Abstract
Ganglions are the cysts derived from myxomatous degeneration of periarticular tissue, commonly found around wrist and foot. Ganglion cysts are uncommon in Knee region and if present their occurrence is mostly incidental and benign. Based on their location, this could be extraarticular or intraarticular. Lesions with similar pathology in subchondral region around joints are lesser common entity called Intraosseous ganglions. Rarer still is the lesion produced by myxomatous degeneration of periosteum of long bone, called periosteal ganglion. We here present a case of 35 year old Male with gradual onset, poorly localised pain behind left knee which was radiologically suggestive of periosteal ganglion, eroding the posterior aspect of femur and confirmed histopathologically following the excision of a lesion from posterior aspect of femoral condyles.
Keywords: Periosteal ganglion, Benign cysts around knee, Intercondylar cyst
1. Introduction
A ganglion cyst is defined as a benign cystic mass that is surrounded by dense connective tissue, without a synovial lining and is filled with a gelatinous fluid rich in hyaluronic acid and other mucopolysaccharides. Ganglia are traditionally divided into the following categories: intra-articular, extra-articular, intraosseous and (rare) periosteal.1 Periosteal ganglions are thought to be derived from myxomatous degeneration of periosteum of long bones. This are often associated with sinister pathology such as cortical erosion, periosteal reaction, compression of overlying tissues and intraarticular meniscal extension.2, 3 These are very rare occurrence with only few cases reported in literature.4, 5, 6 We report a clinical case of this lesser known ganglion in disguise, located atypically in the posterior femoral intercondylar region, which was excised alongwith adjoining periosteum and confirmed histopathologically to be benign ganglionic cyst.
2. Case report
A 35 year old male, presented with chief complaints of pain over popliteal region(left side) since 2 months. It was dull aching, poorly localised, aggravated by walking with painful full flexion. There was no history of trauma, fever and past history was not remarkable apart from patient being Hepatitis B Reactive. On palpation, diffuse swelling, fluctuant, tender and not fixed to overlying skin was evident.
Plain radiograph was essentially normal(Fig. 1). So further investigation with MRI was done. MRI showed loculated, cystic hyperintense lesion on the posterior aspect of femur lower end suggestive of periosteal ganglion cyst sized 17 mm × 15 mm. (Fig. 2, Fig. 3, Fig. 4).
Fig. 1.
Plain radiograph showing little soft tissue shadow on posterior aspect of femoral condyle.
Fig. 2.
MRI Images: T1 and T2 images showing sagittal section of knee with hyperintense lesion on posterior femoral condyle above gastrocnemius origin.
Fig. 3.
MRI Images: T1 and Fat-Suppressed images showing transverse section of knee with hyperintense lesion on posterior femoral condyle. This image shows vicinity of lesion with major vessels.
Fig. 4.
MRI Images: Fat suppressed sagittal section of knee showing multiloculated nature of lesion and no continuation with joint.
Surgical excision of the lesion was done using posterior approach. (Fig. 5). Intraoperatively, the lesion was measured to be 25 mm × 19 mm, multiloculated, lobulated arising from underlying periosteum. (Fig. 6, Fig. 7) Cortex beneath lesion was roughened but no scalloping. There was no tract connecting to knee joint or endosteal breach of cortex. Histologically, tissue overlying the lesion was in continuity with the adjacent normal periosteum of femur and had focal areas of myxomatous degeneration within. It possessed an inner lining of pseudosynovial cells and fibrous tissue covering outside, consistent with the diagnosis of a benign ganglion cyst arising from periosteum. (Fig. 8)
Fig. 5.
Posterior approach to knee taken with midline S shaped incision on posterior aspect of knee.
