Abstract
Objective
To describe a novel technique using preoperative computed tomography (CT) to plan clamp tine placement along the trans-syndesmotic axis (TSA). We hypothesized that preoperative CT imaging provides a reliable template on which to plan optimal clamp tine positioning along the TSA, reducing malreduction rates compared with other described techniques.
Methods
CT images of 48 cadaveric through-knee specimens were obtained and the TSA was measured as well as the optimal position of the medial clamp tine. The syndesmosis was then fully destabilized. Indirect clamp reductions were performed with the medial clamp tine placed at positions 10° anterior to the TSA, along the TSA, and at both 10° and 20° posterior to the TSA. The specimens were then separately reduced using manual digital pressure and palpation alone. CT was performed after each clamp and manual reduction.
Results
On average, reduction clamp tines were within 3±2° of the desired angle and within 5±4% of the templated location along the tibial line for all clamp reduction attempts. Palpation and direct visualization produced the overall lowest malreduction rates in all measurements: 4.9% and 3.0%, respectively. Off-axis clamping 10° anterior or 20° posterior to the patient-specific TSA demonstrated an increased overall malreduction rate: 15.8% and 11.3%, respectively. Significantly more over-compression occurred when a reduction clamp was utilized versus manual digital reduction alone (8.6% vs 0%).
Conclusions
Reduction clamp placement directly along an optimal clamping vector can be facilitated by preoperative CT measurements of the uninjured ankle. However, even in this setting, the use of reduction clamps increases the risk for syndesmotic malreduction and over-compression compared with manual digital reduction or direct visualization.
Introduction
Injuries to the ankle syndesmosis are common in operatively treated ankle fractures. Despite a variety of reduction and fixation techniques, malreductions persist at high rates across the literature, ranging from 16 to 52%.1–6 Two-dimensional radiographic assessment of the fibular position within the incisura is less sensitive than advanced imaging for detecting both linear and rotational malreductions, a difficulty which has been cited as a contributing factor to syndesmotic malreductions.2,7–10 Multiple studies have demonstrated that malreductions are associated with poorer clinical outcomes.3,11–15
Indirect syndesmotic reduction with clamps may lead to malreduction when an off-axis clamping vector is used.16–19 However, anatomic variation of the syndesmosis makes it challenging to position reduction clamps within an ideal range for each individual’s morphology.8,20–22 Moreover, variable incisural morphology may predispose a patient to translation or malrotation of the fibula during reduction.23 Other reduction techniques, including open visualization and direct palpation of the syndesmosis,3,24 as well as the use of computed tomography (CT)1,2,25 and computer navigation techniques26 have evolved in an attempt to overcome the challenges associated with indirect reduction with percutaneous clamping. However, none of these techniques have demonstrated superiority and may represent significant cost implications and logistical challenges with routine use.
There were several aspects to this study. Could the preoperative CT imaging of the contralateral, uninjured ankle be used as a method to determine the native position of the fibula? Would this information serve as a template for the accurate placement of reduction clamp tines intraoperatively on the injured extremity? We also sought to evaluate the specific tolerance of the syndesmotic reduction to off-axis clamping relative to a patient’s specific trans-syndesmotic axis (TSA). Lastly, we aimed to compare the malreduction rates of this method versus the use of direct visualization or palpation to assess reduction quality.
With this data, we wanted to answer several questions. Our first hypothesis was that preoperative CT imaging of the uninjured ankle provided a reliable template for planning of optimal tine positioning, relative to the patient-specific TSA. Our second hypothesis was that clamp positions beyond 10° anterior or posterior to the TSA would lead to increased malreductions. Our final hypothesis was that reproducible and accurate positioning of the reduction clamp tines according to the preoperative template would ultimately lower malreduction rates relative to other reduction techniques.
