Abstract
Background
The patterns of comorbidity among mental disorders have led researchers to model the underlying structure of psychopathology. While studies have suggested a structure including internalizing and externalizing disorders, less is known with regard to the cross-national stability of this model. Moreover, little data is available on the placement of eating disorders, bipolar disorder and psychotic experiences in this structure.
Methods
We evaluated the structure of mental disorders with data from the World Health Organization Composite International Diagnostic Interview, including 15 lifetime mental disorders and six psychotic experiences. Respondents (n=5,478–15,499) were included from 10 high, middle and lower-middle income countries across the world aged 18 years or older. Confirmatory Factor Analyses (CFA) were used to evaluate and compare the fit of different factor structures to the lifetime disorder data. measurement invariance was evaluated with multigroup CFA (MG-CFA).
Results
A second-order model with internalizing and externalizing factors and fear and distress subfactors best described the structure of common mental disorders. MG-CFA showed that this model was stable across countries. Of the uncommon disorders, bipolar disorder and eating disorder were best grouped with the internalizing factor, and psychotic experiences with a separate factor.
Conclusions
These results indicate that cross-national patterns of lifetime common mental-disorder comorbidity can be explained with a second-order underlying structure that is stable across countries and can be extended to also cover less common mental disorders.
Introduction
Co-morbidity among mental disorders is common (e.g., Kessler et al., 1994; Bijl et al., 1998; Hasin & Kilcoyne, 2012; Teesson et al., 2009) and has been hypothesized to reflect the latent general structure of psychopathology (Sher & Trull, 1996; Mineka et al., 1998; Widiger & Clark, 2000; Carragher et al., 2015). Much scientific work has focused on gaining a better understanding of this ‘meta structure’ of mental disorders (e.g., Mineka et al., 1998; Krueger & Markon, 2006; Carragher et al., 2015; Eaton et al., 2015; Kotov et al., 2017) and has shown that the structure of common mental disorders can be explained by two broad underlying domains: internalizing and externalizing (Krueger et al., 1998; Krueger 1999; Krueger & Markon, 2006). Depressive disorders and anxiety disorders load on the internalizing factor and conduct disorder (CD), substance-related disorders and antisocial problems load on the externalizing factor.
The existence of separate, but correlated, internalizing and externalizing domains has been confirmed repeatedly in empirical studies. However, the structure is likely to be more complex and multiple underlying sub-domains are likely to exist. For instance, the internalizing domain has been consistently shown to have at least two lower-order subfactors that explain the more specific clustering of, respectively, ‘fear’ (panic disorder, agoraphobia, specific phobia, social phobia, and obsessive compulsive disorder [OCD]) and ‘distress’ disorders (major depressive episode [MDE], dysthymia, generalized anxiety disorder [GAD] and post-traumatic stress disorder [PTSD] e.g., Krueger et al., 1998; Krueger 1999; Vollebergh et al., 2001; Watson, 2005; Slade & Watson, 2006; Krueger & Markon, 2006; Miller et al., 2011; Eaton et al., 2013a; Kotov et al., 2017). For externalizing disorders, subfactors have been found that explain additional clustering of disorders that are either characterized by ‘norm-violations’ (CD, substance-use disorders) or by ‘oppositional behavior’ (oppositional defiant disorder [ODD], attention deficit hyperactivity disorder [ADHD]; Farmer et al., 2009). It has also been suggested that there may be aggression-related and substance-related subfactors (Krueger et al., 2007). Overall, the findings on the subfactor structure of the externalizing domain have so far been less consistent than for the internalizing domain (e.g., Krueger et al., 2005; Markon & Krueger, 2005; Vrieze et al., 2012).
Despite ongoing discussions about the best lower-order structure, the higher-order, two-factor model has been found to be very robust and is considered to reflect the natural structure of common mental disorders (Krueger, 1999; Watson, 2005; Krueger & Markon, 2006; Kotov et al., 2011; Carragher et al., 2015; Kotov et al., 2017). Various studies have supported this idea. For instance, variations on the internalizing and externalizing domains have been found to be linked to variations on distinct genetic risk factors (Kendler et al., 2011; Lahey et al., 2017). In addition, the internalizing and externalizing domains have been shown to account for a large part of comorbidity patterns that are observed over a patients’ lifetime: the association of disorders with subsequent onset was found to be stronger within each domain than between domains (Kessler et al., 2011a; 2011b). However, disorders from each of the separate domains have also been shown to predict each other over time (Lahey et al., 2017). Structural studies that investigated psychopathology together with personality disorders have shown that the joint latent structure can be described with a finite number of dimensions, including internalizing and externalizing dimensions (Markon et al., 2010; Kotov et al., 2011; Røysamb et al., 2011; Kendler et al., 2011; South & Jarnecke, 2017). The two-factor structure has been shown to be structurally invariant across ethnic groups in the U.S. (Eaton et al., 2013b), gender (Hicks et al., 2007; Kramer et al., 2007; Eaton et al., 2012) and over time (e.g., Vollebergh et al., 2001; Eaton et al., 2011).
Despite the many insights that have been gained from the above described research, important research questions still remain unsatisfactorily answered. The current study aims to address the following of these questions: (1) how stable is the cross-national structure of common mental disorders and (2) where do uncommon mental disorders fit into the structure?
The first question deals with what has been referred to as ‘structural validity’. Establishing the structural validity of the model of mental disorders is very important as this stability across countries determines to what extent factors and (mean) factor-scores can be validly compared across countries when conducting mental health research. Therefore, more insight must be gained into cross-national measurement invariance of the latent structure of common mental disorders. Currently, there is little available research on this. Although the same general latent structure has been replicated in different countries (e.g., Australia: Slade & Watson, 2006; the Netherlands: Vollebergh et al., 2001; Norway: Røysamb et al., 2010), most of this work is from Western countries. Krueger et al. (2003) conducted the only cross-national study of the latent structure of mental disorders with data from the WHO Collaborative Study of Psychological Problems in General Health Care, which were collected in 15 countries around the world (Brazil, Chile, China, France, Germany, Greece, India, Italy, Japan, the Netherlands, New Zealand, Nigeria, Turkey, the U.K. and the U.S.). They showed that 2 factors (internalizing vs. alcohol problems) described the structure best in the cross-national and most of the country datasets. Formal evaluations of measurement invariance showed that the model had configural invariance and metric invariance (invariant factor loadings across countries) across countries, indicating that the factor-loading configuration was invariant but that factor means and residual variances could vary across countries. Unfortunately, this study included only one externalizing disorder (‘hazardous use of alcohol’), prohibiting a thorough investigation of the structural stability of the full externalizing domain. In the current cross-national study, the stability of a model based on a broader range of disorders could be investigated.
