal arteries (SAs) of WT (n = 7 mice) and TERT KO mice (n = 5 mice). *P < 0.05 at specific pressure gradients. H: dilation to Pap in SAs treated with l-NAME and PEG-Cat. I: magnitude of FMD in microvessels of first- vs. third-generation TERT KO mice. FMD was preserved in WT mice, reduced slightly in first-generation TERT KO (TERT−/−) mice (n = 18 mice), and severely impaired in third-generation TERT−/− mice (n = 10 mice). *P < 0.05 at specific pressure gradients. J and K: ACh-mediated dilation in MAs and aortas of WT (n = 8 mice) and TERT KO mice (n = 6 mice) at specific pressure gradients. *P < 0.05 at specific pressure gradients. Values are means ± SD. *P < 0.05 via two-way repeated-measures ANOVA with a post hoc Tukey test. Max, maximal.
ACh-induced dilation was reduced in the MA of TERT KO mice (first generation) compared with WT mice (P < 0.05; Fig. 1J). In contrast, we found no difference in the magnitude of overall peak ACh-induced dilation in conduit arteries (aorta) of first-generation TERT KO versus WT mice (Fig. 1K).
Loss of TERT decreases NO-mediated dilation and promotes H2O2 as a compensatory vasodilator during FMD.
We determined whether genetic loss of TERT or TERC alters the mechanism of FMD in MAs and SAs using a NOS inhibitor [l-NAME (100 µM)] or a H2O2 scavenger [PEG-Cat (500 U/ml)]. l-NAME impaired FMD in the MA and SA of WT mice (Fig. 1, B and F), whereas PEG-Cat had no effect [maximal dilation: 77.4 ± 7.1% with vehicle (n = 18), 20.7 ± 8.6% with l-NAME (n = 7, P < 0.05), and 54.1 ± 10.3% with PEG-Cat (n = 7–18)]. Similarly, as with overall dilator capacity, no differences in the mechanism of FMD were observed between sexes. Endothelium-independent dilation to Pap (Fig. 1, D and H) was not altered compared with WT mice.
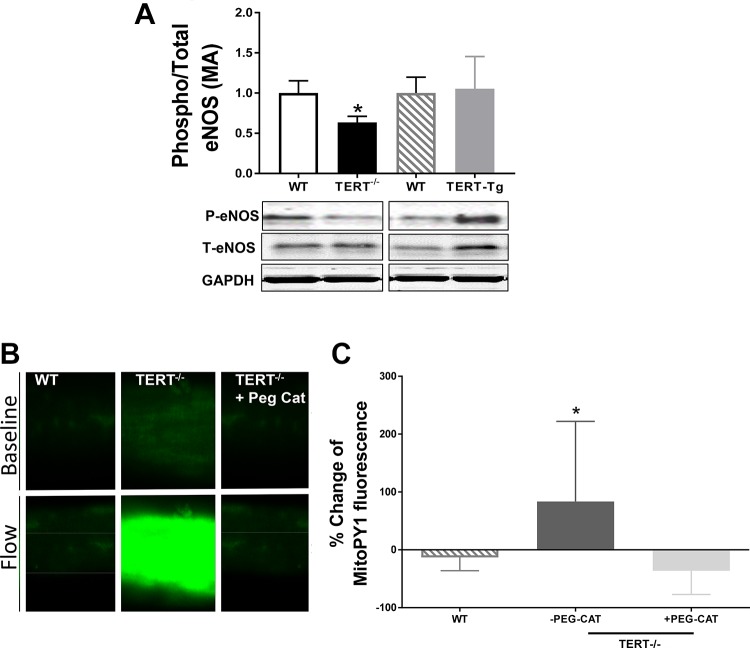
In contrast to WT mice, in the MA and SA of TERT KO mice, PEG-Cat but not l-NAME reduced dilation to flow [maximal dilation: 52.0 ± 6.1% with vehicle (n = 18), 60.4 ± 12.9% with l-NAME (n = 7), and 32.2 ± 12.2% with PEG-Cat (n = 7, P < 0.05); Fig. 1, C and G]. Dilation to Pap was unaltered (Fig. 1, D and H). Loss of NO was supported by a reduced ratio of phosphorylated to total eNOS in lysates from the MA of TERT KO mice (Fig. 2A). An elevation in mitoPY1 fluorescence, which detects mtH2O2, was observed in TERT KO mouse microvessels but not in WT mouse microvessels exposed to flow (Fig. 2, B and C).
