Abstract
Background
Cardiovascular diseases, including acute myocardial infarction (AMI), are leading causes of death among the Japanese, who have the longest life expectancy in the world. Over the past 50 years in Japan, the percentage of elderly individuals has increased 4-fold, from 5.7% in 1960 to 23.1% in 2010. To explore medical practices and emergency care for AMI in this aging society, the Japan Acute Myocardial Infarction Registry (JAMIR) was established as a nationwide real-world database.
Methods
JAMIR conducted retrospective analysis of 20,462 AMI patients (mean age, 68.8 ± 13.3 years; 15,281 men [74.7%]) hospitalized between January 2011 and December 2013.
Results
The rates of ambulance use and emergency PCI were 78.9% and 87.9%, respectively. The median door-to-balloon time was 80 min (interquartile range, 53–143 min). Overall in-hospital mortality was 8.3%, including 6.6% due to cardiac death. JAMIR included 4837 patients aged ≥80 years (23.6%). In this age group, patients who underwent PCI (79.9%) had significantly lower in-hospital mortality than those who did not (11.1% vs. 36.9%, P < 0.001).
Conclusions
The large JAMIR database, with 24% of AMI patients aged ≥80 years, could provide useful information about medical care in an aging society. The reasonable in-hospital outcomes observed may justify consideration of PCI for patients with AMI aged ≥80 years.
Keywords: Acute myocardial infarction, Registry, Aging, Coronary intervention
1. Introduction
Japan is a society that leads the world in terms of population aging. The proportion of the population aged ≥65 years is estimated to increased to nearly 30% in 2025 and 40% in 2060 (http://www8.cao.go.jp/kourei/whitepaper/w-2016/html/zenbun/s1_1_5.html). According to the Ministry of Health, Labour and Welfare of Japan, life expectancy at birth in 2016 was approximately 80.8 years for men and 87.1 years for women (http://www.mhlw.go.jp/english/database/db-hw/lifetb16/dl/lifetb16-01.pdf). Cardiovascular diseases, including acute myocardial infarction (AMI), are leading causes of deaths in Japan (http://www.mhlw.go.jp/toukei/youran/aramashi/shibou.pdf). A nationwide database is therefore required to better prevent the onset and progression of AMI. Comprehensive information from Japan, with its rapidly aging population, will be crucial for developing future perspectives in other countries.
The Japan Acute Myocardial Infarction Registry (JAMIR) was established by integrating 10 regional registries. The present study analyzing the nationwide database was designed to explore medical practices and emergency care for AMI in the aging Japanese society.
2. Methods
2.1. The JAMIR study
Clinical data were collected from 10 representative regional AMI registry groups or institutions in Japan (Supplementary Fig. 1) (Supplementary Table) and analyzed retrospectively. Initially, 20,596 consecutive patients with spontaneous, acute universal classification type 1 myocardial infarction (MI) as proposed by the Joint European Society of Cardiology/American Heart Association/World Heart Federation Task Force [1] who were hospitalized within 24 h from onset between January 2011 and December 2013 were included. Criteria for AMI from the WHO MONICA Project (Monitoring of Trends and Determinants in Cardiovascular Disease) were also used when troponin levels were difficult to assess [2]. JAMIR did not include patients with AMI associated with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) (universal classification type 2) [1].
ST-segment elevation MI (STEMI) was diagnosed when ST elevation ≥1 mm was seen in at least two contiguous leads at any location on the index or qualifying electrocardiogram, when new left bundle branch block was presumed, or when new Q waves were observed. In the absence of ST-segment elevation, patients meeting the diagnostic criteria for MI were considered to have non-STEMI (NSTEMI).
Risk factors for cardiovascular disease were defined as hypertension (>140/90 mm Hg or use of antihypertensive medications), diabetes mellitus (fasting plasma glucose level of ≥126 mg/dL, 2-hour value of ≥200 mg/dL in a 75-g oral glucose tolerance test, casual plasma glucose level of ≥200 mg/dL, hemoglobin A1c ≥ 6.5%, or use of medications for diabetes mellitus), dyslipidemia (high-density lipoprotein cholesterol <40 mg/dL, low-density lipoprotein cholesterol ≥140 mg/dL, or use of lipid-lowering medications) [3], and current smoking (smoking within the preceding year). Emergency coronary angiography (CAG) and PCI were defined as procedures performed within 24 h from AMI onset. In the JAMIR study, the decision for reperfusion was made by the individual cardiologist in charge. Major outcomes in the present study were in-hospital mortality and cardiac mortality. The study was conducted in accordance with the tenets of the Declaration of Helsinki. The institutional review boards of all participating centers approved the present study.
2.2. Data analysis
Characteristic of patients and clinical variables were summarized as means with standard deviations. Categorical variables were expressed as numbers and percentages. Non-normally distributed continuous variables were expressed as medians (interquartile range). Continuous variables were compared using the t-test or Mann-Whitney U test, as appropriate. Categorical variables were analyzed using the chi-squared test. Logistic regression models were used to evaluate clinical variables that were significantly associated with in-hospital mortality. In addition, logistic regression was used to evaluate associations with adjusting for emergency PCI status and clinical variables. Statistical significance was defined as P < 0.05. All analyses were performed using the SAS software package version 9.4 (SAS Institute, Cary, NC, USA).
