Abstract
Background
Vaccination protects individuals directly and communities indirectly by reducing transmission. We aimed to determine whether information about herd immunity and local vaccination coverage could change an individual’s vaccination plans and concern about influenza.
Methods
We surveyed Minnesota residents 18 years during the 2016 Minnesota State Fair. Participants were asked to identify the definition of herd immunity, to report their history of and plans to receive influenza vaccine, to report their concern about influenza, and to estimate the reported influenza vaccination coverage in their county. After providing educational information about herd immunity and local vaccination rates, we reassessed vaccination plans and concerns. We used logistic regression to estimate predicted percentages for those willing to be vaccinated, for concern about influenza, and for changes in these outcomes after the intervention. We then compared those individuals with and without prior knowledge of herd immunity, accounting for other characteristics.
Results
Among 554 participants, the median age was 57 years; most were female (65.9%), white (91.0%), and non-Hispanic/Latino (93.9%). Overall, 37.2% of participants did not know about herd immunity and 75.6% thought that the influenza vaccination coverage in their county was higher than it was reported. Those not knowledgeable about herd immunity were significantly less likely than those knowledgeable about the concept to report plans to be vaccinated at baseline (67.8% versus 78.9%; p = 0.004). After learning about herd immunity and influenza vaccination coverage, the proportion of those not knowledgeable about herd immunity who were willing to be vaccinated increased significantly by 7.3 percentage points (p = 0.001). Educating participants eliminated the significant difference in the proportion planning to be vaccinated between these two groups (80.1% of those knowledgeable and 75.1% of those who were not initially knowledgeable became willing; p = 0.148).
Conclusions
Education about herd immunity and local vaccination coverage could be a useful tool for increasing willingness to vaccinate, generating benefits both to individuals and communities.
Keywords: Influenza vaccination, Herd immunity, Indirect protection, Vaccination coverage
1. Background and significance
Influenza is a vaccine-preventable infectious disease that is responsible for an estimated 3–5 million cases of severe illness and 250,000–500,000 deaths each year primarily among young children, the elderly, and pregnant women [1,2]. The annual incidence depends on many factors including the variability of circulating strains, the proportion of individuals in the population who have acquired natural immunity or who have been immunized, and the efficacy of the annual vaccine [3]. Maintaining high vaccination coverage is important because the effectiveness of the influenza vaccine is relatively low and not everyone can be vaccinated [4–6]. Beginning in 2010 in the United States, annual influenza vaccination was recommended for all individuals aged 6 months or older with the exception of those with medical contraindications [7]. Despite this universal recommendation and the Healthy People 2020 target of 70% vaccinated, the Centers for Disease Control and Prevention estimate that only 45.6% of the U.S. population and 49.7% of Minnesota residents were vaccinated against influenza during the 2015–16 influenza season [8–10].
Vaccination protects individuals directly by inducing an immune response and protects communities indirectly by reducing transmission and the risk of infection. Indirect protection at the community level provides additional benefit beyond what would be expected from direct protection alone [3,11]. This concept of “herd immunity” or “community immunity” demonstrates that vaccinating a high proportion of the population can prevent outbreaks and protect both vaccinated and unvaccinated individuals. The degree to which vaccination can reduce transmission in a population depends upon several factors, including the transmissibility of the pathogen, the network of human interactions and frequency of contacts, and the effectiveness and distribution of the vaccine. Herd immunity is best thought of as a continuum rather than a threshold [12]. Estimates of the influenza vaccination coverage needed to maximize the benefits of herd immunity and reduce disease transmission vary widely; under various scenarios vaccinating 33–73% of the population can prevent outbreaks [3,12].
Previous studies have demonstrated that individuals consider community-level benefits of vaccination in addition to personal benefits when choosing whether to be vaccinated [13]. While willingness to vaccinate was highest when individuals themselves were at risk, Vietri et al. found that college students were more willing to be vaccinated when they were told that 95% of the community would benefit from their decision compared to a scenario where only 10% would benefit [14,15]. A systematic review found that between 1 and 6% of parents chose benefit to others as their primary motive for vaccinating their children while 37% ranked benefit to others as their secondary motive [16,17]. Since maximizing community-level benefits of vaccination requires high levels of vaccine uptake, some vaccination campaigns have sought to increase willingness to be vaccinated by emphasizing the added communal benefits. For example, ‘Do It For The Herd’ is a frequent phrase used to promote free influenza vaccination clinics for University of Minnesota students, faculty, staff, and others which is aimed at increasing vaccination coverage by emphasizing the population-level benefits of decreasing transmission [18].
Despite these efforts, little is known about whether individuals are aware of the impact of their vaccination decision on their community and whether receiving education about the community-level benefits of immunization and the vaccination coverage in their county will influence their willingness to be vaccinated. To address this, we aimed to determine (1) whether participants were familiar with both (a) the concept of herd immunity and the vaccination coverage needed for community-wide protection and (b) the vaccination coverage in their county, and (2) whether individual plans to get vaccinated and/or concern about getting influenza would change after providing education about herd immunity and reported, local vaccination rates.