Fig. 2.
Absence of telomerase reverse transcriptase (TERT) decreases endothelial nitric oxide synthase (eNOS) protein levels and increases mitochondrial reactive oxygen species. A: protein levels of phosphorylated eNOS (P-eNOS) and total eNOS (T-eNOS) were evaluated via Western blot analysis. T-eNOS and P-eNOS levels in mesenteric arteries (MAs) from wild-type (WT), TERT knockout (KO), and TERT transgenic (Tg) mice are shown. n = 6 mice/group. *P < 0.05. B and C: change in Mito Peroxy Yellow 1 (mitoPY1) fluorescence in WT and TERT KO mice in response to elevations in flow and in the presence or absence of polyethylene glycol-catalase (PEG-Cat). Values are means ± SD; n = 5 mice/group. *P < 0.05 vs. WT mice by t-test and one-way ANOVA with a post hoc Tukey test, respectively.
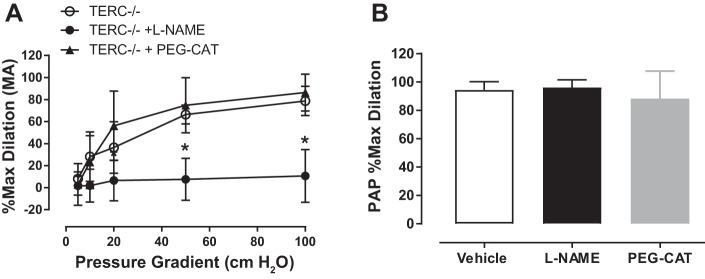
To examine whether TERC similarly influences H2O2 release during FMD, the contributions of NO and H2O2 to dilation were also assessed in TERC KO mice. Interestingly, in these mice, the magnitude and mediator of FMD were similar to WT mice (NO dependent) [maximal dilation: 79 ± 5% with vehicle, 10.7 ± 9.8% with l-NAME (P < 0.05), and 86.4 ± 8.4% with PEG-Cat, n = 7; Fig. 3A]. Pap-induced dilation was unchanged in TERC KO mice (Fig. 3B).
Fig. 3.
Effect of telomerase RNA component (TERC) deletion on microvascular dilation to flow. A: mechanism of flow-mediated dilation in mesenteric arteries (MAs) of TERC knockout (KO) mice. n = 7 mice/group. *P < 0.05 at specific pressure gradients. B: dilation to papaverine (Pap) in MAs of TERC KO mice. Values are means ± SD. P = not significant vs. vehicle via two-way repeated-measures ANOVA with a post hoc Tukey test. l-NAME, Nω-nitro-l-arginine methyl ester; max, maximal; PEG-Cat, polyethylene glycol-catalase.