3. Results
3.1. Patient characteristics and outcomes
Of the 20,596 consecutive AMI patients, 134 patients aged <20 years were excluded. Ultimately, 20,462 patients (15,281 men and 5181 women) with a mean age of 68.8 ± 13.3 years were included. The age distribution of the study patients was as follows: <60 years, 4935 (24.1%); 60–69 years, 5169 (25.3%); 70–70 years, 5521 (27.0%); 80–89 years, 4074 (19.9%); and >90 years, 763 (3.7%). Table 1 summarizes the characteristics of the study patients. STEMI was diagnosed in 79.7% of patients. The rate of ambulance use was 78.9%. Importantly, 87.9% of patients underwent PCI, of whom 91.6% had a final TIMI grade of 3. PCI was inversely associated with high age (no PCI, 73.3 ± 14.0 vs. PCI, 67.8 ± 13.0 years; P < 0.0001), female sex (no PCI, 35.4% vs. PCI, 23.3%; P < 0.0001), Killip class ≥2 (no PCI, 47.6% vs. PCI, 25.0%; P < 0.0001) and culprit lesion in the left main trunk (LMT) (no PCI, 10.7% vs. PCI, 2.4%; P < 0.0001).
Table 1.
Characteristics of the study patients.
| Overall (n = 20,462) | Men (n = 15,281) | Women (n = 5181) | P | Age < 80 years (n = 15,625) | Age ≥ 80 years (n = 4837) | P | |
|---|---|---|---|---|---|---|---|
| Age, y | 68.8 ± 13.3 | 66.3 ± 12.9 | 76.0 ± 11.6 | <0.0001 | 63.7 ± 10.8 | 85.2 ± 4.3 | <0.001 |
| Men, % | 74.7 | 100.0 | 0.0 | – | 81.5 | 52.6 | <0.001 |
| STEMI, % | 79.7 | 80.3 | 77.7 | 0.0004 | 80.7 | 76.3 | <0.001 |
| Killip classification, % | <0.0001 | <0.001 | |||||
| 1 | 71.8 | 74.2 | 64.7 | 76.2 | 57.5 | ||
| 2 | 11.8 | 10.8 | 14.8 | 10.1 | 17.3 | ||
| 3 | 6.3 | 5.4 | 8.9 | 4.7 | 11.6 | ||
| 4 | 10.1 | 9.6 | 11.6 | 9.0 | 13.6 | ||
| Coronary risk factors, % | |||||||
| Hypertension | 63.6 | 61.7 | 68.9 | <0.0001 | 61.4 | 70.4 | <0.001 |
| Diabetes mellitus | 32.8 | 33.0 | 32.2 | 0.299 | 34.0 | 28.9 | <0.001 |
| Dyslipidemia | 46.2 | 46.7 | 44.5 | 0.010 | 49.9 | 34.8 | <0.001 |
| Active smoking | 34.5 | 42.1 | 11.9 | <0.0001 | 40.7 | 14.3 | <0.001 |
| Transportation, % | 0.046 | ||||||
| Ambulance | 78.9 | 78.6 | 79.7 | 78.3 | 80.8 | 0.043 | |
| Self | 18.3 | 18.7 | 17.2 | 19.1 | 15.8 | ||
| In-hospital onset | 2.8 | 2.7 | 3.1 | 2.6 | 3.4 | ||
| Emergency CAG, % | 89.6 | 91.6 | 83.9 | <0.0001 | 92.9 | 79.0 | <0.001 |
| Anterior MI, % | 47.6 | 47.8 | 47.2 | 0.495 | 48.1 | 45.8 | 0.010 |
| LMT culprit lesion, % | 3.0 | 3.2 | 2.4 | 0.020 | 2.9 | 3.4 | 0.186 |
| Primary PCI, % | 87.9 | 89.6 | 82.7 | <0.0001 | 90.3 | 79.9 | <0.001 |
| Door-to-balloon time, min | 80 (52–142) | 80 (51–139) | 85 (55–150) | 0.001 | 79 (51–138) | 87 (55–159) | <0.001 |
| Onset-to-balloon time, min | 230 (141–420) | 225 (138–408) | 237 (150–460) | <0.001 | 220 (138–398) | 250 (162–488) | <0.001 |
| Final TIMI flow, % | 0.279 | 0.002 | |||||
| 0 | 2.1 | 2.1 | 1.9 | 2.0 | 2.5 | ||
| 1 | 1.1 | 1.1 | 1.4 | 1.1 | 1.4 | ||
| 2 | 5.2 | 5.1 | 5.6 | 4.9 | 6.4 | ||
| 3 | 91.6 | 91.7 | 91.1 | 92.0 | 89.8 | ||
| In-hospital mortality, % | 8.3 | 6.9 | 12.4 | <0.0001 | 5.5 | 17.4 | <0.001 |
| Cardiac death | 6.6 | 5.2 | 10.4 | <0.0001 | 4.2 | 14.1 | <0.001 |
CAG, coronary angiography; LMT, left main trunk; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
In-hospital and cardiac death occurred in 8.3% and 6.6% of patients, respectively. The median door-to-balloon time was 81 min (interquartile range, 53–143 min). In-hospital mortality was associated with door-to-balloon time quartiles (0–52 min, 4.5%; 53–80 min, 5.1%; 81–142 min, 6.6%; 143–1440 min, 6.0%; P for trend = 0.003). In addition, in-hospital mortality by Killip class was as follows: Killip 1 (2.3%), Killip 2 (8.6%), Killip 3 (18.0%), and Killip 4 (41.9%), with P for trend <0.0001. A higher prevalence of Killip class ≥2 was observed with increasing age (<60 years, 17.2%; 60–69 years, 23.4%; 70–79 years, 29.9%; 80 years, 40.5%; ≥90 years, 53.8%; P for trend <0.001) (Supplementary Fig. 2).