Methods
Pre-Operative CT Templating
Twenty-four paired (48 total) cadaveric through-knee specimens with intact proximal tibiofibular joints were imaged using CT with the ankle at neutral dorsiflexion. Standardized measurements as described by Nault et. al were utilized to describe the native spatial relationship of the fibula within the incisura (Figure 1).20 Using imaging processing software, OsiriX (open-source software; www.osirixviewer.com), localizer lines were utilized to manipulate both the coronal and axial imaging planes so as to reproduce the plane of a true talar dome lateral. In a step-wise fashion, these CT manipulations recreate the rotational (Figure 2-A) and translational (Figure 2-B) adjustments of the ankle relative to the fluoroscopy machine that are typically required to obtain a perfect talar dome lateral intraoperatively. The plane upon which the superior, medial and lateral talar domes would be superimposed on two-dimensional imaging was then established as the plane of the talar dome lateral on the axial CT. This plane then serves as a reference from which all other measurements were generated. At a level 1cm above the tibial plafond, the TSA angle, defined on the axial CT as the angle between the plane of the a true talar-dome lateral and a line perpendicular to the tangent of the anterior and poster borders of the fibular incisura, was recorded as previously described (Figure 2-C).27 The apex of the TSA was then positioned on the lateral fibular ridge and extended towards the medial tibial cortex, simulating the positions of the lateral and medial clamp tines, respectively. The projected location of the medial clamp tine along the TSA was then recorded as a percentage of the distance from the anterior tibial cortex along the “tibial line”, defined as the distance between the anterior to posterior cortices of the tibia. In addition to the TSA, medial clamp tine positions 10° anterior, 10° and 20° posterior to the TSA were recorded, also as a percentage along the tibial line. These locations along the tibial line were then transposed to their corresponding positions on a true talar-dome lateral using plain radiography (Figure 2-D).
Figure 1.
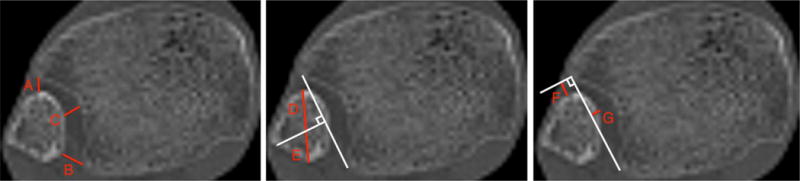
Axial CT view of an intact syndesmosis 1cm above the tibial plafond with measurements (A-G) of fibular position relative to the incisura as originally described by Nault et al.20
Figure 2.
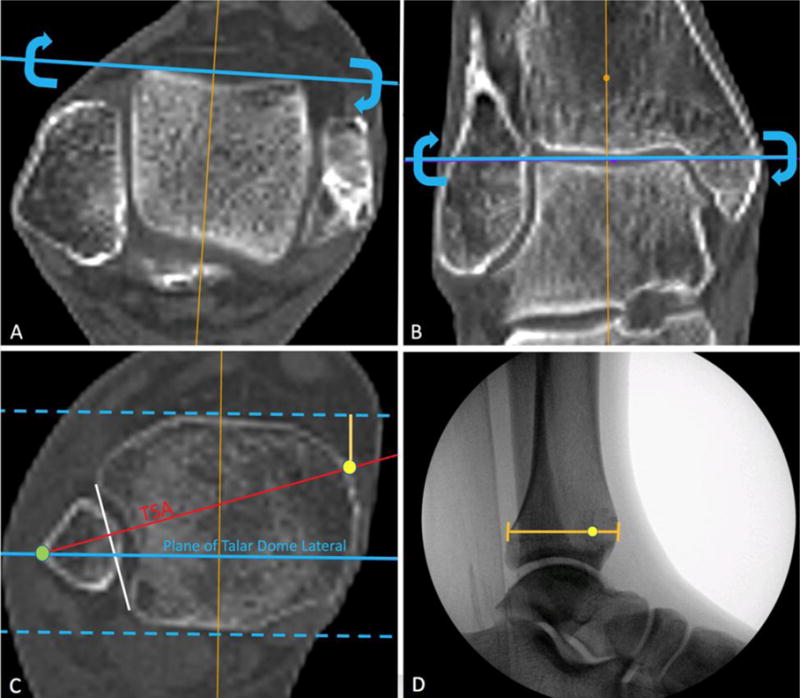
A. Adjustment of axial CT at the level of the talus such that the localizer line runs tangential to the talar dome. Correction in this plane is equivalent to internal or external rotatory adjustments when obtaining a true talar dome lateral using fluoroscopy. B. Adjustment of coronal CT images such that the localizer line runs tangential to the superior talar dome. Correction in this plane is equivalent to abducting or adducting the lower extremity in the plane of the fluoroscopy machine to eliminate the projection of talar dome double densities. C. Blue dotted lines: Anterior and Posterior cortices as visualized in the lateral projection. Red line: The trans-syndesmotic axis (TSA) which runs perpendicular to a line (white) that is tangential to both the anterior and posterior borders of the incisura. Yellow dot: Templated position of the medial clamp tine Green dot: Templated position of the lateral clamp tine D. True talar dome lateral image with the corresponding location of the yellow dot representing the templated position of the medial clamp tine along the TSA.