The optimal placement of many less common mental disorders into the 2-factor model has remained unclear, partly due to the limited availability of datasets that include these less common disorders. Fortunately, more recent, large epidemiological datasets have enabled researchers to extend the original two-factor model by including additional disorders. These studies have shown that psychotic experiences have been found to load on a separate factor (‘thought disorders’ or ‘psychosis’; Kotov et al., 2011; Keyes et al., 2013; Markon, 2010; Wright et al., 2013; Kotov et al., 2017). Bipolar disorders have been found to load on this ‘thought disorders’ factor as well (Kotov et al., 2011), but others have found a ‘bipolar/mania’ sub-factor of the internalizing domain (Forbush & Watson, 2013; Kotov et al., 2015) or have found bipolar disorder to cross-load on the fear and distress subfactors (Eaton et al., 2013a), making it unclear whether bipolar disorder belongs with the internalizing disorders, the thought disorders or both (Kotov et al., 2017). Eating disorders have been found to group with the internalizing disorders, more specifically, as a subfactor of the internalizing domain (Forbush et al., 2010; Forbush & Watson, 2013). Taken together, research on uncommon disorder placement has been comparatively scarce and the results rather inconsistent. This could reflect the multifactorial nature of the studied uncommon disorders, but could also be explained by methodological differences (e.g., the kind and number of included symptoms/disorders) which brings us to a more nuanced notion of common and uncommon disorders: some of the common disorders have rather low prevalence (e.g. panic disorder) while some of the uncommon disorders are in fact more prevalent (e.g. eating disorder). This has a lot to do with methodological differences in their grouping but also in- exclusion of subthreshold variants of a disorder (e.g. psychotic experiences versus schizophrenia). Although not perfect, we will use the term uncommon disorders in the present study to describe eating disorders, bipolar disorder and psychotic experiences. Both from an etiological and clinical perspective, it would be very useful to find out much more about the placement of these disorders into the latent structure, as this could provide very interesting clues about the nature and the extent of overlap between vulnerabilities for common and uncommon, but very severe, disorders (Kotov et al., 2017). To gain a more systematic and complete insight into this, more research is needed using samples, in which all common but also (several) uncommon disorders were systematically assessed. Such datasets were available for the current study.
Given the above described need for further research, the current study aimed to investigate (1) the latent structure of common mental disorders and its measurement invariance across countries, and (2) the placement of uncommon disorders into the latent structure. Data came from the World Mental Health (WMH) surveys, which were conducted in several countries around the world and included a comprehensive assessment of both common internalizing and externalizing disorders, (e.g., ADHD, CD,ODD and Intermittent Explosive Disorder [IED], substance abuse and dependence) and less common disorders. More specifically, a range of models, based on the previous literature was tested to evaluate the optimal placement of (1) eating disorders, (2) bipolar disorder and (3) psychotic experiences in the model.
Methods
World Mental Health Surveys
Data came from the World Mental Health Surveys (Kessler et al, 2004). The WHO Composite International Diagnostic Interview (CIDI) version 3.0 was administered in 29 WMH surveys across the world. Most surveys used stratified multistage clustered area probability household sampling with no substitution for non-participants. Data collection took place between 2001 and 2012, and response rates ranged from 45.9 to 97.2%, with an average of 69.5%. Classification of country income categories was based on the World Bank criteria at the time of each survey (The World Bank, 2009). All WMH surveys were conducted face-to-face by lay interviewers who had received standardized training. Standardized translation, back-translation, harmonization and quality control procedures were applied in all of the participating survey sites (Pennell et al, 2008). Informed consent was obtained according to protocols endorsed by local Institutional Review Boards.
The CIDI was divided into two parts, with Part I assessing core mental disorders and Part II additional disorders and correlates. Part I was completed by all subjects and Part II was administered to all subjects meeting criteria for any of the Part I disorders and a probability subsample of the other subjects. To adjust for differential sampling, all responses in the Part II subsample were weighted by the inverse of their probability of selection into the Part II sample.
Mental Disorders
Analyses were conducted with lifetime CIDI/DSM-IV diagnoses (present/absent), without hierarchy rules. The following common mental disorders were included: Major depressive episode (MDE), Dysthymia, Panic Disorder, Agoraphobia, Social phobia, Specific phobia, GAD, PTSD, ADHD, ODD, Alcohol abuse, Drug abuse, CD and IED. The prevalence rates of these disorders in the different countries have been described previously (see Supplement 1 for disorder-specific references). Alcohol and drug abuse were combined into a single substance-abuse variable (with or without substance dependence). Bipolar-i, bipolar-ii and subthreshold bipolar disorder were assessed with the CIDI and were combined into a single bipolar disorder variable (present/absent). In the eating disorders dataset, bulimia and binge-eating disorder were assessed in all part II subjects in Romania, Brazil, and Poland and in a random part of part-II subjects in the other countries. combined into a single eating-disorder variable (Anorexia Nervosa was not included due to very low prevalence). The assessed psychotic experiences included hallucinations (visual and auditory) and delusions (insertion/withdrawal of thoughts, mind control by some strange force, ideas of reference [e.g., telepathy], plot to harm you/people following you). In this dataset, psychotic experiences were assessed in all part II subjects in Brazil and Romania, and in a random part of the part II sample in the other countries. The six assessed psychotic experiences were used as individual input variables in the CFAs.
Samples
To enable inclusion of as much disorders as possible, all current analyses were run in subjects in the Part II sample within the age-range of 18–44 years because most externalizing disorders (e.g., ADHD) were only assessed in these subjects to limit recall-bias. Bipolar disorder, eating disorders and psychotic experiences were only assessed in subsamples. Therefore, models including these respective disorders were estimated in the subsets of countries, in which they were assessed.
The subsample that was used to investigate the structure of all common mental disorders included 10 samples from 9 countries (Brazil, Colombia, Colombia-Medellin, Mexico, Murcia, North-Ireland, Peru, Poland, Romania, U.S.; n=15,499). This dataset was also used to investigate the optimal placement of bipolar disorder. The additional placement of IED into the model was investigated in a subsample where IED was assessed (Brazil, Colombia, North-Ireland, Peru, Poland, Romania, U.S.; n=12,162). The placement of eating disorders was investigated in a subsample (n=10,585) that included all subjects that were assessed for eating disorders with the CIDI. In Romania, Brazil, and Poland, eating disorders were assessed in all part II subjects. In the other countries, eating disorders were assessed in a random part of part-II subjects. The placement of psychotic experiences was investigated in a subsample of 6 countries, in which they were assessed in addition to common mental disorders and bipolar disorder (Brazil, Colombia, Mexico, Peru, Romania, U.S.; n= 5,478). In each of these countries, psychotic experiences were assessed in a random subsample and only those who had completed the psychosis section were included.
Analyses
Hypothesized models from the literature were fit to the WMH surveys data using confirmatory factor analyses (CFA). Multigroup-CFA (MG-CFA) was used to investigate structural invariance across countries. All CFAs were conducted with Mplus 7 (Muthén & Muthén, 1998–2012), using a mean and variance adjusted Weighted Least Squares estimator (WLSMV). All CFAs were run using the Mplus procedures for complex designs and included WMH surveys design variables (clusters and strata) to account for effects of the complex design (Asparouhov, 2005) and weights to adjust for differential probabilities of selection and discrepancies with census data (see Heeringa et al., 2008 for more info on sampling weights and design variables in WMH). The Comparative Fit Index (CFI) and the Root Mean Square Error of Approximation (RMSEA) were used to evaluate model fit, with a CFI≥0.95 and an RMSEA≤0.06 indicating good fit to the data (Hu & Bentler, 1999).