2. Research methods
2.1. Setting and study design
We conducted a cross-sectional survey in the University of Minnesota’s (UMN) Driven to Discover (D2D) Research Facility over a 4-day period at the 2016 Minnesota State Fair, a 12-day event held annually in August and attended by 1.9 million individuals. The UMN D2D Facility is a building on the grounds of the state fair where researchers can conduct studies by recruiting individuals attending the fair. Prior to implementing the survey, we conducted a small pilot study to refine the questions and the educational information provided.
2.2. Participant recruitment
Potential participants were eligible if they were 18 years of age or older, residents of Minnesota for at least six months of the year, and could read, speak, and understand English. Eligibility and consent were determined prior to participants self-administering the 5–10 minute survey using Apple iPads.
2.3. Survey methodology
The survey consisted of a maximum of 26 questions (Table 1) about demographic characteristics, county of residence, knowledge of herd immunity, history and frequency of influenza vaccination, willingness to get vaccinated, and concern about influenza. Participants were then asked to estimate the percentage of the population of their county that would need to be vaccinated for the community to benefit from herd immunity (by preventing outbreaks, thus protecting everyone even those who are not vaccinated) and to estimate the percentage of the population in their county that had received the influenza vaccine in the previous year. After entering these estimates, participants were presented with written statements via the iPads to educate themselves about (1) the definition of herd immunity; (2) the reported 2015–2016 influenza vaccine uptake among individuals 6 months and older in their own county obtained from the Minnesota Department of Health’s Immunization Information Connection (MIIC), a statewide Immunization Information System (IIS) [19]; and (3) that at least 70% of a community needed to be vaccinated to prevent outbreaks and benefit everyone. Since the estimates for coverage needed to maximize the benefits of herd immunity and reduce disease transmission vary widely, 70% was chosen based on previous research and to align with the Healthy People 2020 influenza vaccination target [3,8]. Following this educational intervention, participants were again asked to report (1) how likely they were to get vaccinated against influenza in the upcoming year and (2) how concerned they would be about getting influenza in the upcoming year if they did not get vaccinated, and, in addition, (3) how concerned they were that an outbreak might occur in their county (post-intervention only). We collected and managed survey data using the Research Electronic Data Capture (REDCap) software, a secure, web-based application designed to support data capture for research studies [20].
Table 1.
Demographic characteristics of the 554 participants who completed the survey.
| Characteristics | Responses | n* | %* |
|---|---|---|---|
| Age | Years, median (IQR) | 57 | 29–66 |
| Sex | Male | 184 | 33.2 |
| Female | 365 | 65.9 | |
| Other | 1 | 0.2 | |
| Missing | 4 | 0.7 | |
| Race | American Indian or Alaska Native | 7 | 1.3 |
| Asian | 14 | 2.5 | |
| Black or African American | 6 | 1.1 | |
| Hawaiian or Other Pacific Islander | 1 | 0.2 | |
| White | 504 | 91.0 | |
| Multiracial | 8 | 1.4 | |
| Other | 12 | 2.2 | |
| Missing | 2 | 0.4 | |
| Ethnicity | Hispanic or Latino | 13 | 2.4 |
| Not Hispanic or Latino | 520 | 93.9 | |
| Missing | 21 | 3.8 | |
| Highest education completed | Elementary School | 5 | 0.9 |
| High School Diploma or GED | 133 | 24.0 | |
| Associates Degree | 98 | 17.7 | |
| Bachelor’s Degree | 191 | 34.5 | |
| Graduate Degree | 124 | 22.4 | |
| Missing | 3 | 0.5 | |
| County of residence (derived from zip code) | Live within Minneapolis/St. Paul metro area (Hennepin, Carver, Scott, Washington, Dakota, Anoka, and Ramsey counties) | 416 | 75.1 |
| Live outside metro area (all other counties) | 138 | 24.9 | |
| Household makeup | Number of Adults 18 years, mean (SD) | 2.1 | 1.2 |
| Number of Children < 18 years, median (range) | 0 | 0–4 | |
| Attending college in the Fall | Yes, full-time | 80 | 14.4 |
| Yes, part-time | 17 | 3.1 | |
| No | 453 | 81.8 | |
| Missing | 4 | 0.7 |
Abbreviations: n = frequency, % = percentage, IQR = interquartile range, SD = standard deviation.
Categorical variables presented as n (%); normally distributed continuous variables presented as mean (SD); non-normally distributed continuous variables presented as median (IQR) or median (range).
2.4. Ethical approval
The University of Minnesota’s Institutional Review Board (IRB) reviewed and approved the study after determining that it met Exempt Category 2 guidelines.