Specimen Preparation and Syndesmotic Reduction
The syndesmosis was then destabilized according to an established protocol, as described by Phisitkul, et al.,16 which included sequential soft tissue transections of the anterior and posterior inferior tibiofibular ligaments, syndesmosis and distal 10cm of the interosseous membrane, and the deltoid ligament. Stress imaging using fluoroscopy was performed to confirm the gross instability of the syndesmosis after destabilization was complete. Using direct measurement with a ruler, the tibial line was marked as a reference 1cm above the tibial plafond. For consistency, this measurement was derived from the nadir of the anterior plafond, using the same technique as the distance was recorded on CT. Then, a true talar dome lateral was obtained using fluoroscopy and the four templated locations were each separately identified by positioning a freer at the appropriate distance along the tibial line and marked with indelible ink. Subsequently, 2mm unicortical stainless steel screws were placed into the medial distal tibia at each of the four marked positions. A screw was also placed directly on the lateral fibular ridge. Reduction clamp tines were then separately placed on the screw heads at positions 10° anterior to the TSA, along the TSA, and at both 10° and 20° posterior to the TSA. CT imaging was then performed with the reduction clamp in each position. Indirect reduction at all positions was performed by a single observer with experience in generating approximately 130 N/m of force with reduction forceps in an effort to standardize the reduction force magnitude.28 The indirect reduction at each location was performed such that the syndesmosis was not exposed to the observer for visual inspection, nor was there an attempt at radiographic reduction assessment prior to the CT being performed at the specified clamped location. After the specimen was imaged at each clamping position, the screws were removed and the unstable syndesmosis was then reduced using the surgeon’s thumb alone as manual digital pressure, while simultaneously palpating the anterior tibiofibular relationship for congruency. Compressive force generated by the thumb was deemed sufficient when there was no palpable step or gap between the tibia and fibula. The position of the fibula was adjusted manually so as to reestablish the anterior tibiofibular line, described as a straight extension from the anterolateral fibular surface to the anterior tubercle of the incisura.29,30 A surgical towel was utilized to cover the anterior tibiofibular relationship to ensure palpation alone was used to assess reduction quality. Lastly, reduction was performed utilizing manual digital pressure with direct visualization of the anterior tibiofibular relationship to assess reduction. These two additional reduction attempts were stabilized with a 0.045 inch Kirschner wire to secure the fibula in the desired position.
Post-Reduction Analysis
A malreduction on CT analysis was defined as a change of >2mm between the native (intact) syndesmotic measurements and those after syndesmotic disruption and reduction with each technique. All reduction measurements were performed by a single author who was experienced with this technique. Specimens were also assessed for the differences between the desired and actual clamping vectors, based off the intended position of the medial clamp tine along the tibial line.
Statistics
Standard descriptive statistics for means and standard deviations for continuous measures and percentages for categorical measures were used to summarize basic measurement data. Interclass coefficient correlations (ICC) were used to assess reliabilities. All CT scans from a single observer were measured twice, at a time point a minimum of 2 weeks after the initial measurement, to calculate the intraobserver reliability. The sample size for 2 observers was determined using a power of 0.9 with a good agreement as an ICC over 0.6. Outcome measures for categorical variables of reduction were assessed with chi-squared tests. All data was analyzed using SPSS (IBM, Chicago, IL).
Source of Funding
This study was made possible through the Orthopaedic Research and Education Foundation Resident Clinician-Scientist Training grant.
Results
Of the 24 paired cadaveric specimens, 10 were from male donors and 14 were from female donors, with an average age of death of 82 years. CT imaging of intact specimens demonstrated a consistent anterior position of the medial extent of the TSA angle along the tibial line. On average, the TSA angle as measured on CT was 22±3° from the plane of the talar dome lateral, and the resulting medial clamp tine position along the tibial line averaged 19±9%. The 10° anterior, 10° and 20° posterior off-axis positions of the medial clamp tine were 4±3%, 41±8% and 66±9%, respectively along the tibial line. When comparing between paired specimens, the average TSA angle difference was 3±2°, and the average difference in the resulting medial tine position was 5±5% along the tibial line.
The CT manipulation and measurement technique to obtain the position of the clamp tines along the TSA was highly consistent. The intraobserver reliability was recorded with an ICC of 0.979 for measuring the TSA angle and an ICC of 0.980 for the medial clamp tine position along the tibial line. Interobserver reliability was also excellent with an ICC of 0.918 for the TSA angle and 0.906 for the medial clamp tine position along the tibial line. Analysis of our intraoperative clamp positioning demonstrated that the overall average angle difference between the templated and actual reduction clamp angle was 3±2°. The overall average difference in reference to the percentage variation along the tibial line between the templated and actual medial clamp tine position was 5±4%.