In the MG-CFAs, the model with the best cross-national fit was estimated with increasing levels of invariance across countries: configural invariance (similar patterns of factor loadings and item-thresholds; loadings and thresholds may differ across countries), partial invariance (constrained factor loadings across countries, freely estimated item-thresholds in each country) and scalar invariance, (factor loadings and item-thresholds constrained across countries). The difference in CFI between models with different levels of invariance (ΔCFI) was used to compare models with different levels of measurement invariance. A difference of ≥0.01 has previously been suggested to indicate a meaningful difference when comparing two groups (Cheung & Rensvold, 2002).
Results
Bivariate associations
Table 2 shows the tetrachoric correlations between the lifetime disorders. The highest correlations among common disorders were observed between MDE and dysthymia (0.82), ODD and CD (0.71), MDE and GAD (0.65), GAD and PTSD (0.65), ADHD and ODD (0.65), and dysthymia and GAD (0.61). In addition, high correlations were observed between several of the psychotic experiences. The lowest correlations among common disorders were observed for Agoraphobia with CD (0.24) and agoraphobia with substance abuse (0.19), eating disorder with CD (0.21), and specific phobia with substance abuse. In addition, lower correlations were observed between many of the psychotic experiences and other disorders.
Table 2.
Tetrachoric correlations of lifetime common mental disorders, bipolar disorder, eating disorder and psychotic experiences
| MDE | Dysth. | GAD | PTSD | PD | Ago | SAD | Sp. Phob. |
ADHD | ODD | CD | Sub- stance |
IED | Eat | Bipol. | PE1: Vis. Hal. |
PE2: Aud. Hal. |
PE3: Thought |
PE4: Mind cont. |
PE5: Tele-pathy |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDE | - | |||||||||||||||||||
| Dysth | 0.82 a | |||||||||||||||||||
| GAD | 0.65 a | 0.61 a | ||||||||||||||||||
| PTSD | 0.56 a | 0.46 a | 0.51 a | |||||||||||||||||
| PD | 0.47 a | 0.46 a | 0.49 a | 0.46 a | ||||||||||||||||
| Ago. | 0.46 a | 0.44 a | 0.44 a | 0.38 a | 0.55 a | |||||||||||||||
| SAD | 0.50 a | 0.49 a | 0.50 a | 0.44 a | 0.47 a | 0.65 a | ||||||||||||||
| Sp. Phob. | 0.42 a | 0.38 a | 0.38 a | 0.38 a | 0.45 a | 0.58 a | 0.52 a | |||||||||||||
| ADHD | 0.39 a | 0.42 a | 0.36 a | 0.42 a | 0.37 a | 0.34 a | 0.45 a | 0.31 a | ||||||||||||
| ODD | 0.36 a | 0.36 a | 0.34 a | 0.41 a | 0.34 a | 0.28 a | 0.43 a | 0.31 a | 0.65 a | |||||||||||
| CD | 0.34 a | 0.35 a | 0.32 a | 0.40 a | 0.38 a | 0.24 a | 0.38 a | 0.28 a | 0.57 a | 0.71 a | ||||||||||
| Substance | 0.29 a | 0.27 a | 0.28 a | 0.32 a | 0.30 a | 0.19 a | 0.29 a | 0.19 a | 0.38 a | 0.48 a | 0.55 a | |||||||||
| IED | 0.40 b | 0.34 b | 0.40 b | 0.31 b | 0.38 b | 0.33 b | 0.39 b | 0.31 b | 0.43 b | 0.44 b | 0.48 b | 0.35 b | - | |||||||
| Eat. | 0.36 c | 0.32 c | 0.33 c | 0.31 c | 0.25 c | 0.39 c | 0.35 c | 0.31 c | 0.39 c | 0.27 c | 0.21 c | 0.28 c | -e | - | ||||||
| Bipol. | 0.52 a | 0.43 a | 0.45 a | 0.38 a | 0.44 a | 0.48 a | 0.44 a | 0.39 a | 0.46 a | 0.46 a | 0.43 a | 0.42 a | -e | -e | - | |||||
| PE 1: Vis. Hal. | 0.27 d | 0.28 d | 0.34 d | 0.29 d | 0.29 d | 0.23 d | 0.19 d | 0.26 d | 0.19 d | 0.26 d | 0.18 d | 0.12 d | -e | -e | 0.24 d | - | ||||
| PE 2: Aud. Hal. | 0.39 d | 0.38 d | 0.22 d | 0.37 d | 0.35 d | 0.20 d | 0.22 d | 0.26 d | 0.21 d | 0.23 d | 0.14 d | 0.17 d | -e | -e | 0.28 d | 0.72 d | - | |||
| PE 3: Thought | 0.48 d | 0.35 d | 0.44 d | 0.41 d | 0.39 d | 0.35 d | 0.34 d | 0.31 d | 0.32 d | 0.25 d | 0.21 d | 0.27 d | -e | -e | 0.37 d | 0.64 d | 0.62 d | - | ||
| PE 4: Mind cont. | 0.45 d | 0.37 d | 0.39 d | 0.20 d | 0.29 d | 0.23 d | 0.05 d | 0.24 d | 0.17 d | 0.16 d | 0.17 d | 0.12 d | -e | -e | 0.25 d | 0.64 d | 0.69 d | 0.84 d | - | |
| PE 5: Telepathy | 0.41 d | 0.41 d | 0.33 d | 0.21 d | 0.24 d | 0.16 d | 0.15 d | 0.14 d | 0.33 d | 0.30 d | 0.25 d | 0.25 d | -e | -e | 0.29 d | 0.76 d | 0.65 d | 0.73 d | 0.82 d | - |
| PE 6: Delusion | 0.44 d | 0.36 d | 0.30 d | 0.51 d | 0.43 d | 0.46 d | 0.42 d | 0.37 d | 0.35 d | 0.17 d | 0.33 d | 0.34 d | -e | -e | 0.39 d | 0.46 d | 0.55 d | 0.77 d | 0.65 d | 0.58 d |
All correlation coefficients estimated with Mplus 7.0.
MDE=Major Depressive Episode; Dysth=Dysthymia; PTSD=Posttraumatic stress disorder; GAD=Generalized Anxiety Disorder; PD=panic disorder; Ago=Agoraphobia; SAD=Social Anxiety disorder; Sp.Phob=Specific phobia; ADHD=Attention Deficit Hyperactivity Disorder; CD=Conduct Disorder; ODD=Oppositional Defiant Disorder; Substance=Substance abuse disorder (with/without dependence); PE=Psychotic experience; Vis. Hal. =having a visual hallucination; Aud.Hal=having an auditory hallucination; Thought=believing that thoughts are extracted from or inserted into your head ; Mind cont.=feeling that your mind was taken over by a strange force; Telepathy= believing that a strange force tries to communicate with you (e.g., through special signs from the radio or TV); Delusion: believing that there is a plot going on against you or that people follow you.
Estimated in sample including Colombia. Peru. Romania, Brazil, Northern Ireland, Poland, Murcia, Medellin, Mexico and the United States (n=15499).
Estimated in subsample including Colombia, Peru, Romania, Brazil, Northern Ireland, Poland and the United States (n=12,162).
Estimated in sample including the complete data or a random subsample that got the eating disorders assessment from Colombia, Peru, Romania, Brazil, Northern Ireland, Poland, Murcia, Medellin, Mexico and the United States (n=10,585).
Estimated in subsample including complete data or a random subsample that got the psychotic experiences assessment from Colombia, Peru, Romania, Brazil, Mexico and the United States (n=5,478).