2.5. Categorization of survey responses
To assess prior knowledge of herd immunity, we asked participants to select the correct definition from five options presented. Participants who chose ‘vaccinating enough people to protect even those who are not vaccinated’ were categorized as ‘knowledgeable about herd immunity’; all others were categorized as ‘not knowledgeable about herd immunity’.
To assess the vaccination coverage needed to prevent outbreaks (herd immunity), we categorized participants as ‘overestimated the reported herd immunity level’ if they estimated a level >75% (more than 5% over 70% coverage), as ‘underestimated the reported herd immunity level’ if they estimated a level < 65% (more than 5% under 70% coverage), and as ‘correct herd immunity level’ if they estimated within ±5% of 70% coverage.
To assess the vaccination coverage in participants’ own counties in the past year, we categorized participants as ‘overestimated the vaccination coverage’ if they estimated a level more than 5% over the reported coverage, as ‘underestimated the vaccination coverage’ if they estimated a level more than 5% under the reported coverage, and as ‘correct vaccination coverage’ if they estimated within ±5% of the reported coverage.
Plans to get vaccinated and concern about getting influenza were assessed on 5-point Likert scales. Participants were categorized as ‘planning to get vaccinated’ if they responded ‘extremely likely’ or ‘likely’, as ‘not planning to get vaccinated’ if they responded ‘extremely unlikely’ or unlikely’, and as ‘undecided’ if they responded ‘undecided’. Participants were categorized as ‘concerned about getting influenza’ if they responded ‘somewhat’, ‘moderately’, or ‘extremely’ concerned, and as ‘not concerned about getting influenza’ if they responded ‘not at all’ or ‘slightly’ concerned. The same categorization was used to categorize the responses for ‘concern about an influenza outbreak’.
2.6. Statistical methods
We aimed to evaluate the relationship between participants’ knowledge of herd immunity, estimates about influenza vaccination coverage, estimates about how high coverage needs to be to protect everyone, and participants’ plans to get vaccinated, concern about getting influenza, and their change in plans and concern before and after the intervention.
Chi-square tests were used to assess the univariate relationships between knowledge of herd immunity and expectations about vaccination coverage and (a) plans to vaccinate, (b) concern about influenza, and (c) concern about an outbreak. Multivariable logistic regression models were used to estimate the predicted probabilities of vaccination plans and concern about getting influenza for participants who were knowledgeable about herd immunity compared with those who were not knowledgeable. The probabilities of these two outcomes were estimated both before and after participants learned about herd immunity, the coverage needed for protection, the benefits of herd immunity, and the reported vaccination coverage in their county. All regression models controlled for age (in years), sex (male, female, other), race (white, non-white), ethnicity (Hispanic/Latino, non-Hispanic/ Latino), education level (High School Degree or less, Associates Degree, Bachelor’s Degree, Graduate Degree), county of residence (within Minneapolis/St. Paul metro area, outside metro) and whether participants had ever had an influenza vaccination (yes, no). Participants with missing responses could not be included in analyses where that response was required. The marginal standardization method was used to estimate the probabilities [21]. Predicted probabilities were multiplied by 100 and reported as percentages. Differences or changes in predicted percentages were reported for all regression models with 95% confidence intervals and p-values calculated using the bootstrap [22]. A significance level of 0.05 was used for all statistical tests. Stata 14 was used for data management and analysis [23].
3. Results
3.1. Participant characteristics
Of the 554 adults who completed the survey, the median age was 57 years, the majority were female (65.9%), white (91.0%), and non-Hispanic or Latino (93.9%) (Table 1). Participants were also highly educated with 56.9% reporting having a Bachelor’s degree or higher (Table 1).
3.2. Participant knowledge
3.2.1. Influenza vaccination
Overall, the majority of participants considered themselves somewhat or very knowledgeable about vaccines (79.9%) (Table 2). Medical professionals, including doctors, pediatricians, and nurses, were the most common primary source of information about vaccines (47.3%) (Table 2). Of the 86.8% of participants who reported having been vaccinated against influenza at least once in their lifetime, the majority (74.6%, n = 359) reported that they had received a flu vaccination last year and 64.0% (n = 308) reported that they had received a flu vaccine every year for the past ten years (Table 2). Respondents were most likely to identify their concern about influenza or concern about their health in general as the primary reason for vaccination (47.6%, n = 229) (Table 2). Of the 13.2% of all participants who indicated that they had never before received an influenza vaccine, 28.8% (n = 21) reported that the primary reason was that they never get sick while 17.8% (n = 13) noted that that they were concerned about potential side effects (Table 2).
Table 2.