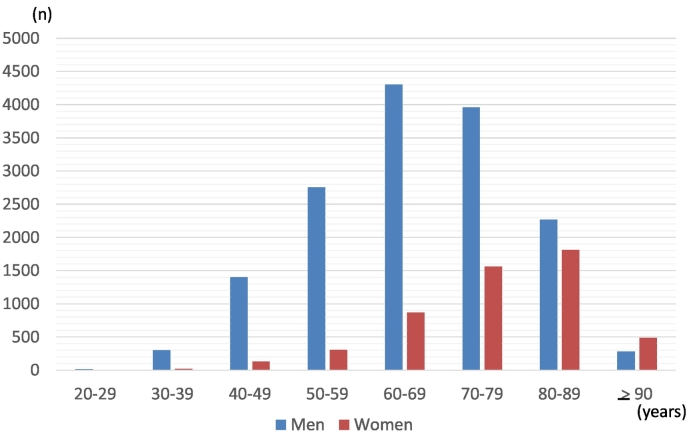
3.2. Sex differences and daily, weekly, and monthly variation in AMI
Fig. 1 shows the age distribution of study participants by gender. Women had a significantly higher mean age than men (76.0 ± 11.6 vs. 66.3 ± 12.9 years; P < 0.0001). Among men, the most common age group was 60–69 years, compared with 80–89 years in women. By gender, there were significant differences in the prevalence of STEMI (women, 77.7% vs. men, 80.3%; P = 0.0004), Killip class ≥2 (women, 35.3% vs. men, 25.8%; P < 0.0001) and hypertension (women, 68.9% vs. men, 61.7%; P < 0.0001) (Table 1). Emergency CAG (women, 83.9% vs. men, 91.6%; P < 0.0001) and primary PCI (women, 82.7% vs. men, 89.6%; P < 0.0001) were less commonly performed in women. Door-to-balloon time (women, 85 [55–150] vs. men, 80 [51–139] minutes; P = 0.001) and onset-to-balloon time (women, 237 [150–460] vs. men, 225 [138–408] minutes; P < 0.001) were significantly longer in women. In-hospital mortality (women, 12.4% vs. men; 6.9%; P < 0.0001) and cardiac mortality (women, 10.4% vs. men, 5.2%; P < 0.0001) were significantly higher in women.
Fig. 1.
Distribution of age among male (blue) and female (red) acute myocardial infarction patients
In the JAMIR study, 23.6% of patients were aged ≥80 years (n = 4837 [2543 men and 2294 women]).
JAMIR, Japan Acute Myocardial infarction Registry.
A circadian variation was observed among all AMI patients, with a peak at 8 AM (6.0%) and a trough at 1 AM (2.9%) (Supplementary Fig. 3A). The difference between peak and trough was significant (P < 0.001). However, a circadian variation with a morning surge was similarly observed in both sexes (Supplementary Fig. 4A left, P = 0.615) and patients aged <65 versus ≥65 years (Supplementary Fig. 4A right, P = 0.871). Regarding day of the week, AMI occurred most frequently on Mondays (15.3%) and least frequently on Sundays (13.4%) (Supplementary Fig. 3B), with a significant difference between these two days (P < 0.001). Patients aged <65 years seemed to have a higher incidence of AMI on Mondays compared to those aged ≥65 years (Supplementary Fig. 4B right, P = 0.076). However, there was no statistically significant difference by sex (Supplementary Fig. 4B left, P = 0.915). We also examined the seasonal variation in AMI. January (9.8%) was the most common month and September (7.3%) was the least common month (Supplementary Fig. 3C, P < 0.001) but this relationship was not significantly different by sex (Supplementary Fig. 4C left, P = 0.783) and age < 65 versus ≥65 years (Supplementary Fig. 4C right, P = 0.114).
3.3. AMI patients aged ≥80 years
In the JAMIR study, 23.6% of patients were aged ≥80 years (n = 4837 [2543 men and 2294 women]). Therefore, we performed subanalyses focusing on this age cut-off, comparing patients aged ≥80 and < 80 years (n = 15,625 [12,738 men and 2887 women]) (Table 1). Patients aged ≥80 years included a significantly lower proportion of males and patients with STEMI, and a higher proportion of patients with advanced Killip class. The rate of ambulance use was higher, door-to-balloon and onset-to-balloon times were longer, and PCI and successful recanalization (TIMI grade 3) rates were lower in patients aged ≥80 years. These factors might have contributed to higher in-hospital mortality (≥80 years, 17.4% vs. <80 years, 5.5%; P < 0.001) and cardiac mortality (≥80 years, 14.1% vs. <80 years, 4.2%; P < 0.001) among patients aged ≥80 years. Importantly, in patients aged ≥80 years, in-hospital mortality was 3-fold higher among those who did not undergo emergency PCI (36.9%) compared to those who underwent PCI (11.1%, P < 0.001). Although age was comparable between patients with STEMI and those with NSTEMI (STEMI; 85.1 ± 4.2 vs NSTEMI; 85.2 ± 4.2 years, P = 0.282) in patients aged ≥80 years, the rate of emergent PCI was higher in STEMI patients than that in NSTEMI patients (STEMI; 86.6 vs NSTEMI; 71.8%, P < 0.0001). Table 2 shows the results of a multivariate analysis of in-hospital mortality in patients aged ≥80 years; STEMI, advanced Killip class, dyslipidemia, anterior wall MI, and not undergoing PCI were independent predictors of in-hospital mortality.