IED was not investigated together with eating disorders bipolar disorder and PEs; Eating disorders were not investigated together with IED, bipolar disorders and PEs
Structural model of the common mental disorders
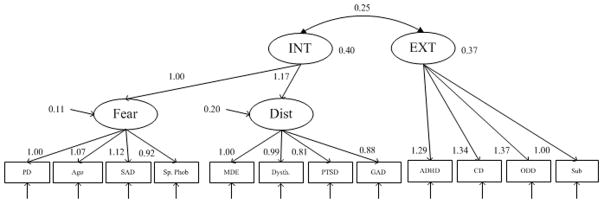
A simple 2-factor model and, a higher-order model with distress and fear sub-factors were estimated (Figure 1a; Table 3). Of these models, the higher-order model showed the best fit to the data (CFI=0.985; RMSEA=0.017), in line with a large body of previous work (Krueger et al., 1998; Krueger 1999; Vollebergh et al., 2001; Watson, 2005; Slade & Watson, 2006; Krueger & Markon, 2006; Miller et al., 2011; Eaton et al., 2013a; Kotov et al., 2017). In this model, all disorders showed considerable standardized loadings on their respective factors, the fear and distress factors showed considerable loadings on the second-order internalizing factor and the correlation between the second-order internalizing and externalizing factors was 0.61. Similar results were found when the analyses were run in a subset of countries that also all assessed IED.
Figure 1.
Factor loadings (unstandardized) of different structural models in the WMH surveys. One loading per factor was fixed to 1 for model identification. INT=internalizing; EXT=externalizing,; PSY=psychotic experiences; PD=panic disorder; Ago=Agoraphobia; SAD=Social Anxiety disorder; Sp.Phob=Specific phobia; MDE=Major Depressive Episode; Dysth=Dysthymia; PTSD=Posttraumatic stress disorder; GAD=Generalized Anxiety Disorder; ADHD=Attention Deficit Hyperactivity Disorder; CD=Conduct Disorder; ODD=Oppositional Defiant Disorder; Sub=Substance abuse disorder (with/without dependence); Eat=Eating disorder; Bipol=Bipolar disorder; Visual=Having visual hallucination; Audit=Having auditory hallucination; Thought=Having ideas of thought extraction or thought insertion; Mind=Feeling that your mind was taken over by an external force; Reference=Feeling that a strange force tries to communicate with you; Plot=Bbelief in an unjust plot that is going on to harm you.
Table 3.
Confirmatory factor analyses of the structure of common and uncommon mental disorders
| Included disorders | Sample (#countries) | Factor model | Fit indices | ||
|---|---|---|---|---|---|
| #FP | CFI | RMSEA (90% CI) | |||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee | 15,499 (10) | 2-factor modelc | 25 | 0.968 | 0.024 (0.022–0.026) |
| Higher-order modeld with fear and distress subfactors | 27 | 0.985 | 0.017 (0.015–0.019) | ||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee +IED | 12,162 (7) | 2-factor modelc | 27 | 0.971 | 0.022 (0.020–0.024) |
| Higher-order modeld with fear and distress subfactors and IED loading on the externalizing factor | 29 | 0.983 | 0.017 (0.015–0.019) | ||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee +Bipolar disorders | 15,499 (10) | Higher-order modeld with bipolar disorder loading directly on the second-order internalizing factor. | 28 | 0.983 | 0.017 (0.015–0.018) |
| Higher-orderd with bipolar disorder loading directly on the externalizing factor. | 28 | 0.974 | 0.021 (0.019–0.022) | ||
| Higher-orderd model with bipolar disorder loading on the fear subfactor | 29 | 0.979 | 0.019 (0.017–0.020) | ||
| Higher-orderd model with bipolar disorder loading on the distress subfactor | 29 | 0.977 | 0.020 (0.018–0.021) | ||
| Higher-orderd model with bipolar disorder loading on the fear and distress subfactor | 30 | 0.980 | 0.018 (0.017–0.020) | ||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee +Eating disorders | 10,585 (10)a | Higher-order: eating disorders loading directly on internalizing | 28 | 0.977 | 0.018 (0.016–0.021) |
| Higher-orderd: eating disorders loading on fear | 29 | 0.986 | 0.015 (0.013–0.017) | ||
| Higher-orderd: eating disorders loading on distress | 29 | 0.984 | 0.015 (0.013–0.018) | ||
| Higher-orderd: eating disorders loading on fear & distress | 30 | 0.986 | 0.015 (0.013–0.017) | ||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee +Psychotic experiences | 5,478 (6)b | 3-factorc: PEs load on their own factor | 39 | 0.972 | 0.015 (0.012–0.017) |
| Higher-order with PEs loading on their own factor | 41 | 0.984 | 0.011 (0.008–0.014) | ||
| MDE, Dysthymia, Panic disorder, PTSD, Social phobia, Specific phobia, Agoraphobia, GAD, ADHD, ODD, Conduct disorder, Substance abusee +Bipolar disorder and Psychotic experiences | 5,478 (6)b | Higher-order with bipolar loading on the internalizing factor | 43 | 0.983 | 0.011 (0.009–0.013) |
| Higher-order with bipolar loading on the PE factor | 43 | 0.959 | 0.017 (0.015–0.019) | ||
| Higher-order with bipolar loading on the internalizing and PE factors | 43 | 0.984 | 0.011 (0.009–0.013) | ||
Eating disorders were assessed in random subsamples in 7 of the 10 included countries.
Psychotic experiences were assessed in random subsamples in 4 of the 6 samples.
Model without cross-loadings and with freely estimated correlation(s) between factors
Model with freely estimated correlation between the higher-order factors
Including abuse and dependence
Structural validity
The invariance of the model of common mental disorders (minus IED) across countries was tested with MG-CFA using country as the group variable. When fitted to the individual samples, good fit of the model was observed in Brazil (CFI=0.969; RMSEA=0.017), Colombia (CFI=0.975; RMSEA=0.015), Colombia-Medellin (CFA=0.976; RMSEA=0.022), Mexico (CFI=0.982; RMSEA=0.016) and the U.S. (CFI=0.98; RMSEA=0.022). In the remaining countries (North Ireland, Murcia, Poland, Romania and Peru), model fitting was complicated by correlations close to 0 (or negative) in the disorder correlation matrix (mostly due to low frequencies of one or more disorders), which led to parameter estimates that were hard to interpret. Subsequent measurement-invariance analyses were therefore conducted with the first 5 samples from 4 countries. The results (Table 4) showed that the model with configural invariance across the 5 samples fit the data well (CFI=0.978; RMSEA=0.019). Constraining the first-order and second-order factor loadings led to a small decrease in fit (CFI=0.976; RMSEA=0.018). Constraining all first and second order factor loadings and all item-thresholds to be the same across samples (scalar invariance) led to a larger decrease in fit (CFI=0.962; RMSEA=0.021; ΔCFI=0.016). The decrease in CFI from the configural model to the model with constrained factor loadings (ΔCFI=0.002) indicated that partial invariance did hold across the 5 samples. The decrease in CFI from the configural model to the scalar model (ΔCFI=0.016) indicated that the model did not have scalar invariance across the 5 samples.