Palpation and direct visualization without the use of reduction clamps produced the overall lowest malreduction rates in all measurements: 4.9% and 3.0%, respectively. When reduction clamps were used, the overall average malreduction rate was lowest in the 10° posterior (6%) and TSA (9.8%) clamping groups, followed by the 20° posterior (11.3%) groups and 10° anterior (15.8%). Off-axis clamping of 10°anterior or 20° posterior to the patient-specific TSA demonstrated an increased overall malreduction rate (p = 0.02) (Figure 3). There was a significant difference in over-compression for all specimens where a reduction clamp was utilized (8.6%), as compared to the groups where manual digital reduction was performed alone (0%, p = 0.003).
Figure 3.
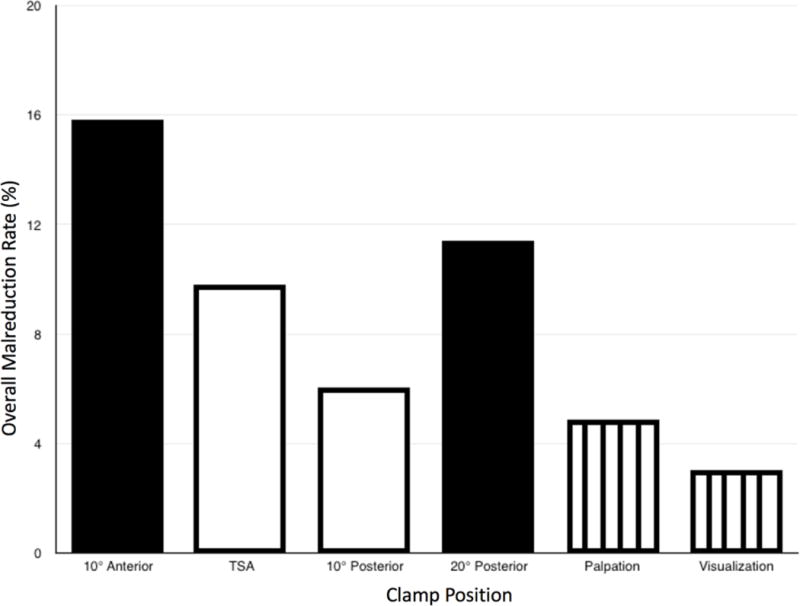
Overall malreduction rates versus clamp positioning relative to the TSA angle. The highest malreduction rates occurred when the medial clamp tine was placed 10 degrees anterior, or 20 degrees posterior to the TSA. Lowest malreduction rates were seen in the palpation and direct visualization techniques.
Discussion
Controversy exists in the recent literature regarding optimal methods to obtain, and fixation techniques to maintain, an appropriate reduction of the ankle syndesmosis. High rates of syndesmotic malreduction are prevalent even with increased awareness of these technical considerations.1–6 Syndesmotic malreductions have been associated with worse functional outcomes in several studies,3,11–15 although the threshold of this association has been called into question.31,32 Indirect reduction of syndesmotic injuries with reduction clamps has been a historic standard. However, a high degree of anatomic variability of the syndesmosis makes it challenging to optimize the clamp vector that is applied.8,20–22 Our study demonstrates that preoperative contralateral CT imaging is a viable technique to both template and position the desired location of the medial clamp tine to achieve an optimal clamping vector. However, this novel reduction planning technique was still outperformed by more direct approaches. Moreover, we found a significant amount of over-compression in all clamping groups compared with those where syndesmotic diastasis was reduced by manual digital pressure alone.
Use of intraoperative CT imaging to assess and potentially revise malreductions is cost prohibitive and is not available to many surgeons who may treat this injury.1,2,25 However, standard CT imaging, if done preoperatively, is widely available and not as cost-prohibitive. Prior studies have established anatomic consistency bilaterally for a given individual.20–22,33–35 This finding was consistent in this study as the average TSA angle and resulting medial tine position along the tibial line were similar between specimens. Therefore, the contralateral, uninjured side may be used as a reliable template to establish a desired clamping vector during preoperative planning. The utility of this approach to syndesmotic reduction is dependent upon the reproducibility of the preoperative CT measurements and the accuracy of clamp tine placement along the templated vector intraoperatively. The intra- and interobserver reliability for this novel series of measurements was determined to be highly agreeable. In addition to the reproducibility of the CT measurements, this study found that there was sufficient accuracy of clamp placement intraoperatively relative to the templated location.