Survey questions, description of the educational information provided, and distribution of responses from the 554 participants who completed the survey.
| Survey question | Responses | n | % |
|---|---|---|---|
| Which of the following sentences do you think describes the term ‘Herd Immunity’? | Vaccinating enough people to protect even those who are not vaccinated. | 348 | 62.8 |
| Vaccinating animals to protect humans from infection. | 109 | 19.7 | |
| Vaccinating only those at high risk for disease. | 48 | 8.7 | |
| Vaccinating adults and children several times within a year. | 45 | 8.1 | |
| Vaccinating children who have already had the disease. | 4 | 0.7 | |
| How knowledgeable would you say you are about vaccines? | Not very knowledgeable. | 111 | 20.0 |
| Somewhat knowledgeable. | 363 | 65.5 | |
| Very knowledgeable. | 80 | 14.4 | |
| Where do you most often hear about vaccines? | Doctors, pediatrician, or nurses. | 262 | 47.3 |
| TV, radio, or newspaper. | 138 | 24.9 | |
| Friends or family. | 61 | 11.0 | |
| Websites written by governmental groups like the Center for Disease Control (CDC) or the MN Department of Health. | 44 | 7.9 | |
| Other sources. | 28 | 5.1 | |
| Websites written by individuals or blog. | 11 | 2.0 | |
| I don’t usually hear about vaccines. | 10 | 1.8 | |
| At this point in the survey, participants were presented with information about influenza vaccination: | |||
| “Influenza and the “Flu” Vaccine | |||
| – The flu is a common respiratory illness. It is spread person to person by coughs and sneezes | |||
| – The flu causes fever, chills, cough, congestion, body aches, and fatigue. | |||
| – The flu can cause serious illness, hospitalization, and in rare cases, death. | |||
| – Flu vaccines are available every year before the flu season begins in the fall and everyone aged 6 months and older is recommended to get the vaccine. | |||
| – Some flu vaccines are given as a shot in the arm and some are sprayed into the nose.” | |||
| How concerned would you be that you might get the flu this year if you do not get the flu vaccine? | Not at all concerned. | 94 | 17.0 |
| Slightly concerned. | 113 | 20.4 | |
| Somewhat concerned. | 127 | 22.9 | |
| Moderately concerned. | 134 | 24.2 | |
| Extremely concerned. | 86 | 15.5 | |
| Have you EVER had a flu vaccine? | Yes | 481 | 86.8 |
| No | 73 | 13.2 | |
| If you have had a flu vaccine: What is the PRIMARY reason you got the flu vaccine? | I am concerned about flu or my health in general. | 229 | 47.6 |
| Doctor or other healthcare professional recommended it. | 111 | 23.1 | |
| My work or school requires it. | 76 | 15.8 | |
| My family members or friends recommended it. | 33 | 6.9 | |
| I am concerned about my loved ones getting sick. | 25 | 5.2 | |
| Other. | 7 | 1.5 | |
| [If you have had a flu vaccine]: Have you had a flu vaccine WITHIN the last year? | Yes. | 359 | 74.6 |
| No. | 116 | 24.1 | |
| I don’t know. | 6 | 1.3 | |
| [If you have had a flu vaccine]: How often have you received the flu vaccine in the past 10 years? | Once or twice. | 88 | 18.3 |
| Every few years. | 85 | 17.7 | |
| Every year. | 308 | 64.0 | |
| If you have NOT had a flu vaccine: What is the PRIMARY reason you have not had the flu vaccine? | I never get sick. | 21 | 28.8 |
| I’m concerned about potential side effects. | 13 | 17.8 | |
| Other. | 11 | 15.1 | |
| I don’t think the flu vaccine is effective. | 8 | 11.0 | |
| I don’t like needles. | 8 | 11.0 | |
| I have a medical condition and cannot get vaccinated. | 4 | 5.5 | |
| Vaccines are against my religious or personal beliefs. | 4 | 5.5 | |
| I did not know about this vaccine. | 3 | 4.1 | |
| Getting vaccinated is too expensive or time consuming. | 1 | 1.4 | |
| How likely are you to get the flu vaccine this year? | Extremely unlikely. | 75 | 13.5 |
| Unlikely. | 51 | 9.2 | |
| Undecided. | 64 | 11.6 | |
| Likely. | 67 | 12.1 | |
| Extremely likely. | 297 | 53.6 | |
| At this point in the survey, participants were presented with information about the concept of herd immunity: | |||
| “Herd Immunity | |||
| At the beginning of the survey, we asked you to choose the definition of herd immunity. | |||
| Herd immunity is vaccinating enough people to protect everyone and prevent outbreaks. | |||
| If a high enough percent of the population is vaccinated, EVERYONE benefits. | |||
| Even those who are not vaccinated will be protected from the disease. | |||
| For each disease, the percent of people who need to be vaccinated to ensure that everyone is protected is different”. | |||