Table 4.
analyses of measurement invariance across five samples of the higher-order structural model of common mental disorders.
| Model | Model parameters | Fit indices | ||
|---|---|---|---|---|
|
| ||||
| CFI | RMSEA (90%CI) | ΔCFI | ||
| 1. Configural invariance | -1st and 2nd order factor loadings, item-thresholds and factor correlations unconstrained; | 0.978 | 0.019 (0.016–0.022) | - |
Fixed parameters:
|
||||
|
| ||||
| 2. Partial invariance | -1st and 2nd order factor loadings constrained; -Item-thresholds and correlations unconstrained. |
0.976 | 0.018 (0.015–0.021) | 0.002 |
Fixed parameters:
|
||||
|
| ||||
| 3. Scalar invariance | 1st and 2nd order factor loadings and item-thresholds constrained. -Factor means, factor correlations unconstrained. |
0.962 | 0.021 (0.019–0.024) | 0.016 |
Fixed parameters:
|
||||
CFI=comparative fit index; RMSEA=root mean squared error of approximation.
All models testing invariance across 10 samples.
All models estimated with the theta parameterization in Mplus 7 (Muthén & Muthén, 1998–2012).
Structural model of common disorders and bipolar disorders
The placement of bipolar disorder in the higher-order model was investigated next (Table 3). Different ways of grouping bipolar disorder with the internalizing factor all led to better fit than grouping it with the externalizing domain. Models with bipolar disorder loading separately on the second-order internalizing factor alongside the distress and fear sub-factors (in line with Forbush & Watson [2013] and Kotov et al. [2015]) showed slightly better fit (CFI=0.982; RMSEA=0.017) than a configuration with bipolar disorder loading on either the fear or distress subfactors, or bipolar disorder cross-loading on the fear and distress sub-factors (as found by Eaton et al. [2013]; CFI=0.980; RMSEA=0.018), but the difference in model-fit was very small, suggesting that bipolar disorder can be grouped with the internalizing domain.
Structural model of common disorders and eating disorders
The placement of eating disorders in the higher-order model was investigated next. In line with previous work (Forbush et al., 2010; Forbush & Watson, 2013), placing eating disorders as a subdomain under the internalizing domain led to better fit than grouping eating disorders with the externalizing domain. However, unlike previously found, a model with eating disorders loading directly on the internalizing factor (i.e., as a separate internalizing subdomain) alongside the distress and fear subfactors was not the best-fitting solution. A model with eating disorders loading on the distress and/or on the fear subfactor(s) showed better fit. However, fit was very similar across the latter models (all RMSEA=0.015) making it is hard to draw definite conclusions about the best subfactor-grouping of eating disorders (see Figure 1b for an illustration of the model with eating disorders loading on the distress subfactor)
Structural model of common disorders and psychotic experiences
A model with all psychotic experiences loading on a separate factor alongside the internalizing and externalizing factors fit the data well (Table 3; CFI=0.972; RMSEA=0.015) and a higher-order model with a psychotic experiences factor, and distress and fear subfactors for the internalizing factor showed even better fit (CFI=0.984; RMSEA=0.011).
Structural model of common disorders, bipolar disorder and PEs
A model with all common disorders, bipolar disorder and psychotic experiences was estimated next. IED and eating disorders were not included in these analyses because they were only assessed in smaller subsamples. Several higher-order models were compared, evaluating whether bipolar disorder could be better grouped with the internalizing disorders, with the psychotic experiences, or with both (see Table 3). The results showed that a model with bipolar disorders set to load directly on the internalizing factor (see Figure 1c) fit the data better than a model with bipolar disorder loading on the same factor as the psychotic experiences. Setting bipolar disorder to cross-load on both factors did not improve fit much (same RMSEA) compared to the first model. In this model, bipolar disorders showed a very small standardized loading on the psychotic experiences factor (−0.19), which differed strongly in terms of direction and magnitude from the other psychotic experiences loadings (0.76–0.91).
Discussion
We addressed several unresolved issues regarding the structure of mental disorders using the largest cross-national dataset to date encompassing a relatively wide selection of both internalizing and externalizing disorders, and both common and uncommon disorders. Overall, we found that a higher-order model with an internalizing and externalizing factor and fear and distress subfactors, described the structure of common mental disorders well. Investigations of measurement invariance of this structure across 5 selected countries showed that the factor loadings can be assumed to be stable. Investigations of the placement of uncommon disorders into the model showed that eating disorders and bipolar disorder could be grouped under the internalizing factor and that psychotic experiences were best modeled as a separate domain within the model. When bipolar disorder and psychotic experiences were included together in a single model, bipolar disorder was still best grouped with the internalizing domain (but not with a specific subfactor).
The results confirmed the higher-order structure of common mental disorders that has been observed in many previous studies (i.e. Krueger et al., 1998; Krueger 1999; Vollebergh et al., 2001; Watson, 2005; Slade & Watson, 2006; Krueger & Markon, 2006; Miller et al., 2008; Eaton et al., 2013b). Importantly, the current findings about measurement invariance showed that the structure was relatively stable across 5 different countries. These findings align with the only previous cross-national study that also found evidence for metric cross-national measurement invariance (Krueger, 2003). The current results extend on these previous findings by showing that a higher-order model that encompasses a full range of externalizing disorders, instead of only substance-related problems, fits the data well and shows metric invariance across countries.
When investigated together with the common mental disorders, bipolar disorder was found to be best grouped with the internalizing factor, in line with previous research showing bipolar/mania to be an internalizing subfactor (e.g., Forbush & Watson, 2013; Kotov et al., 2015). Other authors found bipolar disorder to cross-load on the distress and fear subfactors when investigated in the context of other internalizing disorders (Eaton et al., 2013), but such model-configurations were not found to fit better in the current study. These results indicate that, in the context of the included common mental disorders, bipolar disorder shows a clear general association with the internalizing domain. Previously, bipolar disorders have also been shown to be partly related to a ‘thought problems’ dimension together with e.g., psychosis (Kotov et al., 2017). Therefore, this was also evaluated by investigating a model that included both bipolar disorder and psychotic experiences. These analyses showed that grouping bipolar disorder strictly with the psychotic experiences led to a decrease in fit and letting bipolar disorder cross-load on the internalizing and psychotic experiences factor did hardly improve fit. This could be explained by the fact that the internalizing and psychotic experiences factors were already strongly correlated, making the added cross-loading redundant. In addition, the fact that six psychotic experiences from a single interview module (see below for further discussion) were used and just a single bipolar-disorder indicator, could have made the setup of the analysis suboptimal to evaluate the existence of a broad thought-disorder factor. Finally, an alternative explanation may be that there is significant heterogeneity in our measure of bipolar disorder. As it consists of different subtypes and represents different episodes, it is possible that some subtypes or episodes may be more strongly related to either internalizing disorders or thought problems.
As previously observed (Forbush et al., 2010; Forbush & Watson, 2013) models grouping eating disorders with the internalizing disorders fit best to the data. Setting eating disorders to load on the fear, distress or both subfactors led to similar model-fit, but led to better fit than setting eating disorders to load directly on the internalizing domain. These findings suggest that, when investigated in the context of common mental disorders, eating disorders show a general association with the internalizing domain and its subdomains, although its exact placement remained somewhat unclear. These somewhat ambiguous findings could partly be related to the fact that only one pooled eating-disorder indicator was used in the current model. It could be that a separate eating disorder (sub)factor could be identified if more individual indicators were used, also including Anorexia Nervosa.