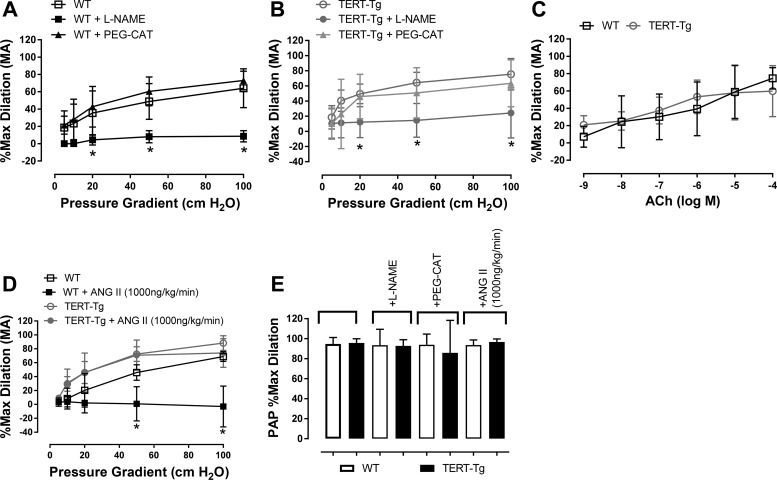
TERT overexpression protects against ANG II-induced microvascular dysfunction.
We first performed experiments to determine whether overexpression of TERT alters baseline microvascular function (NO bioavailability or overall dilation) using an established TERT Tg model (2). In the MA, endothelium-dependent dilation to flow (Fig. 4, A and B) and ACh (Fig. 4C) as well as endothelium-independent dilation to Pap (Fig. 4E) were similar to that observed in WT mice. The mechanism of FMD was unaltered relative to WT animals (remained NO dependent) [maximal dilation: 64.1 5.8% in the vehicle-WT group (n = 15) vs. 76.9 5.6 in the vehicle-TERT Tg group (n = 12) and 16.1 7.8% in the l-NAME-WT group (P < 0.05 vs. vehicle) vs. 24.4 12.5% in the l-NAME-TERT Tg group (P < 0.05 vs. vehicle), n = 7–12; Fig. 4, A and B].
Fig. 4.
Effect of telomerase reverse transcriptase overexpression (TERT Tg) on baseline flow-mediated dilation (FMD) and angiotensin II (ANG II)-induced endothelial dysfunction. The mediator of FMD was determined by incubation with Nω-nitro-l-arginine methyl ester (l-NAME; nitric oxide synthase inhibitor) or polyethylene glycol-catalase (PEG-Cat; H2O2 scavenger) in isolated mesenteric arteries (MAs) from wild-type (WT; A) mice (n = 15 mice) and TERT Tg (B) mice (n = 12 mice). C: acetylcholine (ACh)-induced dilation in WT and TERT Tg mice (n = 5 mice/group). D and E: FMD was assessed in MAs from WT and TERT Tg mice after treatment with 1,000 ng·kg−1·min−1 ANG II (osmotic minipump, n = 4 mice/group). E: dilation to papaverine (Pap) in all treatment conditions. Dilation to ACh and Pap was unchanged in conduit arteries (aorta) in TERT Tg mice at specific pressure gradients. Values are means ± SD. *P < 0.05 via two-way repeated-measures ANOVA with a post hoc Tukey test. Max, maximal.
Next, we examined whether TERT modifies the in vivo microvascular response to ANG II infusion via osmotic minipumps (12). To evaluate the protective effects of TERT overexpression on ANG II-induced microvascular endothelial dysfunction, we infused a pressor dose of ANG II (1,000 ng·kg−1·min−1) (3). In WT mice, prolonged high-dose ANG II infusion caused a complete loss of endothelium-dependent dilation to flow (Fig. 4D). However, TERT Tg animals showed only a small reduction in overall dilator capacity [maximal dilation: 88.22 ± 4.58% with vehicle vs. 74.0 ± 7.3% with ANG II (1,000 ng·kg−1·min−1), n = 4, P = not significant; Fig. 4D].