Table 2.
Factors associated with in-hospital mortality in patients aged ≥80 years.
| Unadjusted |
Adjusted |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Male sex | 0.77 | 0.66–0.89 | 0.0005 | 1.23 | 0.91–1.66 | 0.18 |
| STEMI | 1.51 | 1.20–1.91 | 0.0004 | 1.81 | 1.20–2.72 | 0.005 |
| Killip classification | ||||||
| 1 | 1.00 | 1.00 | ||||
| 2–4 | 6.83 | 5.59–8.34 | <0.0001 | 4.99 | 3.63–6.85 | <0.0001 |
| Coronary risk factors | ||||||
| Hypertension | 0.99 | 0.83–1.18 | 0.91 | 1.08 | 0.78–1.50 | 0.65 |
| Diabetes mellitus | 1.01 | 0.85–1.21 | 0.89 | 1.03 | 0.75–1.42 | 0.84 |
| Dyslipidemia | 0.56 | 0.47–0.67 | <0.0001 | 0.52 | 0.37–0.74 | 0.0002 |
| Active smoking | 0.75 | 0.58–0.97 | 0.026 | 0.94 | 0.60–1.47 | 0.78 |
| Transportation | ||||||
| Ambulance | 1.60 | 1.26–2.04 | 0.0001 | 1.73 | 1.00–3.01 | 0.052 |
| Self | 1.00 | 1.00 | ||||
| In-hospital onset | 1.65 | 1.04–2.63 | 0.033 | 2.17 | 0.92–5.07 | 0.075 |
| Anterior MI | 1.71 | 1.43–2.06 | <0.0001 | 1.68 | 1.25–2.26 | 0.0006 |
| No emergency PCI | 4.71 | 3.96–5.60 | <0.0001 | 2.49 | 1.62–3.82 | <0.0001 |
MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
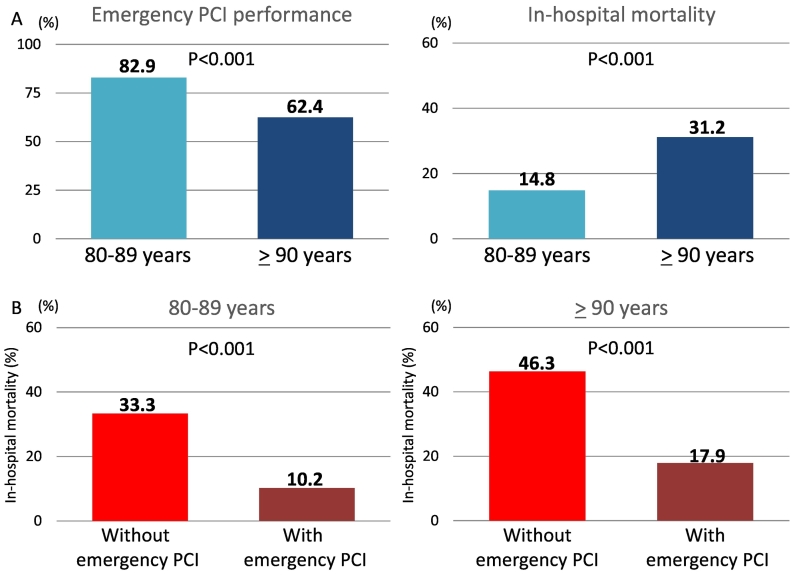
We then compared patients in their 80s (n = 4074) with patients in their 90s (n = 763). The proportion who underwent emergency PCI was lower (90s, 62.4% vs. 80s, 82.9%; P < 0.001) (Fig. 2A left) and in-hospital mortality was higher (90s, 31.2% vs. 80s, 14.8%; P < 0.001) among patients in their 90s (Fig. 2A right). Fig. 2B shows in-hospital mortality in these two age groups by PCI status. Among patients who underwent PCI, in-hospital mortality occurred in 10.2% of patients in their 80s and 17.9% in patients in their 90s, which was significantly lower than in those who did not undergo PCI (33.3% in 80s, P < 0.001; 46.3% in 90s, P < 0.001). Logistic regression analysis in patients aged ≥80 years revealed that emergency PCI was performed significantly more often in patients with STEMI (OR, 2.24; 95% CI, 1.62–3.10; P < 0.0001) but was less often performed in patients with Killip class ≥2 disease (OR, 0.50; 95% CI, 0.37–0.68: P < 0.0001). Patients in the 90s might be less likely to undergo emergency PCI (OR, 0.69; 95% CI, 0.44–1.08; P = 0.103).