In line with previous findings that psychotic experiences reflect a separate mental-health domain (i.e. ‘thought problems’) alongside the internalizing and externalizing domains (e.g. Markon, 2010; Wright et al., 2013), the current results showed that a model with psychotic experiences loading on their own separate factor fit the data well. Interestingly, this factor showed considerable correlation with the internalizing factor, indicating that psychotic experiences are related to other mental disorders, in line with previous work showing the cross-diagnostic importance of psychotic experiences (Rössler et al., 2011; Fusar-Poli et al., 2012; Werberloff et al., 2012).
The current results align with previous work in the WMH surveys. Kessler et al. (2011a, 2011b) investigated the role of the internalizing and externalizing domains in the development of comorbidity patterns within persons over time and showed that these were explained to a strong degree by within-domain clustering. The current results confirmed that the 2-factor structure of mental disorders and expanded on these results by providing more insight into the finer-grained structure and placement of mental disorders into a higher-order factor model.
An important implication of the higher-order model is that variations in mental health/disorders could be explained by causal influences that occur at different levels with different degrees of disorder specificity. Some influences can be disorder-specific, some occur at the level of the subfactor and are shared with a limited set of other disorders (i.e. other fear or distress disorders), and some occur at the level of the higher-order domains (i.e. internalizing or externalizing) and are shared with all other disorders within the domain.
It is important to note that there are also influences that are very non-specific and influence all disorders, irrespective of their grouping with first- or second order factors (Lahey et al., 2017). Indeed, the internalizing and externalizing domains have been repeatedly shown to be robustly correlated, which could indicate the existence of an overarching general factor of psychopathology that accounts for the shared variance of all disorders (‘p-factor’; Caspi et al., 2017; Lahey et al., 2017). To investigate this, bifactor models can be used that incorporate both a general factor and domain-specific group factors (e.g., Lahey et al., 2017). Although it has been pointed out that bifactor models can become complex and very hard to interpret (Eid et al., in press; Koch et al., in press), their use in structural research of mental disorders is an interesting topic for further investigation.
There are some limitations that should be kept in mind when interpreting the findings of this study. First, the analyses were limited to those WMH surveys with data on all disorders and to subjects in the age-range of 18 to 45 years, which may limit the generalizability of the findings to other populations. Second, the models were fitted on cross-national datasets but prevalence rates could differ across surveys. Still, the investigations of measurement invariance indicated that at least partial invariance across countries could be assumed, although only part of the countries could be included in these analyses as some countries showed very low disorder frequencies. Investigations of measurement invariance across larger sets of countries will probably only be possible with smaller models that include a very limited range of disorders. This could be done in future research. Third, psychotic experiences, rather than psychotic disorders and schizophrenia were assessed and included in the analyses. On the one hand, this could seem somewhat inconsistent, as all other modelled mental problems were included as formal disorders. On the other hand, psychotic experiences are more common than full-blown psychotic disorders, which provides more possibilities to model the full psychotic spectrum, irrespective of diagnosis. However, it is possible that some of the observed clustering of psychotic experiences in the analyses can be explained by the fact that they were assessed differently from the other diagnoses. Finally, the general indices of fit indicated good fit for all tested models. As such all model-comparisons were among models that (objectively) fit the data well and were often based on very small differences in fit.
The current results show that the structure of mental disorders is best represented by a higher-order factor model with some degree of cross-national stability. In addition, eating disorders were shown to group with the internalizing domain, bipolar disorder was shown to group most strongly with the internalizing domain and psychotic experiences were shown to group with their own domain that was correlated with the other domains.
Supplementary Material
Table 1.
WMH sample characteristics by World Bank income categoriesa
| Sample size | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Country by income category | Surveyb | Sample characteristicsc | Field dates | Age range | Part I | Part II | Part II aged 18–44 |
Response rated |
| Low and lower middle income countries | ||||||||
| Colombia | NSMH | All urban areas of the country (approximately 73% of the total national population). | 2003 | 18–65 | 4,426 | 2,381 | 1,731 | 87.7 |
| Peru | EMSMP | Five urban areas of the country (approximately 38% of the total national population). | 2004–5 | 18–65 | 3,930 | 1,801 | 1,287 | 90.2 |
|
|
||||||||
| Total | (8,356) | (4,182) | (3,018) | 88.9 | ||||
|
| ||||||||
| Upper-middle income countries | ||||||||
| Brazil - São Paulo | São Paulo Megacity | São Paulo metropolitan area. | 2005–8 | 18–93 | 5,037 | 2,942 | 1,824 | 81.3 |
| Colombia – Medelline | MMHHS | Medellin metropolitan area | 2011–12 | 19–65 | 3,261 | 1,673 | 970 | 97.2 |
| Mexico | M-NCS | All urban areas of the country (approximately 75% of the total national population). | 2001–2 | 18–65 | 5,782 | 2,362 | 1,736 | 76.6 |
| Romania | RMHS | Nationally representative. | 2005–6 | 18–96 | 2,357 | 2,357 | 940 | 70.9 |
|
|
||||||||
| Total | (16,437) | (9,334) | (5,470) | 80.5 | ||||
|
| ||||||||
| High-income countries | ||||||||
| N. Ireland | NISHS | Nationally representative. | 2005–8 | 18–97 | 4,340 | 1,986 | 907 | 68.4 |
| Poland | EZOP | Nationally representative | 2010–11 | 18–65 | 10,081 | 4,000 | 2,276 | 50.4 |
| Spain - Murcia | PEGASUS- Murcia | Murcia region. | 2010–12 | 18–96 | 2,621 | 1,459 | 631 | 67.4 |
| United States | NCS-R | Nationally representative. | 2001–3 | 18–99 | 9,282 | 5,692 | 3,197 | 70.9 |
|
|
||||||||
| Total | (26,324) | (13,137) | (7,011) | 60.8 | ||||
| TOTAL N | (51,117) | (26,653) | (15,499) | 69.9 | ||||
The World Bank (2012) Data. Accessed May 12, 2012 at: http://data.worldbank.org/country. Some of the WMH countries have moved into new income categories since the surveys were conducted. The income groupings above reflect the status of each country at the time of data collection. The current income category of each country is available at the preceding URL.
NSMH (The Colombian National Study of Mental Health); EMSMP (La Encuesta Mundial de Salud Mental en el Peru); MMHHS (Medellín Mental Health Household Study); M-NCS (The Mexico National Comorbidity Survey); RMHS (Romania Mental Health Survey); NISHS (Northern Ireland Study of Health and Stress); EZOP (Epidemiology of Mental Disorders and Access to Care Survey); PEGASUS-Murcia (Psychiatric Enquiry to General Population in Southeast Spain-Murcia);NCS-R (The US National Comorbidity Survey Replication).
Most WMH surveys are based on stratified multistage clustered area probability household samples in which samples of areas equivalent to counties or municipalities in the US were selected in the first stage followed by one or more subsequent stages of geographic sampling (e.g., towns within counties, blocks within towns, households within blocks) to arrive at a sample of households, in each of which a listing of household members was created and one or two people were selected from this listing to be interviewed. No substitution was allowed when the originally sampled household resident could not be interviewed. Several WMH surveys (Poland, Spain-Murcia) used country resident or universal health-care registries to select respondents without listing households. 4 of the 10 surveys are based on nationally representative samples.