| What do you think is the minimum percent of people who need to get the flu vaccine to protect everyone, even those who are not vaccinated (to reach herd immunity and prevent outbreaks)?a | Overestimated the reported herd immunity level. | 234 | 42.2 |
| Underestimated the reported herd immunity level. | 167 | 30.1 | |
| Estimated a herd immunity level within 5% of 70%. | 151 | 27.3 | |
| What percent of people in your county do you think got the flu vaccine last year?a,b | Overestimated the vaccination coverage. | 419 | 75.6 |
| Underestimated the vaccination coverage. | 55 | 9.9 | |
| Estimated a vaccination coverage within 5% of reported. | 76 | 13.7 | |
| At this point in the survey, participants were presented with the following information: | |||
| “At least 70% of a population needs to get the flu vaccine to protect EVERYONE, even those who are not vaccinated. | |||
| against the strains that match the vaccine. It is best if everyone over the age of 6 months is vaccinated”. | |||
| “Last year, XX% of [your] county got the flu vaccine.” [The reported vaccination coverage for the country of residence was presented here]. | |||
| With this in mind, how concerned are you that a flu outbreak might occur in your county this year? | Not at all concerned. | 51 | 9.2 |
| Slightly concerned. | 94 | 17.0 | |
| Somewhat concerned. | 176 | 31.8 | |
| Moderately concerned. | 150 | 27.1 | |
| Extremely concerned. | 83 | 15.0 | |
| With this in mind, how concerned would you be that you might get the flu this year if you did not get the flu vaccine? | Not at all concerned. | 65 | 11.7 |
| Slightly concerned. | 102 | 18.4 | |
| Somewhat concerned. | 122 | 22.0 | |
| Moderately concerned. | 135 | 24.4 | |
| Extremely concerned. | 130 | 23.5 | |
| With this in mind, how likely are you to receive the flu vaccine this year? | Extremely unlikely. | 67 | 12.1 |
| Unlikely. | 42 | 7.6 | |
| Undecided. | 60 | 10.8 | |
| Likely. | 73 | 13.2 | |
| Extremely likely. | 312 | 56.3 | |
Missing responses were not included here or in related analysis.
Participants were also asked to report the county in which they lived.
Overall, based on the survey responses alone without adjusting for any other factors or considering prior knowledge, before learning about herd immunity or vaccination coverage levels, 65.7% of participants reported that they were likely to get vaccinated in the upcoming year, while 22.7% were not planning to get vaccinated and 11.6% were undecided (Table 2).
3.2.2. Herd immunity
The majority of participants (62.8%) correctly identified the definition of herd immunity (Table 2). In unadjusted analyses, prior to the intervention, 79.9% of participants who were knowledgeable about herd immunity were planning to get vaccinated compared to only 64.6% of participants who were not knowledgeable (Chi-squared test of proportion; p = 0.0002); after the intervention, 81.8% of knowledgeable participants reported plans to get vaccinated compared to 70.9% of participants who were not knowledgeable (Chi-squared test of proportion; p = 0.005).
3.3. Expectations about local vaccination coverage and coverage needed to benefit from herd immunity
Minnesota county-level influenza vaccination coverage for 2015–2016 ranged from a low of 26.3% in Todd County to a high of 50.6% in Lincoln County. The majority of participants (80.7%) were residents of Hennepin, Ramsey, Dakota, Anoka, Washington, Olmsted, Scott, Chisago, Wright, and Carver counties (listed in descending order), where influenza vaccination coverage ranged from 27.2% to 40.8%. Only 13.7% of participants estimated the influenza vaccination coverage within 5% of the reported coverage in their own county (Table 2). The majority of participants (75.6%) assumed that vaccination coverage was higher than reported levels (Table 2), overestimating the percentage vaccinated by 28.0 percentage points on average (Fig. 1). Participants estimated a wide range of coverage levels needed to benefit from herd immunity; 30.1% thought that <65% coverage would be needed and 42.2% estimated that over 75% coverage would be needed (Table 2).
Fig. 1.
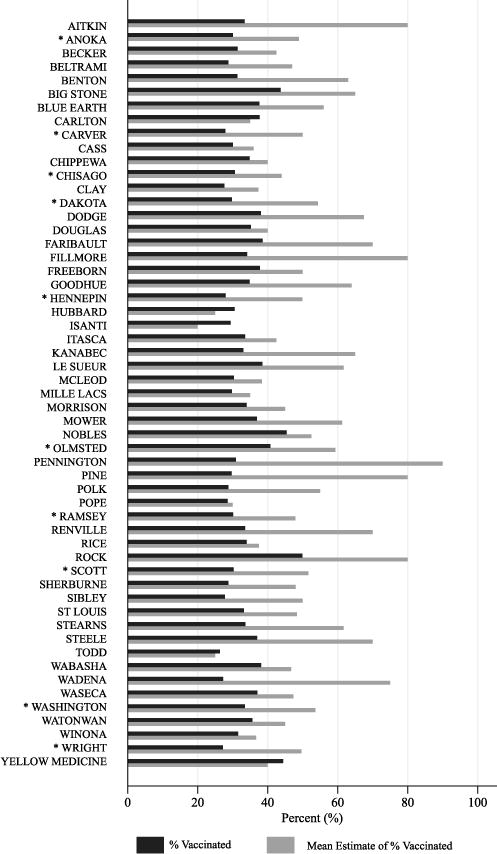
Comparison of the mean estimated influenza vaccination coverage given by participants compared to the reported coverage levels for each county in Minnesota. The majority of participants (80.7%) were residents of the following counties, denoted by (*): Hennepin, Ramsey, Dakota, Anoka, Washington, Olmsted, Scott, Chisago, Wright, and Carver (listed in descending order).