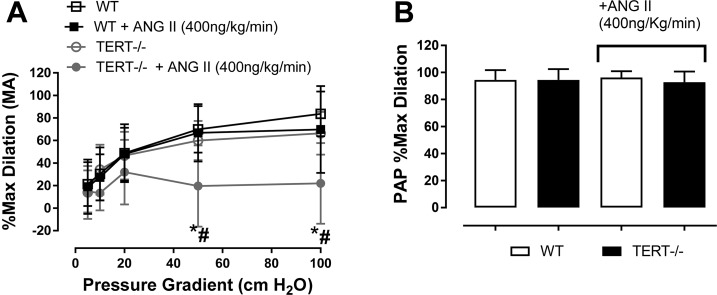
In TERT KO but not WT mice, the subpressor dose of ANG II [400 ng·kg−1·min−1 for 14 days (26)] significantly decreased FMD (Fig. 5A) without affecting endothelium-independent dilation to Pap (Fig. 5B).
Fig. 5.
Effect of telomerase reverse transcriptase (TERT) deletion on the angiotensin II (ANG II)-induced endothelial dysfunction. A: flow-mediated dilation was assessed in isolated mesenteric arteries (MAs) from wild-type (WT) and telomerase reverse transcriptase knockout (TERT−/−) mice after treatment with 400 ng·kg−1·min−1 ANG II (osmotic minipump). n = 6 mice/group. *P < 0.05 at specific pressure gradients; #P < XXXXXX. B: dilation to papaverine (Pap) in both treatment conditions. Values are means ± SD; n = 6. P = not significant via two-way repeated-measures ANOVA with a post hoc Tukey test. Max, maximal.
DISCUSSION
Novel findings.
This study reports four major new findings. First, loss of TERT impairs overall peak dilation to flow and ACh in the microcirculation but not in larger conduit arteries in first-generation mice and progressive loss of TERT in later generations further decreases the magnitude of microvascular FMD. Second, genetic loss of TERT shifts the primary mediator of microvascular FMD from NO to H2O2. Third, absence of TERT potentiates, whereas an increase in TERT prevents, ANG II-induced microvascular dysfunction. Finally, loss of the RNA component of telomerase, TERC, does not alter the vascular phenotype.
Role of TERT in maintaining physiological vasodilation.
The present data support the idea that telomerase maintains physiological NO-dependent dilation to flow. In particular, the loss of the enzymatic TERT subunit contributes to the development of microvascular endothelial dysfunction, characterized by a reduced overall dilator capacity and heightened contribution of H2O2 to FMD. These findings suggest that loss of TERT may be a key component of the pathophysiology of cardiovascular diseases affected by overabundance of microvascular ROS, which may precipitate proinflammatory changes, or impaired overall dilator capacity, which may lead to downstream ischemia. The data presented in this report are consistent with our earlier findings using short-term pharmacological TERT inhibition (2, 9) and extend these initial observations to chronic and in vivo effects of TERT in a genetic model. Moreover, the observation that deletion of TERC does not contribute the microvascular phenotypes identified in early generations underlines the physiological relevance of TERT itself as an independent regulator of ROS generation and FMD. This observation supports previous work by Santos and colleagues (25) indicating that ablation of either TERC or TERT alone does not result in equivalent functional effects, likely because of TERT’s unique ability to localize to the mitochondria. Additionally, our finding that progressive loss of overall peak dilation occurs in later generations of TERT KO mice suggests that telomere shortening may augment the effect of loss of TERT on the microcirculation.
Role of TERT in pathological vasodilation.
Recently, it has been shown that telomerase activity is negatively correlated with the development of abdominal aortic aneurysm, which is closely linked to elevated ANG II levels (8). Previous work has shown that ANG II significantly diminishes telomerase activity in endothelial progenitor cells (15), while we and others have previously shown that ANG-(1–7), which opposes pathological actions of ANG II, positively regulates telomerase activity (9). This suggests that an intimate relationship exists between the renin-angiotensin system and telomerase in the cardiovascular system. We demonstrate that increased TERT itself can counteract the negative effects of elevated ANG II on microvascular vasodilator capacity. Further studies are needed to further characterize TERT’s capacity to limit ANG II-induced pathological changes in the microcirculation. As both loss of TERT and elevations of ANG II are known to increase mitochondrial ROS production, a mechanistic connection on this level should be explored.