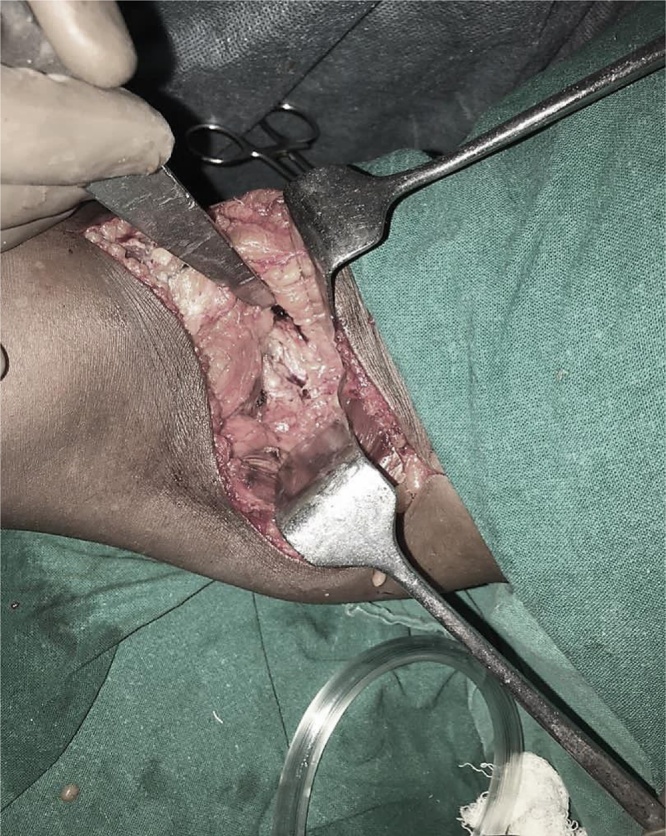
Fig. 6.
Retraction of surrounding tissues to make visible the underlying periosteal ganglion.
Fig. 7.
Completely excised ganglion cyst measuring 25 mm × 19 mm.
Fig. 8.
Histopathology showing pseudosynovial cells arranged in cuboidal pattern enclosing gelatinous mucin.
On follow up after 3 months, patient did not have pain and full Range of movements.
3. Discussion
Mucoid degeneration and ganglionic cysts arising from periosteum around knee are rather rare lesions. Ganglions are postulated to be cystic lesions with fibrous capsule arising from juxta-articular soft tissue enclosing soft gelatinous matter.1 Depending on location these could be either extraarticular or intraarticular. The next common location of them being intraosseous. Intraosseous ganglions are usually seen in long bones near the joint space in epiphyseal-metaphyseal region; often within subchondral region or near ligament insertion.7, 8, 9 These are usually found in medial malleolus, femoral head and proximal tibia.10
Periosteal ganglion are rarest of ganglionic varieties with very sparse mentioning in scientific literature.It was first described by Olliers (1864) and Poncet (1874) as a peculiar form of periostitis; “periostitis albuminosa” or “ganglion periostale.”4, 11 Common appearance of this cysts are long bones of lower limb, peculiarly near pes anserinus of proximal tibia. Other locations are distal end of ulna, radius, femur, medial malleolus and ilium.4, 5, 11
The etiological reason for appearance of periosteal ganglion is largely unknown. Repetitive stress and trauma are speculated causes. Periosteal connective tissue undergoes mucoidal degeneration and fibroblastic proliferation occurs which inturn produces intercellular mucin and collagen. Collagen alongwith fibroblasts makes up the outer fibrous wall. While mucin makes up gelatinous content to form cystic lesion. The inner cells of wall are clubbed cuboidally to give a pseudosynovial appearance.6
Periosteal ganglions show little male preponderance and appear commonly in age group 40–50 years. Usual presentation is swelling, diffuse tenderness and occasional derangement of joint.5 Unusual presentation occurs in ganglions associated with major vessels and nerves. Major vessel may bleed into ganglion such that it becomes hot, swollen, red and painful.12 Nerve compression by ganglion can lead to paresthesia, associated muscular dystrophy and fatty infiltration as visible in MRI.13
MRI shows multilobulated cyst-like mass in vicinity to periosteum which is hypo/iso-intense to muscle and surrounding bony cortex. However, it appears hyperintense due to rich protein content in T-2 weighed images.
Other differential diagnoses for this lesion include parosteal lipoma, periosteal aneurysmal bone cyst, subperiosteal abscess or hematoma, periosteal chondroma and hydatid cyst.
Definitive diagnoses of this lesion is established after histopathological examination is done post-excision. Periosteal ganglions are considered benign cysts with usually good prognosis. However recurrence still remains a major issue; particularly when communication between ganglion and adjacent joint is not excised, surrounding bone with periosteum is not excised, and when further mucoid degeneration occurs in connective tissues occupying the surgical defect.6
Conflict of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
Dr Maitry Shah. Senior Resident, Paediatrics Department, Smt. N.H.L. Municipal medical College, Ahmedabad. For linguistic support.