3.4. Impact of information about herd immunity and vaccination coverage on plans to be vaccinated
Results from the multivariable logistic regression model indicated that, before the educational information was presented, a significantly higher proportion of participants who were knowledgeable about herd immunity planned to get vaccinated compared with those who were not knowledgeable (78.9% [95% CI: 75.1–82.6%] versus 67.8% [95% CI: 61.3–74.2%]; p = 0.004) (Table 3). Significant increases in vaccination plans pre- and post-intervention were observed among participants who were not knowledgeable about herd immunity but not among those who were knowledgeable about herd immunity, as would be expected (Table 3). Among those who were not knowledgeable about herd immunity, the percentage planning to get vaccinated increased 7.3 percentage points (95% CI for the change: +3.1, 12.5) from 67.8% to 75.1% (p = 0.001) after learning about herd immunity (Table 3). While before the intervention, those knowledgeable about herd immunity were significantly more likely to have plans to be vaccinated than those not knowledgeable about herd immunity (p = 0.004), after the intervention, there was no significant difference between the two groups (p = 0.148) (Table 3).
Table 3.
Predicted percentages of those with plans to received influenza vaccination as estimated from a logistic regression model*
| Category | Subcategory | Before educational intervention (n = 434)
|
After educational intervention (n = 442)
|
Change before and after intervention
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % with plans to get vaccinated | Lower CI | Upper CI | P-value | % with plans to get vaccinated | Lower CI | Upper CI | P-value | Difference in % with plans to get vaccinated | Lower CI | Upper CI | P-value | ||
| Herd Immunity | Knowledgeable | 78.9 | 75.1 | 82.6 | ref | 80.1 | 76.5 | 83.7 | ref | 1.2 | −1.4 | 3.9 | 0.334 |
| Not knowledgeable | 67.8 | 61.3 | 74.2 | 0.004 | 75.1 | 69.6 | 80.6 | 0.148 | 7.3 | 2.7 | 12.5 | 0.001 | |
Model included the following covariates to adjust for potential confounding (age, sex, race, ethnicity, education, metro area residence, and history of influenza vaccination).
3.5. Impact of information about herd immunity and vaccination coverage on change in concern about influenza
In univariate analyses, a significantly higher proportion of participants who learned that the reported vaccination coverage in their county was lower than they expected were concerned about an outbreak occurring than those who found out that the coverage was higher than they expected (76.4% versus 63.6%; p = 0.04). However, there was no significant difference in concern about influenza between those who were knowledgeable and not knowledgeable about herd immunity before or after the intervention, though the proportion concerned increased significantly in both groups (Table 4).
Table 4.
Predicted percentages of those concerned about influenza as estimated from a logistic regression model*
| Category | Subcategory | Before educational intervention (n = 489)
|
After educational intervention (n = 489)
|
Change before and after intervention
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % concerned about influenza | Lower CI | Upper CI | P-value | % concerned about influenza | Lower CI | Upper CI | P-value | Difference in % concerned about influenza | Lower CI | Upper CI | P-value | ||
| Herd Immunity | Knowledgeable | 63.1 | 58.3 | 67.9 | ref | 69.9 | 65.2 | 74.5 | ref | 6.7 | 3.3 | 11.0 | <0.001 |
| Not knowledgeable | 62.7 | 56.3 | 69.2 | 0.926 | 71.1 | 65.2 | 77.0 | 0.745 | 8.4 | 3.1 | 15.2 | 0.004 | |
Model included the following covariates to adjust for potential confounding (age, sex, race, ethnicity, education, metro area residence, and history of influenza vaccination).
4. Discussion
We found that while the majority of participants were familiar with the concept of herd immunity, most incorrectly believed that the vaccination coverage in their county was higher than it actually was during the 2015–16 influenza season. Those who were least informed about herd immunity were the least likely to plan to get vaccinated before the intervention and also had the largest significant increase in the proportion willing to be vaccinated after receiving education about local vaccination coverage and the benefits of herd immunity. This suggests that educating individuals about the importance of the community benefits of vaccination, even when briefly providing basic information, could have important implications for improving vaccine uptake especially among those least knowledgeable.