Although prior studies have analyzed the relationship between off-axis clamping and syndesmotic malreduction,16–19 this is the first study to assess clamping vectors relative to an individual’s specific anatomy and trans-syndesmotic axis. Whereas classically, syndesmotic screws are placed at 30° from the coronal plane,36 defining a universal ideal clamping vector is challenging due to this high degree of anatomic variation of the fibular position within the incisura and the morphology of the incisura itself. In this series, the average TSA angle and the resulting medial clamp tine position along the tibial line were similar to a previous study using CT imaging software to simulate clamp tine placement.27
When reduction clamps were used, the overall average malreduction rate was lowest in the TSA and 10° posterior clamping groups. Off-axis clamping of 10°anterior or 20° posterior to the patient-specific TSA demonstrated an increased overall malreduction rate. This data may help define a “safe zone” where clamping vectors along or slightly posterior to the TSA may reduce the risk of malreductions. This area corresponded to an average range of positions between 18% and 41% along the tibial line. This is consistent with a prior study, where the optimal position of the medial clamp tine was defined along a centroidal axis that resulted in a simulated safe medial clamping position anterior to the midline.19
However, when the syndesmosis is widely displaced, even perfect position of the clamp tines according to the preoperative plan may result in an off-axis clamp vector if the fibular ridge is translated in the anteroposterior plane to a large degree. In vivo, there is typically more anteroposterior than lateral syndesmotic instability,37 highlighting the clinical relevance as it pertains to off-axis clamping vectors. Despite this optimized clamping technique using advanced imaging, palpation and direct visualization produced the overall lowest malreduction rates in all measurements. Other literature reports these techniques as having improved malreduction rates over indirect reduction with clamping.3,24 Therefore, the routine use of pre-operative or intra-operative CT imaging specifically for clamp vector placement is neither warranted nor cost-effective. Although not utilized in this study, more anterior and distal visualization of talofibular articular congruency is another accepted approach for visualizing syndesmotic reduction.38
Overcompression of the syndesmosis has been demonstrated in multiple cadaveric studies,16,39,40 as well as in vivo.41 This is facilitated by the large mechanical advantage produced by the reduction forceps, especially when larger pelvic reduction forceps are utilized. Despite meticulous clamping technique, this study demonstrated a significant difference in over-compression for all specimens where a reduction clamp was utilized. Importantly, there was no evidence of any under-compression in the specimens that underwent manual digital reduction. Prior literature suggested that over-compression is not possible in the setting of a reduced fibula and dorsiflexed ankle; this has likely perpetuated the false notion of safety when forcefully clamping across the syndesmotic axis.42 Due to the dynamic movement of the distal tibiofibular articulation with ankle range of motion,43 overcompression may carry significant clinical implications. In our study, manual digital pressure was sufficient to provide the appropriate amount of force to overcome syndesmotic instability without demonstrating any degree of overcompression. Lastly, the additional advantage of using manual digital reduction is that the surgeon has enhanced tactile feedback for detecting subtle incongruencies of the distal tibiofibular articulation. The use of reduction forceps does not provide this same tactile feedback and may more easily produce a gross malreduction that goes undetected.
Previous studies by the senior author (MJG) have sought to promote the safe use of reduction clamps to generate an indirect reduction, by optimizing both proper clamp tine positioning44 and reduction force.28 Despite the conclusions in this study, some surgeons will still choose to avoid opening the syndesmosis routinely and are more comfortable with an indirect reduction technique. Additionally, other scenarios (e.g. compromised soft tissues) may make open reduction with direct exposure undesirable. In these circumstances, the preoperative CT-templating technique demonstrated in this study could be a useful approach. Our evolving advocacy of an open reduction under direct vision is with the acknowledgment that there are still many surgeon and patient-specific scenarios where it is useful to have alternative, reproducible techniques for optimizing reduction via an indirect approach.
This study does have some notable shortcomings. Although the method of syndesmotic disruption is one that has been standardized in prior cadaveric studies, this model may not exactly replicate the degree of disruption seen in vivo. The high degree of instability of the syndesmosis produced in this model may inherently render clamping techniques less reliable due to the extent of gross anteroposterior translation of the fibula and potential resultant change in the clamping vector, however this would be a way to show the most damage indirect clamp reduction can cause. Lesser degrees of syndesmotic instability may be more amenable to this CT clamping strategy as the lateral fibular ridge would be in a more consistent location to provide the correct vector. Another weakness of this study is the lack of standardization of the clamp force. We attempted to reduce bias by training a single author to detect a clamp force of approximately 130 N/m by subjective tactile feel alone. The lack of a digital tensiometer on the reduction clamps is an important shortcoming of this study. Lastly, the trans-syndesmotic axis itself may not perfectly define the most optimal clamping vector in all specimens. The eccentricity of the fibula within the incisura could render the TSA, as a perpendicular line to the anterior and posterior tubercles of the incisura, a vector that may not completely account for an eccentric position in the intact state.