The response rate is calculated as the ratio of the number of households in which an interview was completed to the number of households originally sampled, excluding from the denominator households known not to be eligible either because of being vacant at the time of initial contact or because the residents were unable to speak the designated languages of the survey. The weighted average response rate is 69.9%.
Colombia moved from the “lower and lower-middle income” to the “upper-middle income” category between 2003 (when the Colombian National Study of Mental Health was conducted) and 2010 (when the Medellin Mental Health Household Study was conducted), hence Colombia’s appearance in both income categories. For more information, please see footnote a.
Acknowledgments
This work was supported by a VICI grant (no: 91812607) received by Peter de Jonge from the Netherlands organization for Scientific research (NWO-ZonMW). The World Health Organization World Mental Health (WMH) Survey Initiative is supported by the United States National Institute of Mental Health (NIMH; R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the United States Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline, and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis.
The São Paulo Megacity Mental Health Survey is supported by the State of São Paulo Research Foundation (FAPESP) Thematic Project Grant 03/00204-3. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection. The Mental Health Study Medellín – Colombia was carried out and supported jointly by the Center for Excellence on Research in Mental Health (CES University) and the Secretary of Health of Medellín. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the PanAmerican Health Organization (PAHO). The Northern Ireland Study of Mental Health was funded by the Health & Social Care Research & Development Division of the Public Health Agency. The Peruvian World Mental Health Study was funded by the National Institute of Health of the Ministry of Health of Peru. The Polish project Epidemiology of Mental Health and Access to Care –EZOP Project (PL 0256) was supported by Iceland, Liechtenstein and Norway through funding from the EEA Financial Mechanism and the Norwegian Financial Mechanism. EZOP project was co-financed by the Polish Ministry of Health. The Romania WMH study projects “Policies in Mental Health Area” and “National Study regarding Mental Health and Services Use” were carried out by National School of Public Health & Health Services Management (former National Institute for Research & Development in Health, present National School of Public Health Management & Professional Development, Bucharest), with technical support of Metro Media Transilvania, the National Institute of Statistics – National Centre for Training in Statistics, SC. Cheyenne Services SRL, Statistics Netherlands and were funded by Ministry of Public Health (former Ministry of Health) with supplemental support of Eli Lilly Romania SRL. The Psychiatric Enquiry to General Population in Southeast Spain – Murcia (PEGASUS-Murcia) Project has been financed by the Regional Health Authorities of Murcia (Servicio Murciano de Salud and Consejería de Sanidad y Política Social) and Fundación para la Formación e Investigación Sanitarias (FFIS) of Murcia. The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust.
The Brazilian Council for Scientific and Technological Development supports Dr Laura Helena Andrade (CNPq Grant # 307784/2016-9).
None of the funders had any role in the design, analysis, interpretation of results, or preparation of this paper. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of the World Health Organization, other sponsoring organizations, agencies, or governments.
The WHO World Mental Health Survey collaborators are Sergio Aguilar-Gaxiola, MD, PhD, Ali Al-Hamzawi, MD, Mohammed Salih Al-Kaisy, MD, Jordi Alonso, MD, PhD, Laura Helena Andrade, MD, PhD, Corina Benjet, PhD, Guilherme Borges,ScD, Evelyn J. Bromet, PhD, Ronny Bruffaerts, PhD, Brendan Bunting, PhD, Jose Miguel Caldas de Almeida, MD, PhD, Graça Cardoso, MD, PhD, Somnath Chatterji, MD, Alfredo H. Cia, MD, Louisa Degenhardt, PhD, Koen Demyttenaere, MD, PhD, John Fayyad, MD, Silvia Florescu, MD, PhD, Giovanni de Girolamo, MD, Oye Gureje, MD, DSc, FRCPsych, Josep Maria Haro, MD, PhD, Yanling He, MD, Hristo Hinkov, MD, PhD, Chi-yi Hu, MD, PhD, Yueqin Huang, MD, MPH, PhD, Peter de Jonge, PhD, Aimee Nasser Karam, PhD, Elie G. Karam, MD, Norito Kawakami, MD, DMSc, Ronald C. Kessler, PhD, Andrzej Kiejna, MD, PhD, Viviane Kovess-Masfety, MD, PhD, Sing Lee, MB, BS, Jean-Pierre Lepine, MD, Daphna Levinson, PhD, John McGrath, MD, PhD, Maria Elena Medina-Mora, PhD, Jacek Moskalewicz, PhD, Fernando Navarro-Mateu, MD, PhD, Beth-Ellen Pennell, MA, Marina Piazza, MPH, ScD, Jose Posada-Villa, MD, Kate M. Scott, PhD, Tim Slade, PhD, Juan Carlos Stagnaro, MD, PhD, Dan J. Stein, FRCPC, PhD, Margreet ten Have, PhD, Yolanda Torres, MPH, Dra.HC, Maria Carmen Viana, MD, PhD, Harvey Whiteford, MBBS, PhD, David R. Williams, MPH, PhD, Bogdan Wojtyniak, ScD.
Footnotes
Declaration of Interest
In the past 3 years, Dr. Kessler received support for his epidemiological studies from Sanofi Aventis, was a consultant for Johnson & Johnson Wellness and Prevention, and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Kessler is a co-owner of DataStat, Inc., a market research firm that carries out healthcare research.