Study limitations.
There are several limitations that should be acknowledged. First, with the present experimental design, we cannot differentiate endothelial-specific effects of TERT or ANG II from smooth muscle or systemic effects. Second, telomere shortening may have contributed to the observed microvascular phenotype in first-generation TERT KO mice. Importantly, it has been previously shown that early-generation TERT KO mice have relatively conserved telomeres (24), rendering such a confounding effect unlikely.
In translating these findings, it will be important to consider the effects of upregulating telomerase in noncardiac diseases. For example, although not an oncogene, TERT is involved in support of tumor growth and metastasis (1). The risk versus benefit of TERT activation or inhibition needs to be carefully considered in different cell types. Current evidence indicates that the proliferative functions of TERT are driven by its canonical telomere nuclear lengthening effects (1). Separating mitochondrial and nuclear actions of telomerase would help advance further discovery in this field.
Conclusions.
This study demonstrates that loss of TERT but not TERC increases ROS formation and precipitates microvascular dysfunction. Decreased TERT augments, whereas overexpression of TERT prevents, ANG II-induced microvascular endothelial dysfunction. These data reveal a protective effect of TERT on microvascular function in vivo with potential implications for the treatment of cardiovascular diseases. Future directions involve exploring potential mechanisms whereby elevated TERT exerts protective effects on the microcirculation at baseline and in response to ANG II-induced microvascular stress. Subcellular localization of TERT to the mitochondria may reverse the negative long-term effects of heightened microvascular H2O2 on remodeling, inflammation, and other phenotypic changes associated with cardiovascular disease pathogenesis.
GRANTS
This work was supported by National Heart, Lung, and Blood Institute Grants R01-HL-133029 (to A. M. Beyer) and R01-HL-113612 (to D. D. Gutterman). K. Ait-Aissa is the recipient of American Heart Association Postdoctoral Fellowship 16POST26430075. A. O. Kadlec is a member of the Medical Scientist Training Program at Medical College of Wisconsin (MCW), which is partially supported by National Institute of General Medical Sciences Training Grant T32-GM-080202. This work was partially funded by the Advancing a Healthier Wisconsin Endowment through support of the MCW Redox Biology Program (to A. M. Beyer).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
K.A.-A., D.D.G., and A.M.B. conceived and designed research; K.A.-A., J.H., and A.M.B. performed experiments; K.A.-A. and A.M.B. analyzed data; K.A.-A., A.O.K., D.D.G., and A.M.B. interpreted results of experiments; K.A.-A., A.O.K., and A.M.B. prepared figures; K.A.-A. and A.O.K. drafted manuscript; A.O.K., D.D.G., and A.M.B. edited and revised manuscript; K.A.-A., A.O.K., J.H., D.D.G., and A.M.B. approved final version of manuscript.
ACKNOWLEDGMENTS
TERT Tg mice were obtained from Dr. Dennis C. Bruemmer. We thank David Zhang for assistance with septal artery isolation.