A recently published study by Betsch et al. [24] evaluated the likelihood of vaccination when participants were told that their contribution to herd immunity protects a large proportion of their community. They concluded that communication about herd immunity benefits improved the willingness of individuals to consider vaccination and that social motives could increase vaccination rates when used as a tool for vaccine advocacy [24]. In our study, we tested a simple, novel intervention by educating respondents about the concept of herd immunity and the vaccination levels in their county, the latter being information that is not typically readily available to individuals. We found that this information led to changes in the proportion of individuals who planned to get vaccinated, suggesting higher vaccine acceptance, especially among those who were previously uninformed about herd immunity. Allison et al. conducted a cross-sectional survey about school-based immunization programs, and they found that if parents believed that influenza vaccination was a social norm, they were more likely to have their child immunized [25]. In this study, we have also demonstrated the value of informing individuals about local vaccination rates, even when vaccination rates are low. Future studies could further explore this concept by testing more complex and nuanced interventions that incorporate knowledge of local vaccination uptake into educational campaigns as part of efforts to increase vaccination. Our results also suggest that increases in plans to get vaccinated might be achieved if information about herd immunity and local vaccination rates were made available more widely. The potential impact of such an intervention on vaccination rates would require further investigation.
Our study explored the effects of learning about local vaccination rates and the community-level benefits of herd immunity on plans to get vaccinated during the upcoming year. We delivered an innovative educational intervention to examine whether information about herd immunity and local vaccination rates could impact individual plans to get vaccinated and concern about getting influenza immediately among a large sample of adults. However, our study may be limited in that we utilized a convenience sample, which is unlikely to be representative of the broader population given the demographic distribution; in addition, participants self-reported their influenza vaccination status, their history of influenza vaccination, their plans to get vaccinated in the future, and their concern about getting influenza. Further studies are needed to determine whether these self-reported changes translate into changes in actual vaccination rates; our study provides evidence to motivate researchers to investigate further. Other studies could also take into consideration the confidence that participants have in vaccinations or providers, access to affordable and convenient vaccinations, and whether complacency about vaccination exists as all could influence vaccine hesitancy.
The findings of our study present a first step towards investigating how learning local vaccination rates and the benefits of herd immunity may increase plans to get vaccinated. When participants were informed about herd immunity, the vaccination coverage in their county, and the vaccination coverage needed to prevent outbreaks, the percentage of participants with plans to get vaccinated increased significantly among those who were not previously knowledgeable about herd immunity when compared to those who were knowledgeable. Prior to the intervention, knowledgeable participants were more likely to have plans to vaccinate, while after the education was delivered, plans to get vaccinated increased among those who were not knowledgeable and there was no significant difference in the percent of participants with plans to vaccinate between those who were previously knowledgeable about herd immunity and those who were not.
5. Conclusions
Education about herd immunity and local vaccination coverage could be a useful tool in increasing vaccination rates and benefiting communities. After the intervention, a higher proportion of participants reported that they had plans to get vaccinated and were concerned about getting influenza after learning about herd immunity and the vaccination coverage in their county. Initially, those who were least informed about herd immunity were significantly less likely than those with some knowledge of herd immunity to plan to get vaccinated, but their willingness to vaccinate significantly increased after receiving education about local vaccination coverage and the benefits of herd immunity, closing the gap between the two groups and increasing the proportion planning to be vaccinated.
Acknowledgments
We thank Miriam Muscoplat from the Minnesota Department of Health for assistance with the Minnesota Immunization Information Connection (MIIC) data. This work was supported by the J.B. Hawley Student Research Award [Spring 2016 (PI: Jacqueline Logan)] and in part by the National Center for Advancing Translational Sciences of the National Institutes of Health Award [#UL1TR000114 (PI: Nicole E. Basta)]. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Footnotes
Conflict of interest statement
None.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Contributors’ statement
JL conducted the pilot study, collected data, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. DN coordinated the study, collected data, and reviewed and revised the manuscript. BG collected data and reviewed and revised the manuscript. BK conducted analyses, aided in interpreting results, and reviewed and revised the manuscript. JW aided in interpreting results, and reviewed and revised the manuscript. FAA assisted in conceptualizing and designing the study, collected data, and reviewed and revised the manuscript. NEB conceptualized and designed the study, collected data, directed the analysis, aided in interpreting results, drafted sections of the manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1.World Health Organization. Influenza (Seasonal) World Health Organization. 2016 [updated November 2016] Available from: < http://www.who.int/mediacentre/factsheets/fs211/en/>.