References
- Asparouhov T. Sampling Weights in Latent Variable Modeling. Structural Equation Modeling. 2005;12(3):411–434. [Google Scholar]
- Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Social Psychiatry and Psychiatric Epidemiology. 1998;33(12):587–95. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- Brodbeck J, Stulz N, Itten S, Regli D, Znoj H, Caspar F. The structure of psychopathological symptoms and the associations with DSM-diagnoses in treatment seeking individuals. Comprehensive Psychiatry. 2014;55(3):714–26. doi: 10.1016/j.comppsych.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Carragher N, Krueger RF, Eaton NR, Slade T. Disorders without borders: current and future directions in the meta-structure of mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2015;50(3):339–50. doi: 10.1007/s00127-014-1004-z. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, Moffitt TE. The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clinical Psychological Science. 2(2):119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating Goodness-of-Fit Indexes for Testing Measurement Invariance. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9:233–255. [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, Grant BF, Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. Journal of Abnormal Psychology. 2012;121(1):282–8. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Noordhof A, Skodol AE, Markon KE, Grant BF, Hasin DS. Ethnicity and psychiatric comorbidity in a national sample: evidence for latent comorbidity factor invariance and connections with disorder prevalence. Social Psychiatry and Psychiatric Epidemiology. 2013b;48(5):701–10. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, Hasin DS, Grant BF. The structure and predictive validity of the internalizing disorders. Journal of Abnormal Psychology. 2013a;122(1):86–92. doi: 10.1037/a0029598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Oltmanns TF. Aging and the structure and long-term stability of the internalizing spectrum of personality and psychopathology. Psychology and Aging. 2011;26(4):987–93. doi: 10.1037/a0024406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Rodriguez-Seijas C, Carragher N, Krueger RF. Transdiagnostic factors of psychopathology and substance use disorders: a review. Social Psychiatry and Psychiatric Epidemiology. 2015;50(2):171–82. doi: 10.1007/s00127-014-1001-2. [DOI] [PubMed] [Google Scholar]
- Eid M, Geiser C, Koch T, Heene M. Anomalous results in g-factor models: Explanations and alternatives. Psychological Methods. doi: 10.1037/met0000083. (in press) Advance online publication . [DOI] [PubMed]
- Farmer RF, Seeley JR, Kosty DB, Lewinson PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. Journal of Abnormal Psychology. 2009;118(4):699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, South SC, Krueger RF, Iacono WG, Clark LA, Keel PK, Legrand LN, Watson D. Locating eating pathology within an empirical diagnostic taxonomy: evidence from a community-based sample. Journal of Abnormal Psychology. 2010;119(2):282–92. doi: 10.1037/a0019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychological Medicine. 2013;43(1):97–108. doi: 10.1017/S0033291712001092. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P. Predicting psychosis: Meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry. 2012;69(3):220. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- Hasin D, Kilcoyne B. Comorbidity of psychiatric and substance use disorders in the United States: current issues and findings from the NESARC. Current Opinions in Psychiatry. 2012;25(3):165–71. doi: 10.1097/YCO.0b013e3283523dcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, Wells EJ, Hubbard F. Sample designs and sampling procedures. In: Kessler RC, Üstun TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York, NY: Cambridge University Press; 2008. [Google Scholar]
- Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, McGue M. Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: A longitudinal twin study. Journal of Abnormal Psychology. 2007;116(3):433–47. doi: 10.1037/0021-843X.116.3.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. American Journal of Psychiatry. 2011;168(1):29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Cox BJ, Green JG, Ormel J, McLaughlin KA, Merikangas KR, Petukhova M, Pine DS, Russo LJ, Swendsen J, Wittchen HU, Zaslavsky AM. The effects of latent variables in the development of comorbidity among common mental disorders. Depression and Anxiety. 2011;28(1):29–39. doi: 10.1002/da.20760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu C, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustün TB. Development of lifetime comorbidity I the World Health Organization world mental health surveys. Archives of General Psychiatry. 2011a;68(1):90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Zaslavsky AM. The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Current Opinions in Psychiatry. 2011b;24(4):307–12. doi: 10.1097/YCO.0b013e3283477b22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, Skodol AE, Wall MM, Grant B, Siever LJ, Hasin DS. Thought disorder in the meta-structure of psychopathology. Psychological Medicine. 2013;43(8):1673–83. doi: 10.1017/S0033291712002292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch T, Holtmann J, Bohn J, Eid M. Explaining General and Specific Factors in Longitudinal, Multimethod, and Bifactor Models: Some Caveats and Recommendations. Psychological Methods. doi: 10.1037/met0000146. (in press) Advance online publication. [DOI] [PubMed]
- Kotov R, Chang SW, Fochtmann LJ, Mojtabai R, Carlson GA, Sedler MJ, Bromet EJ. Schizophrenia in the internalizing-externalizing framework: a third dimension? Schizophrenia Bulletin. 2011a;37(6):1168–78. doi: 10.1093/schbul/sbq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011b;68(10):1003–11. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Kotov R, Perlman G, Gámez W, Watson D. The structure and short-term stability of the emotional disorders: a dimensional approach. Psychological Medicine. 2015;45(8):1687–98. doi: 10.1017/S0033291714002815. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, Miller JD, Moffitt TE, Morey LC, Mullins-Sweatt SN, Ormel J, Patrick CJ, Regier DA, Rescorla L, Ruggero CJ, Samuel DB, Sellbom M, Simms LJ, Skodol AE, Slade T, South SC, Tackett JL, Waldman ID, Waszczuk MA, Widiger TA, Wright AGC, Zimmerman M. The Hierarchical Taxonomy of Psychopathology (HiTOP): A Dimensional Alternative to Traditional Nosologies. Journal of Abnormal Psychology. 2017;126(4):454–477. doi: 10.1037/abn0000258. [DOI] [PubMed] [Google Scholar]
- Kramer MD, Krueger RF, Hicks BM. The role of internalizing and externalizing liability factors in accounting for gender differences in the prevalence of common psychopathological syndromes. Psychological Medicine. 2007;38(1):51–61. doi: 10.1017/S0033291707001572. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107(2):216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology. 2003;112(3):437–47. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. Journal of Abnormal Psychology. 2005;114(4):537–50. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116(4):645–66. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–33. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56(10):921–6. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121(4):971–7. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, Zald DH. A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin. 2017;143(2):142–186. doi: 10.1037/bul0000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Archives of General Psychiatry. 2005;62(12):1352–9. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40(2):273–88. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Miller MW, Fogler JM, Wolf EJ, Kaloupek DG, Keane TM. The internalizing and externalizing structure of psychiatric comorbidity in combat veterans. Journal of Traumatic Stress. 2008;21(1):58–65. doi: 10.1002/jts.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Pennell B, Mneimneh Z, Bowers A, Chardoul S, Wells J, Viana M, Dinkelmann K, Gebler N, Florescu S, He Y, Huang Y, Tomov T, Vilagut G. Implementation of the World Mental Health Surveys. In: Kessler R, Üstün T, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. Cambridge University Press; Cambridge, UK: 2008. pp. 33–57. [Google Scholar]
- Rössler W, Hengartner MP, Ajdacic-Gross V, Haker H, Angst J. Sub-clinical psychosis symptoms in young adults are risk factors for subsequent common mental disorders. Schizophrenia Research. 2011;131(1):18–23. doi: 10.1016/j.schres.2011.06.019. [DOI] [PubMed] [Google Scholar]
- Røysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, Torgersen S, Reichborn-Kjennerud T. The joint structure of DSM-IV Axis I and Axis II disorders. Journal of Abnormal Psychology. 2010;120(1):198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Trull TJ. Methodological issues in psychopathology research. Annual Review of Psychology. 1996;47:371–400. doi: 10.1146/annurev.psych.47.1.371. [DOI] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36(11):1593–600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- South SC, Jarnecke AM. Structural equation modeling of personality disorders and pathological personality traits. Personality Disorders: Theory, Research, and Treatment. 2017;8(2):113–129. doi: 10.1037/per0000215. [DOI] [PubMed] [Google Scholar]
- Teesson M, Slade T, Mills K. Comorbidity in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry. 2009;43(7):606–14. doi: 10.1080/00048670902970908. [DOI] [PubMed] [Google Scholar]
- Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Archives of General Psychiatry. 2001;58(6):597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Vrieze SI, Perlman G, Krueger RF, Iacono WG. Is the continuity of externalizing psychopathology the same in adolescents and middle-aged adults? A test of the externalizing spectrum’s developmental coherence. Journal of Abnormal Child Psychology. 2012;40(3):459–70. doi: 10.1007/s10802-011-9571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. [Accessed May 12, 2009];Data and Statistics. at: http://go.worldbank.org/D7SN0B8YU0.
- Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114(4):522–36. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Werbeloff N, Drukker M, Dohrenwend BP, Levav I, Yoffe R, van Os J, Davidson M, Weiser M. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Archives of General Psychiatry. 2012;69(5):467–75. doi: 10.1001/archgenpsychiatry.2011.1580. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Clark LA. Toward DSM-V and the classification of psychopathology. Psychological Bulletin. 2000;126(6):946–63. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- Wright AG, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The structure of psychopathology: toward an expanded quantitative empirical model. Journal of Abnormal Psychology. 2013;122(1):281–94. doi: 10.1037/a0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.