Dr Shimul Patel. Resident, Pathology Department, Smt. N.H.L. Municipal Medical College, Ahmedabad. For histopathological study.
Contributor Information
Padmanabh H. Vora, Email: dr.padm.vora@gmail.com.
Neel M. Bhavsar, Email: drnmbortho@gmail.com.
Rameez Musa, Email: musarameez@gmail.com.
Ajay Trivedi, Email: ajaytrivedi682@gmail.com.
Prarthan Amin, Email: petzamin@gmail.com.
References
- 1.Perdikakis E., Skiadas V. MRI characteristics of cysts and cyst-like lesions in and around the knee: what the radiologist needs to know. Insights Imaging. 2013;4(3):257–272. doi: 10.1007/s13244-013-0240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy E.F., Matz S., Steiner G.C., Dorfman H.D. Periosteal ganglion: a cause of cortical bone erosion. Skeletal Radiol. 1983;10:243–246. doi: 10.1007/BF00357897. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi H., Kotoura Y., Hosono M., Tsuboyama T., Sakahara H., Koinishi J. Periosteal ganglion of the tibia. Skeletal Radiol. 1996;25:381–383. doi: 10.1007/s002560050099. [DOI] [PubMed] [Google Scholar]
- 4.Valls R., Melloni P., Darnell A., Munoz J., Canalies J. Diagnostic imaging of tibial periosteal ganglion. Eur Radiol. 1997;7:70–72. doi: 10.1007/s003300050112. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson N.N., Asarch A., Tschetter A.J., Stone M. Periosteal ganglia presenting as subcutaneous nodules on the tibia. JAMA Dermatol. 2014;150:663–664. doi: 10.1001/jamadermatol.2013.6352. [DOI] [PubMed] [Google Scholar]
- 6.Byers Paul D., Wadsworth Thomas G. Periosteal ganglion. J Bone Joint Surg. 1970;52-B:290–295. [PubMed] [Google Scholar]
- 7.Williams H.J., Davies A.M., Allen G., Evans N., Mangham D.C. Imaging features of intraosseous ganglia: a report of 45 cases. Eur Radiol. 2004;14:1761–1769. doi: 10.1007/s00330-004-2371-8. [DOI] [PubMed] [Google Scholar]
- 8.Battaglia T.C., Freilich A.M., Diduch D.R. An intra-articular knee cyst in a 2-year-old associated with an aberrant anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15:36–38. doi: 10.1007/s00167-006-0119-5. [DOI] [PubMed] [Google Scholar]
- 9.Başbozkurt M., Hapa O., Demiralp B. Distal femoral intraosseous ganglia: cause or result of a degenerative process: 17-year follow-up of a case. Musculoskelet Surg. 2011;95:147–150. doi: 10.1007/s12306-011-0113-z. [DOI] [PubMed] [Google Scholar]
- 10.Schajowicz F., Clavel Sainz M., Slullitel J.A. Juxta-articular bone cysts (intra-osseous ganglia): A clinicopathological study of eighty eight cases. J Bone Joint Surg. 1979;61-B:107–116. doi: 10.1302/0301-620X.61B1.422629. [DOI] [PubMed] [Google Scholar]
- 11.Reghunath A., Mittal M.K., Khanna G., Anil V. Tibial periosteal ganglion cyst: the ganglion in disguise. Indian J Radiol Imaging. 2017;27(1):105–109. doi: 10.4103/0971-3026.202953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry M., Heyse-Moore G.H. Acute haemorrhage into a subperiosteal ganglion. J Bone Joint Surg. 1990;72-B:519. doi: 10.1302/0301-620X.72B3.2341461. [DOI] [PubMed] [Google Scholar]
- 13.De Maeseneer M., De Boeck H., Shahabpour M., Hoorens A., Oosterlinck D., Van Tiggelen R. Subperiosteal ganglion cyst of the tibia: a communication with the knee demonstrated by delayed arthrography. J Bone Joint Surg. 1999;81-B:643–646. doi: 10.1302/0301-620x.81b4.9445. [DOI] [PubMed] [Google Scholar]