Conclusions
Preoperative CT measurements of the uninjured ankle may be utilized to reproducibly plan and achieve an optimal clamping vector for an individual patient’s native anatomy. However, despite the use of this advanced imaging technique, the use of reduction clamps increases the risk for syndesmotic malreduction and over-compression compared with manual digital reduction or direct visualization. This study adds to the increasing evidence that routine use of percutaneously applied reduction clamps may lead to an increased number of syndesmotic malreductions and should be replaced by direct visualization or palpation of the syndesmosis with manual digital reduction.
Acknowledgments
The authors wish to thank Abigail B. Cosgrove for her assistance in editing the initial manuscript.
Conflicts of Interest and Source of Funding:
Anna N. Miller: AAOS: Board or committee member; American College of Surgeons: Board or committee member; AONA: Other financial or material support; AOTrauma North America: Board or committee; member; Journal of Orthopaedic Trauma: Editorial or governing board; Orthopaedic Trauma Association: Board or committee member
William Ricci: Cable Fix LLC: Other financial or material support; Journal of Bone and Joint Surgery – American: Publishing royalties, financial or material support; Journal of Orthopaedic Trauma: Editorial or governing board; McGinley Orthopaedics: Other financial or material support; MicroPort: IP royalties; OKU Trauma/AAOS: Editorial or governing board; Orthopaedic Trauma Association: Board or committee member; Rockwood & Green Fracture in Adults/Wolters Kluwer Health – Lippincott Williams & Wilkins: Editorial or governing board; Smith & Nephew: IP royalties; Paid consultant; Research support; Synthes: Research support; Wolters Kluwer Health – Lippincott Williams & Wilkins: Publishing royalties, financial or material support; Zimmer-Biomet: Paid consultant
Christopher McAndrew: Journal of Bone and Joint Surgery – American: Publishing royalties, financial or material support; Synthes: Paid presenter or speaker
Michael Gardner: BoneSupport AB: Paid consultant; Current Opinion in Orthopaedics: Editorial or governing board; Journal of Bone and Joint Surgery – American: Publishing royalties, financial or material support; KCI: Paid consultant; Orthopaedic Trauma Association: Board or committee member; Pacira Pharmaceuticals: Paid consultant; Stryker: Paid consultant; Synthes: Paid consultant; Research support; Wolters Kluwer Health – Lippincott Williams & Wilkins: Publishing royalties, financial or material support
The other authors (Cosgrove, Spraggs-Hughes, Putnam) have no disclosures.
This publication was aided by a grant from the Orthopaedic Research and Education Foundation with funding provided by Thomas S. Sculco, MD.
References
- 1.Franke J, Recum von J, Suda AJ, Grützner PA, Wendl K. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am. 2012;94(15):1386–1390. doi: 10.2106/JBJS.K.01122. [DOI] [PubMed] [Google Scholar]
- 2.Davidovitch RI, Weil Y, Karia R, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg Am. 2013;95(20):1838–1843. doi: 10.2106/JBJS.L.00382. [DOI] [PubMed] [Google Scholar]
- 3.Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26(7):439–443. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 4.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the Tibiofibular Syndesmosis in Ankle Fractures. Foot Ankle Int. 2006;27(10):788–792. doi: 10.1177/107110070602701005. [DOI] [PubMed] [Google Scholar]
- 5.Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40(12):2828–2835. doi: 10.1177/0363546512461480. [DOI] [PubMed] [Google Scholar]
- 6.Wikerøy AKB, Høiness PR, Andreassen GS, Hellund JC, Madsen JE. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. 2010;24(1):17–23. doi: 10.1097/BOT.0b013e3181bedca1. [DOI] [PubMed] [Google Scholar]
- 7.Koenig SJ, Tornetta P, Merlin G, et al. Can We Tell if the Syndesmosis is Reduced Using Fluoroscopy? J Orthop Trauma. 2015;29(9):1–e330. doi: 10.1097/BOT.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 8.Beumer A, van Hemert WLW, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;(423):227–234. doi: 10.1097/01.blo.0000129152.81015.ad. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Lu J, Yang H, Mekhail AO, Yeasting RA. Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot Ankle Int. 1997;18(11):693–698. doi: 10.1177/107110079701801103. [DOI] [PubMed] [Google Scholar]