Fig. 2.
A: Frequency of emergency PCI (left) and in-hospital mortality (right) in patients aged 80–89 years versus ≥ 90 years
B: In-hospital mortality in patients aged 80–89 years (left) and ≥ 90 years (right) with and without PCI.
PCI, percutaneous coronary intervention.
4. Discussion
The nationwide real-world JAMIR database with 20,462 AMI patients demonstrated that in-hospital mortality and cardiac mortality were 8.3% and 6.6%, respectively, with a high rate of ambulance use and emergency PCI. JAMIR data were characterized by the advanced age of the study population (24% of patients were aged ≥80 years). Reasonable in-hospital outcomes may justify consideration of PCI for patients of extremely advanced age with AMI.
4.1. Comparison of JAMIR and nationwide claims-based data
JAMIR is the largest registry consisting of 20,462 Japanese patients with AMI with a mean age of 68.8 ± 13.3 years (men, 66.3 ± 12.9 years; women, 76.0 ± 11.6 years) and overall in-hospital mortality of 8.3%. The Japanese Registry of All Cardiac and Vascular Diseases (JROAD)-DPC, using data from the Japanese Diagnosis Procedure Combination / Per Diem Payment System (DPC/PDPS), recently provided nationwide data from hospitalization records between April 1, 2012 and March 31, 2013. It has 35,824 patients with AMI [4]. The mean age of the male (n = 25,788, 72.0%) and female (n = 10,036, 28.0%) AMI patients was 67 ± 13 and 77 ± 13 years, respectively. Overall in-hospital mortality in patients with AMI was 14.5%. By Killip class, in-hospital mortality was 1.7% for Killip 1, 4.0% for Killip 2, 13.5% for Killip 3, and 47.5% for Killip 4. Important characteristics such as age, sex, and in-hospital mortality by Killip classification were similar between JAMIR and JROAD-DPC data. These validated findings indicate that the present nationwide JAMIR study may reflect the status of current AMI patients in Japan.
JAMIR additionally provided detailed data about medical practices and emergency care including ambulance use, direct PCI, and door-to-balloon time. Despite the high prevalence of STEMI among patients with advanced Killip class (28.2% of patients had ≥ class 2 disease), relatively low in-hospital mortality was associated with high performance of emergency care. Rates of ambulance use and emergency PCI were high, 78.9% and 87.9%, respectively, and the median door-to-balloon time was 80 min.
The present study confirmed that AMI onset was more common in the morning, on Mondays, and in the winter. Many studies have demonstrated that the onset of AMI had a distinct pattern, with a peak incidence in the morning within the first few hours after awakening [[5], [6], [7], [8]]. The early morning–awakening peak for AMI is related to circadian differences in endogenous levels of circulating catecholamines and other stress hormones and hypercoagulability during the early morning [7, 8]. Regarding the day of the week, a Monday predominance was observed for AMI [9]. Several potential triggering factors such as occupational stress, higher blood pressure, and unfavorable biochemical status have been proposed [[9], [10], [11]]. This study and past studies have shown a peak incidence of AMI during the winter and the lowest incidence during the summer. Social events, emotional reactions, physical activity, and low temperature during the winter could alter blood pressure, prothrombotic state, and myocardial oxygen supply, leading to increased ventricular wall stress and reduced coronary blood flow [[12], [13], [14], [15]].
4.2. Comparison of clinical characteristics among JAMIR and other registries
A large-scale, multi-center, nationwide JAMIR registry could allow for characterizing Japanese patients with AMI and medical practices and comparing them to those in other countries. Recently, representative nationwide registries of AMI include the Korea Acute Myocardial Infarction Registry-National Institute of Health (KAMIR-NIH) [16] and the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) [17]. The KAMIR-NIH registry included 13,624 patients (mean age, 64.1 years; male, 73.5%) enrolled between 2011 and 2015 from 20 centers. The PCI rate and in-hospital mortality were 87.4% and 3.9%, respectively. A disparity in in-hospital mortality may be related in part with the presentation and severity of AMI (STEMI, 48.2%; Killip class ≥2, 21.7%), although further studies are needed. The SWEDEHEART registry described temporal changes in treatment and outcomes from 1995 to 2014 in consecutive 105,674 patients with STEMI hospitalized at 72 hospitals. In particular, among the approximately 20,000 STEMI patients (median age, 69 [60–79] years; male, 68.4%) enrolled between 2011 and 2014, the PCI rate was over 75%. Despite relatively low in-hospital mortality (7.8–7.9% during 2011–2014 in the SWEDEHEART registry), the median time from symptom onset to primary PCI was 190 min. Taken together with the median onset-to-balloon time of 230 min in JAMIR, efforts to minimize onset-to-balloon time are recommended to improve clinical outcome in patients with STEMI.
Gender-related disparities continue to exist and AMI mortality in women remains substantial. KAMIR investigators previously demonstrated that cardiac death after AMI was more frequently observed in women than men, possibly because acute cardiac procedures were less commonly performed in women, who are older at AMI presentation [18]. Recently, the SWEEDHEART registry demonstrated that excess mortality among women was reduced after adjusting for the use of guideline-indicated treatments for AMI such revascularization therapies and medications [19]. The present JAMIR study demonstrated that in-hospital mortality and cardiac mortality were significantly higher in women, which might be associated with older age and fewer PCI procedures performed in women. Further prospective studies are needed to clarify whether an early invasive strategy could benefit patients, especially women, with AMI.