REFERENCES
- 1.Ait-Aissa K, Ebben JD, Kadlec AO, Beyer AM. Friend or foe? Telomerase as a pharmacological target in cancer and cardiovascular disease. Pharmacol Res 111: 422–433, 2016. doi: 10.1016/j.phrs.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyer AM, Freed JK, Durand MJ, Riedel M, Ait-Aissa K, Green P, Hockenberry JC, Morgan RG, Donato AJ, Peleg R, Gasparri M, Rokkas CK, Santos JH, Priel E, Gutterman DD. Critical role for telomerase in the mechanism of flow-mediated dilation in the human microcirculation. Circ Res 118: 856–866, 2016. doi: 10.1161/CIRCRESAHA.115.307918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beyer AM, Guo DF, Rahmouni K. Prolonged treatment with angiotensin 1–7 improves endothelial function in diet-induced obesity. J Hypertens 31: 730–738, 2013. doi: 10.1097/HJH.0b013e32835ecbe5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res 87: 840–844, 2000. doi: 10.1161/01.RES.87.10.840. [DOI] [PubMed] [Google Scholar]
- 5.Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 349: 1027–1035, 2003. doi: 10.1056/NEJMoa025050. [DOI] [PubMed] [Google Scholar]
- 6.Dai DF, Rabinovitch PS, Ungvari Z. Mitochondria and cardiovascular aging. Circ Res 110: 1109–1124, 2012. doi: 10.1161/CIRCRESAHA.111.246140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickinson BC, Chang CJ. A targetable fluorescent probe for imaging hydrogen peroxide in the mitochondria of living cells. J Am Chem Soc 130: 9638–9639, 2008. doi: 10.1021/ja802355u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dimitroulis D, Katsargyris A, Klonaris C, Avgerinos ED, Fragou-Plemenou M, Kouraklis G, Liapis CD. Telomerase expression on aortic wall endothelial cells is attenuated in abdominal aortic aneurysms compared to healthy nonaneurysmal aortas. J Vasc Surg 54: 1778–1783, 2011. doi: 10.1016/j.jvs.2011.06.079. [DOI] [PubMed] [Google Scholar]
- 9.Durand MJ, Zinkevich NS, Riedel M, Gutterman DD, Nasci VL, Salato VK, Hijjawi JB, Reuben CF, North PE, Beyer AM. Vascular actions of angiotensin 1–7 in the human microcirculation: novel role for telomerase. Arterioscler Thromb Vasc Biol 36: 1254–1262, 2016. doi: 10.1161/ATVBAHA.116.307518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gutterman DD, Chabowski DS, Kadlec AO, Durand MJ, Freed JK, Ait-Aissa K, Beyer AM. The human microcirculation: regulation of flow and beyond. Circ Res 118: 157–172, 2016. doi: 10.1161/CIRCRESAHA.115.305364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higashi Y, Maruhashi T, Noma K, Kihara Y. Oxidative stress and endothelial dysfunction: clinical evidence and therapeutic implications. Trends Cardiovasc Med 24: 165–169, 2014. doi: 10.1016/j.tcm.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Hsueh WA, Wyne K. Renin-angiotensin-aldosterone system in diabetes and hypertension. J Clin Hypertens (Greenwich) 13: 224–237, 2011. doi: 10.1111/j.1751-7176.2011.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Husain K, Hernandez W, Ansari RA, Ferder L. Inflammation, oxidative stress and renin angiotensin system in atherosclerosis. World J Biol Chem 6: 209–217, 2015. doi: 10.4331/wjbc.v6.i3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kadlec AO, Chabowski DS, Ait-Aissa K, Hockenberry JC, Otterson MF, Durand MJ, Freed JK, Beyer AM, Gutterman DD. PGC-1α (peroxisome proliferator-activated receptor γ coactivator 1-α) overexpression in coronary artery disease recruits NO and hydrogen peroxide during flow-mediated dilation and protects against increased intraluminal pressure. Hypertension 70: 166–173, 2017. doi: 10.1161/HYPERTENSIONAHA.117.09289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawada N, Imai E, Karber A, Welch WJ, Wilcox CS. A mouse model of angiotensin II slow pressor response: role of oxidative stress. J Am Soc Nephrol 13: 2860–2868, 2002. doi: 10.1097/01.ASN.0000035087.11758.ED. [DOI] [PubMed] [Google Scholar]