- 10.Pneumaticos SG, Noble PC, Chatziioannou SN, Trevino SG. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int. 2002;23(2):107–111. doi: 10.1177/107110070202300205. [DOI] [PubMed] [Google Scholar]
- 11.Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Koval KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma. 2010;24(1):7–11. doi: 10.1097/BOT.0b013e3181b1542c. [DOI] [PubMed] [Google Scholar]
- 12.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19(2):102–108. doi: 10.1097/00005131-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Bauer M, Jonsson K, Nilsson B. Thirty-year follow-up of ankle fractures. Acta Orthop Scand. 1985;56(2):103–106. doi: 10.3109/17453678508994329. [DOI] [PubMed] [Google Scholar]
- 14.Tunturi T, Kemppainen K, Pätiälä H, Suokas M, Tamminen O, Rokkanen P. Importance of anatomical reduction for subjective recovery after ankle fracture. Acta Orthop Scand. 1983;54(4):641–647. doi: 10.3109/17453678308992903. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy JG, Soffe KE, Dalla Vedova P, et al. Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma. 2000;14(5):359–366. doi: 10.1097/00005131-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Phisitkul P, Ebinger T, Goetz J, Vaseenon T, Marsh JL. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg Am. 2012;94(24):2256–2261. doi: 10.2106/JBJS.K.01726. [DOI] [PubMed] [Google Scholar]
- 17.Miller AN, Barei DP, Iaquinto JM, Ledoux WR, Beingessner DM. Iatrogenic Syndesmosis Malreduction via Clamp and Screw Placement. J Orthop Trauma. 2013;27(2):100–106. doi: 10.1097/BOT.0b013e31825197cb. [DOI] [PubMed] [Google Scholar]
- 18.Nimick CJ, Collman DR, Lagaay P. Fixation orientation in ankle fractures with syndesmosis injury. J Foot Ankle Surg. 2013;52(3):315–318. doi: 10.1053/j.jfas.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy MT, Carmody O, Leong S, Kennedy C, Dolan M. A computed tomography evaluation of two hundred normal ankles, to ascertain what anatomical landmarks to use when compressing or placing an ankle syndesmosis screw. Foot (Edinb) 2014;24(4):157–160. doi: 10.1016/j.foot.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Nault M-L, Hébert-Davies J, Laflamme G-Y, Leduc S. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. 2013;27(11):638–641. doi: 10.1097/BOT.0b013e318284785a. [DOI] [PubMed] [Google Scholar]
- 21.Dikos GD, Heisler J, Choplin RH, Weber TG. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma. 2012;26(7):433–438. doi: 10.1097/BOT.0b013e3182535f30. [DOI] [PubMed] [Google Scholar]
- 22.Lepojärvi S, Pakarinen H, Savola O, Haapea M, Sequeiros RB, Niinimäki J. Posterior translation of the fibula may indicate malreduction: CT study of normal variation in uninjured ankles. J Orthop Trauma. 2014;28(4):205–209. doi: 10.1097/BOT.0b013e3182a59b3c. [DOI] [PubMed] [Google Scholar]
- 23.Cherney SM, Spraggs-Hughes AG, McAndrew CM, Ricci WM, Gardner MJ. Incisura Morphology as a Risk Factor for Syndesmotic Malreduction. Foot Ankle Int. 2016;37(7):748–754. doi: 10.1177/1071100716637709. [DOI] [PubMed] [Google Scholar]
- 24.Miller AN, Carroll EA, Parker RJ, Boraiah S, Helfet DL, Lorich DG. Direct Visualization for Syndesmotic Stabilization of Ankle Fractures. Foot Ankle Int. 2009;30(5):419–426. doi: 10.3113/FAI-2009-0419. [DOI] [PubMed] [Google Scholar]
- 25.Richter M, Zech S. Intraoperative 3-dimensional imaging in foot and ankle trauma-experience with a second-generation device (ARCADIS-3D) J Orthop Trauma. 2009;23(3):213–220. doi: 10.1097/BOT.0b013e31819867f6. [DOI] [PubMed] [Google Scholar]
- 26.Dubois-Ferrière V, Gamulin A, Chowdhary A, Fasel J, Stern R, Assal M. Syndesmosis reduction by computer-assisted orthopaedic surgery with navigation: Feasibility and accuracy in a cadaveric study. Injury. 2016;47(12):2694–2699. doi: 10.1016/j.injury.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 27.Putnam SM, Linn MS, Spraggs-Hughes A, McAndrew CM, Ricci WM, Gardner MJ. Simulating clamp placement across the trans-syndesmotic angle of the ankle to minimize malreduction: A radiological study. Injury. 2017 Jan; doi: 10.1016/j.injury.2017.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haynes J, Cherney S, Spraggs-Hughes A, McAndrew CM, Ricci WM, Gardner MJ. Increased Reduction Clamp Force Associated With Syndesmotic Overcompression. Foot Ankle Int. 2016;37(7):722–729. doi: 10.1177/1071100716634791. [DOI] [PubMed] [Google Scholar]