4.3. Impact of coronary intervention for patients aged ≥80 years
Although current guidelines recommend early coronary revascularization with PCI in patients with AMI, there has been very limited information of its use in patients aged ≥80 years, in particular those aged ≥90 years. One of the unique features of JAMIR was the advanced age of the study population, with a substantial proportion of patients being ≥80 years (n = 4837, 24%). This age group had a PCI rate of 79.9% (80s, 82.9% and 90s, 62.4%) and in-hospital mortality of 17.4% (80s, 14.8% and 90s, 31.2%). In the KAMIR registry (n = 14,885, 2005–2007), 2415 AMI patients (16%) were aged ≥80 years. The PCI rate was 71.7% in patients in their 80s and 57.2% in patients in their 90s (overall, 70.1%) and in-hospital mortality was 11.4% in patients in their 80s and 15.7% in patients in their 90s [20]. Lower in-hospital mortality despite a lower PCI rate in KAMIR compared to JAMIR might be related in part to AMI presentation and severity. In the London Heart Attack Group Cohort (n = 10,249, all treated with PCI, 2005–2011), 1051 STEMI patients (10.3%) were ≥ 80 years and had in-hospital mortality of 7.7% (2.2% in patients aged <80 years treated with PCI) [21].
In this JAMIR study, in addition to STEMI, advanced Killip class, and anterior wall MI, non-emergency PCI was an independent factor for in-hospital mortality in patients aged ≥80 years. Considering the results of our multivariate analysis, AMI patients aged ≥80 years with complicated conditions may benefit from emergency PCI. Recently, the After Eighty study, a randomized, controlled multicenter trial, revealed that an invasive strategy such as PCI was superior to a conservative strategy in patients aged ≥80 years with NSTEMI or unstable angina. However, the efficacy of an invasive strategy may be attenuated in patients aged over approximately 90 years [22]. Advances in PCI technology (e.g., new generation DES) and techniques (e.g., the transradial approach) and pharmacotherapy (e.g., tailored antithrombotic therapy) over the past decade have led to better outcomes and a lower risk of complications [23].
Our study has some limitations. As a retrospective observational study, residual confounding or selection bias cannot be completely excluded as an alternative explanation of our findings. The database merged several registries and intertrial variability in care may have influenced results in the present pooled patient population. Our study findings only apply to AMI patients with onset-to-door time ≤ 24 h. Several agents such as P2Y12 inhibitors are critical not only for the improvement of prognosis in AMI patients but also for the safety including bleeing in particular in advanced age population. However, the data of these agents as well as dislipidemic status were not included in this study and therefore further study is needed.
5. Conclusions
The large-scale JAMIR database of patients with AMI could provide useful information about medical care in the aging society of Japan. In this registry characterized by the advanced age of the study population, with one-quarter of AMI patients aged ≥80 years, reasonable in-hospital outcomes may justify consideration of PCI for very elderly patients with AMI.
The following are the supplementary data related to this article.
Supplementary Fig. 1 Ten regional registries make up the Japan Acute Myocardial Infarction Registry (JAMIR).
Supplementary Fig. 2 Distribution of Killip class in 5 age groups: <60 years (n = 4935), 60–69 years (n = 5169), 70–79 years (n = 5521), 80–89 years (n = 4074), and ≥ 90 years (n = 763).
Blue, red, green, and purple bars show Killip classes 1, 2, 3, and 4, respectively.
Supplementary Fig. 3 Variation in acute myocardial infarction onset by (A) time of day, (B) day of the week, and (C) month (n = 20,462).
Supplementary Fig. 4 Variations in acute myocardial infarction onset by (A) time of day, (B) day of the week, and (C) month stratified by sex (men, blue; women, orange) and age group (<65 years, green; ≥65 years, blue).
The detail of 10 regional registries consisting of the Japan Acute Myocardial Infarction Registry (JAMIR) and their related articles.
Sources of support
This work was supported in part by a Grant-in-Aid for Scientific Research (17K09542) from the Ministry of Education, Science, and Culture, Japan. There are no financial or other relationships that could lead to a conflict of interest.
Conflict of interest
There are no financial or other relationships that could lead to a conflict of interest.
Contributor Information
Kazuo Kimura, Email: c-kimura@urahp.yokohama-cu.ac.jp.
Satoshi Yasuda, Email: yasuda.satoshi.hp@mail.ncvc.go.jp.
Appendix A. JAMIR Investigators
Sapporo ACS Network: Takashi Takenaka (Hokkaido Medical Center), Daisuke Hotta (Hokkaido Cardiovascular Hospital); Iwate ACS Registry: Tomonori Itoh (Iwate Medical University School of Medicine); Yamagata AMI Registry: Tetsu Watanabe (Yamagata University School of Medicine); Miyagi AMI Registry Study: Kiyotaka Hao (Tohoku University); Jichi Medical University: Kazuomi Kario; Tokyo CCU Network: Takeshi Yamamoto (Nippon Medical School Hospital); Naoki Sato (Nippon Medical School Musashi-Kosugi Hospital); Atsuo Namiki (Kanto Rosai Hospital); Hiroshi Suzuki (Showa University Fujigaoka Hospital); Makoto Suzuki (Sakakibara Heart Institute); Yokohama Cardiovascular Workshop: Masami Kosuge (Yokohama City University Medical Center); Mie ACS Registry Masaaki Ito (Mie University); Takashi Tanigawa (Matsusaka Chuo Hospital); NCVC AMI Registry: Yasuhide Asaumi (National Cerebral and Cardiovascualr Center); Kumamoto Acute Coronary Events Study: Kenichi Tsujita (Kumamoto University); JAMIR data center: Yoshihiro Miyamaoto (National Cerebral and Cardiovascualr Center).