- 2.Cox RJ, Brokstad KA, Ogra P. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand J Immunol. 2004;59(1):1–15. doi: 10.1111/j.0300-9475.2004.01382.x. [DOI] [PubMed] [Google Scholar]
- 3.Plans-Rubio P. The vaccination coverage required to establish herd immunity against influenza viruses. Prev Med. 2012;55(1):72–7. doi: 10.1016/j.ypmed.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases. Seasonal Influenza Vaccine Effectiveness, 2005-2017. Centers for Disease Control and Prevention; 2017. [updated June 26, 2017] Available from: < https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm>. [Google Scholar]
- 5.Belongia EA, Simpson MD, King JP, Sundaram ME, Kelley NS, Osterholm MT, et al. Variable influenza vaccine effectiveness by subtype: a systematic review and meta-analysis of test-negative design studies. Lancet Infect Dis. 2016;16(8):942–51. doi: 10.1016/S1473-3099(16)00129-8. [DOI] [PubMed] [Google Scholar]
- 6.McLean HQ, Thompson MG, Sundaram ME, Kieke BA, Gaglani M, Murthy K, et al. Influenza vaccine effectiveness in the United States during 2012–2013: variable protection by age and virus type. J Infect Dis. 2015;211(10):1529–40. doi: 10.1093/infdis/jiu647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grohskopf LA, Sokolow LZ, Broder KR, Olsen SJ, Karron RA, Jernigan DB, et al. Prevention and Control of Seasonal Influenza with Vaccines Recommendations of the Advisory Committee on Immunization Practices — United States, 2016-17 Influenza Season. 2016 [updated Aug 26]. Available from: < https://www.cdc.gov/mmwr/volumes/65/rr/rr6505a1.htm>.
- 8.Healthy People 2020 Goals and Objectives for Immunization and Infectious Disease. United States Department of Health and Human Services Office of Disease Prevention and Health Promotion; Available from: < https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives>. [Google Scholar]
- 9.Santibanez TKK, Zhai Y, O’Halloran A, Liu L, Bridges C, Lu P-J, et al. Flu vaccination coverage, United States, 2015-16 Influenza Season. 2016 Available from: < https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm>.
- 10.Centers for Disease Control and Prevention. FluVaxView 2015-16 Influenza Season Vaccination Coverage Report. 2016 Available from: < https://www.cdc.gov/flu/fluvaxview/reportshtml/reporti1516/reporti/index.html>.
- 11.Basta NE, Chao DL, Halloran ME, Matrajt L, Longini IM., Jr Strategies for pandemic and seasonal influenza vaccination of schoolchildren in the United States. Am J Epidemiol. 2009;170(6):679–86. doi: 10.1093/aje/kwp237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52(7):911–6. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 13.Shim E, Chapman GB, Townsend JP, Galvani AP. The influence of altruism on influenza vaccination decisions. J R Soc Interface. 2012;9(74):2234–43. doi: 10.1098/rsif.2012.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vietri JT, Li M, Galvani AP, Chapman GB. Vaccinating to help ourselves and others. Med Decis Making. 2012;32(3):447–58. doi: 10.1177/0272989X11427762. [DOI] [PubMed] [Google Scholar]
- 15.Skea ZC, Entwistle VA, Watt I, Russell E. ’Avoiding harm to others’ considerations in relation to parental measles, mumps and rubella (MMR) vaccination discussions – an analysis of an online chat forum. Soc Sci Med. 2008;67(9):1382–90. doi: 10.1016/j.socscimed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Quadri-Sheriff M, Hendrix KS, Downs SM, Sturm LA, Zimet GD, Finnell SM. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics. 2012;130(3):522–30. doi: 10.1542/peds.2012-0140. [DOI] [PubMed] [Google Scholar]
- 17.Marshall H, Ryan P, Roberton D. Uptake of varicella vaccine–a cross sectional survey of parental attitudes to nationally recommended but unfunded varicella immunisation. Vaccine. 2005;23(46–47):5389–97. doi: 10.1016/j.vaccine.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 18.Flu Clinics University of Minnesota. 2017 Available from: < http://www.bhs.umn.edu/public-health/flu.htm>.
- 19.Minnesota Department of Health. MIIC and the Public. Available from: < http://www.health.state.mn.us/divs/idepc/immunize/registry/public.html>.
- 20.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962–70. doi: 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Localio AR, Margolis DJ, Berlin JA. Relative risks and confidence intervals were easily computed indirectly from multivariable logistic regression. J Clin Epidemiol. 2007;60(9):874–82. doi: 10.1016/j.jclinepi.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 23.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 24.Betsch CBR, Bohm R, Korn L, Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Human Behav. 2017;1(0056) [Google Scholar]
- 25.Allison MA, Reyes M, Young P, Calame L, Sheng X, Weng HY, et al. Parental attitudes about influenza immunization and school-based immunization for school-aged children. Pediatr Infect Dis J. 2010;29(8):751–5. doi: 10.1097/INF.0b013e3181d8562c. [DOI] [PubMed] [Google Scholar]