- 29.Reb CW, Hyer CF, Collins CL, Fidler CM, Watson BC, Berlet GC. Clinical Adaptation of the “Tibiofibular Line” for Intraoperative Evaluation of Open Syndesmosis Reduction Accuracy: A Cadaveric Study. Foot Ankle Int. 2016;37(11):1243–1248. doi: 10.1177/1071100716660822. [DOI] [PubMed] [Google Scholar]
- 30.Gifford PB, Lutz M. The Tibiofibular Line: An Anatomical Feature to Diagnose Syndesmosis Malposition. Foot Ankle Int. 2014;35(11):1181–1186. doi: 10.1177/1071100714546187. [DOI] [PubMed] [Google Scholar]
- 31.Warner SJ, Fabricant PD, Garner MR, Schottel PC, Helfet DL, Lorich DG. The Measurement and Clinical Importance of Syndesmotic Reduction After Operative Fixation of Rotational Ankle Fractures. J Bone Joint Surg Am. 2015;97(23):1935–1944. doi: 10.2106/JBJS.O.00016. [DOI] [PubMed] [Google Scholar]
- 32.Laflamme M, Belzile EL, Bédard L, van den Bekerom MPJ, Glazebrook M, Pelet S. A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J Orthop Trauma. 2014;29(5):1–223. doi: 10.1097/BOT.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 33.Mukhopadhyay S, Metcalfe A, Guha AR, et al. Malreduction of syndesmosis–are we considering the anatomical variation? Injury. 2011;42(10):1073–1076. doi: 10.1016/j.injury.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 34.Elgafy H, Semaan HB, Blessinger B, Wassef A, Ebraheim NA. Computed tomography of normal distal tibiofibular syndesmosis. Skeletal Radiol. 2010;39(6):559–564. doi: 10.1007/s00256-009-0809-4. [DOI] [PubMed] [Google Scholar]
- 35.Shah AS, Kadakia AR, Tan GJ, Karadsheh MS, Wolter TD, Sabb B. Radiographic evaluation of the normal distal tibiofibular syndesmosis. Foot Ankle Int. 2012;33(10):870–876. doi: 10.3113/FAI.2012.0870. [DOI] [PubMed] [Google Scholar]
- 36.Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15(6):330–339. doi: 10.5435/00124635-200706000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Candal-Couto JJ, Burrow D, Bromage S, Briggs PJ. Instability of the tibio-fibular syndesmosis: have we been pulling in the wrong direction? Injury. 2004;35(8):814–818. doi: 10.1016/j.injury.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 38.Shah AR, Tornetta P, Veltre D, Yakavonis M. Reducing the Syndesmosis Under Direct Vision: Where Should I Look? San Diego, CA: 2017. [DOI] [PubMed] [Google Scholar]
- 39.Schon JM, Mikula JD, Backus JD, et al. 3D Model Analysis of Ankle Flexion on Anatomic Reduction of a Syndesmotic Injury. Foot Ankle Int. 2016;38(4):436–442. doi: 10.1177/1071100716681605. [DOI] [PubMed] [Google Scholar]
- 40.Morellato J, Louati H, Bodrogi A, et al. The Effect of Varying Tension of a Suture Button Construct in Fixation of the Tibiofibular Syndesmosis-Evaluation Using Stress Computed Tomography. J Orthop Trauma. 2017;31(2):103–110. doi: 10.1097/BOT.0000000000000737. [DOI] [PubMed] [Google Scholar]
- 41.Cherney SM, Haynes JA, Spraggs-Hughes AG, McAndrew CM, Ricci WM, Gardner MJ. In Vivo Syndesmotic Overcompression After Fixation of Ankle Fractures With a Syndesmotic Injury. J Orthop Trauma. 2015;29(9):414–419. doi: 10.1097/BOT.0000000000000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tornetta P, Spoo JE, Reynolds FA, Lee C. Overtightening of the ankle syndesmosis: is it really possible? The Journal of Bone & Joint Surgery. 2001;83-A(4):489–492. doi: 10.2106/00004623-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Nault M-L, Marien M, Hébert-Davies J, et al. MRI Quantification of the Impact of Ankle Position on Syndesmosis Anatomy. Foot Ankle Int. 2017;38(2):215–219. doi: 10.1177/1071100716674309. [DOI] [PubMed] [Google Scholar]
- 44.Cosgrove CT, Putnam SM, Cherney SM, Ricci WM, Spraggs-Hughes AG, McAndrew CM, Gardner MJ. Medial Clamp Tine Positioning Affects Ankle Syndesmosis Malreduction. J Orthop Trauma. 2017 Apr;:1. doi: 10.1097/BOT.0000000000000882. [DOI] [PMC free article] [PubMed] [Google Scholar]