References
- 1.Thygesen K., Alpert J.S., Jaffe A.S., Simoons M.L., Chaitman B.R., White H.D., Joint ESCAAHAWHFTFftUDoMI, Katus H.A., Lindahl B., Morrow D.A., Clemmensen P.M., Johanson P., Hod H., Underwood R., Bax J.J., Bonow R.O., Pinto F., Gibbons R.J., Fox K.A., Atar D., Newby L.K., Galvani M., Hamm C.W., Uretsky B.F., Steg P.G., Wijns W., Bassand J.P., Menasche P., Ravkilde J., Ohman E.M., Antman E.M., Wallentin L.C., Armstrong P.W., Simoons M.L., Januzzi J.L., Nieminen M.S., Gheorghiade M., Filippatos G., Luepker R.V., Fortmann S.P., Rosamond W.D., Levy D., Wood D., Smith S.C., Hu D., Lopez-Sendon J.L., Robertson R.M., Weaver D., Tendera M., Bove A.A., Parkhomenko A.N., Vasilieva E.J., Mendis S. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–2035. [Google Scholar]
- 2.Tunstall-Pedoe H., Kuulasmaa K., Amouyel P., Arveiler D., Rajakangas A.M., Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 3.Teramoto T., Sasaki J., Ishibashi S., Birou S., Daida H., Dohi S., Egusa G., Hiro T., Hirobe K., Iida M., Kihara S., Kinoshita M., Maruyama C., Ohta T., Okamura T., Yamashita S., Yokode M., Yokote K., Japan Atherosclerosis S. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan −2012 version. J. Atheroscler. Thromb. 2013;20:517–523. doi: 10.5551/jat.15792. [DOI] [PubMed] [Google Scholar]
- 4.Yasuda S., Nakao K., Nishimura K., Miyamoto Y., Sumita Y., Shishido T., Anzai T., Tsutsui H., Ito H., Komuro I., Saito Y., Ogawa H. On the behalf of JI. The current status of cardiovascular medicine in Japan- analysis of a large number of health records from a Nationwide claim-based database, JROAD-DPC. Circ. J. 2016;80:2327–2335. doi: 10.1253/circj.CJ-16-0196. [DOI] [PubMed] [Google Scholar]
- 5.Hammoudeh A.J., Alhaddad I.A. Triggers and the onset of acute myocardial infarction. Cardiol. Rev. 2009;17:270–274. doi: 10.1097/CRD.0b013e3181bdba75. [DOI] [PubMed] [Google Scholar]
- 6.Culic V., Eterovic D., Miric D. Meta-analysis of possible external triggers of acute myocardial infarction. Int. J. Cardiol. 2005;99:1–8. doi: 10.1016/j.ijcard.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Cohen M.C., Rohtla K.M., Lavery C.E., Muller J.E., Mittleman M.A. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am. J. Cardiol. 1997;79:1512–1516. doi: 10.1016/s0002-9149(97)00181-1. [DOI] [PubMed] [Google Scholar]
- 8.Gnecchi-Ruscone T., Piccaluga E., Guzzetti S., Contini M., Montano N., Nicolis E. Morning and Monday: critical periods for the onset of acute myocardial infarction. The GISSI 2 Study experience. Eur. Heart J. 1994;15:882–887. doi: 10.1093/oxfordjournals.eurheartj.a060605. [DOI] [PubMed] [Google Scholar]
- 9.Willich S.N., Lowel H., Lewis M., Hormann A., Arntz H.R., Keil U. Weekly variation of acute myocardial infarction. Increased Monday risk in the working population. Circulation. 1994;90:87–93. doi: 10.1161/01.cir.90.1.87. [DOI] [PubMed] [Google Scholar]
- 10.Murakami S., Otsuka K., Kubo Y., Shinagawa M., Yamanaka T., Ohkawa S., Kitaura Y. Repeated ambulatory monitoring reveals a Monday morning surge in blood pressure in a community-dwelling population. Am. J. Hypertens. 2004;17:1179–1183. doi: 10.1016/j.amjhyper.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 11.Urdal P., Anderssen S.A., Holme I., Hjermann I., Mundal H.H., Haaland A., Torjesen P. Monday and non-Monday concentrations of lifestyle-related blood components in the Oslo diet and exercise study. J. Intern. Med. 1998;244:507–513. doi: 10.1046/j.1365-2796.1998.00395.x. [DOI] [PubMed] [Google Scholar]
- 12.Wilkinson P., Pattenden S., Armstrong B., Fletcher A., Kovats R.S., Mangtani P., McMichael A.J. Vulnerability to winter mortality in elderly people in Britain: population based study. BMJ. 2004;329:647. doi: 10.1136/bmj.38167.589907.55. (Clinical researched) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woodhouse P.R., Khaw K.T., Plummer M., Foley A., Meade T.W. Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet. 1994;343:435–439. doi: 10.1016/s0140-6736(94)92689-1. [DOI] [PubMed] [Google Scholar]
- 14.Culic V. Seasonal distribution of acute myocardial infarction: a need for a broader perspective. Int. J. Cardiol. 2006;109:265–266. doi: 10.1016/j.ijcard.2005.03.074. [DOI] [PubMed] [Google Scholar]