- 16.Kuo L, Chilian WM, Davis MJ. Interaction of pressure- and flow-induced responses in porcine coronary resistance vessels. Am J Physiol Heart Circ Physiol 261: H1706–H1715, 1991. doi: 10.1152/ajpheart.1991.261.6.H1706. [DOI] [PubMed] [Google Scholar]
- 17.Kuo L, Davis MJ, Cannon MS, Chilian WM. Pathophysiological consequences of atherosclerosis extend into the coronary microcirculation. Restoration of endothelium-dependent responses by l-arginine. Circ Res 70: 465–476, 1992. doi: 10.1161/01.RES.70.3.465. [DOI] [PubMed] [Google Scholar]
- 18.Kuo L, Hein TW. Vasomotor regulation of coronary microcirculation by oxidative stress: role of arginase. Front Immunol 4: 237, 2013. doi: 10.3389/fimmu.2013.00237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larsen BT, Bubolz AH, Mendoza SA, Pritchard KA Jr, Gutterman DD. Bradykinin-induced dilation of human coronary arterioles requires NADPH oxidase-derived reactive oxygen species. Arterioscler Thromb Vasc Biol 29: 739–745, 2009. doi: 10.1161/ATVBAHA.108.169367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, Zhao H, Li H, Kalyanaraman B, Nicolosi AC, Gutterman DD. Mitochondrial sources of H2O2 generation play a key role in flow-mediated dilation in human coronary resistance arteries. Circ Res 93: 573–580, 2003. doi: 10.1161/01.RES.0000091261.19387.AE. [DOI] [PubMed] [Google Scholar]
- 21.Miura H, Bosnjak JJ, Ning G, Saito T, Miura M, Gutterman DD. Role for hydrogen peroxide in flow-induced dilation of human coronary arterioles. Circ Res 92: e31–e40, 2003. doi: 10.1161/01.RES.0000054200.44505.AB. [DOI] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; Writing Group Members; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 133: e38–e360, 2016. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 23.Phillips SA, Bian JT, Church EC, Das EK, Vidovich M, Gutterman DD. Hydrogen peroxide prevents impaired endothelium-dependent dilation following acute exertion in chronic exercising but not in sedentary subjects (Abstract). Circulation 120, Suppl 18: S1013, 2009. [Google Scholar]
- 24.Sahin E, Colla S, Liesa M, Moslehi J, Müller FL, Guo M, Cooper M, Kotton D, Fabian AJ, Walkey C, Maser RS, Tonon G, Foerster F, Xiong R, Wang YA, Shukla SA, Jaskelioff M, Martin ES, Heffernan TP, Protopopov A, Ivanova E, Mahoney JE, Kost-Alimova M, Perry SR, Bronson R, Liao R, Mulligan R, Shirihai OS, Chin L, DePinho RA. Telomere dysfunction induces metabolic and mitochondrial compromise. Nature 470: 359–365, 2011. doi: 10.1038/nature09787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma NK, Reyes A, Green P, Caron MJ, Bonini MG, Gordon DM, Holt IJ, Santos JH. Human telomerase acts as a hTR-independent reverse transcriptase in mitochondria. Nucleic Acids Res 40: gkr758, 2011. doi: 10.1093/nar/gkr758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simon G, Abraham G, Cserep G. Pressor and subpressor angiotensin II administration. Two experimental models of hypertension. Am J Hypertens 8: 645–650, 1995. doi: 10.1016/0895-7061(95)00047-S. [DOI] [PubMed] [Google Scholar]
- 27.Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM; Microcirculatory Alterations in Resuscitation and Shock Investigators . Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med 49: 88–98.e2, 2007. doi: 10.1016/j.annemergmed.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 28.van de Hoef TP, van Lavieren MA, Damman P, Delewi R, Piek MA, Chamuleau SA, Voskuil M, Henriques JP, Koch KT, de Winter RJ, Spaan JA, Siebes M, Tijssen JG, Meuwissen M, Piek JJ. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv 7: 301–311, 2014. doi: 10.1161/CIRCINTERVENTIONS.113.001049. [DOI] [PubMed] [Google Scholar]
- 29.Yu MA, Sánchez-Lozada LG, Johnson RJ, Kang DH. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens 28: 1234–1242, 2010. doi: 10.1097/HJH.0b013e328337da1d. [DOI] [PubMed] [Google Scholar]