- 15.Marchant B., Ranjadayalan K., Stevenson R., Wilkinson P., Timmis A.D. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: the influence of environmental temperature. Br. Heart J. 1993;69:385–387. doi: 10.1136/hrt.69.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim J.H., Chae S.C., Oh D.J., Kim H.S., Kim Y.J., Ahn Y., Cho M.C., Kim C.J., Yoon J.H., Park H.Y., Jeong M.H. Korea acute myocardial infarction-National Institutes of Health Registry I. Multicenter cohort study of acute myocardial infarction in Korea-interim analysis of the Korea acute myocardial infarction registry-National Institutes of Health Registry. Circ. J. 2016;80:1427–1436. doi: 10.1253/circj.CJ-16-0061. [DOI] [PubMed] [Google Scholar]
- 17.Szummer K., Wallentin L., Lindhagen L., Alfredsson J., Erlinge D., Held C., James S., Kellerth T., Lindahl B., Ravn-Fischer A., Rydberg E., Yndigegn T., Jernberg T. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995–2014. Eur. Heart J. 2017;38:3056–3065. doi: 10.1093/eurheartj/ehx515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korea Acute Myocardial Infarction Registry I, Lee K.H., Jeong M.H., Ahn Y.K., Kim J.H., Chae S.C., Kim Y.J., Hur S.H., Seong I.W., Hong T.J., Choi D., Cho M.C., Kim C.J., Seung K.B., Chung W.S., Jang Y.S., Cho J.G., Park S.J., Other Korea Acute Myocardial infarction Registry I Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int. J. Cardiol. 2008;130:227–234. doi: 10.1016/j.ijcard.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 19.Alabas O.A., Gale C.P., Hall M., Rutherford M.J., Szummer K., Lawesson S.S., Alfredsson J., Lindahl B., Jernberg T. Sex differences in treatments, relative survival, and excess mortality following acute myocardial infarction: National Cohort Study Using the SWEDEHEART Registry. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.007123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee K.H., Ahn Y., Kim S.S., Rhew S.H., Jeong Y.W., Jang S.Y., Cho J.Y., Jeong H.C., Park K.H., Yoon N.S., Sim D.S., Yoon H.J., Kim K.H., Hong Y.J., Park H.W., Kim J.H., Cho J.G., Park J.C., Jeong M.H., Cho M.C., Kim C.J., Kim Y.J., Investigators K. Characteristics, in-hospital and long-term clinical outcomes of nonagenarian compared with octogenarian acute myocardial infarction patients. J. Korean Med. Sci. 2014;29:527–535. doi: 10.3346/jkms.2014.29.4.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bromage D.I., Jones D.A., Rathod K.S., Grout C., Iqbal M.B., Lim P., Jain A., Kalra S.S., Crake T., Astroulakis Z., Ozkor M., Rakhit R.D., Knight C.J., Dalby M.C., Malik I.S., Mathur A., Redwood S., MacCarthy P.A., Wragg A. Outcome of 1051 octogenarian patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: observational cohort from the London heart attack group. J. Am. Heart Assoc. 2016;5 doi: 10.1161/JAHA.115.003027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tegn N., Abdelnoor M., Aaberge L., Endresen K., Smith P., Aakhus S., Gjertsen E., Dahl-Hofseth O., Ranhoff A.H., Gullestad L., Bendz B., After Eighty Study I Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (after eighty study): an open-label randomised controlled trial. Lancet. 2016;387:1057–1065. doi: 10.1016/S0140-6736(15)01166-6. [DOI] [PubMed] [Google Scholar]
- 23.Shanmugam V.B., Harper R., Meredith I., Malaiapan Y., Psaltis P.J. An overview of PCI in the very elderly. J. Geriatr. Cardiol. 2015;12:174–184. doi: 10.11909/j.issn.1671-5411.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Fig. 1 Ten regional registries make up the Japan Acute Myocardial Infarction Registry (JAMIR).
Supplementary Fig. 2 Distribution of Killip class in 5 age groups: <60 years (n = 4935), 60–69 years (n = 5169), 70–79 years (n = 5521), 80–89 years (n = 4074), and ≥ 90 years (n = 763).
Blue, red, green, and purple bars show Killip classes 1, 2, 3, and 4, respectively.
Supplementary Fig. 3 Variation in acute myocardial infarction onset by (A) time of day, (B) day of the week, and (C) month (n = 20,462).
Supplementary Fig. 4 Variations in acute myocardial infarction onset by (A) time of day, (B) day of the week, and (C) month stratified by sex (men, blue; women, orange) and age group (<65 years, green; ≥65 years, blue).
The detail of 10 regional registries consisting of the Japan Acute Myocardial Infarction Registry (JAMIR) and their related articles.